-
PDF
- Split View
-
Views
-
Cite
Cite
S G Parker, T Downes, M Godfrey, R Matthews, F C Martin, Age and Ageing to introduce a new category of paper: healthcare improvement science, Age and Ageing, Volume 48, Issue 2, March 2019, Pages 178–184, https://doi.org/10.1093/ageing/afy175
Close - Share Icon Share
Abstract
Age and Ageing is now inviting papers on healthcare improvement for older people. In this article we outline the nature and scope of healthcare improvement and reference improvement models and the tools and methods of improvement science. We emphasise the issues of sustainability, including scale and spread; evaluation – including associated ethical consideration and the involvement of patients and the public in healthcare improvement and associated research. Throughout we refer to resources the authors have found useful in their own work, and provide a bibliography of sources and web-links which will provide essential guidance and support for potential contributors to this new category of submission to Age and Ageing.
Key points
Age and Ageing is now inviting papers on healthcare improvement for older people.
This article outlines the nature and scope of healthcare improvement and improvement models and describes the tools and methods.
Key issues include sustainability, evaluation and involvement of patients and the public in healthcare improvement activities.
A bibliography of useful resources for potential contributors is provided.
Introduction
The notion of managing and improving the quality of healthcare is enshrined in clinical governance processes and therefore regularly encountered by all practitioners. The quality and safety of healthcare is a key concern for governments, healthcare providers and practitioners, patients and carers. Improving the quality of the care and services provided for older people is core business for the readers of Age and Ageing.
Accordingly, the journal is now inviting papers on healthcare improvement for older people. These articles will describe systematic efforts intended to improve healthcare for older people, and (where specifically relevant to the care of older people) the methodological innovations by which improvement was achieved and evaluated.
Our primary intention is to disseminate information about useful interventions which have had the intended improvement results which may be able to inform improvement efforts elsewhere. This requires description of the intervention, what improvement methods were employed and why, and data supporting the proposed causal relationships with outcomes. Systematic evaluation demonstrating the lack of a desired effect and/or undesired effects can be equally useful. A closely related aim is to better understand why improvement efforts ‘worked’, (or not), i.e. what causal mechanisms were in play and what were the key enabling or moderating aspects of context demonstrated in the example reported.
Our secondary aim is to contribute to the development of the science of improvement: by this, we mean a better understanding of the various improvement approaches and how these are best studied. Such enquiry will likely illuminate the complexity of healthcare behaviours and the mechanisms by which improvements in healthcare can be achieved. Other journals are devoted entirely to this area within a much broader scope of activity: our scope will be focused on those with most relevance to a better understanding of ageing-related factors such as frailty or dementia and to the delivery of healthcare for older people.
In this paper, we will describe briefly the key elements of improvement science which will underpin the approach Age and Ageing will take in selecting submitted articles for publication. The importance of considering the SQUIRE standards for reporting, and associated glossary and explanations [1, 2] is emphasised. As well as proposing a structure for the submitted report, this guidance provides a useful glossary of terms to encourage consistency of taxonomy in this emerging science.
It is our intention that the reference list with this paper be a useful bibliography for those who are intending to submit a QI article to Age and Ageing, so we have included sources which we have found most useful and informative in our own QI work. Instructions for Authors can be found in Appendix 1, available in Age and Ageing online.
What is healthcare improvement?
Central to the notion of improving healthcare is the concept of the gaps between the care patients receive and the evidence about what they should receive. Further, it embraces the notion of service or system performance as well as the individual practitioner–patient interaction. A widely used definition of healthcare quality is from the Institute of Medicine which has six domains: safety, effectiveness, patient-centred, timely, efficiency and equity [3]. The process of healthcare improvement is about bridging gaps in any or all of these [4]. The scope of improvement includes introduction of new services, the implementation of new processes or procedures in an existing service, or modifying existing processes, for example to increase reliability efficiency or patient experience (see Table 1).
| Item . | Key points . |
|---|---|
| Introducing the problem |
|
| Rationale | What is your reason for choosing the intervention/change process? Refer to any models of improvement and/or behavioural change, and other theoretical perspectives. What assumptions underpin the expectation of intended changes? |
| Aim | Consider expressing this in terms of one or more domains of quality. Be as specific as possible. |
| Context | Describe the infrastructure, staffing, previous QI experience, levers for change, etc. See text above for further elaboration. |
| Intervention |
|
| Measuring change | Explain why and how measures were made, including short-term process changes used in PDSA as well as outcome measures reflecting the aims of the intervention |
| Analysis and Results | Explain the analytic approach, specifying how improvement was distinguished from other changes. Include balance measures. |
| Interpretation and Discussion | Main messages about both the utility of the intervention and the approach to its evaluation. Describe barriers encountered and how these were or were not overcome. Describe limitations relevant to internal and external generalisability. Consider sustainability and potential impact on clinical services. |
| Item . | Key points . |
|---|---|
| Introducing the problem |
|
| Rationale | What is your reason for choosing the intervention/change process? Refer to any models of improvement and/or behavioural change, and other theoretical perspectives. What assumptions underpin the expectation of intended changes? |
| Aim | Consider expressing this in terms of one or more domains of quality. Be as specific as possible. |
| Context | Describe the infrastructure, staffing, previous QI experience, levers for change, etc. See text above for further elaboration. |
| Intervention |
|
| Measuring change | Explain why and how measures were made, including short-term process changes used in PDSA as well as outcome measures reflecting the aims of the intervention |
| Analysis and Results | Explain the analytic approach, specifying how improvement was distinguished from other changes. Include balance measures. |
| Interpretation and Discussion | Main messages about both the utility of the intervention and the approach to its evaluation. Describe barriers encountered and how these were or were not overcome. Describe limitations relevant to internal and external generalisability. Consider sustainability and potential impact on clinical services. |
| Item . | Key points . |
|---|---|
| Introducing the problem |
|
| Rationale | What is your reason for choosing the intervention/change process? Refer to any models of improvement and/or behavioural change, and other theoretical perspectives. What assumptions underpin the expectation of intended changes? |
| Aim | Consider expressing this in terms of one or more domains of quality. Be as specific as possible. |
| Context | Describe the infrastructure, staffing, previous QI experience, levers for change, etc. See text above for further elaboration. |
| Intervention |
|
| Measuring change | Explain why and how measures were made, including short-term process changes used in PDSA as well as outcome measures reflecting the aims of the intervention |
| Analysis and Results | Explain the analytic approach, specifying how improvement was distinguished from other changes. Include balance measures. |
| Interpretation and Discussion | Main messages about both the utility of the intervention and the approach to its evaluation. Describe barriers encountered and how these were or were not overcome. Describe limitations relevant to internal and external generalisability. Consider sustainability and potential impact on clinical services. |
| Item . | Key points . |
|---|---|
| Introducing the problem |
|
| Rationale | What is your reason for choosing the intervention/change process? Refer to any models of improvement and/or behavioural change, and other theoretical perspectives. What assumptions underpin the expectation of intended changes? |
| Aim | Consider expressing this in terms of one or more domains of quality. Be as specific as possible. |
| Context | Describe the infrastructure, staffing, previous QI experience, levers for change, etc. See text above for further elaboration. |
| Intervention |
|
| Measuring change | Explain why and how measures were made, including short-term process changes used in PDSA as well as outcome measures reflecting the aims of the intervention |
| Analysis and Results | Explain the analytic approach, specifying how improvement was distinguished from other changes. Include balance measures. |
| Interpretation and Discussion | Main messages about both the utility of the intervention and the approach to its evaluation. Describe barriers encountered and how these were or were not overcome. Describe limitations relevant to internal and external generalisability. Consider sustainability and potential impact on clinical services. |
A study of four clinical systems (availability of clinical information in surgical outpatient clinics; prescribing for hospital inpatients; availability of equipment in theatres; and availability of equipment needed for the insertion of peripheral intravenous lines) in seven NHS hospitals found them to be 81%–87% reliable, each with significant inter-hospital variation, ranging typically by over 20%. A fifth of reliability failures were associated with potential clinical harm. In comparison, the worst performing airline had 2.8% reliability failure in delivering airline luggage correctly [5].
The scope of healthcare improvement
Improvement is not straightforward. Healthcare is a complex issue [6]), and requires creative processes which take account of local context, unforeseen obstacles and unintended effects [7]. The emerging discipline of improvement science is developing the theories, essential tools and frameworks that support successful implementation of improvements in healthcare.
There is no single definition of quality improvement, but it is about achieving desired outcomes across any or all domains of quality ‘through using a systematic change method and strategies’ to impact structures, processes, culture and behaviours [8]. The beginnings of many quality improvement methods can be traced back to the start of production quality control that emerged in the 1920s from pioneers such as W. Edwards Deming [9] and Walter Shewart [10] working in the early telecommunications industry. It was during this same decade that the enumerative statistical framework that drives randomised control trials was being constructed by Sir Ronald Fisher [11] and William Gosset [12] while working in agriculture and the Guinness brewery, respectively.
Quality improvement is about bringing about change in a complex healthcare system. Clinicians are already trained in a form of complex system improvement. Box 1 uses an analogy from clinical practice to illustrate the nature of the improvement process.
Assessment by history and examination
Investigation to refine or refute diagnoses, and collect collateral information
Shared decision-making to select and administer treatment
Re-evaluation quantitatively and qualitatively to determine the impact of treatment
Modifications to both the diagnostic formulation and the treatment plan
Continuing process of data acquisition, engagement and modification
Quality Improvement uses an analogous approach to improve the complex healthcare systems experienced by patients and staff.
Improvement models
A number of Improvement Models have been developed, e.g. the Knowledge to Action Framework[13], that of the USA-based Institute of Healthcare Improvement (IHI model) [14]. Other agencies have adapted or refined existing models to provide tailored guidance, for example, the NHS Change Model [15, 16] highlights the following key areas for consideration:
leadership by all
spread and adoption
improvement methodology
rigorous delivery
transparent measurement
system drivers
engagement to mobilise.
The majority share the same underlying principles:
Understanding the processes and system using tools such as process mapping, observing decision-making and practice, user/patient focus groups and patient shadowing (history and examination).
Understanding the demand, capacity and flow data of the service (investigations).
Defining the problem and causation, often enabling a graphic representation of a ‘programme theory’ (diagnosis).
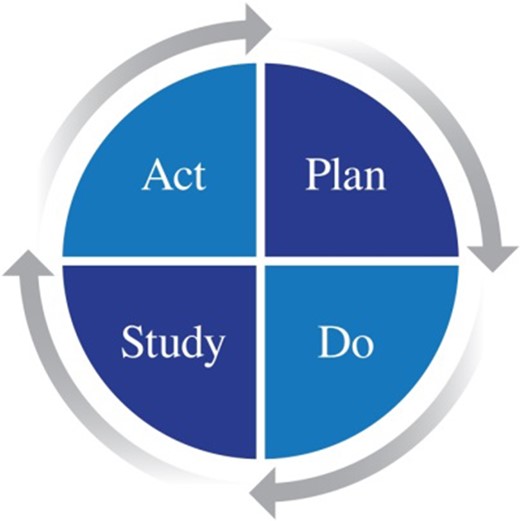
Choosing the tools such as PDSA (Plan-Do-Study-Act) to bring about change including leadership, staff engagement and patient co-design (treatment).
Evaluate and measure changes to guide modifications and recognise improvement (review).
The IHI model is widely used and like many QI methods such as Lean and Six Sigma [17], combines measurement and analysis—using statistical process control (SPC), for example—with small tests of change (plan-do-study-act (PDSA) cycles).
Quality improvement tools and methods
Tools to support quality improvement and the analysis and presentation of data are widely available from NHS improvement [18] and other organisations such as the IHI [14] and Health Quality Improvement Partnership (HQIP) [19].
A systematic review of Programme Theory diagrams (42 driver diagrams and 21 action–effect diagrams) suggested that there were common and desirable features which would lend themselves to a checklist or scoring system for use by those involved in the conduct or evaluation of healthcare improvement work [20]. These included: assessment of overall aim, logical overview, clarity of components, cause–effect relationships, evidence and measurement. Action–effect diagrams as reported in research literature from practical examples were found on average to comply better with the quality features of programme theory than driver diagrams fidelity of approach and the skill of the practitioners are probably the key issues.
The PDSA cycle is very often the engine of improvement efforts, for example, as in Lean and Six Sigma. Reed and Card (2015) [21] consider that ‘the purpose of the PDSA method lies in learning as quickly as possible whether an intervention works in a particular setting and to making adjustments accordingly to increase the chances of delivering and sustaining the desired improvement’. This iterative design process enables complex system design to be achieved in multiple small steps.
This image is reproduced from: https://deming.org/explore/p-d-s-a
PDSA cycles comprise a series of interdependent steps and key principles, the application of which is affected by local context [22]. Improvement work that successfully uses the power of PDSA can improve care pathways, behaviours and culture but collection, analysis and interpretation of the data which is collected to monitor the impact of PDSA cycles and confirm improvement is of critical importance. The need for rigour is frequently underestimated [23].
Therefore, reporting some detail of how the PDSA process was applied strengthens a QI report. Although guidance exists [24], reporting in QI articles is often poor. In a systematic review of 73 published reports which included PDSA, 47 documented the cycles in sufficient detail for full analysis against a standard framework for assessment. Overall, less than a fifth (14/73) fully documented the sequence of iterative cycles and only 15% (7/47) reported the use of quantitative data to inform progression of cycles [25].
Commonly, time series are used to display and measure change, analysed using the theory of SPC [26, 27]. This enables real-time feedback on the items of interest, which may be process changes or sometimes the targets outcomes, thus enabling modifications of the improvement activities. It is important to differentiate between background or ‘common cause’ variation in the figures (which will be present in all healthcare datasets) and ‘special cause’ variation which may be associated with external events such as the system change intervention. SPC rules are applied to distinguish special cause variation from background common cause. Equally, it is important to collect ‘balancing measures’ which may detect unintended effects [28]. Such effects may impact system efficiency of performance or patient experience. An increased occurrence of unplanned hospital readmissions is an example which impacts both. Unintended adverse effects are particularly likely in frail older people.
The key issue in the use of this method is the interpretation of the analysis, including the measure of variance used in calculating control limits and its use in informing decisions in the context of the specific healthcare quality improvement activity being undertaken [29].
The importance of context
Context is a key issue in whether and how interventions to improve healthcare quality impact the intended outcomes [24, 30–33]. Context is defined broadly as ‘all factors that are not part of a quality improvement intervention itself’ [34]. Within organisations context can mean factors such as leadership, organisational culture and data infrastructure/information systems [34]. External contexts might include the structural, political and cultural factors influencing how the implementation process will proceed [32, 33, 35, 36]. Although not mentioned as a contextual factor in the SQUIRE guidance, the patient population characteristics are clearly important in understanding the mechanism of any impact on clinical outcomes or patient experience. The applicability and feasibility of a quality improvement intervention will be affected by the patient casemix.
Context can make a big difference to ‘what works’. To illustrate how internal context might affect improvement activity, imagine how the form of leadership might be different between (for example) implementing changes in operating theatre practice and changing practice to prevent delirium in an acute medical ward. For external context, imagine how approaches to reducing the incidence of hospital acquired infection would be different between a northern European teaching hospital and an army field hospital in a war zone.
The tendency to attribute effects to interventions (rather than interventions and contexts working together) is further exacerbated by the problem that the forces that create positive conditions for quality and safety may be invisible to those who create them or may not be possible (or straightforward) to articulate. This makes it difficult for others to reproduce or recreate them.
Context cannot be understood as a fixed template upon which change happens, rather part of a complex system in which the impact of purposive changes are never precisely predictable [7]. Nevertheless, as emphasised in SQUIRE guidance, an important step in designing a QI intervention, and in reporting it, is to understand the problem, and have a theory-based rationale for the intervention chosen and the explicit assumptions underpinning the choice of its suitability. This programme theory can be articulated using one of the approaches outlined earlier.
Thus, evaluating complex change processes requires that we ask not only ‘does it work’ but for whom and in what organisational contexts. The intervention as described in published reports may offer only a partial account of the reasons why the success was achieved.
So to help others to make changes and speed up the spread of improvements proven in other settings, explanatory accounts of improvement initiatives require a descriptive account of the intervention (as implemented) and evidence of the contextual elements considered important at the outset of introducing the intervention (or change process) as recommended by SQUIRE guidance. Therefore, it may be helpful to use published TIDieR guidance in preparing a careful description of the intervention and context [37].
Sustainability
Maintaining the gains made by improvements has been recognised as a challenge for some time, and while there is diversity in the literature on how it is defined and how it can be influenced, there is one clear and compelling message: sustainability of initiatives requires thoughtful planning and attention [38]. Reports which include the sustainability approaches would be helpful to judge external feasibility. Several approaches to conceptualising and describing sustainability efforts have been published [39, 41]. Use of the comparative, case study method [54] and other types of longitudinal studies can provide insight into processes effective in sustaining and embedding change [40].
Scale and spread
In 2007, Ara Darzi wrote ‘In this country, [UK] we have a proud record of invention, but we lag behind in systematic uptake of our own inventions.’ [41] Even when ideas are adopted and embedded elsewhere, scale and spread of improvements within the NHS (and also other settings) are often slow and laborious. A Health Foundation and Innovation report in 2017 identified that greater recognition and support of both innovators and adopters is required. Innovators require resource to codify an innovation’s core features, whilst adopters need time, space and resources to implement [42]. Successful spread is, therefore, best achieved intentionally and strategically. The most widely applied and proven methodology is QI collaboratives used internationally in a broad range of health systems and in clinical settings [43], such as the Breakthrough Series Collaborative developed by the IHI [44]. A successful example in relation to reduction of central venous catheter bloodstream infections has been reported from intensive care units in the USA [45].
Other approaches include bringing together research and knowledge exchange leadership collaborations though which the principles of improvement science are developed and applied in specific contexts, such as the Australian Cognitive Decline Partnership Centre [46]. The World Health Organisation Regional Office for Europe has provided a comprehensive overview of quality of care strategies in the European Union [47].
Evaluating QI
Despite the widespread advocacy for QI, the evidence that it produces positive impacts in healthcare has been very mixed, with many of the better-designed studies producing disappointing results [48, 49]. Application of methods developed in other sectors into healthcare has invigorated improvement approaches, but evidence of successful application remains patchy [50]. Explanations include unhelpful contextual factors such as lack of senior organisational support, inconsistent use of specific QI methods, or replication in a new context of an intervention without attention (or understanding) of causal mechanisms which facilitated the desired outcomes in the original setting [51]. This underlines the need for systematic and rigorous evaluation of improvement activities [17]
Systematic review suggests that successful implementation of change is associated with fairly consistent factors in the following domains: preparation, having the people and setting with the capacity for implementation, the type of implementation employed, resources, leverage, enabling features and attention to sustainability [52]. A recent iteration based on extensive experience and literature review also incorporated concepts from complexity theory and proposed a model with 12 ‘rules’ as a practical guide for implementation and evaluation [53].
To address the issues of multiple intervention/context interactions, requires multiple methods of data gathering to gain insight into processes and outcomes from different perspectives. Qualitative methods such as interviewing and focus groups may elucidate how the quality improvement effort is understood as meaningful and engaged with by clinicians and wider groups of staff, patients and caregivers, including the barriers to, and enablers of change. Ethnographic methods can offer ‘real time’ understanding of processes, decision-making and practice in the often chaotic, complex and messy healthcare environment [54]. Observation and conversations ‘in the moment’ are particularly powerful in accessing experience of care processes among patients whose verbal facility and ability to recall is impaired as a consequence of dementia [55]. Quantitative methods including RCT’s are essential to systematic exploration of outcomes.
Similarly, different methodological approaches may address varying aspects of improvement. For example, there is increasing interest in understanding what sustains quality improvement initiatives over time (see below). Yet much of the research focuses on early phases of implementation, including introduction and early adoption.
Ethical considerations
A challenge faced by all those involved in improving healthcare is the question of ethics. For both academics and frontline staff, it can be challenging to differentiate between research, QI and clinical audit. Any activity that ‘poses a risk of psychological or physical harm to a patient’ should have ethical consideration. The Healthcare Quality Improvement Partnership (HQIP) provides guidance to aid decision-making [56].
Involvement of patients and the public in health improvement and associated research
The importance of involving potential or actual service users in healthcare improvement activities, both to assess quality of existing services or co-design innovation, is well represented in national policy guidance in most developed health services. Nevertheless, the empirical evidence of impact is poor, and learning is limited by poor reporting and weak conceptualisation [57].
In routine services, involvement is often restricted to recording patient experience but can be so much more, using the experience and insights about all aspects of design and delivery. Authentic practice, which is meaningful and conducted ‘with’ and ‘by’ patients and carers, not ‘to’, ‘for’, or ‘about’ them is elusive. In common with improvement science, involvement requires an evidence base that takes better account of context and complexity. The involvement approaches used remain underdeveloped and under-researched, usually with too little attention on how to enable shared power and decision [58].
Advances in the conceptual understanding and the practice of co-production have the potential to increase the impact of patient and public engagement and involvement in healthcare improvement [59] and will hopefully lead to more consistency and theory-based reporting of this activity. Empirical data is emerging on how best to share learning about patient and public involvement and how this contributes to improvement [60, 61].
Summary
Better understanding of QI science may be enhanced by a more consistent reporting [38]. Age & Ageing is now inviting papers on healthcare improvement for older people. Here, we have briefly described the key elements of QI science, which we hope will assist prospective authors in conducting and reporting their QI initiatives in high quality reports for submission to the journal
We emphasise the importance of considering the SQUIRE guidance [1, 2] and the instructions for authors in preparing reports for the journal. Prospective authors are encouraged to explore the resources referred to in the text and bibliography to support their work.
Declaration of Conflict of Interest: None.
Declaration of Sources of Funding: This article presents independent research funded by the National Institute for Health Research (NIHR) under the Collaboration for Leadership in Applied Health Research and Care (CLAHRC) programme for North West London. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
References
PLEASE NOTE: The very long list of references has meant that only the most important are listed here. The full list of references is available in Age and Ageing online.
https://improvement.nhs.uk/resources/ (3 September 2018, date last accessed).



Comments