-
PDF
- Split View
-
Views
-
Cite
Cite
Mikael Rostila, Agneta Cederström, Matthew Wallace, Maria Brandén, Bo Malmberg, Gunnar Andersson, Disparities in Coronavirus Disease 2019 Mortality by Country of Birth in Stockholm, Sweden: A Total-Population–Based Cohort Study, American Journal of Epidemiology, Volume 190, Issue 8, August 2021, Pages 1510–1518, https://doi.org/10.1093/aje/kwab057
Close - Share Icon Share
Abstract
Preliminary evidence points to higher morbidity and mortality from coronavirus disease 2019 (COVID-19) in certain racial and ethnic groups, but population-based studies using microlevel data are lacking so far. We used register-based cohort data including all adults living in Stockholm, Sweden, between January 31, 2020 (the date of the first confirmed case of COVID-19) and May 4, 2020 (n = 1,778,670) to conduct Poisson regression analyses with region/country of birth as the exposure and underlying cause of COVID-19 death as the outcome, estimating relative risks and 95% confidence intervals. Migrants from Middle Eastern countries (relative risk (RR) = 3.2, 95% confidence interval (CI): 2.6, 3.8), Africa (RR = 3.0, 95% CI: 2.2, 4.3), and non-Sweden Nordic countries (RR = 1.5, 95% CI: 1.2, 1.8) had higher mortality from COVID-19 than persons born in Sweden. Especially high mortality risks from COVID-19 were found among persons born in Somalia, Lebanon, Syria, Turkey, Iran, and Iraq. Socioeconomic status, number of working-age household members, and neighborhood population density attenuated up to half of the increased COVID-19 mortality risks among the foreign-born. Disadvantaged socioeconomic and living conditions may increase infection rates in migrants and contribute to their higher risk of COVID-19 mortality.
Abbreviations
- CI
confidence interval
- COVID-19
coronavirus disease 2019
- DeSO
Demographic Statistical Areas
- RR
relative risk
- SES
socioeconomic status
The coronavirus disease 2019 (COVID-19) pandemic has led to a worldwide increase in morbidity and mortality (1). Despite the widely adopted message that the virus “does not discriminate,” preliminary evidence suggests that the interaction between COVID-19 and the social environment does (2), pointing to higher morbidity and mortality among persons of low socioeconomic status (SES) and minority groups in some countries (3–6). In response, scholars have highlighted the urgent need to study social and ethnic disparities in COVID-19 morbidity and mortality (7–11) and understand the mechanisms behind them. The Swedish strategy of keeping society open and promoting individual responsibility in lieu of lockdown is unique and could have unintended consequences for vulnerable groups, including migrants (12). This fact, combined with the ability to take advantage of the detailed and reliable population registers available in Sweden, provides a unique and timely setting for the study of COVID-19 mortality among international migrants according to their country of birth.
There are a few studies on disparities in COVID-19 mortality by country of birth, with nearly all of the evidence so far pertaining to ethnic and racial disparities (3–6). Nevertheless, some studies have documented important disparities. A county-level study in the United States found that counties with higher proportions of Black residents had more COVID-19 diagnoses and deaths, after adjustment for county-level characteristics such as age, poverty, comorbidity, and epidemic duration (3). A United Kingdom study documented an increased risk of COVID-19 death for Black African, Black Caribbean, Indian, Pakistani, and Bangladeshi ethnic groups in the United Kingdom after adjustment for age and broad geographic region (4). Another United Kingdom study found that, compared with White study participants, Black participants had a 4-fold increased risk of COVID-19 infection and there was a doubled risk among Asians and other “non-Whites” (5). Niedzwiedz et al. (6) found that Black Britons and South Asian migrants were more likely to test positive for COVID-19 and more likely to be hospitalized than White Britons. Adjustment for health and behavioral risk factors led to little change, with only modest attenuation by socioeconomic variables. Nevertheless, the findings so far are not based on total-population microdata, which would provide the most reliable source of knowledge for health policy intervention.
Improving knowledge on the patterns and causes of disparities in COVID-19 mortality across migrant groups is needed in order to design health policies to prevent excess morbidity and mortality in these groups. Using microlevel registry data covering the total population in Stockholm, Sweden, we aimed in this study to: 1) document disparities in COVID-19 mortality by country of birth; 2) compare said disparities with all-cause mortality disparities excluding COVID-19 deaths occurring during the pandemic; and 3) study whether SES (education, income, and employment status), number of working-age household members, housing type, and neighborhood population density attenuated disparities in COVID-19 mortality by country of birth.
METHODS
Data
We performed a register-based cohort study that included the adult population aged 21 years or more living in Stockholm from January 31, 2020, when the first case of COVID-19 was diagnosed in Sweden, until May 4, 2020, the last date on which reliable information on COVID-19 deaths was available in our data. We included only persons who had lived in Sweden for at least 2 years in order to exclude newly arrived migrants with limited information in Swedish registers. The cohort included 1,778,670 individuals, of whom 31% were foreign-born. The data came from the collection of Swedish register data entitled “Ageing Well,” organized at Stockholm University, and comprised register data from Statistics Sweden (detailed information on socioeconomic, geographic, housing, and household-related variables for each individual) that had been linked with data in the cause-of-death register maintained by the National Board of Health and Welfare. The data cannot be made publicly available because they include sensitive personal health information protected by Swedish law. This study was approved by the Swedish Ethical Review Authority.
Variables
COVID-19 mortality was identified through the Swedish cause-of-death registry using International Classification of Diseases, Tenth Revision, codes U07.1, U07.2, and B3.42. Detailed information on country of birth was readily available in the registers. The initial phase was an exploratory data analysis that aimed to identify predictors for COVID-19 mortality. The final models included sex, age, disposable income, education, employment status, type of housing, number of working-age members in the household, and population density in the residential area. These predictors were the strongest and most stable predictors of COVID-19 mortality in our data. We considered other predictors, including occupational status. However, we did not find a strong association between occupational status and COVID-19 death, perhaps because most of the deaths were concentrated among older nonworking members of the population. Country of birth was grouped into 6 geographic areas: Sweden, other Nordic countries (Finland, Denmark, Norway, and Iceland), Europe (including Russia), the Middle East (including Turkey), Africa, and the rest of the world. Individual disposable income was grouped into quartiles, with a separate category for missing data. Education was classified into primary, secondary, and postsecondary schooling, with a separate category for missing data, while employment status was coded as a binary variable. Housing type was grouped into apartments/houses and special housing (which includes elderly-care homes), with a separate category for missing data, and the number of working-age members of the household was grouped as 0, 1–2, or ≥3. Population density at the neighborhood level was grouped into 5 quintiles and calculated on the basis of geographic partitioning of Stockholm County into 1,287 demographic statistical areas (demografiska statistikområden (DeSO)). Sweden is geographically subdivided into 5,984 DeSO with approximately 700–2,700 inhabitants each.
Statistical analyses
Duration of follow-up was defined according to the amount of time between the start date (January 31, 2020, the date of the first confirmed case in Sweden) and death or the end of follow-up (May 4, 2020). We performed Poisson regression analyses with COVID-19 death as an event, with log follow-up time included as an offset in the models, in order to estimate the mortality rate ratios between migrant groups and native-born Swedes. When population density was included, a random-intercept multilevel Poisson model was used to account for the dependence between individual-level observations on the group level, with DeSO as the grouping variable, and we calculated the median rate ratio to assess the general contextual effect. In the multilevel models, aggregated data were used to decrease computation time in which the death count in each category of the covariates (age, sex, country of birth, etc.) was aggregated and used as the outcome. We also fitted the corresponding models with all-cause mortality excluding COVID-19 mortality as a comparison. We nested 3 models: Model 1 adjusted only for age and sex; model 2 added the socioeconomic variables income, education, and employment status; and model 3 also included housing type, number of working-age members in the household, and population density on the DeSO level. To understand which specific birth countries were driving the grouped birth country results, we also fitted models 1–3 on detailed birth country.
We also carried out some sensitivity analyses to complement our main results. First, we fitted models considering the independent contributions of the mediating variables of interest to assess their relative contributions to migrants’ excess risk of mortality from COVID-19. Second, to examine sex differences in migrant groups, we fitted models 1–3, specifying an interaction between sex and migrants’ region of origin. Third, to examine age differences in migrant groups, we fitted models 1–3 with stratification for the age groups ≤65 years and ≥66 years. Fourth, because we were concerned about restricting the available data to Stockholm, rather than all of Sweden (though Stockholm is the worst-hit region thus far), we fitted models 1–3 with the entire population of Sweden. Specifically, we specified an interaction between residence in Stockholm County and migrants’ region of origin. Results from all of these analyses are available in the Web material and are described briefly at the end of the Results section. The statistical analyses were performed using R 4.0.1 (R Core Team, 2020; R Foundation for Statistical Computing, Vienna, Austria), and the lme4 (version 1.1-25 (2020)) software package (13).
RESULTS
Table 1 presents descriptive statistics for COVID-19 deaths, for deaths due to all other causes, and for predictor variables: income, education, employment, number of working-age household members, housing type, and neighborhood population density. Data are provided for the total population of Stockholm by region of birth, showing considerable variation. Web Figures 1–3 (available at https://doi.org/10.1093/aje/kwab057) provide information on the distribution of COVID-19 deaths by calendar date (Web Figure 1), age and nativity status (Web Figure 2), and age and grouped birth country (Web Figure 3).
Characteristics of the Adult Population of Stockholm, Sweden, by Region of Birth, January 31–May 4, 2020
| . | Geographic Area of Birth . | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic . | Sweden . | Other Nordic Countries . | Europe . | Middle East . | Africa . | Rest of World . | ||||||
| No. . | % . | No. . | % . | No. . | % . | No. . | % . | No. . | % . | No. . | % . | |
| Population size | 1,232,511 | 58,206 | 165,988 | 127,125 | 63,461 | 131,379 | ||||||
| Period at risk, years | 313,336 | 14,772 | 42,219 | 32,432 | 16,151 | 33,438 | ||||||
| Mortality | ||||||||||||
| COVID-19 deaths | 1,016 | 129 | 106 | 135 | 35 | 33 | ||||||
| Other deaths | 3,313 | 324 | 299 | 149 | 45 | 81 | ||||||
| Age group, years | ||||||||||||
| 21–49 | 648,203 | 53 | 13,729 | 24 | 105,959 | 64 | 77,000 | 61 | 45,169 | 71 | 95,689 | 73 |
| 50–64 | 291,142 | 24 | 17,145 | 29 | 32,380 | 20 | 35,245 | 28 | 13,970 | 22 | 25,087 | 19 |
| ≥65 | 293,166 | 24 | 27,332 | 47 | 27,649 | 17 | 14,880 | 12 | 4,322 | 7 | 10,603 | 8 |
| Sex | ||||||||||||
| Male | 622,584 | 51 | 36,258 | 62 | 81,765 | 49 | 59,080 | 46 | 29,310 | 46 | 68,687 | 52 |
| Female | 609,927 | 49 | 21,948 | 38 | 84,223 | 51 | 68,045 | 54 | 34,151 | 54 | 62,692 | 48 |
| Educational level | ||||||||||||
| Postsecondary education | 610,761 | 50 | 22,152 | 38 | 73,862 | 44 | 46,185 | 36 | 18,132 | 29 | 58,982 | 45 |
| Secondary education | 485,916 | 39 | 21,846 | 38 | 45,917 | 28 | 39,849 | 31 | 23,820 | 38 | 33,156 | 25 |
| Primary education | 126,875 | 10 | 11,279 | 19 | 14,420 | 9 | 32,044 | 25 | 15,290 | 24 | 17,330 | 13 |
| Missing data | 8,959 | 1 | 2,929 | 5 | 31,789 | 19 | 9,047 | 7 | 6,219 | 10 | 21,911 | 17 |
| Quartile of disposable income | ||||||||||||
| 1 (least income) | 237,090 | 19 | 17,109 | 29 | 58,211 | 35 | 52,879 | 42 | 24,237 | 38 | 48,394 | 37 |
| 2 (less income) | 302,351 | 25 | 15,699 | 27 | 39,027 | 24 | 32,717 | 26 | 17,920 | 28 | 29,866 | 23 |
| 3 (more income) | 325,684 | 26 | 12,262 | 21 | 35,138 | 21 | 25,507 | 20 | 13,544 | 21 | 25,843 | 20 |
| 4 (most income) | 364,931 | 30 | 12,042 | 21 | 24,840 | 15 | 13,320 | 10 | 5,204 | 8 | 17,368 | 13 |
| Missing data | 2,455 | 0 | 1,094 | 2 | 8,772 | 5 | 2,702 | 2 | 2,556 | 4 | 9,908 | 8 |
| Employed | ||||||||||||
| Yes | 959,242 | 78 | 31,952 | 55 | 111,738 | 67 | 84,677 | 67 | 44,632 | 70 | 90,006 | 69 |
| No | 273,269 | 22 | 26,254 | 45 | 54,250 | 33 | 42,448 | 33 | 18,829 | 30 | 41,373 | 31 |
| Housing type | ||||||||||||
| House or apartment | 754,130 | 61 | 37,980 | 65 | 122,599 | 74 | 95,084 | 75 | 54,392 | 86 | 102,856 | 78 |
| Special-care housing | 12,836 | 1 | 1,199 | 2 | 1,324 | 1 | 1,834 | 1 | 1,418 | 2 | 1,049 | 1 |
| Missing data | 465,545 | 38 | 19,027 | 33 | 42,065 | 25 | 30,207 | 24 | 7,651 | 12 | 27,474 | 21 |
| No. of working-age persons in household | ||||||||||||
| 0 | 231,143 | 19 | 21,212 | 36 | 18,164 | 11 | 7,435 | 6 | 1,629 | 3 | 5,295 | 4 |
| 1–2 | 797,752 | 65 | 29,269 | 50 | 90,104 | 54 | 71,525 | 56 | 34,075 | 54 | 77,208 | 59 |
| ≥3 | 177,104 | 14 | 6,256 | 11 | 50,550 | 30 | 43,817 | 34 | 25,273 | 40 | 44,038 | 34 |
| Missing data | 26,512 | 2 | 1,469 | 3 | 7,170 | 4 | 4,348 | 3 | 2,484 | 4 | 4,838 | 4 |
| Quintile of population density | ||||||||||||
| 1 (least dense) | 274,777 | 22 | 13,455 | 23 | 26,836 | 16 | 18,108 | 14 | 5,820 | 9 | 16,615 | 13 |
| 2 (less dense) | 257,729 | 21 | 11,565 | 20 | 29,827 | 18 | 22,481 | 18 | 8,534 | 13 | 24,229 | 18 |
| 3 (somewhat dense) | 238,296 | 19 | 11,953 | 21 | 34,726 | 21 | 30,324 | 24 | 12,578 | 20 | 27,127 | 21 |
| 4 (more dense) | 223,069 | 18 | 10,984 | 19 | 38,517 | 23 | 29,406 | 23 | 20,023 | 32 | 32,819 | 25 |
| 5 (most dense) | 236,307 | 19 | 10,065 | 17 | 35,200 | 21 | 26,387 | 21 | 15,984 | 25 | 30,164 | 23 |
| Missing data | 2,333 | 0 | 184 | 0 | 882 | 1 | 419 | 0 | 522 | 1 | 425 | 0 |
| . | Geographic Area of Birth . | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic . | Sweden . | Other Nordic Countries . | Europe . | Middle East . | Africa . | Rest of World . | ||||||
| No. . | % . | No. . | % . | No. . | % . | No. . | % . | No. . | % . | No. . | % . | |
| Population size | 1,232,511 | 58,206 | 165,988 | 127,125 | 63,461 | 131,379 | ||||||
| Period at risk, years | 313,336 | 14,772 | 42,219 | 32,432 | 16,151 | 33,438 | ||||||
| Mortality | ||||||||||||
| COVID-19 deaths | 1,016 | 129 | 106 | 135 | 35 | 33 | ||||||
| Other deaths | 3,313 | 324 | 299 | 149 | 45 | 81 | ||||||
| Age group, years | ||||||||||||
| 21–49 | 648,203 | 53 | 13,729 | 24 | 105,959 | 64 | 77,000 | 61 | 45,169 | 71 | 95,689 | 73 |
| 50–64 | 291,142 | 24 | 17,145 | 29 | 32,380 | 20 | 35,245 | 28 | 13,970 | 22 | 25,087 | 19 |
| ≥65 | 293,166 | 24 | 27,332 | 47 | 27,649 | 17 | 14,880 | 12 | 4,322 | 7 | 10,603 | 8 |
| Sex | ||||||||||||
| Male | 622,584 | 51 | 36,258 | 62 | 81,765 | 49 | 59,080 | 46 | 29,310 | 46 | 68,687 | 52 |
| Female | 609,927 | 49 | 21,948 | 38 | 84,223 | 51 | 68,045 | 54 | 34,151 | 54 | 62,692 | 48 |
| Educational level | ||||||||||||
| Postsecondary education | 610,761 | 50 | 22,152 | 38 | 73,862 | 44 | 46,185 | 36 | 18,132 | 29 | 58,982 | 45 |
| Secondary education | 485,916 | 39 | 21,846 | 38 | 45,917 | 28 | 39,849 | 31 | 23,820 | 38 | 33,156 | 25 |
| Primary education | 126,875 | 10 | 11,279 | 19 | 14,420 | 9 | 32,044 | 25 | 15,290 | 24 | 17,330 | 13 |
| Missing data | 8,959 | 1 | 2,929 | 5 | 31,789 | 19 | 9,047 | 7 | 6,219 | 10 | 21,911 | 17 |
| Quartile of disposable income | ||||||||||||
| 1 (least income) | 237,090 | 19 | 17,109 | 29 | 58,211 | 35 | 52,879 | 42 | 24,237 | 38 | 48,394 | 37 |
| 2 (less income) | 302,351 | 25 | 15,699 | 27 | 39,027 | 24 | 32,717 | 26 | 17,920 | 28 | 29,866 | 23 |
| 3 (more income) | 325,684 | 26 | 12,262 | 21 | 35,138 | 21 | 25,507 | 20 | 13,544 | 21 | 25,843 | 20 |
| 4 (most income) | 364,931 | 30 | 12,042 | 21 | 24,840 | 15 | 13,320 | 10 | 5,204 | 8 | 17,368 | 13 |
| Missing data | 2,455 | 0 | 1,094 | 2 | 8,772 | 5 | 2,702 | 2 | 2,556 | 4 | 9,908 | 8 |
| Employed | ||||||||||||
| Yes | 959,242 | 78 | 31,952 | 55 | 111,738 | 67 | 84,677 | 67 | 44,632 | 70 | 90,006 | 69 |
| No | 273,269 | 22 | 26,254 | 45 | 54,250 | 33 | 42,448 | 33 | 18,829 | 30 | 41,373 | 31 |
| Housing type | ||||||||||||
| House or apartment | 754,130 | 61 | 37,980 | 65 | 122,599 | 74 | 95,084 | 75 | 54,392 | 86 | 102,856 | 78 |
| Special-care housing | 12,836 | 1 | 1,199 | 2 | 1,324 | 1 | 1,834 | 1 | 1,418 | 2 | 1,049 | 1 |
| Missing data | 465,545 | 38 | 19,027 | 33 | 42,065 | 25 | 30,207 | 24 | 7,651 | 12 | 27,474 | 21 |
| No. of working-age persons in household | ||||||||||||
| 0 | 231,143 | 19 | 21,212 | 36 | 18,164 | 11 | 7,435 | 6 | 1,629 | 3 | 5,295 | 4 |
| 1–2 | 797,752 | 65 | 29,269 | 50 | 90,104 | 54 | 71,525 | 56 | 34,075 | 54 | 77,208 | 59 |
| ≥3 | 177,104 | 14 | 6,256 | 11 | 50,550 | 30 | 43,817 | 34 | 25,273 | 40 | 44,038 | 34 |
| Missing data | 26,512 | 2 | 1,469 | 3 | 7,170 | 4 | 4,348 | 3 | 2,484 | 4 | 4,838 | 4 |
| Quintile of population density | ||||||||||||
| 1 (least dense) | 274,777 | 22 | 13,455 | 23 | 26,836 | 16 | 18,108 | 14 | 5,820 | 9 | 16,615 | 13 |
| 2 (less dense) | 257,729 | 21 | 11,565 | 20 | 29,827 | 18 | 22,481 | 18 | 8,534 | 13 | 24,229 | 18 |
| 3 (somewhat dense) | 238,296 | 19 | 11,953 | 21 | 34,726 | 21 | 30,324 | 24 | 12,578 | 20 | 27,127 | 21 |
| 4 (more dense) | 223,069 | 18 | 10,984 | 19 | 38,517 | 23 | 29,406 | 23 | 20,023 | 32 | 32,819 | 25 |
| 5 (most dense) | 236,307 | 19 | 10,065 | 17 | 35,200 | 21 | 26,387 | 21 | 15,984 | 25 | 30,164 | 23 |
| Missing data | 2,333 | 0 | 184 | 0 | 882 | 1 | 419 | 0 | 522 | 1 | 425 | 0 |
Abbreviation: COVID, coronavirus disease 2019.
Characteristics of the Adult Population of Stockholm, Sweden, by Region of Birth, January 31–May 4, 2020
| . | Geographic Area of Birth . | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic . | Sweden . | Other Nordic Countries . | Europe . | Middle East . | Africa . | Rest of World . | ||||||
| No. . | % . | No. . | % . | No. . | % . | No. . | % . | No. . | % . | No. . | % . | |
| Population size | 1,232,511 | 58,206 | 165,988 | 127,125 | 63,461 | 131,379 | ||||||
| Period at risk, years | 313,336 | 14,772 | 42,219 | 32,432 | 16,151 | 33,438 | ||||||
| Mortality | ||||||||||||
| COVID-19 deaths | 1,016 | 129 | 106 | 135 | 35 | 33 | ||||||
| Other deaths | 3,313 | 324 | 299 | 149 | 45 | 81 | ||||||
| Age group, years | ||||||||||||
| 21–49 | 648,203 | 53 | 13,729 | 24 | 105,959 | 64 | 77,000 | 61 | 45,169 | 71 | 95,689 | 73 |
| 50–64 | 291,142 | 24 | 17,145 | 29 | 32,380 | 20 | 35,245 | 28 | 13,970 | 22 | 25,087 | 19 |
| ≥65 | 293,166 | 24 | 27,332 | 47 | 27,649 | 17 | 14,880 | 12 | 4,322 | 7 | 10,603 | 8 |
| Sex | ||||||||||||
| Male | 622,584 | 51 | 36,258 | 62 | 81,765 | 49 | 59,080 | 46 | 29,310 | 46 | 68,687 | 52 |
| Female | 609,927 | 49 | 21,948 | 38 | 84,223 | 51 | 68,045 | 54 | 34,151 | 54 | 62,692 | 48 |
| Educational level | ||||||||||||
| Postsecondary education | 610,761 | 50 | 22,152 | 38 | 73,862 | 44 | 46,185 | 36 | 18,132 | 29 | 58,982 | 45 |
| Secondary education | 485,916 | 39 | 21,846 | 38 | 45,917 | 28 | 39,849 | 31 | 23,820 | 38 | 33,156 | 25 |
| Primary education | 126,875 | 10 | 11,279 | 19 | 14,420 | 9 | 32,044 | 25 | 15,290 | 24 | 17,330 | 13 |
| Missing data | 8,959 | 1 | 2,929 | 5 | 31,789 | 19 | 9,047 | 7 | 6,219 | 10 | 21,911 | 17 |
| Quartile of disposable income | ||||||||||||
| 1 (least income) | 237,090 | 19 | 17,109 | 29 | 58,211 | 35 | 52,879 | 42 | 24,237 | 38 | 48,394 | 37 |
| 2 (less income) | 302,351 | 25 | 15,699 | 27 | 39,027 | 24 | 32,717 | 26 | 17,920 | 28 | 29,866 | 23 |
| 3 (more income) | 325,684 | 26 | 12,262 | 21 | 35,138 | 21 | 25,507 | 20 | 13,544 | 21 | 25,843 | 20 |
| 4 (most income) | 364,931 | 30 | 12,042 | 21 | 24,840 | 15 | 13,320 | 10 | 5,204 | 8 | 17,368 | 13 |
| Missing data | 2,455 | 0 | 1,094 | 2 | 8,772 | 5 | 2,702 | 2 | 2,556 | 4 | 9,908 | 8 |
| Employed | ||||||||||||
| Yes | 959,242 | 78 | 31,952 | 55 | 111,738 | 67 | 84,677 | 67 | 44,632 | 70 | 90,006 | 69 |
| No | 273,269 | 22 | 26,254 | 45 | 54,250 | 33 | 42,448 | 33 | 18,829 | 30 | 41,373 | 31 |
| Housing type | ||||||||||||
| House or apartment | 754,130 | 61 | 37,980 | 65 | 122,599 | 74 | 95,084 | 75 | 54,392 | 86 | 102,856 | 78 |
| Special-care housing | 12,836 | 1 | 1,199 | 2 | 1,324 | 1 | 1,834 | 1 | 1,418 | 2 | 1,049 | 1 |
| Missing data | 465,545 | 38 | 19,027 | 33 | 42,065 | 25 | 30,207 | 24 | 7,651 | 12 | 27,474 | 21 |
| No. of working-age persons in household | ||||||||||||
| 0 | 231,143 | 19 | 21,212 | 36 | 18,164 | 11 | 7,435 | 6 | 1,629 | 3 | 5,295 | 4 |
| 1–2 | 797,752 | 65 | 29,269 | 50 | 90,104 | 54 | 71,525 | 56 | 34,075 | 54 | 77,208 | 59 |
| ≥3 | 177,104 | 14 | 6,256 | 11 | 50,550 | 30 | 43,817 | 34 | 25,273 | 40 | 44,038 | 34 |
| Missing data | 26,512 | 2 | 1,469 | 3 | 7,170 | 4 | 4,348 | 3 | 2,484 | 4 | 4,838 | 4 |
| Quintile of population density | ||||||||||||
| 1 (least dense) | 274,777 | 22 | 13,455 | 23 | 26,836 | 16 | 18,108 | 14 | 5,820 | 9 | 16,615 | 13 |
| 2 (less dense) | 257,729 | 21 | 11,565 | 20 | 29,827 | 18 | 22,481 | 18 | 8,534 | 13 | 24,229 | 18 |
| 3 (somewhat dense) | 238,296 | 19 | 11,953 | 21 | 34,726 | 21 | 30,324 | 24 | 12,578 | 20 | 27,127 | 21 |
| 4 (more dense) | 223,069 | 18 | 10,984 | 19 | 38,517 | 23 | 29,406 | 23 | 20,023 | 32 | 32,819 | 25 |
| 5 (most dense) | 236,307 | 19 | 10,065 | 17 | 35,200 | 21 | 26,387 | 21 | 15,984 | 25 | 30,164 | 23 |
| Missing data | 2,333 | 0 | 184 | 0 | 882 | 1 | 419 | 0 | 522 | 1 | 425 | 0 |
| . | Geographic Area of Birth . | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic . | Sweden . | Other Nordic Countries . | Europe . | Middle East . | Africa . | Rest of World . | ||||||
| No. . | % . | No. . | % . | No. . | % . | No. . | % . | No. . | % . | No. . | % . | |
| Population size | 1,232,511 | 58,206 | 165,988 | 127,125 | 63,461 | 131,379 | ||||||
| Period at risk, years | 313,336 | 14,772 | 42,219 | 32,432 | 16,151 | 33,438 | ||||||
| Mortality | ||||||||||||
| COVID-19 deaths | 1,016 | 129 | 106 | 135 | 35 | 33 | ||||||
| Other deaths | 3,313 | 324 | 299 | 149 | 45 | 81 | ||||||
| Age group, years | ||||||||||||
| 21–49 | 648,203 | 53 | 13,729 | 24 | 105,959 | 64 | 77,000 | 61 | 45,169 | 71 | 95,689 | 73 |
| 50–64 | 291,142 | 24 | 17,145 | 29 | 32,380 | 20 | 35,245 | 28 | 13,970 | 22 | 25,087 | 19 |
| ≥65 | 293,166 | 24 | 27,332 | 47 | 27,649 | 17 | 14,880 | 12 | 4,322 | 7 | 10,603 | 8 |
| Sex | ||||||||||||
| Male | 622,584 | 51 | 36,258 | 62 | 81,765 | 49 | 59,080 | 46 | 29,310 | 46 | 68,687 | 52 |
| Female | 609,927 | 49 | 21,948 | 38 | 84,223 | 51 | 68,045 | 54 | 34,151 | 54 | 62,692 | 48 |
| Educational level | ||||||||||||
| Postsecondary education | 610,761 | 50 | 22,152 | 38 | 73,862 | 44 | 46,185 | 36 | 18,132 | 29 | 58,982 | 45 |
| Secondary education | 485,916 | 39 | 21,846 | 38 | 45,917 | 28 | 39,849 | 31 | 23,820 | 38 | 33,156 | 25 |
| Primary education | 126,875 | 10 | 11,279 | 19 | 14,420 | 9 | 32,044 | 25 | 15,290 | 24 | 17,330 | 13 |
| Missing data | 8,959 | 1 | 2,929 | 5 | 31,789 | 19 | 9,047 | 7 | 6,219 | 10 | 21,911 | 17 |
| Quartile of disposable income | ||||||||||||
| 1 (least income) | 237,090 | 19 | 17,109 | 29 | 58,211 | 35 | 52,879 | 42 | 24,237 | 38 | 48,394 | 37 |
| 2 (less income) | 302,351 | 25 | 15,699 | 27 | 39,027 | 24 | 32,717 | 26 | 17,920 | 28 | 29,866 | 23 |
| 3 (more income) | 325,684 | 26 | 12,262 | 21 | 35,138 | 21 | 25,507 | 20 | 13,544 | 21 | 25,843 | 20 |
| 4 (most income) | 364,931 | 30 | 12,042 | 21 | 24,840 | 15 | 13,320 | 10 | 5,204 | 8 | 17,368 | 13 |
| Missing data | 2,455 | 0 | 1,094 | 2 | 8,772 | 5 | 2,702 | 2 | 2,556 | 4 | 9,908 | 8 |
| Employed | ||||||||||||
| Yes | 959,242 | 78 | 31,952 | 55 | 111,738 | 67 | 84,677 | 67 | 44,632 | 70 | 90,006 | 69 |
| No | 273,269 | 22 | 26,254 | 45 | 54,250 | 33 | 42,448 | 33 | 18,829 | 30 | 41,373 | 31 |
| Housing type | ||||||||||||
| House or apartment | 754,130 | 61 | 37,980 | 65 | 122,599 | 74 | 95,084 | 75 | 54,392 | 86 | 102,856 | 78 |
| Special-care housing | 12,836 | 1 | 1,199 | 2 | 1,324 | 1 | 1,834 | 1 | 1,418 | 2 | 1,049 | 1 |
| Missing data | 465,545 | 38 | 19,027 | 33 | 42,065 | 25 | 30,207 | 24 | 7,651 | 12 | 27,474 | 21 |
| No. of working-age persons in household | ||||||||||||
| 0 | 231,143 | 19 | 21,212 | 36 | 18,164 | 11 | 7,435 | 6 | 1,629 | 3 | 5,295 | 4 |
| 1–2 | 797,752 | 65 | 29,269 | 50 | 90,104 | 54 | 71,525 | 56 | 34,075 | 54 | 77,208 | 59 |
| ≥3 | 177,104 | 14 | 6,256 | 11 | 50,550 | 30 | 43,817 | 34 | 25,273 | 40 | 44,038 | 34 |
| Missing data | 26,512 | 2 | 1,469 | 3 | 7,170 | 4 | 4,348 | 3 | 2,484 | 4 | 4,838 | 4 |
| Quintile of population density | ||||||||||||
| 1 (least dense) | 274,777 | 22 | 13,455 | 23 | 26,836 | 16 | 18,108 | 14 | 5,820 | 9 | 16,615 | 13 |
| 2 (less dense) | 257,729 | 21 | 11,565 | 20 | 29,827 | 18 | 22,481 | 18 | 8,534 | 13 | 24,229 | 18 |
| 3 (somewhat dense) | 238,296 | 19 | 11,953 | 21 | 34,726 | 21 | 30,324 | 24 | 12,578 | 20 | 27,127 | 21 |
| 4 (more dense) | 223,069 | 18 | 10,984 | 19 | 38,517 | 23 | 29,406 | 23 | 20,023 | 32 | 32,819 | 25 |
| 5 (most dense) | 236,307 | 19 | 10,065 | 17 | 35,200 | 21 | 26,387 | 21 | 15,984 | 25 | 30,164 | 23 |
| Missing data | 2,333 | 0 | 184 | 0 | 882 | 1 | 419 | 0 | 522 | 1 | 425 | 0 |
Abbreviation: COVID, coronavirus disease 2019.
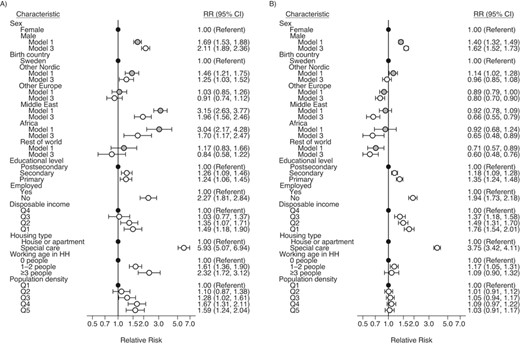
Figure 1A shows initial elevated age- and sex-adjusted mortality rate ratios from COVID-19 in model 1 among migrants from the Middle East (relative risk (RR) = 3.2, 95% confidence interval (CI): 2.6, 3.8), Africa (RR = 3.0, 95% CI: 2.2, 4.3), and the other Nordic countries (RR = 1.5, 95% CI: 1.2, 1.8) in comparison with the Swedish-born population living in Stockholm. These excess relative risks are attenuated for all 3 migrant groups when socioeconomic, housing, and neighborhood characteristics are considered. In model 3, mortality rate ratios fall considerably but remained elevated among migrants from the Middle East (RR = 2.0, 95% CI: 1.6, 2.5), Africa (RR = 1.7, 95% CI: 1.2, 2.5), and the other Nordic countries (RR = 1.3, 95% CI: 1.0, 1.5). Web Table 1 shows that 45% of the overall excess mortality is explained for migrants from the other Nordic countries (largely because of the addition of socioeconomic factors between model 1 and model 2), 56% for those from the Middle East (largely between model 1 and model 2), and 66% for those from Africa (split more equally between the addition of socioeconomic factors between model 1 and model 2 and neighborhood and household factors between model 2 and model 3). Web Table 2 indicates that, of the predictors included in the models, disposable income, employment status, and population density primarily contribute to the associations found, while housing type does not. In model 3 the median rate ratio is 1.77, indicating a fairly large contextual effect—meaning that the rate of change in the occurrence of COVID-19 mortality when comparing identical subjects from 2 randomly selected neighborhoods is substantial.
A) Relative risk (RR) of coronavirus disease 2019 (COVID-19) mortality among migrants to Sweden, by region of origin, as compared with the Swedish-born population, January 31–May 4, 2020. In model 1 (gray circles), the RRs were adjusted for age and sex only, while in model 3 (white circles) they were adjusted for socioeconomic status, housing, and neighborhood characteristics. Disposable income was categorized into 4 quartiles (Q1–Q4) and population density was categorized into 5 quintiles (Q1–Q5). B) RRs for all-cause mortality excluding COVID-19 deaths. The estimates for age are not shown, because the values were on a different scale. Black circles represent the reference group for each risk factor analyzed. Bars, 95% confidence intervals (CIs). HH, household.
In Figure 1B, we present results from a similar analysis for all-cause mortality excluding deaths from COVID-19. Initially, we find no excess relative risk for the migrant groups except for migrants from the other Nordic countries, who have a slightly elevated mortality risk in model 1 (RR = 1.1, 95% CI: 1.0, 1.3). As is the case with COVID-19 deaths, adjusting for SES reduces the relative death risk of migrants. For all-cause mortality excluding COVID-19, this leads to the emergence of sizeable mortality advantages in nearly all groups as compared with the Swedish population in model 3: Europe (RR = 0.8, 95% CI: 0.7, 0.9), the Middle East (RR = 0.7, 95% CI: 0.6, 0.8), Africa (RR = 0.7, 95% CI: 0.5, 0.9), and the rest of the world (RR = 0.6, 95% CI: 0.5, 0.8). In contrast to the COVID-19 model, risk factors specific to COVID-19 mortality did not significantly affect all-cause mortality without COVID-19 deaths. In the multilevel model, we found a significantly lower median rate ratio of 1.19, indicating that contextual effects are much less pronounced for all-cause mortality. Full regression tables for the models shown in Figure 1 can be found in Web Table 3 (for COVID-19) and Web Table 4 (for all other causes of death combined).
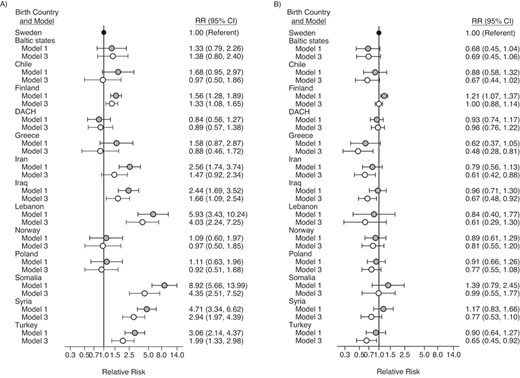
Figure 2A shows a more granular origin variable for migrants, displaying mortality rate ratios for individual birth countries for which at least 10 COVID-19 deaths have been recorded in Stockholm. The numbers of deaths, population sizes, and durations of time at risk are shown in Web Table 5. We found elevated mortality rate ratios for COVID-19 among migrants from Finland (RR = 1.6, 95% CI:1.3, 1.9), Iran (RR = 2.6, 95% CI: 1.7, 3.7), Iraq (RR = 2.4, 95% CI: 1.7, 3.5), Lebanon (RR = 5.9, 95% CI: 3.4, 10.2), Somalia (RR = 8.9, 95% CI: 5.7, 14.0), Syria (RR = 4.7, 95% CI: 3.3, 6.6), and Turkey (RR = 3.1, 95% CI: 2.1, 4.4), but not for the Baltic states (Estonia, Latvia, and Lithuania), Chile, the Germanic states (Germany, Austria, and Switzerland), Greece (including Cyprus), Norway, or Poland. These excess relative risks are attenuated to varying degrees when socioeconomic, housing, and neighborhood characteristics are considered, ranging from 38% of the excess risk being explained for Lebanon to 70% for Iran (see Web Table 1). This is reflected in comparatively lower excess risks in model 3 among migrants from Iran (RR = 1.5, 95% CI: 0.9, 2.3), Finland (RR = 1.3, 95% CI: 1.1, 1.7), Iraq (RR = 1.7, 95% CI: 1.1, 2.5), Lebanon (RR = 4.0, 95% CI: 2.2, 7.3), Somalia (RR = 4.4, 95% CI: 2.5, 7.5), Syria (RR = 2.9, 95% CI: 2.0, 4.4), and Turkey (RR = 2.0, 95% CI: 1.3, 3.0).
A) Relative risk (RR) of coronavirus disease 2019 (COVID-19) mortality among migrants to Sweden, by birth country, as compared with the Swedish-born population, January 31–May 4, 2020. In model 1 (gray circles), the RRs were adjusted for age and sex only, while in model 3 (white circles) they were adjusted for socioeconomic status, housing, and neighborhood characteristics. B) RRs for all-cause mortality excluding COVID-19 deaths. Only estimates for birth country are shown. Black circles represent the reference group (birth in Sweden). Bars, 95% confidence intervals (CIs). DACH, Deutschland, Austria, Confoederatio Helvetica (Germany, Austria, and Switzerland).
In Figure 2B, the analysis for all-cause mortality (excluding COVID-19 deaths) shows an initial excess relative risk only among migrants from Finland (RR = 1.2, 95% CI: 1.1, 1.4) in model 1. As for the regions of origin, we found lower mortality in comparison with the Swedish population after adjusting for SES, housing type, and neighborhood characteristics in model 3, including for those countries where we observed large COVID-19 death risks, such as Iran (RR = 0.6, 95% CI: 0.4, 0.9), Iraq (RR = 0.7, 95% CI: 0.5, 0.9), and Turkey (RR = 0.7, 95% CI: 0.5, 0.9). Partial regression tables (showing the relative risks for the exposure variable only) for the models presented in Figure 2 can be found in Web Table 6 (for COVID-19) and Web Table 7 (for all other causes of death combined). The values for the median rate ratio were not significantly different from those for the country-specific models.
In the sensitivity analyses, we first included all of Sweden and interacted country of birth with a dichotomous variable indicating whether an individual lived in the Stockholm area or not. These analyses, shown in Web Table 8, indicated that migrants from the Middle East and Africa had elevated mortality from COVID-19 irrespective of whether they lived in Stockholm or elsewhere in Sweden. However, the size of the mortality rate ratio was much larger among migrants in these 2 groups if they lived in other parts of Sweden. This analysis also revealed that excess COVID-19 mortality among migrants from othe Nordic countries was largely a feature of those living in Stockholm.
Second, the interaction between country of birth and sex (Web Table 9) revealed that the magnitudes of the initial incidence rate ratios were smaller among women from the other Nordic countries, Africa, and the Middle East than among men from those countries. Adjusting for socioeconomic and living conditions then attenuated the risks more in the male populations than in the female ones, leading to excesses of a similar magnitude in the fully adjusted model.
Finally, stratifying the analyses by age (Web Table 10) revealed that the disparities observed in Figure 1 were consistent by age. Namely, for persons aged ≤65 years and ≥66 years alike, there were elevated rate ratios for COVID-19 mortality among migrants from other Nordic countries, the Middle East, and Africa. However, the risk ratio for COVID-19 mortality was much larger at young-to-midlife ages than at older ages in all groups (most notably among African migrants).
DISCUSSION
Findings
In this study, we examined disparities in COVID-19 mortality by birth country among migrants in Stockholm and investigated whether any disparities could be explained by socioeconomic and living conditions. We also analyzed all-cause mortality minus COVID-19 deaths that occurred during the pandemic to determine whether migrants are particularly overrepresented among persons dying from COVID-19. We found substantially higher COVID-19 mortality among migrants from Middle Eastern countries and Africa but also among migrants from the Nordic countries in comparison with Swedish-born individuals. When studying specific birth countries, we found especially high and persistent COVID-19 mortality among persons born in Somalia, Lebanon, Syria, and Turkey. We also found that the relative risk of COVID-19 death was more than doubled among people born in Iran or Iraq. A moderately higher risk was also found among migrants from Finland. In addition, differences in socioeconomic, household, and neighborhood characteristics explained one-half to two-thirds of the excess relative risk. All of this stands in sharp contrast to the results for all-cause mortality excluding COVID-19, where most migrant groups had lower mortality than native-born Swedes during the pandemic, consistent with previous findings in Sweden (14, 15). Taken together, these findings suggest that many migrant groups have been particularly vulnerable to death during the COVID-19 pandemic.
In the literature, 2 main explanations for higher COVID-19 mortality among certain ethnic groups can be distinguished (8, 16). The first relates to vulnerabilities due to a generally lower SES among migrants, which in turn implies poorer living conditions. Not being able to successfully socially isolate, due to low income or crowded housing, is likely to amplify both infection rates and, subsequently, death rates. The second explanation relates to the higher prevalence of underlying risk factors in migrants or higher genetic vulnerability for infectious diseases leading to a higher fatality rate.
Our findings suggested that some of the increased COVID-19 mortality risk was attenuated after adjustment for education, disposable income, and employment status, which suggests that poorer socioeconomic conditions could explain some of the higher COVID-19 mortality in foreign-born persons. Lower SES translates into occupations that are more precarious (17) and more often found in the service sector, where personal contact is more frequent and the possibility of working from home is limited. It is well-known that SES is also strongly associated with several diseases, health problems, and health risk behaviors in Sweden and elsewhere (18). Previous studies have also found higher risks of cardiovascular risk factors and diseases, high blood pressure, diabetes, smoking, and obesity in foreign-born persons in Sweden, especially among Middle Eastern migrants (19–23). Such health risks could relate to migrants’ lower SES (24), and adjustment for SES could hence account for both risk factors inherent in low-status occupations with more personal contact and underlying comorbidity, explaining the higher COVID-19 mortality in the foreign-born.
When models additionally adjusted for the number of working-age people in the household and population density, excess COVID-19 mortality risks were additionally reduced across migrant groups. Overall, these findings suggest that migrants’ living and social conditions could make social distancing more difficult, which could lead to a higher risk of virus transmission. Accordingly, previous Swedish studies have found that foreign-born persons are overrepresented in crowded housing conditions (25), which are more prevalent in neighborhoods with high population density. Having family members of working age in the household could especially increase the risk of virus transmission in migrants, since they are more likely to be employed in low-paid essential occupations within the health-care sector or the service sector, which makes working from home and social distancing much more difficult. People who continue to work and commute to work during a pandemic could increase the risk of virus transmission to other household members. A higher proportion of foreign-born persons live in multigenerational households, which could increase the risk of virus transmission to elderly family members belonging to higher-risk groups (25). Finally, living in a specialized-care institution has a strong overall association with COVID-19 mortality. Findings suggest that Sweden has experienced high contagion rates in elderly-care facilities during the pandemic (26). However, according to our findings, living in institutionalized care does not account for migrants’ excess risk of COVID-19 mortality. Interestingly, our most important mediating variables accounted only for increased risk of COVID-19–related mortality by country of birth and not all-cause mortality disparities excluding COVID-19 deaths, which suggests that these could be considered determinants of virus transmission and not overall mortality in migrants. Along the same lines, we found a more pronounced spatial clustering effect for COVID-19 deaths than for overall mortality.
Ultimately, our findings confirm the existence of social patterning of disease (27). The results align with the “fundamental cause of disease” theory of Phelan et al. (28)—that is, that country of birth/ethnicity is a fundamental cause of disease, in this case COVID-19 infection. Similarly to most diseases and health problems (27), the increased risk of COVID-19 mortality in foreign-born persons reflects the fact that those who are in a worse position with regard to important social and economic resources will be more afflicted by COVID-19. Although the profile and risk factors of COVID-19 vary from those of other infectious diseases, vulnerable social groups in society suffer a higher risk of COVID-19, since they have fewer social and economic resources to avoid infection.
Strengths and limitations
Some limitations of this study should be noted. The remaining excess risk of COVID-19 mortality found in foreign-born persons could indicate a higher fatality rate in the foreign-born due to a higher prevalence of underlying adverse health conditions and risk factors, found in the previous literature (20–24). Although SES could be considered a proxy for some of these risk factors, we could not directly study underlying risk factors for COVID-19 and how they vary across migrant groups in our registry data. It would be desirable to link data from hospital discharge registers to our data in order to investigate comorbidity as an explanatory factor for migrants’ excess risk of death. It is also possible that our indicators of SES did not completely capture individuals’ total socioeconomic resources. For instance, no information on wealth was available in our data. Furthermore, there is a risk of underestimation of the number of COVID-19 deaths in registries, since patients have to receive a COVID-19 diagnosis by a physician before death. COVID-19 diagnoses could be missing in patients with rapid disease progression. Nonetheless, this is probably still a much smaller constraint in our study when compared with many others, because of the high-quality registry data used. Furthermore, information on genetic predisposition and genetic vulnerability, social interaction patterns, language proficiency, adherence to guidelines and information, and cultural and religious attitudes and norms regarding virus transmission could contribute to the understanding of disparities in COVID-19 mortality by country of birth. Unfortunately, such information was not available in our registry data.
There was also an issue of missing data for some of our variables. To assess the effect of missing values, we refitted the models after excluding persons with missing data on educational level, income, and employment. Although the levels of missingness among migrants from the Middle East (7%) and Africa (10%) were moderately low, a considerable number of migrants in both of these groups both had died from COVID-19 and did not have a recorded educational level. As such, exclusion of these persons changed the estimates such that excess mortality from COVID-19 could no longer be observed among migrants in these groups. It was our opinion that excluding them would bias the results more than including them in a separate “missing data” category. This was especially true in the baseline model, in which we calculated the unadjusted risk of death from COVID-19. Excluding cases with missing data on income, employment, and housing type did not change the results significantly.
Conclusions
In this total population study, we found large disparities in COVID-19 mortality by country of birth in Stockholm—the worst-affected area in Sweden and one of the most affected regions in the world. Migrants’ disadvantaged socioeconomic and living conditions explained a considerable share of their higher COVID-19 mortality risk. Policies aiming to reduce disparities in COVID-19 mortality by ethnicity/country of birth should consider such conditions when designing health interventions. However, it is crucial to continue to study risk factors explaining migrants’ higher prevalence of COVID-19 deaths in order to prevent such disparities in both Sweden and other countries with substantial migrant populations.
ACKNOWLEDGMENTS
Author affiliations: Department of Public Health Sciences, Faculty of Social Sciences, Stockholm University, Stockholm, Sweden (Mikael Rostila, Agneta Cederström); Centre for Health Equity Studies, Stockholm University/Karolinska Institutet, Stockholm, Sweden (Mikael Rostila, Agneta Cederström); Stockholm University Demography Unit, Department of Sociology, Faculty of Social Sciences, Stockholm University, Stockholm, Sweden (Maria Brandén, Matthew Wallace Gunnar Andersson); Institute for Analytical Sociology, Linköping University, Norrköping, Sweden (Maria Brandén); and Department of Human Geography, Faculty of Social Sciences, Stockholm University, Stockholm, Sweden (Bo Malmberg).
This work was funded by the Swedish Research Council for Health, Working Life and Welfare (grants 2016-07128, 2016-07115, 2016-07105, and 2019-00603).
We thank Dr. Thomas Niedomysl for facilitating and enabling this study.
Conflict of interest: none declared.
REFERENCES
The Swedish Governments Official Investigations.