-
PDF
- Split View
-
Views
-
Cite
Cite
Sadri O. Sozer, Francisco J. Agullo, Humberto Palladino, Autologous Augmentation Gluteoplasty With a Dermal Fat Flap, Aesthetic Surgery Journal, Volume 28, Issue 1, January 2008, Pages 70–76, https://doi.org/10.1016/j.asj.2007.10.003
Close - Share Icon Share
Abstract
Background: Buttock contouring represents a surgical challenge, particularly when both ptosis and volume deficit are present. Isolated buttock lifts may cause a flattened buttock contour, whereas augmentation with implants or fat injections alone my not correct the ptosis.
Objective: We describe a buttock lift with a dermal fat flap that provides correction of the buttock contour in such cases.
Methods: A retrospective review was conducted of 10 patients, aged 26 to 57 years, who underwent a buttock lift with autologous dermal flap augmentation. Patients were followed up between 6 months and 2 years.
Results: A comparison of preoperative and postoperative photographs indicated improved buttock contour and maximum augmentation at the midlevel of the buttocks. There were no major or minor complications. Patient satisfaction was high.
Conclusions: Autologous dermal flap gluteal augmentation is a versatile technique that addresses both buttock ptosis and volume deficit. Drawbacks include an extended incision line that, however, is easily concealed by underwear or a bikini.
Developments in surgical techniques over the past century now allow safe and efficient surgical correction of contour deformities.1 The trunk, buttocks, and thighs represent areas of increased patient interest and surgical technique modification. In particular, there has recently been an increase in patients seeking buttocks augmentation and contour restoration. However, buttock implants have been associated with various rates of complications and difficulties, which has limited their wide acceptance by surgeons and patients.2–5 Lipografting has been shown to be an effective means of moderately increasing buttocks volume, but this procedure does not directly address ptosis.6–14
As an alternative, the use of a number of adipocutaneous flaps to address gluteal augmentation in different settings has been described in this region.15–21 The ideal flap should be versatile, not vascularly compromised, and give the maximum projection at the midlevel of the buttocks. In 2005, the authors reported a series of 50 turnover dermal fat flaps for buttock augmentation in patients undergoing bariatric and aesthetic surgery with lower body lifts to prevent a flattened buttocks contour.21 Drawing from this experience, a novel method for isolated buttock lift with autoprosthesis augmentation was developed for patients seeking aesthetic augmentation and ptosis correction of the gluteal area.
The use of local adipocutaneous flaps to provide coverage for the lumbosacral defects is a common plastic surgery procedure.19–22 These principles were used to create an autologous buttock implant to provide additional projection. A seagull incision is made from the sacrum to the lateral buttocks bilaterally. Excess tissue is marked for excision to achieve a buttock lift. A perforator-based dermal fat flap originating within the regularly excised supragluteal tissue is rotated caudally to function as an autologous buttock implant.
Materials and Methods
A retrospective study was undertaken of patients who were treated for buttock contour deformities from January 2004 to December 2006. Of these, 74 patients underwent a buttock lift with autologous dermal fat flap augmentation, but 64 of these were part of a circumferential body lift, and 10 were isolated buttock lift and augmentation. Criteria for selecting patients for this procedure included any grade of buttock ptosis accompanied by decreased buttock projection and volume. Only patients willing to accept the scar were included.
Additional cosmetic procedures were performed at the same time in 50% of the patients. All of the procedures were performed at a certified outpatient surgery center with 23-hour postoperative observation. All surgeries were performed by the senior author. Patients were followed up for a period between 6 months and 2 years.
Each patient's medical record was reviewed, focusing on physical and mental health, expectations, and indications for the procedure. The details of the operation were explained and the patients were shown before and after pictures to ensure they clearly understood the magnitude of the procedure and the location of the scars. Lateral and posterior preoperative and postoperative photographs were compared. Patient and surgeon satisfaction were recorded and compared, as were the operative time, total resection weight, blood loss, and complications.
Endpoints considered for a successful procedure included maximum gluteal projection at the midlevel of the buttocks, verified by a horizontal line from the point of maximal projection of the mons pubis. Ptosis correction was verified by elevation of the gluteal mass and the correction of the infragluteal fold to a shorter line with a downward slope.23 Other indications of aesthetically pleasing buttocks included a V-shaped crease in the proximal portion of the gluteal crease and lumbar hyperlordosis.24,25
Preoperative Markings
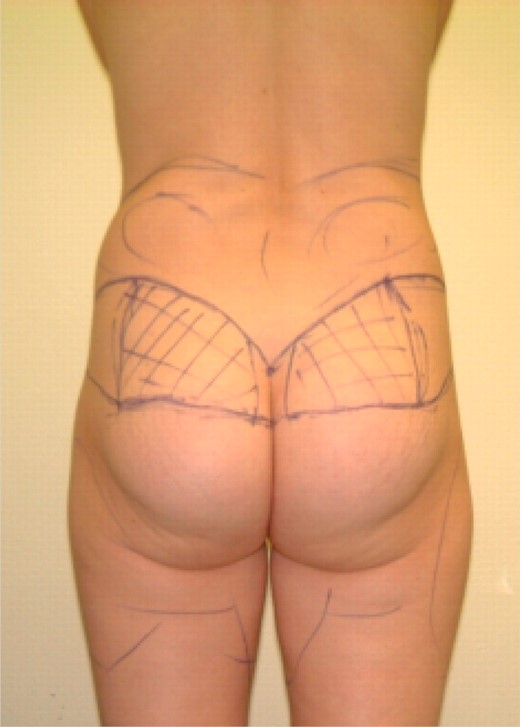
Preoperative markings are a crucial component to successful surgery and to achieving desired results. Patients are marked before surgery in prone and standing positions. The symmetry of the incisions was evaluated while the patient was standing (Figure 1).
The superior or cephalic line was marked first. By the end of the procedure, this line would be lowered by 1 or 2 cm and would dictate the localization of the final scar. The line was drawn starting above the intergluteal crease extending in a curvilinear fashion a few centimeters below the iliac crest. At the sacrum, the line from the contralateral side was joined forming a V, creating an aesthetically pleasing V-shaped crease.24,25 This would form a scar that is slightly arched, follows the skin's tension lines, and is easily concealed by underwear. The inferior line was designed by use of the pinching method to estimate the amount of possible skin resection. The direction of elevation of the ptotic buttocks was caudal and slightly medial.
A dermal fat flap originating between the superior and inferior lines was marked within the medial two thirds of the supragluteal tissue marked for excision. The flap was demarcated medially 2 to 3 cm lateral from the midline. The lateral demarcation of the flap was approximately three quarters of the distance from the midline to the posterior axillary line. The size of the flap was individualized according to each patient's buttock contour and desired result.
The gluteal flap was based randomly on superior gluteal artery perforators. The same random circulation has been used for V to Y advancement flaps in the area for decubital ulcers. Perfusion to the skin overlying the gluteal region was supplied by 20 to 25 perforating branches of the superior and inferior gluteal arteries, both of which branch from the internal iliac artery.22,23,26–28 The abundant vascular supply of the gluteal region provided robust perfusion to surrounding tissue flaps.29
Depending on the patient's contour deformities, the areas of lipoplasty were marked. Lipoplasty was routinely performed in the flanks, sacrum, and posterior thigh, following the aesthetic units of the buttocks and accentuating its final contour.
Surgical Technique
The patient was placed in the prone position under general anesthesia with the lower extremities abducted on arm boards. Lipoplasty was performed in the flanks, sacral area, below the infragluteal crease, and other areas dictated by the patient's contour deformities. The subcutaneous tissue was infiltrated with tumescent solution consisting of Hartmann solution 1 L with 1 mg of epinephrine and 1% lidocaine 10 mL. Deep and superficial lipoplasty of the areas marked with fat deposits was performed following the traditional method.
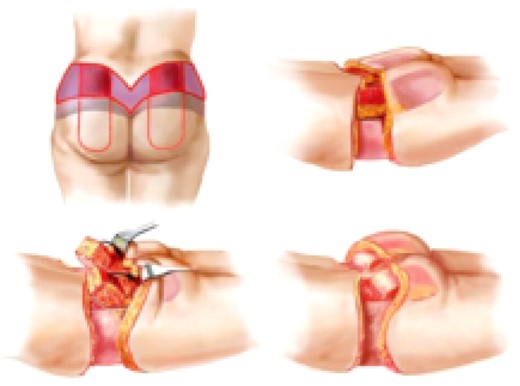
The marked wedge of supragluteal skin was resected down to the fascia, and the gluteal flap was deepithelialized (Figure 2). The flap was dissected down to the fascia at a perpendicular angle superiorly, medially, and laterally. The inferior border of the flap was dissected inferiorly in an oblique angle to the level of the fascia. A pocket was created for insertion of the flap by undermining the buttock in the plane above the fascia and extending it a sufficient length to approach the inferior gluteal crease. The fascia in the superior border of the dermal fat flap was divided and undermined inferiorly, until the flap could be rotated caudally 180 degrees. The inferior superficial tip of the flap was cut to assess for adequate blood flow. The flap was rotated caudally 180 degrees into the pocket and anchored to the fascia with polyglactin 910 (3/0 Vicryl) suture (Ethicon, New Brunswick, NJ). Securing the deepithelialized surface upside down gave the flap a more rounded and implant-like shape. The remaining buttock skin was pulled in the reverse direction to cover the flap and two drains were placed. The superficial fascial system was repaired with polyglactin 910 (0 Vicryl), and the tissues were closed in a layered fashion.
Creation of an autologous buttock augmentation flap. Tissue to be excised is in purple, and the deepithelialized flaps are in red. The flap is dissected down to the fascia perpendicularly in the superior, medial, and lateral edge, and at an oblique angle, inferiorly undermining it. Fascia is undermined superiorly until the flap can be rotated caudally 180 degrees into the pocket and anchored to the fascia with suture. The remaining buttock skin is pulled to cover the flap.
The patient was then placed in the supine position and redraped and prepped. After dog-ears were resected, the superficial fascial system was repaired with polyglactin 910 (0 Vicryl), and the tissues were closed in a layered fashion. The superior and inferior edges were approximated in a layer closure with subdermic running absorbable polyglactin 910 (3/0 Vicryl) and subcutaneous running absorbable poliglecaprone 25 (4/0 Monocryl).
Results
Ten female patients, aged 26 to 57 years, underwent the procedure. The body mass index ranged from 21.0 to 29.2 kg/m2 (mean 24.6 kg/m2). The mean operative time was 150 minutes (range, 120 to 160 minutes). The total resection weight ranged from 1.9 to 2.5 kg (mean 2.2 kg), with an average volume of fat obtained by lipoplasty of 750 mL. Mean operative blood loss was 95 mL (range 80 to 110 mL), and none of the patients required transfusions. No cases of major or minor complications were reported. Necrosis of the buttock dermal fat flap was not encountered.
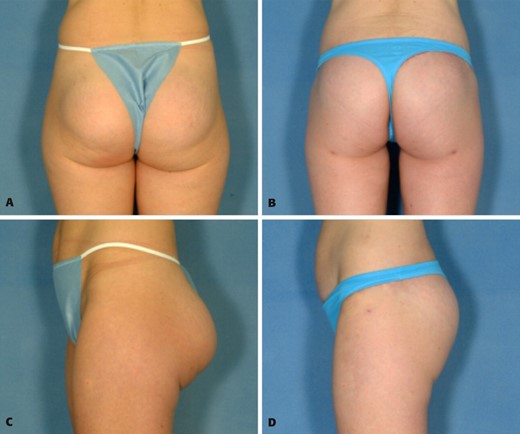
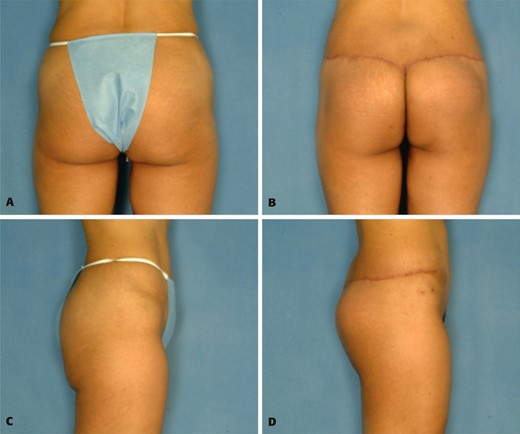
Comparing preoperative and postoperative pictures (Figures 3 to 6), all of the cases resulted in significant improved contour and firmness of the skin in the buttocks. The infragluteal fold became less evident, the buttock mass was elevated, and augmentation was achieved with the maximum projection at midlevel of the gluteus. Lipoplasty aided in the accentuation of lumbar lordosis, which gives the impression of greater buttocks projection. A V-shaped proximal gluteal crease was accentuated by the procedure. Both patient and surgeon satisfaction were recorded as good to excellent in each case, and in most cases, the results exceeded patients' expectations, per postoperative interviews. The scars were considered acceptable with respect to the procedure and easily hidden by a bikini bathing suit. One-year follow-up demonstrated stability in the body contour repair.
A, C, Preoperative views of a 32-year-old woman with prior buttock augmentation with round 270-cc silicone gel–filled implants that resulted in ptosis and double bubble appearance. B, D, Postoperative views 6 months after removal of implants and performance of a buttock lift with autoprosthesis augmentation.
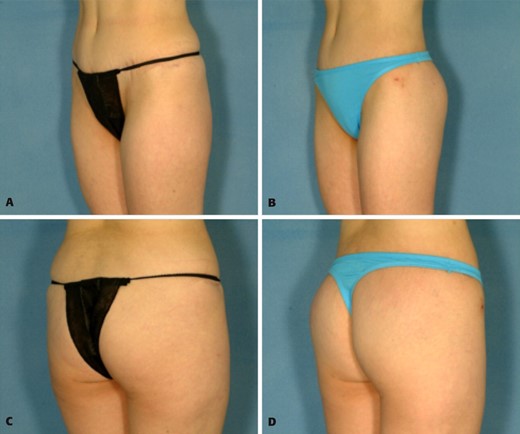
A, C, Preoperative view of a thin 45-year-old woman who was unhappy with the sagging and lack of projection of her buttocks. Postoperative views 6 months after autoprosthesis buttock lift and augmentation demonstrate shortening of elongated buttock and increased projection. The infragluteal crease is considerably shorter, and there is additional improvement of the waistline.
A, C, Preoperative views of a 42-year-old patient who desired correction of buttock contour and augmentation. B, D, Postoperative views 6 months after augmentation.
A, C, Preoperative views of a 40-year-old woman who desired improvement of the buttocks and waist and lateral thigh contour. B, D, Postoperative views 6 months after buttocks lift with autoprosthesis augmentation and lateral thigh lift.
One of the cases involved a patient who had prior buttock augmentation with 270-cc cohesive round silicone implants (Figure 3). The patient was unhappy with her subsequent buttock ptosis and “double bubble” appearance. Removal of the prosthesis, with immediate buttock lift and augmentation with the dermal fat flap described was performed, resulting in correction of the deformity and a pleasing buttock contour.
Discussion
Body contouring continues to increase in popularity, and the alternatives and procedures to address the deformities are numerous. The trunk, buttocks, and thighs represent areas of increased patient interest and surgical technique modification. Consequently, familiarity with the presentation and effective treatment of these patients is becoming increasingly important.28–30 Recently, there has been an increase in patients seeking buttock augmentation and contour restoration.
The buttock lift described is based on modifications of prior experiences of several surgeons.1,15,17,19,31–42 With the evolution of this procedure, it is possible to achieve lifting of the buttock and lateral thigh, reduction in the number and size of adipose cutaneous folds of the lower and middle back, improvement in the waist silhouette, and elimination of redundant flank tissue. The result is an improved body contour and tightening of the skin.
To increase projection in the buttocks contour, other local flaps have been described.15–21 In our experience and judgment, these flaps have limited mobility and produce augmentation above the midlevel of the buttocks or give additional bulk to the sacral area.
The flap described allows the surgeon to improve the buttocks contour without extending the procedure significantly (<30 minutes) or increasing morbidity. The flap has good mobility, is well vascularized by the numerous gluteal perforators in the region, and results in a natural reshaping of the gluteal area. The procedure results in increased projection of the buttocks at the midlevel demarcated by a horizontal line from the mons pubis, a shortened infragluteal fold with a downward slope, a V-shaped proximal gluteal crease, and lumbar hyperlordosis. The scars remain within the anatomic subunits of the lower trunk and buttocks and thus remain hidden with most undergarments and bathing suits.
Conclusion
The high satisfaction rate, the ease of concealing the incision with clothing, and the low complication rate suggest that this is a reliable, versatile technique. The creation of an autologous buttock implant from a dermal fat flap provides additional projection during the buttock lift. The flap has reliable circulation, requires minimal additional operating time, does not increase operative morbidity rates, and can be custom designed for each patient. The procedure allows for a more substantial augmentation when compared with fat grafting, and in our experience is safer than implants, while allowing for a lift at the same time. It has proven to be a reliable procedure for correcting unsatisfactory outcomes with implants. Drawbacks include an extended incision line that is easily concealed by underwear or bikini.
Disclosures
The authors have no financial interest in and receive no compensation from manufacturers of products mentioned in this article.
References
1
2
3
4
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42