-
PDF
- Split View
-
Views
-
Cite
Cite
Mehmet Bayramiçli, Hakan Şirinoğlu, Doğuş Yalçın, Outcome After Breast Reduction Considering Body Mass Index and Resection Amount, Aesthetic Surgery Journal, Volume 37, Issue 10, November-December 2017, Pages 1103–1110, https://doi.org/10.1093/asj/sjx110
Close - Share Icon Share
Abstract
It is presumed that breast reduction improves patients’ quality of life and promotes weight loss. Preoperative body mass index (BMI) and the amount of breast tissue (breast reduction amount [BRA]) in proportion to the patient’s body weight are important variables to affect the breast reduction outcome.
This study was designed to evaluate the short and long-term effects of breast reduction from the perspective of BMI and BRA.
One hundred fifty-seven consecutive patients were invited to participate in the study. All clinical information was recorded on a breast surgery form. Patients completed a standardized questionnaire preoperatively, at postoperative year 1, and after postoperative year 5. Patients were grouped according to their BMI as “normal weight” and “overweight” and according to BRA as “minor/moderate reductions” and “major reductions.” The differences in the BMI values and the life scores were compared between the BMI and BRA groups.
Sixty-four patients were included in the study. Postoperative year 1 BMIs were significantly lower than both the preoperative BMIs and postoperative year 5+ BMIs. The year 1 BMI decrease in the major reduction group was higher than the decrease in the minor/moderate reduction group. The postoperative life scores of all subgroups were better than the preoperative life scores.
Reduction mammaplasty has a significant effect on short-term weight loss and the improvement in lifestyle. Patients tend to return to their original body weight in the long term. BRA is a significant variable in short-term weight loss, but neither BMI nor BRA has any other significant effect on the outcome in any time section.

Women with large breasts often display signs of decreased physical activity, poor general health, and a diminished self-esteem. Breast reduction has been shown to improve patients’ quality of life and their ability to exercise and promote weight loss.1-12 A significant increase in self-confidence and self-esteem was observed in many patients in comparison to the preoperative period.13,14 Symptomatic relief due to volume resections—regardless of the patients’ preoperative weight—has been indicated as the main reason for this improvement, and all of these beneficial effects have been demonstrated in relatively short-term studies.1,3,8,15,16 However, it is not clear whether these improvements will be maintained in the long-term or whether the motivating force of reduction mammaplasty to acquire a new healthy lifestyle will be a short-lived stimulus.
The outcome of breast reduction may be affected by several variables. The preoperative body mass index (BMI) indicating the degree of a patient’s obesity (total body fat) and the amount of breast tissue resection (breast reduction amount [BRA]) in proportion to the patient’s body weight may be significant factors to be considered in the follow-up.17,18
In this study, we tried to answer the following questions: (1) Does breast reduction have any effect on patients’ total body weight because of restored breast/body proportion? (2) Does breast reduction have any effect on patients’ lifestyle? (3) Are these effects long-lasting? (4) Is the outcome affected by variables such as BMI and BRA?
METHODS
One hundred fifty-seven consecutive patients who underwent bilateral reduction mammaplasties by the senior surgeon (M.B.) between January 2005 and November 2010 were invited to participate in the study.
Demographic data, preoperative physical examination findings, surgical technique, and preoperative and postoperative photographic documentation were recorded on a breast surgery-specific form. The height and weight of each patient were measured and the preoperative BMI values were calculated. Clinical information also included the history of endocrinologic disease, diabetes, pregnancies, depression, and existence of menopause. All patients filled in a written informed consent form, which was prepared according to the Declaration of Helsinki.
A standardized questionnaire that includes questions about the general features of the patient along with questions scoring the quality of life (“0” being the best, “5” being the worst) and to evaluate the patient satisfaction was prepared by the authors (Appendix A, available as Supplementary Material online at www.aestheticsurgeryjournal.com). Questions of Sexual and Bodily Self-Consciousness (SBSC) of appearance and Negative Self-Concept (NSC) parts of the Derriford Appearance Scale (DAS-59) were used for this issue.19 This questionnaire was applied to all patients preoperatively, at postoperative year 1, and at or after postoperative year 5.
All patients were operated on under general anesthesia and discharged from the hospital the following day. Three different pedicles including superior,20 septum-based lateral,21 and septum-based central pedicles,22 and free-nipple graft techniques, were used according to the needs of the patients. The weight of the resected breast tissue was recorded. The resection weight was correlated to the body weight of the patient in terms of the percentage to obtain an objective parameter of comparison between the patients.23 This parameter was recorded as the BRA.
The follow-up schedule had been arranged at 5 to 7 days, 3 to 8 weeks, 6 months, and 12 months postoperatively unless wound and scar treatment required that the patient have more frequent visits. The long-term follow-up data was collected after 5 years either by outpatient visits, e-mail, or phone.
Patients were excluded from the study if they declined to participate in the study, had secondary breast surgery in the postoperative period, could not be contacted in the long term, or had incomplete medical records and follow-ups.
Patients were grouped by using two basic data: BMI and BRA, which is the proportion (percentage) of the resected breast tissue weight to the body weight of the patient. Patients with preoperative BMI ≤25 were grouped as “normal weight,” whereas the patients with preoperative BMI > 25 were grouped as “overweight” separately for BMI.3 The median was used to separate the patients according to their BRA into two groups. Patients with BRA lower than the median were grouped as having “minor/moderate reductions,” whereas patients with BRA higher than the median were grouped as having “major reductions”.
The primary objective of the statistical analysis was to compare the outcome in two different follow-up sections: at postoperative year 1 and at or after postoperative year 5. The differences in the quality-of-life scores and the BMI values across preoperative, postoperative year 1, and postoperative year 5+ were compared between the BMI and BRA groups.
We utilized the unpaired t-test for differences in means between the study groups, the chi-squared test to assess the significance of differences in proportions, the Mann-Whitney-U test to compare the differences in the scores for the questions between the groups, and the Wilcoxon signed-rank test to identify any significant differences caused by the paired nature of our observations. Binomial distribution and transition probabilities were reported by student’s t distribution. A 5% significance level was used for statistical analysis. The SPSS statistical software package (SPSS software version 22, IBM Corp., New York, NY, USA) was used for the calculations.
RESULTS
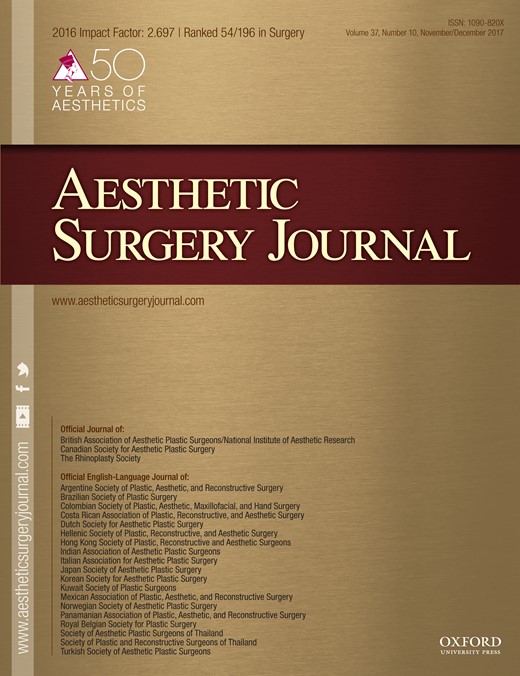
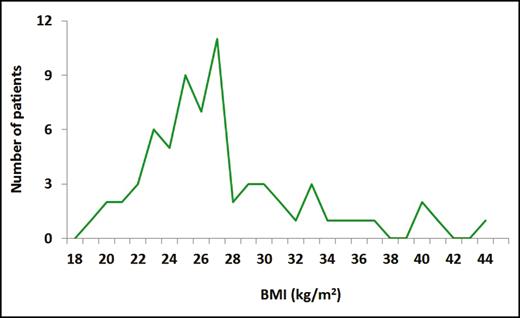
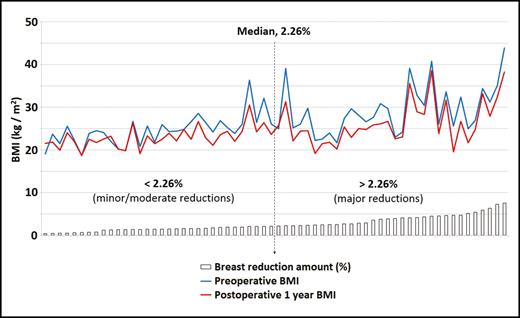
Sixty-four patients who had completed the questionnaire preoperatively, and at follow-up postoperative year 1 and year 5+ were included in the study. The mean age was 45.7 years (range, 23-71 years). The average follow-up time was 71.48 months (range, 58-101 months). The average height of the patients was 161.2 cm (range, 140-172 cm). BMI was in a range of 18.6 to 43.8 kg/m2 (mean, 27.81 kg/m2) (Figure 1). All patients were operated on under general anesthesia. The mean weight of the resected breast tissue was calculated as 2511.8 grams (range, 280-6500 grams). The correlation of resected breast tissue weight to the total body weight varied between 0.425% and 7.558%, with the median being 2.26% (Figure 2). No major complications requiring additional surgical intervention were observed.
Distribution scale of preoperative BMI (kg/m2). The range is 18.6 to 43.8 with a mean value of 27.81.
Distribution scale of breast reduction amount (BRA). The range is 0.425% to 7.558% and the median is 2.26%. The majority of the BRA values were accumulated between 1.4% and 2.8%.
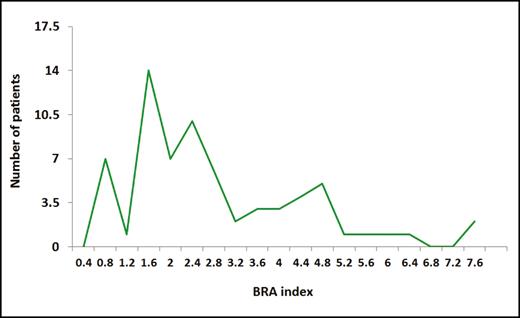
In the preoperative period, 26 of the patients were in menopause, four patients had hypothyroidism, three patients had diabetes, and two patients had hyperthyroidism. At the end of the follow-up period, 35 patients were in menopause, seven patients had diabetes, six patients had hypothyroidism, five patients had pregnancies, five patients had hypertension, four patients had hyperthyroidism, one patient had chronic obstructive lung disease, one patient was treated for breast cancer, and one patient was operated on because of larynx cancer (Figure 3).
Changes in health and endocrinological status of the patients at the end of the postoperative year 5+ follow-up period. COLD, chronic obstructive lung disease.
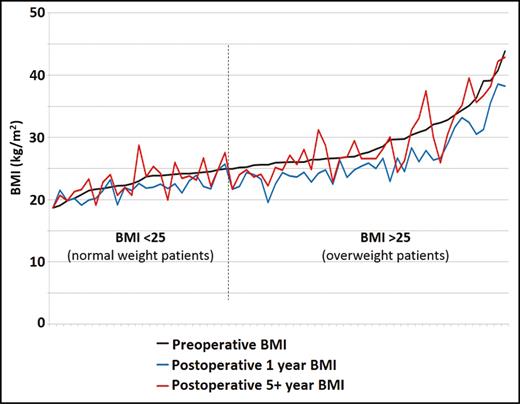
BMI values of “normal weight” patients (n = 26) and “overweight” patients (n = 38) were compared across preoperative, postoperative year 1, and postoperative year 5+ values separately. In both groups, postoperative year 1 BMIs were significantly lower than the preoperative and postoperative year 5+ BMIs (P < 0.0001). There was no significant difference between the preoperative BMIs and the postoperative year 5+ BMIs in both groups (P > 0.05). The results of the BMI measurements are shown in Figure 4.
BMI changes in three time sections. A significant BMI reduction is obvious at postoperative year 1 (blue line). The same reduction is not observed in the postoperative 5+ year BMI (red line) when compared with the preoperative BMI (black line). The vertical reference line (dotted) represents the threshold for BMI subgroups: left side < 25 (normal weight patients); right side > 25 (overweight patients). There is no significant difference between the BMI subgroups.
The BMI differences are also compared according to BRA parameters. BMI scores decreased in both BRA groups at postoperative year 1. The decrease in the BRA > 2.26 group is 19%, whereas it is 9% in the BRA < 2.26 group. The difference is statically significant (P = 0.018) (Figure 5). However, there are no other statistically significant BMI differences between the BRA groups.
Postoperative year 1 BMI reduction according to BRA. The vertical dotted line represents the median value (2.26%) for the division of BRA subgroups. The decrease in BMI in postoperative year 1 is significantly greater in the major reduction group (P < 0.05).
The numeric results of the DAS-59 questionnaire were calculated along with the percentage of change (Table 1). The differences in the quality-of-life scores were compared according to the patients’ preoperative BMI and BRA separately. Both the postoperative year 1 (average: 1.78) and the postoperative year 5+ (average: 1.91) scores for all 64 patients were significantly better than the preoperative life score average (3.84) (P < 0.0001). Such significance is also observed for both BMI and both BRA groups (all P-values are P < 0.0001). There is no significant difference between the scores of the BMI and BRA subgroups for postoperative year 1 and postoperative year 5+ (P > 0.05).
Mean Preoperative, Postoperative Year 1, and Postoperative Year 5+ Scores Along with the Percentage Changes Obtained, According to DAS-59
| . | Mean preoperative score . | Mean postoperative year 1 score . | Mean postoperative year 5+ follow-up score . | Percentage change (%) between the preoperative period and postoperative year 1 . | Percentage change (%) between the preoperative period and postoperative year 5+ . |
|---|---|---|---|---|---|
| SBSC Questions | |||||
| Q-4: Avoiding undressing in front of partner | 3.84 | 1.78 | 1.91 | -54 | -50 |
| Q-9: Avoiding communal changing rooms | 4.20 | 1.48 | 1.59 | -64 | -62 |
| Q-23: Adverse effect on sex life | 3.81 | 1.94 | 1.94 | -49 | -49 |
| Q-24: Adverse effect on marriage | 3.81 | 1.91 | 2.00 | -50 | -48 |
| Q-37: Distress when going to the beach | 4.78 | 1.00 | 1.13 | -79 | -76 |
| Q-43: Distress from being unable to wear favorite clothes | 4.91 | 0.92 | 1.02 | -81 | -79 |
| Q-46: Distress from being unable to play games | 4.47 | 1.22 | 1.22 | -73 | -73 |
| Q-49: Distress from being unable to look in the mirror | 4.83 | 1.02 | 1.13 | -79 | -77 |
| NSC Questions | |||||
| Q-52: How confident do you feel? | 4.56 | 1.22 | 1.22 | -73 | -73 |
| Q-54: How secure do you feel? | 4.33 | 1.31 | 1.39 | -70 | -68 |
| Q-55: How cheerful do you feel? | 4.45 | 1.09 | 1.16 | -76 | -74 |
| Q-56: How normal do you feel? | 4.80 | 0.91 | 1.02 | -81 | -79 |
| Q-57: How feminine do you feel? | 4.64 | 1.03 | 1,16 | -78 | -75 |
| . | Mean preoperative score . | Mean postoperative year 1 score . | Mean postoperative year 5+ follow-up score . | Percentage change (%) between the preoperative period and postoperative year 1 . | Percentage change (%) between the preoperative period and postoperative year 5+ . |
|---|---|---|---|---|---|
| SBSC Questions | |||||
| Q-4: Avoiding undressing in front of partner | 3.84 | 1.78 | 1.91 | -54 | -50 |
| Q-9: Avoiding communal changing rooms | 4.20 | 1.48 | 1.59 | -64 | -62 |
| Q-23: Adverse effect on sex life | 3.81 | 1.94 | 1.94 | -49 | -49 |
| Q-24: Adverse effect on marriage | 3.81 | 1.91 | 2.00 | -50 | -48 |
| Q-37: Distress when going to the beach | 4.78 | 1.00 | 1.13 | -79 | -76 |
| Q-43: Distress from being unable to wear favorite clothes | 4.91 | 0.92 | 1.02 | -81 | -79 |
| Q-46: Distress from being unable to play games | 4.47 | 1.22 | 1.22 | -73 | -73 |
| Q-49: Distress from being unable to look in the mirror | 4.83 | 1.02 | 1.13 | -79 | -77 |
| NSC Questions | |||||
| Q-52: How confident do you feel? | 4.56 | 1.22 | 1.22 | -73 | -73 |
| Q-54: How secure do you feel? | 4.33 | 1.31 | 1.39 | -70 | -68 |
| Q-55: How cheerful do you feel? | 4.45 | 1.09 | 1.16 | -76 | -74 |
| Q-56: How normal do you feel? | 4.80 | 0.91 | 1.02 | -81 | -79 |
| Q-57: How feminine do you feel? | 4.64 | 1.03 | 1,16 | -78 | -75 |
Mean Preoperative, Postoperative Year 1, and Postoperative Year 5+ Scores Along with the Percentage Changes Obtained, According to DAS-59
| . | Mean preoperative score . | Mean postoperative year 1 score . | Mean postoperative year 5+ follow-up score . | Percentage change (%) between the preoperative period and postoperative year 1 . | Percentage change (%) between the preoperative period and postoperative year 5+ . |
|---|---|---|---|---|---|
| SBSC Questions | |||||
| Q-4: Avoiding undressing in front of partner | 3.84 | 1.78 | 1.91 | -54 | -50 |
| Q-9: Avoiding communal changing rooms | 4.20 | 1.48 | 1.59 | -64 | -62 |
| Q-23: Adverse effect on sex life | 3.81 | 1.94 | 1.94 | -49 | -49 |
| Q-24: Adverse effect on marriage | 3.81 | 1.91 | 2.00 | -50 | -48 |
| Q-37: Distress when going to the beach | 4.78 | 1.00 | 1.13 | -79 | -76 |
| Q-43: Distress from being unable to wear favorite clothes | 4.91 | 0.92 | 1.02 | -81 | -79 |
| Q-46: Distress from being unable to play games | 4.47 | 1.22 | 1.22 | -73 | -73 |
| Q-49: Distress from being unable to look in the mirror | 4.83 | 1.02 | 1.13 | -79 | -77 |
| NSC Questions | |||||
| Q-52: How confident do you feel? | 4.56 | 1.22 | 1.22 | -73 | -73 |
| Q-54: How secure do you feel? | 4.33 | 1.31 | 1.39 | -70 | -68 |
| Q-55: How cheerful do you feel? | 4.45 | 1.09 | 1.16 | -76 | -74 |
| Q-56: How normal do you feel? | 4.80 | 0.91 | 1.02 | -81 | -79 |
| Q-57: How feminine do you feel? | 4.64 | 1.03 | 1,16 | -78 | -75 |
| . | Mean preoperative score . | Mean postoperative year 1 score . | Mean postoperative year 5+ follow-up score . | Percentage change (%) between the preoperative period and postoperative year 1 . | Percentage change (%) between the preoperative period and postoperative year 5+ . |
|---|---|---|---|---|---|
| SBSC Questions | |||||
| Q-4: Avoiding undressing in front of partner | 3.84 | 1.78 | 1.91 | -54 | -50 |
| Q-9: Avoiding communal changing rooms | 4.20 | 1.48 | 1.59 | -64 | -62 |
| Q-23: Adverse effect on sex life | 3.81 | 1.94 | 1.94 | -49 | -49 |
| Q-24: Adverse effect on marriage | 3.81 | 1.91 | 2.00 | -50 | -48 |
| Q-37: Distress when going to the beach | 4.78 | 1.00 | 1.13 | -79 | -76 |
| Q-43: Distress from being unable to wear favorite clothes | 4.91 | 0.92 | 1.02 | -81 | -79 |
| Q-46: Distress from being unable to play games | 4.47 | 1.22 | 1.22 | -73 | -73 |
| Q-49: Distress from being unable to look in the mirror | 4.83 | 1.02 | 1.13 | -79 | -77 |
| NSC Questions | |||||
| Q-52: How confident do you feel? | 4.56 | 1.22 | 1.22 | -73 | -73 |
| Q-54: How secure do you feel? | 4.33 | 1.31 | 1.39 | -70 | -68 |
| Q-55: How cheerful do you feel? | 4.45 | 1.09 | 1.16 | -76 | -74 |
| Q-56: How normal do you feel? | 4.80 | 0.91 | 1.02 | -81 | -79 |
| Q-57: How feminine do you feel? | 4.64 | 1.03 | 1,16 | -78 | -75 |
There is considerable improvement in the scores of social life in both time sections (namely, distress when going to the beach, distress from being unable to wear favorite clothes, distress from being unable to look in the mirror and how normal do you feel?) for both the BMI and BRA groups. However, no significant difference between the preoperative and postoperative (both year 1 and year 5+) scores of the questions about the intimate life (namely, avoiding undressing in front of partner, adverse effect on sex life, adverse effect on marriage) in either variable was noted. The most significant improvements were in the scores of “distress of going to the beach and being unable to wear favorite clothes” for normal-weight patients (BMI < 25) and “distress from being unable to play games” for gross-reduction patients (BRA > 2.26).
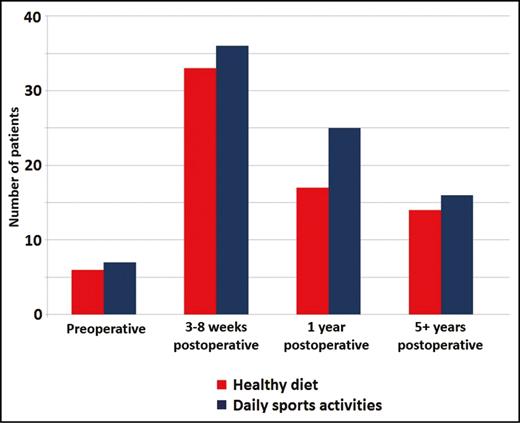
There is significant improvement in starting and maintaining postoperative sports activities and dieting in all patient groups in the short term when compared with their preoperative habits. Six patients out of 64 (9, 3%) were on a healthy diet before the operation. This number increased to 33 (51, 5%) in the early postoperative follow-up period (3-8 weeks), and 17 of them resumed the healthy diet until the end of postoperative year 1 (26, 5%) (P < 0.01). However, only 14 patients (21, 8%) could keep their healthy eating habit to the end of the follow-up period (P > 0.05). Seven patients were in physical activity programs including walking, pilates, and gym activities in the preoperative term (10.9%). This number increased to 36 (56, 2%) in the early postoperative visit (3-8 weeks). Twenty-five of these patients (39, 1%) continued their sportive activities for one year, which is significantly higher than the preoperative rate (P < 0.05). Only 16 of these patients (25%) were still performing daily sports activities after 5+ years (P > 0.05) (Figure 6). There is no significant difference between any of the subgroups in terms of improvement in postoperative sports and dieting (P > 0.05).
There is significant improvement in starting and maintaining sports activities and dieting in the postoperative period. Significant improvement was observed in postoperative year 1; however, the improvement was not maintained in the long term (postoperative year 5+).
DISCUSSION
The main purpose of the breast reduction operation is to restore the compatibility of breast/body proportion through breast tissue resection. Two variables, the preoperative BMI and the breast size, are important in this context, because the physical relief of reducing the breast weight has been reported to be the main stimulus.2,4 This study was designed to evaluate the short- and long-term effects of breast reduction from the perspective of preoperative BMI and the amount of resected breast tissue.
All patients, regardless of their preoperative BMI and BRA, have significant weight loss in postoperative year 1. Previously, significant weight loss after breast reduction was reported in an overweight patient group,12 and in another study, weight loss after the operation was directly associated with the patient’s motivation.11 In the latter study, the patients who perceived breast reduction as a motivation had demonstrated significant weight loss, whereas the others who did not have the same motivation did not lose weight, but rather gained weight postoperatively. However, postoperative weight loss emerged as a common outcome in our study in the postoperative year 1 follow-up of all patient groups. Moreover, major reduction patients lost significantly more weight than the minor/moderate reduction patients in postoperative year 1. Although the reduction amount had not been correlated to the degree of relief in many physical symptoms after reduction mammaplasty,3,15,16,24,25 it appears to be a significant variable in the short-term weight loss.
Another interesting finding of our study is the tendency of all patients to gain their original body weights in the long term (5+ years) regardless of their preoperative BMI or BRA. This outcome may have similarities with the reports in obese patient groups who continued to have limited activity and did not lose significant amounts of weight after a long postoperative follow-up period.26,27 However, the normal weight group patients also have the same weight regain trend in our study, which may be related to the lifestyle change.
A change in lifestyle after reduction mammaplasty has a serious impact on a patient’s physical fitness. Several studies have reported a significant improvement in the lifestyle of the patients in terms of physical activity and the amount of time devoted to exercise.3,28-30 Similarly, in the short term, a significant number of patients in our study groups tried to change their lifestyle by increasing physical activity and changing their eating habits. However, this motivation appears to be insufficient in the long term, when weight regain may be attributable to the inability to maintain healthy eating and exercise behaviors.31 At this point, menopause and aging should also be mentioned as an important contributing factor of weight regain.32,33 A possible weakness of our study is the high number of menopause patients, which might interfere with the regain of weight in the long term. It needs to be clarified in further studies conducted on a younger patient group to reduce the possible effect of menopause and hormonal changes.
All life scores were found to be better after reduction mammaplasty in both postoperative years 1 and 5+ follow-up regardless of the preoperative BMI and BRA. This significant improvement of body image satisfaction is consistent with the results of previous studies.2,5,10,34-37 Neither BMI nor BRA has any significant effect on patient satisfaction in terms of life scores. The operation proved to have positive effect on the social life of the patients in all groups. However, in contrast to previous studies, we cannot find any improvement in the scores of intimate life,38,39 which might be a reflection of cultural differences.
Numerous studies investigated the beneficial effects of reduction mammaplasty on the relief of physical symptoms, the improvement of life quality and self-esteem, the increase in physical activity, a healthier eating behavior and weight loss, etc.2,4 Several reports focused on patient BMI and the resection amount of breast tissue as the critical variables that might interfere with the outcome. However, the main discussion point of these reports was the insurance company restrictions, and these variables were generally investigated regarding their effects on the health benefits of the patients.1,3,12,15,16,40,41 Our patient population has a normal distribution pattern without any restrictions of age, BMI, and resection amount; also in addition, surgeon dependent bias is minimal.42,43 The long-term outcome studies considering the BMI and the amount of breast resection are focused on the patient satisfaction analysis through retrospective answers to the questionnaire. A retrospective comparison of the preoperative and postoperative issues at the end of the follow-up period is controversial due to its highly subjective nature.28,29,44 In the present study, the prepared questionnaires were filled out, and its scores were evaluated at that time. The statistical comparisons were made at the end of the study to prevent any kind of bias.
The resection amount in breast reduction is also an important variable to be considered. Several studies took this variable into account when dealing with the outcome analysis. However, the criterion in these studies was the direct weight of the resection specimen in grams without considering the patients’ body morphology. The weight of the resected breast tissue cannot be an independent variable without correlating it to the individual patient’s body composition.23 Two patients with the same BMI may have distinct body sizes. A breast resection amount of, eg, 1000 grams cannot be considered the same burden for small and large-sized patients. Therefore, our BRA value—the proportion of the resected breast tissue weight to the body weight of the patient—provide reliable data and convincing evidence for analysis.
The present study differs from the other studies because of our concrete finding that the positive impact of the breast reduction surgery is observed in a limited time period, notably in the postoperative year 1. Both the surgeon and the patient should be aware that the motivation of surgery, which is the main reason for a healthy diet, increased daily sportive activities, that weight loss may be transient, and that the majority of patients tend to return to their preoperative life habits and body weight in the long term.
Our results were obtained from 64 patients, which is approximately 40% of the original patient population. Although it is quite an acceptable sample size for the evaluation of the long-term outcome after breast reduction surgery, it is a limitation of our study in terms of generalizing the conclusions. Thus, it would certainly be better to analyze these variables in a greater patient group.
CONCLUSION
Reduction mammaplasty has a significant effect on short-term weight loss and gives the patients a strong motivation to change their habits into a more healthy lifestyle. However, all patients tend to return to their original body weight in the long-term follow-up, despite their high satisfaction rates and, despite their efforts to resume healthy lifestyle habits. The BRA appears to be a significant variable in short-term weight loss, but neither BMI nor BRA has any other significant effect on the outcome in any time section.
Supplementary Material
This article contains supplementary material located online at www.aestheticsurgeryjournal.com.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES