-
PDF
- Split View
-
Views
-
Cite
Cite
Taina Poranen-Clark, Mikaela B von Bonsdorff, Merja Rantakokko, Erja Portegijs, Johanna Eronen, Katja Pynnönen, Johan G Eriksson, Anne Viljanen, Taina Rantanen, The Temporal Association Between Executive Function and Life-Space Mobility in Old Age, The Journals of Gerontology: Series A, Volume 73, Issue 6, June 2018, Pages 835–839, https://doi.org/10.1093/gerona/glx217
Close - Share Icon Share
Abstract
Life-space mobility, an indicator of community mobility, describes person’s movements in terms of the distance from home, the frequency of movement, and the need of assistance for movement. Executive function (EF) is a higher-order cognitive function that supervises motor control and plays a key role in a person’s ability to function independently. Cognitive impairment often co-occurs with restricted life-space mobility; however, the direction of the longitudinal associations between EF and life-space mobility is unclear. The aim of this study was to investigate the temporal associations between EF and life-space mobility among community-dwelling older people.
One hundred eight community-dwelling persons aged 76 to 91 years participated in the 2 year follow-up study. EF was measured with the Trail Making Test. The Life-Space Assessment (range 0–120, higher scores indicate more mobility) was used to assess life-space mobility. Cross-lagged model design was used to examine longitudinal relationship between EF and life-space mobility. The model was adjusted for age and gender.
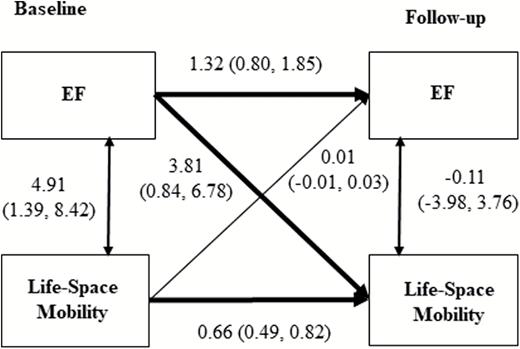
Average age of participants at baseline was 82.2 (SD 4.1) years and 59% were women. Better EF at baseline predicted higher life-space mobility at follow-up (path coefficient = 3.81, 95% confidential interval; 0.84, 6.78, p = .012), whereas baseline life-space mobility did not predict EF at follow-up.
EF was a determinant of life-space mobility. Supporting EF may enhance maintaining independence and active participation in old age.
Life-space mobility reflects a person’s physical ability as well as psychosocial capability relative to the environmental requirements (1). Life-space mobility assessment includes estimates of the distance, the frequency, and the need of assistance for mobility (1). Moving outside more often and traveling further away from home on a regular basis may be viewed as higher environmental complexity of mobility among older people (2,3). The further away from one’s home an individual moves the more complex the environment and the greater cognitive investments might be required (2). There is evidence that older people with better cognitive function have larger life-space mobility (4). Executive function (EF) has an important role in performance of control processes, which are required when planning and carrying out complex, goal-oriented tasks (5). Therefore, EF might be an important higher-order cognitive domain for older people enabling them to maintain their life-space mobility (6).
Coexisting mobility limitations and cognitive impairments are prevalent among community-dwelling older people (7) interfering with their independency and active participation in society. However, according to previous studies, the direction of the association between cognition and mobility is inconsistent (8). There are some evidence from longitudinal studies which used Mini-Mental State Examination (MMSE) as a measure of cognitive functioning, that having greater life-space mobility may be a protective factor for cognitive decline (3,9). Furthermore, constricted life-space mobility has been found to be associated with increased risk of Alzheimer diseases and mild cognitive impairment (10). Impaired EF is prevalent even among community-dwelling older people without a formal diagnosis of cognitive impairment and has been found to be associated with longitudinal declines in functional status (11–13). Furthermore, one previous study suggests that poor EF measured with the Trail Making Test (TMT) is a strong predictor of decline in lower extremity function (14), which is known to be associated with constricted life-space mobility (15). The results of a recent study reported TMT performance being associated with gait adaptation indicating that EF is important for planning and adjusting stepping in situations where rapid gait adjustment may be needed (16). Thus, the importance of EF may increase as task complexity increases in unfamiliar environments farther away from home. The TMT performance requires among other things attention, cognitive flexibility, and task switching (5) that are cognitive processes needed for everyday challenges for older people when moving around in environment (16). Consequently, using EF as a measure of cognitive functioning when investigating temporal association between cognition and life-space mobility could add useful information to current literature. The aim of this study was to assess the temporal association between EF and life-space mobility. Establishing the direction of the association between EF and life-space mobility might help us to target interventions more accurately to the factor in which declines seem to appear first.
Methods
Study Population
At baseline, altogether 169 community-dwelling people aged 76 to 91 years participated in the Hearing, Cognition, and Wellbeing Study. Face-to-face interviews and sensory, physical, and cognitive functioning measurements were conducted in the participants’ homes. Of the initial 169 persons, 108 participated in the follow-up study 2 years later (32 were not interested to participate, 19 had deceased, one moved outside study area, and nine were not reached) and formed the analytic sample of this study.
The participants of the current study were part of the Life-Space Mobility in Old Age (LISPE) study, described in detail previously (17). LISPE is a population-based study among community living older people including 848 participants. Using random number tables, a subset of 230 individuals was selected for the Hearing, Cognition, and Wellbeing substudy in year 2014 (18). Those willing to participate and who did not experience severe problems in communicating underwent the examinations and interviews during spring 2014 (n = 169). The Hearing, Cognition and Wellbeing substudy sample (n = 169) did not differ from the initial LISPE study sample (N = 848) in terms of sex, age, years of education, number of chronic conditions, lower extremity performance measured with the short physical performance battery (SPPB), or cognitive functioning measured with MMSE (all p-values > .127).
The LISPE study and the Hearing, Cognition, and Wellbeing substudy both comply with the principles of good scientific conduct and good clinical practice in all aspects of the Declaration of Helsinki and were approved by the Ethical Committee of the University of Jyväskylä. All participants gave a written informed consent.
Executive Function
EF was measured with TMT. The TMT is a paper-and-pencil task providing information on visual search, attention, processing speed, cognitive flexibility, and EF (19,20). The TMT consists of two parts. In the TMT-A task, participants were asked to make a trail with a pencil, sequentially drawing lines to connect randomly arranged encircled numbers (from 1 to 25) spread over a sheet of paper. In the TMT-B task, participants were asked to make a trail in numeric and alphabetical order (1-A-2-B-3-C, etc.) by drawing lines to connect randomly arranged encircles containing numbers (from 1 to 13) and letters (from A to L) spread over a sheet. The participants were asked to perform the task as quickly as possible without lifting the pencil from the paper. If an error occurred, the examiner pointed it out immediately. Then, the participants were asked to revert to last correct number or letter and continue there to complete the task at the expense of additional time. Time to complete each task was measured in seconds (21,22). A maximum accepted time to complete each part of the test was 240 seconds and maximum accepted amount of errors was 4 6,21,23. δ-TMT was calculated by subtracting time to perform TMT-A from time to perform TMT-B to control for the effects of motor function, visual scanning, and processing speed. δ-TMT has been used in previous studies to indicate executive functioning (24,25).
EF was categorized into three approximately equal distribution-based groups as follows. At baseline and follow-up, poor EF included those who started to do the TMT test but who could not complete the test an acceptable way; they did not perform TMT-A or TMT-B tasks within the given time (max 240 seconds), or made more than four errors, or who did not complete the task so that δ-TMT could not have been calculated (6). Intermediate EF included those whose δ-TMT was between 95 and 179 seconds at the baseline and between 97 and 180 seconds at the follow-up. Good EF included those whose δ-TMT was 94 seconds or less at the baseline and 97 seconds or less at the follow-up. The cutoff between intermediate and good EF was defined according to the median value of δ-TMT among those who completed the tests.
Life-Space Mobility
Life- space mobility was measured with the 15-item University of Alabama at Birmingham Study of Aging Life-Space Assessment (LSA) (1), which was translated into Finnish (26). The reliability of the Finnish translation of life-space assessment has been found to be acceptable (26). Life-space mobility assessment measures person’s actual mobility during 4 weeks preceding the assessment on the following life-space levels (=level score): bedroom (score 0), other rooms (1), outside home (2), neighborhood (3), town (4), beyond town (5). Participants were also asked how many times they attained each life-space level (=frequency score): daily (score 4), 4–6 times/week (3), 1–3 times/week (2), less than once a week(1), and whether they needed help from another person or used assistive device (=assistance score): no assistance (2), use of device only (1.5), personal assistance (1). A composite score was calculated as follows: level score × frequency score × assistance score at respective level, and then summed for all levels. Thus, a composite score reflects distance, frequency, and independence of movement and was used as an indicator of life-space mobility (26). The score ranges between 0 and 120, and higher scores indicated higher life-space mobility (17,26).
Covariates and Descriptive Variables
Participants’ age and gender derived from the national population register were used as covariates in the analysis. Number of self-reported chronic conditions, global cognitive functioning, and lower extremity functioning were used to describe the characteristics of the participants. Number of self-reported chronic conditions were calculated from a list of 22 physician-diagnosed diseases and an additional open-ended question about any other physician-diagnosed chronic diseases (15,17). Global cognitive functioning was assessed with MMSE, range 0–30 (27). Lower extremity functioning was assessed with SPPB. The test battery comprises three tests assessing standing balance, walking speed over a distance of 2.44 m, and time taken to complete five chair rises. Each test is rated from 0 to 4 points according to established age- and gender-specific cutoff points (28,29). A sum score (range 1–12) was calculated if at least two of the tests were completed. Higher scores indicate better lower extremity function (6,15).
Statistical Analyses
The longitudinal cross-lagged associations between EF and life-space mobility were estimated using cross-lagged model design. Cross-lagged analysis enables to study whether EF at baseline is associated with life-space mobility at follow-up after controlling for life-space mobility at baseline, or vice versa. The unstandardized values were used in the analyses. A weighted least square estimator was used to obtain parameter estimates. The model was adjusted for age and gender. The analysis were performed with MPLUS version 5.21 (Muthén and Muthén, 1998–2009) which uses the full information maximum likelihood procedure for handling missing values. The proportion of missing data in individual variables varied between 2.7% and 4.6%. The interaction between gender and EF on life-space mobility was not statistically significant (p > .185); thus, all analyses were pooled by gender. For all tests, two-tailed p-values are reported and the level of significance was set at p < .05. The descriptive data analyses were carried out with SPSS IBM version 24.0 (SPSS, Armonk, NY, IBM Corp.).
Results
Characteristics of the study participants at baseline and follow-up are presented in Table 1. The average age of the participants at baseline was 82.2 years (SD 4.1) and 59.3% of them were women. The proportion of those with poor EF increased during the 2 year follow-up from 24.3% to 29.5%. However, the global cognition measured with Mini-Mental State Examination remained nearly stable during the 2 year follow-up period. The average composite score of life-space mobility declined during the 2 year follow-up from 63.1 (SD 19.7) to 61.5 (SD 21.2) (Table1).
Means, SD, and proportions of characteristics of participants at baseline and at 2 year follow-up (n = 108)
| . | Baseline . | Follow-up . |
|---|---|---|
| % . | % . | |
| Women | 59.3 | 59.2 |
| Executive function (n = 103) | ||
| Good | 41.7 | 37.1 |
| Intermediate | 34.0 | 33.0 |
| Poor | 24.3 | 29.5 |
| Mean (SD) | Mean (SD) | |
| Age | 82.2 (4.1) | 84.3 (4.1) |
| Life-space mobility | 63.1 (19.7) | 61.5 (21.2) |
| Number of chronic conditions | 3.2 (1.6) | 3.4 (1.7) |
| Cognitive functioning (MMSE) | 26.3 (2.7) | 26.2 (3.0) |
| Lower extremity function (SPPB) | 9.21 (2.1) | 9.10 (2.2)† |
| . | Baseline . | Follow-up . |
|---|---|---|
| % . | % . | |
| Women | 59.3 | 59.2 |
| Executive function (n = 103) | ||
| Good | 41.7 | 37.1 |
| Intermediate | 34.0 | 33.0 |
| Poor | 24.3 | 29.5 |
| Mean (SD) | Mean (SD) | |
| Age | 82.2 (4.1) | 84.3 (4.1) |
| Life-space mobility | 63.1 (19.7) | 61.5 (21.2) |
| Number of chronic conditions | 3.2 (1.6) | 3.4 (1.7) |
| Cognitive functioning (MMSE) | 26.3 (2.7) | 26.2 (3.0) |
| Lower extremity function (SPPB) | 9.21 (2.1) | 9.10 (2.2)† |
Note: MMSE = Mini-Mental State Examination; SPPB = Short physical performance battery.
†n =106.
Means, SD, and proportions of characteristics of participants at baseline and at 2 year follow-up (n = 108)
| . | Baseline . | Follow-up . |
|---|---|---|
| % . | % . | |
| Women | 59.3 | 59.2 |
| Executive function (n = 103) | ||
| Good | 41.7 | 37.1 |
| Intermediate | 34.0 | 33.0 |
| Poor | 24.3 | 29.5 |
| Mean (SD) | Mean (SD) | |
| Age | 82.2 (4.1) | 84.3 (4.1) |
| Life-space mobility | 63.1 (19.7) | 61.5 (21.2) |
| Number of chronic conditions | 3.2 (1.6) | 3.4 (1.7) |
| Cognitive functioning (MMSE) | 26.3 (2.7) | 26.2 (3.0) |
| Lower extremity function (SPPB) | 9.21 (2.1) | 9.10 (2.2)† |
| . | Baseline . | Follow-up . |
|---|---|---|
| % . | % . | |
| Women | 59.3 | 59.2 |
| Executive function (n = 103) | ||
| Good | 41.7 | 37.1 |
| Intermediate | 34.0 | 33.0 |
| Poor | 24.3 | 29.5 |
| Mean (SD) | Mean (SD) | |
| Age | 82.2 (4.1) | 84.3 (4.1) |
| Life-space mobility | 63.1 (19.7) | 61.5 (21.2) |
| Number of chronic conditions | 3.2 (1.6) | 3.4 (1.7) |
| Cognitive functioning (MMSE) | 26.3 (2.7) | 26.2 (3.0) |
| Lower extremity function (SPPB) | 9.21 (2.1) | 9.10 (2.2)† |
Note: MMSE = Mini-Mental State Examination; SPPB = Short physical performance battery.
†n =106.
Figure 1 shows the unstandardized coefficients of cross-lagged model with 2 year follow-up for EF and life-space mobility. At baseline, better EF was associated with higher life-space mobility. Both EF and life-space mobility showed relatively strong stability between baseline and follow-up assessments. After controlling for age, gender, and taking into account previous measurements of EF and life-space mobility, the analysis revealed that better EF at baseline predicted higher life-space mobility at follow-up (path coefficient = 3.81, 95% confidential interval; 0.84, 6.78, p = .012), whereas baseline life-space mobility was not associated with EF at follow-up (Figure 1). The cross-lagged model fitted the data well Comparative Fit Index was 1.000, Tucker Lewis Index was 1.000, and root mean square error approximation less than 0.0005.
Unstandardized coefficients (95% confidence intervals) of cross-lagged model with 2 year follow-up for EF and life-space mobility adjusted for age and gender (n = 108). Path coefficients are statistically significant if zero is not included in the confidential intervals.
Compared with those who did not participate in the follow-up study (n = 61), those who participated (n = 108) were younger (82.2 years, SD 4.1 vs. 83.6 years, SD 4.3, p = .038), and they had higher SPPB (9.3, SD 2.0 vs. 7.2, SD 3.4, p < .001), MMSE (26.3, SD 2.7 vs. 25.4, SD 2.5, p = .033), and life-space mobility scores (63.1, SD 19.7 vs. 51.2, SD 20.4, p < .001) at baseline. The proportion of those who dropped out was highest among those with poor EF (53.7%), followed by those with intermediate (30.0%) or good (18.9%) EF. Those with poor EF at baseline were five times (OR = 4.99, 95% CI 2.09, 11.92), and those with intermediate EF almost two times (OR =1.84, 95% CI 0.74, 4.61) more likely to drop out from the follow-up compared with those with good EF.
Finally, we conducted additional cross-lagged modeling; first, to examine a stricter cut-point for good TMT, second, to analyze MMSE as an indicator of global cognition, and third, using δ-TMT as a continuous variable. Using more strict cut-points suggested by an earlier study (good δ-TMT performance < 60 seconds) (30) to define good EF (at baseline cut-point for good EF was ≤60 seconds and at follow-up ≤72 seconds) did not change the results. The analysis for MMSE and life-space mobility revealed similar associations as with using EF; coefficients and 95% confidential intervals for baseline MMSE predicting follow-up life-space was 1.22 (0.29, 2.15) and baseline life-space mobility predicting follow-up MMSE 0.01(−0.01, 0.03). The associations for EF as a continuous variable and life-space mobility among those who completed both parts of the TMT test (n = 78) were not statistically significant in either of the directions.
Discussion
To the best of our knowledge, we were the first to examine the temporal association between EF and life-space mobility among community-dwelling older people. Better EF at baseline predicted higher life-space mobility at follow-up, whereas baseline life-space mobility did not predict EF at follow-up. Thus, our findings suggest that impaired EF is a precedent for restricted life-space mobility rather than restriction of life-space would further influence cognitive decline.
It is obvious in the light of previous studies that cognition is interrelated with mobility (7). In addition to emerging literature on the associations between cognitive function and mobility, we were using specific higher-order cognitive domain, EF, and a multidimensional mobility measure, life-space mobility, as measurements. Life-space mobility reflects person’s actual mobility through a given area over a specific time period and incorporates not only physical aspects of mobility but also psychosocial capability for participation in society (1). Furthermore, we examined which one of these measurements, EF or life-space mobility, is a stronger predictor for one another, whereas previous studies have predicted associations only for one of the possible directions (9,10). This was done by using analysis that enables simultaneous examination of longitudinal influences of one factor on the other and vice versa, while controlling for contemporary associations between factors, and the stability of each factor over time. The association between EF and mobility has been reported being bidirectional (8,31). However, our results are in line with some of the previous studies suggesting that EF is a predictor for mobility decline (12–14) and conflicting the previous results that suggest that life-space mobility predicts changes in cognitive functioning (3,9,10). The latter might be explained by the fact that neither of the studies had EF as a measure of cognitive functioning. After all, a person might have some deficit of EF, despite evident cognitive impairment (12).
According to the environmental complexity theory, a more demanding environment requires more cognitive investment leading to increase in cognitive activity consequently resulting in better cognitive functioning (2). However, our results suggest that higher-order cognitive functioning such as executive functioning is a prerequisite for the capability to move further away from home and enabling to widen one’s life-space. Life-space mobility is a mobility measure that takes into account all movement in its’ different forms through one’s environment. The life-space mobility reaching only to one’s close neighborhood may require less cognitive investment than if an individual would be orienteering oneself further away from a familiar environment, and perhaps using a vehicle for transportation. Reduction in life-space mobility may reflect early changes in cognitive functioning. Impairment in EF may affect an individual’s willingness to travel further away from home even before any other markers of cognitive decline have appeared. Restricted life-space mobility may be seen as an early sign of cognitive decline resulting from EF impairment.
In recent years, the understanding of the role of the brain in age-related declines in mobility has increased (32,33). Furthermore, EF has been identified as one of the potential mediators between age-related cognitive decline and functional ability (34). Cognitive processes such as attention, action-inhibition, and task-switching are dependent on EF and needed for motor control (35). These control processes are primarily supported by frontal areas of the brain that are most vulnerable in the aging process (35), which might potentially explain the causal relationship between EF and life-space mobility. Decline in life-space mobility has been found to be associated with decline in quality of life (36) and development of ADL disability (37). Our earlier study suggested that poor EF may predict a steeper decline in life-space mobility but the results did not quite reach statistical significant; hence, the causal association between EF and life-space mobility stayed unclear (6). However, the result of this study confirms our earlier suggestions of EF being a predictor of life-space mobility. Furthermore, poorer lower extremity functioning and difficulties in use of transportation partly explained the association between poor EF and lower life-space mobility (6). Thus, we did not adjust for SPPB as it being potential mediator between EF and life-space mobility (6). Future studies should examine if promoting EF by means of cognitive training interventions could possibly delay mobility limitations that further diminish life-space mobility.
Our study had several strengths. By using life-space mobility and EF as measurements in this study, we were able to further existing literature relative to association between cognitive functioning and mobility. Furthermore, we were able to include considerable old people (range 78–93 years at follow-up) from all social strata into this study, and the participant did not have severe cognitive decline at baseline (mean MMSE 26.3, SD 2.7, and 12% < 23). In addition, we used computer-assisted face-to-face interviews by trained interviewers at participants’ homes, which probably improve the quality of data. Furthermore, we conducted several further modeling to test our results. Using more strict cut-points for good EF showed that the results were not dependent on the intermediate-good cut-point. The results of the cross-lagged model using MMSE instead of EF as the cognitive measure revealed similar associations. We found no statistically significant associations in either of directions when using EF measure as a continuous variable in cross-lagged modeling. This suggests that the cross-lagged association between baseline EF and follow-up life-space mobility observed in the larger sample where all the participants were included was driven by the poor values. This also supports our finding that the null life space mobility—EF association was not due to the scale properties of the categorized EF variable but rather due to the absence of a causal relationship. We are aware that the limited sample size in these sensitivity analyses decreases power even further; however, the coefficient is so low that it may not be considered material.
Our study had some limitations. First of all, due to the fact that the participants with poorer functioning were more likely to drop out from the follow-up study, the results can be generalized only to somewhat better functioning community-dwelling older adults, and it is probably that the strength of the associations over time may be underestimated. Second, we had only a 2 year follow-up. Although this is a significant time period among older people to experience noticeable changes in functional capability, a longer follow-up period might reveal stronger effects. Third, we were using a single test to measure EF instead of multiple tests due to time constraints in the study protocol considering that the participants were very old. Although TMT is a widely used test and simple and easy to perform, further studies should use several test batteries for a more comprehensive evaluation of EF.
Conclusions
According to our knowledge, we were the first to explore the temporal association between EF and life-space mobility among community-dwelling older people. The results of the study suggest that better EF is a precedent for higher life-space mobility laying ground to future studies on the topic using larger sample sizes and longer follow-up periods with multiple follow-up points. Supporting EF may help maintain higher life-space mobility enhancing independency and quality of life in old age.
Funding
This study was supported by the Academy of Finland (the Future of Living and Housing Program ASU-LIVE; grant number 255403 [to TR], number 263729 [to AV]; number 285747 [to MR]; numbers 129369, 129907, 135072, 129255, and 126775 [to JGE], and number 257239 [to MBvB]; Finnish Ministry of Education and Culture [to TR, MR, and EP]. TP-C was supported by Yrjö Jahnsson Foundation and Juho Vainio Foundation.
Conflict of Interest Statement
None declared.