-
PDF
- Split View
-
Views
-
Cite
Cite
David JW Knight, Ravi P Mahajan, Patient positioning in anaesthesia, Continuing Education in Anaesthesia Critical Care & Pain, Volume 4, Issue 5, October 2004, Pages 160–163, https://doi.org/10.1093/bjaceaccp/mkh044
Close - Share Icon Share
Abstract
The aim of optimal positioning for surgery is to provide the best surgical access while minimizing potential risk to the patient. Each position carries some degree of risk and this is magnified in the anaesthetized patient who cannot make others aware of compromised positions. Commonly adopted positions include supine, lithotomy, Lloyd Davies, lateral, seated and prone. Many of these are modified with the addition of a vertical tilt (Trendelenburg or reverse Trendelenburg). This article addresses the general complications associated with positioning as well as the position-specific physiological changes and complications.
Key points
Safe positioning requires planning and good communication between the anaesthetist and surgeon.
Adequate numbers of skilled personnel are required at the beginning and at the end of a surgical procedure to facilitate safe positioning.
Knowledge of physiological changes associated with the position can help predict potential problems.
All equipment should be secured and rechecked after every change in position.
Many complications do not reveal themselves for up to several days after surgery.
General complications
Transferring unconscious patients
Many patients are transferred and positioned on operating tables whilst they are unconscious. The manoeuvring and the final position itself have a bearing on potential injuries sustained under anaesthesia. The anaesthetist should ensure that all members of staff understand their individual roles and responsibilities in facilitating the movement. Intravascular lines, endotracheal tubes and urinary catheters should be free to move and adequately secured before any movement. The function and position of all equipment must be reassessed after repositioning (Table 1).
Repositioning checklist
| A . | Airway . | Endotracheal tube/LMA . | Patent and in correct position . |
|---|---|---|---|
| B | Breathing | Ventilation | Pulmonary compliance satisfactory |
| Auscultation | Both axillae | ||
| Monitoring | Sao2 | ||
| Capnograph trace and shape | |||
| C | Circulation | Monitoring | HR/BP/ECG still functioning and readings stable |
| Intravascular lines | All still in situ, patent and accessible | ||
| D | Disability/neurology | Eyes Neurovascular | Closed and protected Padded vulnerable areas and avoidance of excessive passive stretch |
| E | Exposure | All cables, catheters and electrodes | Checked and removed from the patient/operating table interface |
| Access | Maintain access for review of at risk areas if possible |
| A . | Airway . | Endotracheal tube/LMA . | Patent and in correct position . |
|---|---|---|---|
| B | Breathing | Ventilation | Pulmonary compliance satisfactory |
| Auscultation | Both axillae | ||
| Monitoring | Sao2 | ||
| Capnograph trace and shape | |||
| C | Circulation | Monitoring | HR/BP/ECG still functioning and readings stable |
| Intravascular lines | All still in situ, patent and accessible | ||
| D | Disability/neurology | Eyes Neurovascular | Closed and protected Padded vulnerable areas and avoidance of excessive passive stretch |
| E | Exposure | All cables, catheters and electrodes | Checked and removed from the patient/operating table interface |
| Access | Maintain access for review of at risk areas if possible |
Repositioning checklist
| A . | Airway . | Endotracheal tube/LMA . | Patent and in correct position . |
|---|---|---|---|
| B | Breathing | Ventilation | Pulmonary compliance satisfactory |
| Auscultation | Both axillae | ||
| Monitoring | Sao2 | ||
| Capnograph trace and shape | |||
| C | Circulation | Monitoring | HR/BP/ECG still functioning and readings stable |
| Intravascular lines | All still in situ, patent and accessible | ||
| D | Disability/neurology | Eyes Neurovascular | Closed and protected Padded vulnerable areas and avoidance of excessive passive stretch |
| E | Exposure | All cables, catheters and electrodes | Checked and removed from the patient/operating table interface |
| Access | Maintain access for review of at risk areas if possible |
| A . | Airway . | Endotracheal tube/LMA . | Patent and in correct position . |
|---|---|---|---|
| B | Breathing | Ventilation | Pulmonary compliance satisfactory |
| Auscultation | Both axillae | ||
| Monitoring | Sao2 | ||
| Capnograph trace and shape | |||
| C | Circulation | Monitoring | HR/BP/ECG still functioning and readings stable |
| Intravascular lines | All still in situ, patent and accessible | ||
| D | Disability/neurology | Eyes Neurovascular | Closed and protected Padded vulnerable areas and avoidance of excessive passive stretch |
| E | Exposure | All cables, catheters and electrodes | Checked and removed from the patient/operating table interface |
| Access | Maintain access for review of at risk areas if possible |
Peripheral nerve injuries
According to the American Society of Anesthesiologists Closed Claims Project database, perioperative nerve injury is the second most common class of injury (16%). Death (32%) and brain damage (12%) are rated first and third. These injuries can be severely debilitating and, to complicate matters, are often asymptomatic for several days after sugery. The traditionally held view that these injuries can be prevented/reduced by avoiding general anaesthesia are not supported by a recent prospective review that showed no significant difference in the incidence of ulnar neuropathy (the most common preoperative nerve injury) in patients undergoing general anaesthesia, regional anaesthesia or sedation.
The four underlying pathological mechanisms behind nerve injuries are:
stretch,
compression,
generalized ischaemia, and
metabolic derangement.
However, an identifiable mechanism of injury is found in <10% of cases. It is logical to identify patients at risk of developing a neuropathy (elderly, underlying neuropathy, diabetes, etc.) and then to reduce stretch/pressure on nerves during anaesthesia by careful positioning and padding.
Ocular injuries
The frequency of eye injury during anaesthesia and surgery is very low (<0.1% of anaesthetics), but the spectrum of injury ranges from mild discomfort to permanent loss of vision. Corneal abrasions are reported most commonly. They are caused by direct trauma to the cornea by foreign objects (face masks, surgical drapes, etc) combined with decreased basal tear production secondary to general anaesthesia. These injuries are largely preventable by application of eye tape but are not influenced by the use of eye ointment.
Special consideration should be given to the prone position where a head ring or horseshoe headrest is often utilized. In this position, the head may move significantly during a surgical procedure and result in direct pressure on the eye. If this pressure exceeds arterial pressure then arterial inflow may be reduced dramatically, resulting in potentially devastating retinal ischaemia.
Pressure sores
All patient positions are associated with abnormal amounts of pressure on relatively small parts of the body surface. A reduction in perfusion can result in tissue ischaemia, tissue breakdown and development of a pressure sore. Whilst macroscopic evidence of intraoperative development of pressure sore is unusual, the events precipitating postoperative development of this problem often commence in the intraoperative period. Dissipation of pressure is the main aim when preventing pressure sores. Careful positioning, padding, regular assessment and early postoperative mobilization help to achieve this.
Individual positions
Supine
Upon assuming the supine position, lung volumes are impaired by cephalad movement of the abdominal contents. The resulting reduction in functional residual capacity (FRC) is detrimental to gas exchange with an increase in ventilation–perfusion mismatching and decrease in pulmonary compliance. These effects are most significant if the closing capacity of the lung exceeds FRC.
Redistribution of pooled venous blood from the lower limbs increase venous return to the heart and subsequent increase in cardiac output. This may partially offset the cardiovascular depressant effects of many anaesthetic techniques.
The main complications are airway obstruction and decreased tidal volumes. Severe hypotension may occur as a result of compression of the inferior vena cava against the vertebral bodies; this typically affects obese or pregnant patients. Central redistribution of blood may lead to volume overload in the failing heart. In supine patients, there is an increased risk of regurgitation of gastric contents. The eye is at particular risk of direct or indirect trauma and it should be remembered that corneal drying can occur in as little as 10 min if the eye is left exposed. Both supraorbital and facial nerves are at risk of crush injuries from facemasks and endotracheal tube ties, respectively.
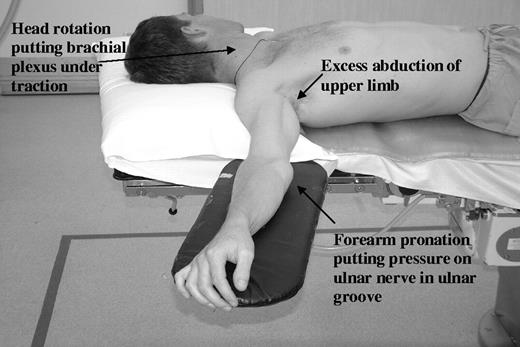
The brachial plexus (primarily C8 and T1 nerve roots) lies in close proximity to the relatively fixed first rib, clavicle and humerus and is predisposed to compression against these structures (Fig. 1). Damage here is often confused with distal ulnar injury as the ulnar nerve also originates primarily from C8/T1. To reduce the risk of brachial plexus injury, the arm should not be abducted by >90°, the hand pronated and head turned towards the abducted arm. More than a quarter of all perioperative nerve injuries involve the ulnar nerve. The classic site of injury is the exposed ulnar groove behind the medial epicondyle of the humerus. At this point, the nerve is exposed to both direct trauma from the sides of the operating table and indirect trauma from stretch. However, the cause of neuropathy is unknown in the vast majority of patients. The incidence is 3 times greater in males compared with females.
Poor positioning of upper limb leading to nerve traction and compression.
The classic supine position leads to loss of the natural lumbar lordosis and this is associated with postoperative low back pain. Maintenance of the lordosis with an inflatable wedge or another suitable device should be considered in all patients. The occiput, sacrum and heel are at risk of developing pressure sores and these areas should always be well padded. If heel pads are used, it is wise to ensure that the knee still maintains some degree of flexion otherwise a hyperextension injury may result.
Trendelenburg (head-down)
The Trendelenburg position was initially described with the torso supine and the legs upon the shoulders of an assistant. Later modifications lead to the classic 45° head-down tilt. However, the term is now often used to describe any head-down position.
Pulmonary and cardiovascular changes in this position are generally similar to, but more extreme than, those associated with the supine position. Diaphragmatic movement can be limited severely by the weight of the abdominal viscera; this further reduces FRC and increases atelectasis.
Ventilation-perfusion mismatch, raised intracranial pressure, raised intraocular pressure and passive regurgitation are potential complications; the severity and likelihood of these increases with amount of tilt.
Reverse Trendelenburg
The physiological effects of this position are similar to those associated with the seated position (see below). Beneficial physiological effects include an increase in head and neck venous drainage, reduction in intracranial pressure and reduced likelihood of passive regurgitation. The main complications of this position are hypotension and increased risk of venous air embolism (VAE).
Lithotomy/Lloyd Davies
The key difference between the lithotomy and Lloyd Davies position is the degree of hip and knee flexion. The resulting physiological changes and complications of these two positions are very similar and will therefore be considered together.
Physiological changes are similar to those seen in the Trendelenburg position (see above). It is important to remember that the leg elevation redistributes pooled lower limb blood and this may lead to volume overload in susceptible individuals. There is almost always some cephalad movement of the endotracheal tube upon assuming the lithotomy from the supine position. Unanticipated stimulation of the carina with bronchospasm or endobronchial intubation may result.
Resting the arms by the side of the patient can lead to crushed or even amputated digits when the leg section of the table is replaced or elevated at the end of the procedure. It is important to assess any limitation of joint movement before induction of anaesthesia as this may indicate important constraints on possible positioning. It is good practice to flex both legs at the hips and knees simultaneously. Extreme flexion of the hip joints can cause neural damage by stretch (sciatic and obturator nerves) or by direct pressure (compression of the femoral nerve as it is passes under the inguinal ligament). Distally, the common peroneal nerve and saphenous nerve are particularly at risk of compression injury as they wind round the neck of the fibula and medial tibial condyle, respectively.
In the lithotomy position, calf compression is almost inevitable and this predisposes to venous thromboembolism and compartment syndrome. The aetiology of compartment syndrome is probably a decrease in perfusion pressure caused by a combination of the weight of extremities against the supportive devices, reduction in compartment capacity and elevation of the lower limb above the heart. The risk was thought to be reduced by the use of foot stirrups alone as apposed to combined calf and foot supports; however there is little evidence to support this. The most consistent factor in development of compartment syndromes is the duration of the procedure. Patients requiring the lithotomy position for a period of >5 h may be considered for continuous invasive compartment pressure measurement.
Lateral
In the anaesthetized patient, the dependent lung is relatively under-ventilated and over-perfused, while the non-dependent lung is over-ventilated and under-perfused. This leads to a generally well tolerated increase in ventilation-perfusion inequality but can cause hypoxaemia in compromised patients.
This position is associated with the greatest number of ocular complications. These are primarily corneal abrasions, but occur in equal frequency in both the dependent and non-dependent eyes. The brachial plexus is at risk if the head and neck do not have sufficient lateral support. An axillary roll traditionally supports the thorax. If placement is inadequate, the neurovascular bundle can be compressed in the axilla. Even with adequate support, venous hypertension in the dependent arm is almost inevitable due to outflow obstruction. Padding should be placed between the legs to prevent damage to both common peroneal and saphenous nerve.
Seated
The classic seated position is only used in a few specialized centres and for specific procedures. The cardiovascular system is primarily affected by venous pooling, which can lead to resistant hypotension. Excessive neck flexion/extension may also be associated with obstruction of the neck veins.
The best-described and most feared complication of this position is venous air embolism, in particular during craniotomy. The pathophysiology is a combination of position related subatmospheric venous pressure and the non-collapsible nature of the dural sinuses. The description of prevention, detection and treatment of this complication is beyond the scope of this article but was reviewed recently in this journal (see key references).
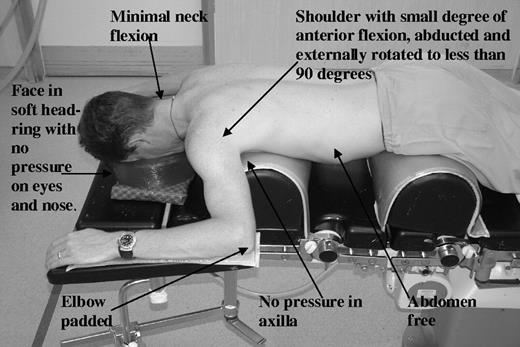
Prone
Many of the physiological changes that occur in this position can be minimized by careful positioning and, in particular, avoiding pressure on the abdomen (Fig. 2). The consequences of a high intra-abdominal pressure are inferior vena caval compression, reduced venous return and subsequent poor cardiac output. Associated pulmonary problems are caused by an increase in transdiaphragmatic pressure leading to reduced thoracic compliance.
An increase in FRC, changes in diaphragmatic excursions and improved ventilation–perfusion matching can significantly improve oxygenation in the prone position. This technique has been utilized for treatment of refractory hypoxaemia and in early acute respiratory distress syndrome ∼70–80% of patients turned prone initially benefit from improved oxygenation.
However, this position is most frequently associated with position-related injuries. Many of these can be avoided if adequate staff members are present to facilitate the manoeuvre at both beginning and end of the procedure. The head and neck need to be carefully positioned to prevent excess pressure on the nose and eyes. These structures are at particular risk; even if the initial position appears adequate, small movements are potentially hazardous. The final position of the upper limb should maintain a small degree of anterior flexion and then be abducted and externally rotated to <90°. This movement should be done in both upper limbs simultaneously. The brachial plexus is still at risk in this position and care should be taken to ensure that the chest support is not impinging upon the axilla. Forearm supports/pads should be in place to prevent direct compression of the ulnar nerve in the cubital tunnel and indirect compression of the axillary neurovascular bundle by axial pressure from the humerus. The dorsum of the foot as well as knees, pelvic area, breasts, axilla, elbows and face are all at risk of pressure necrosis in this position. Care should be taken to ensure that all these areas are properly supported and padded throughout the procedure.
Key references
Mure M, Lindahl SGE. Prone position improves gas exchange—but how?
Erie JK. Effect of position on ventilation. In: Faust RJ, ed. Anesthesiology Review, 2nd Edn. Philadelphia: Churchill Livingstone,
Roth R, Thisted RA, Erickson JP, Black S, Schreider BD. Eye injuries after nonocular surgery: a study of 60 965 anesthetics from 1998 to 1992.
Warner ME, LaMaster LM, Thoeming AK, Marienau ME, Warner MA. Compartment syndrome in surgical patients.