-
PDF
- Split View
-
Views
-
Cite
Cite
Li Ran, Xuyu Chen, Ying Wang, Wenwen Wu, Ling Zhang, Xiaodong Tan, Risk Factors of Healthcare Workers With Coronavirus Disease 2019: A Retrospective Cohort Study in a Designated Hospital of Wuhan in China, Clinical Infectious Diseases, Volume 71, Issue 16, 15 October 2020, Pages 2218–2221, https://doi.org/10.1093/cid/ciaa287
Close - Share Icon Share
Abstract
Coronavirus Disease 2019 (COVID-19), which originated in Wuhan, China, has caused many healthcare workers (HCWs) to be infected. Seventy-two HCWs manifested with acute respiratory illness were retrospectively enrolled to analyze the risk factors. The high-risk department, longer duty hours, and suboptimal hand hygiene after contacting with patients were linked to COVID-19.
At present, the pneumonia epidemic caused by SARS-Cov-2 originating in Wuhan, China is still alarming, having drawn a high-level concern over the world. According to the experience during the 2002 severe acute respiratory syndrome (SARS) outbreak, more emphasis should be placed on healthcare workers’ (HCWs) protection, because an approximately 1725 of front-line HCWs were infected by SARS [1]. Given the current Coronavirus Disease 2019 (COVID-19) epidemic, the infection among medical and nursing personnel is a common occurrence, ever since the first 15 affected cases were reported in Wuhan [2]. It was estimated that a total of 1716 Chinese HCWs were infected by COVID-19 until 11 February 2020 [3]. To better understand how to protect staff, it is necessary to understand the predisposing factors for HCW infection and nosocomial transmission. This retrospective cohort study of HCWs with acute respiratory illness in the designated hospital of Wuhan University sought to determine risk factors and behaviors associated with the development of COVID-19.
METHODS
Participants
We conducted a retrospective cohort study among the HCWs (>18 years of age) with acute respiratory symptoms in a single-center setting, who worked at the forefront to fight against COVID-19 since its outbreak. To define the cohort, all participants were clinicians and nurses from a designated hospital. The designated hospital is a 3300-bed grade-A tertiary hospital serving for the medical treatment in this outbreak. The case with acute respiratory symptoms was defined by any or multiple present symptoms like cough, fever, brachypnea, chest distress, headache, hemoptysis, others related to acute respiratory illness, and diarrhea, testing with radiologic characters, and laboratory evidence. All participants gave informed consent.
Procedure
HCWs in different departments were divided into 2 groups based on risk exposure. High-risk exposure was defined as the high-risk department (HRD) with interventional medical or surgical procedures that generate respiratory aerosols, including the respiratory department, infection department, intensive care unit (ICU), and surgical department. Other low-risk clinical departments were regarded as general groups (GD). Diagnosed cases of SARS-CoV-2 infection were identified as outcome variables. The follow-up ended on 28 January because all HCWs were confirmed with COVID-19 infection or noninfection. HCWs were required to fulfill an online questionnaire giving detailed information on sociodemographic characteristics, time to symptomatic progression, contact history, medical practice, hand hygiene, and proper personal protective equipment (PPE) (Appendix 1). A total of 83 questionnaires were collected, of which 72 were valid, with an effective rate of 86.75%.
Case Definition
The outcome variable was regarded as diagnosed COVID-19, which is defined according to “The diagnosis of COVID-19 conformed to diagnosis and treatment of novel coronavirus pneumonia (Trial Version 3)” issued by the National Health Commission of the People’s Republic of China. All cases were diagnosed with the test by polymerase chain reaction (PCR) nucleic acid. The novel coronavirus nucleic acid was detected by real-time fluorescence reverse transcription PCR, and the virus gene was sequenced, which was highly homologous with the known new coronavirus.
Statistical Analysis
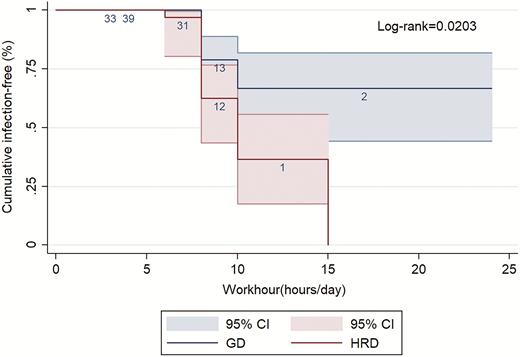
Continuous variables were described as mean (standard deviation) and median (interquartile range [IQR]), whereas categoric variables were presented as counts (frequency or percentages). Relative risk (RR) and its 95% confidence interval (CI) were calculated to compare outcomes between groups. Mentel-Haenszel tests and multivariate logistic regression were respectively used to identify the confounding factors and to assess the interaction effect between 2 variables. Kaplan-Meier survival curve was established, and the log-rank test was for subgroup differences. Statistical analyses were conducted using STATA software (version 14.0). P value <.05 was considered to be statistically significant.
RESULTS
Baseline of Sociodemographic Characteristics
Of these 72 people, 39 were classified in GD and 33 in HRD. Ages ranged from 21 to 66 years with a median (IQR) of 31 (28–40,12). The median (IQR) of daily work was 8 (8–10, 2) hours (Table 1). Before the cohort started, subject baseline characteristics were compared. Sex (χ 2 = 2.243, P = .134), types of HCWs (χ 2 = 0.076, P = .782), and age (35.24 vs 37.98, P = .579) were generally well balanced between the exposed and nonexposed group.
Sociodemographic Characteristics, Contact Histories, and Medical Operation and Protection of the Participants
| . | Total Cohort . | Infection . | Non-infection . |
|---|---|---|---|
| . | No./Median (IQR) . | No./Median (IQR) . | No./Median (IQR) . |
| Sex (male/female) | 22/50 | 14/14 | 8/36 |
| Age (years) | 31(28–40) | 39(31.25–46.75) | 30(26–34.50) |
| Occupation (clinician/nurse) | 38/34 | 19/9 | 19/25 |
| HRD/ GD | 33/39 | 18/10 | 15/29 |
| Isolation/Nonisolation ward | 6/66 | 1/27 | 5/39 |
| Worktime (hours/day) | 8(8–10) | 8(8–10) | 8(8–10) |
| Diagnosed family member (yes/no) | 3/69 | 3/25 | 0/44 |
| Suspected/Healthy family member (yes/no) | 2/70 | 1/27 | 1/43 |
| Diagnosed patient (yes/no) | 55/17 | 15/13 | 40/4 |
| Suspected patient (yes/no) | 41/31 | 11/17 | 30/14 |
| Huanan seafood market | 1/71 | 0/28 | 1/43 |
| Others (yes/no) | 0/72 | 0/0 | 0/72 |
| High-exposure operation (yes/no) | 13/59 | 3/25 | 10/34 |
| Tracheal intubation (yes/no) | 0/72 | 0/28 | 0/44 |
| Tracheotomy (yes/no) | 0/72 | 0/28 | 0/44 |
| Tracheal tube removal (yes/no) | 1/71 | 0/28 | 1/43 |
| CPR (yes/no) | 1/71 | 0/28 | 1/43 |
| Sputum suction (yes/no) | 11/61 | 2/26 | 9/35 |
| Fiber bronchoscopy (yes/no) | 1/71 | 0/28 | 1/43 |
| Laryngoscope (yes/no) | 0/72 | 0/28 | 0/44 |
| Unqualified hand-washing (yes/no) | 50/22 | 24/4 | 26/18 |
| Suboptimal hand hygiene before contact with patients (yes/no) | 39/33 | 22/6 | 17/27 |
| Suboptimal hand hygiene after contact with patients (yes/no) | 28/44 | 17/11 | 11/33 |
| Improper personal protective equipment (yes/no) | 49/23 | 24/4 | 25/19 |
| . | Total Cohort . | Infection . | Non-infection . |
|---|---|---|---|
| . | No./Median (IQR) . | No./Median (IQR) . | No./Median (IQR) . |
| Sex (male/female) | 22/50 | 14/14 | 8/36 |
| Age (years) | 31(28–40) | 39(31.25–46.75) | 30(26–34.50) |
| Occupation (clinician/nurse) | 38/34 | 19/9 | 19/25 |
| HRD/ GD | 33/39 | 18/10 | 15/29 |
| Isolation/Nonisolation ward | 6/66 | 1/27 | 5/39 |
| Worktime (hours/day) | 8(8–10) | 8(8–10) | 8(8–10) |
| Diagnosed family member (yes/no) | 3/69 | 3/25 | 0/44 |
| Suspected/Healthy family member (yes/no) | 2/70 | 1/27 | 1/43 |
| Diagnosed patient (yes/no) | 55/17 | 15/13 | 40/4 |
| Suspected patient (yes/no) | 41/31 | 11/17 | 30/14 |
| Huanan seafood market | 1/71 | 0/28 | 1/43 |
| Others (yes/no) | 0/72 | 0/0 | 0/72 |
| High-exposure operation (yes/no) | 13/59 | 3/25 | 10/34 |
| Tracheal intubation (yes/no) | 0/72 | 0/28 | 0/44 |
| Tracheotomy (yes/no) | 0/72 | 0/28 | 0/44 |
| Tracheal tube removal (yes/no) | 1/71 | 0/28 | 1/43 |
| CPR (yes/no) | 1/71 | 0/28 | 1/43 |
| Sputum suction (yes/no) | 11/61 | 2/26 | 9/35 |
| Fiber bronchoscopy (yes/no) | 1/71 | 0/28 | 1/43 |
| Laryngoscope (yes/no) | 0/72 | 0/28 | 0/44 |
| Unqualified hand-washing (yes/no) | 50/22 | 24/4 | 26/18 |
| Suboptimal hand hygiene before contact with patients (yes/no) | 39/33 | 22/6 | 17/27 |
| Suboptimal hand hygiene after contact with patients (yes/no) | 28/44 | 17/11 | 11/33 |
| Improper personal protective equipment (yes/no) | 49/23 | 24/4 | 25/19 |
Abbreviations: GD, general department; HRD, high-risk department; IQR, interquartile range.
Sociodemographic Characteristics, Contact Histories, and Medical Operation and Protection of the Participants
| . | Total Cohort . | Infection . | Non-infection . |
|---|---|---|---|
| . | No./Median (IQR) . | No./Median (IQR) . | No./Median (IQR) . |
| Sex (male/female) | 22/50 | 14/14 | 8/36 |
| Age (years) | 31(28–40) | 39(31.25–46.75) | 30(26–34.50) |
| Occupation (clinician/nurse) | 38/34 | 19/9 | 19/25 |
| HRD/ GD | 33/39 | 18/10 | 15/29 |
| Isolation/Nonisolation ward | 6/66 | 1/27 | 5/39 |
| Worktime (hours/day) | 8(8–10) | 8(8–10) | 8(8–10) |
| Diagnosed family member (yes/no) | 3/69 | 3/25 | 0/44 |
| Suspected/Healthy family member (yes/no) | 2/70 | 1/27 | 1/43 |
| Diagnosed patient (yes/no) | 55/17 | 15/13 | 40/4 |
| Suspected patient (yes/no) | 41/31 | 11/17 | 30/14 |
| Huanan seafood market | 1/71 | 0/28 | 1/43 |
| Others (yes/no) | 0/72 | 0/0 | 0/72 |
| High-exposure operation (yes/no) | 13/59 | 3/25 | 10/34 |
| Tracheal intubation (yes/no) | 0/72 | 0/28 | 0/44 |
| Tracheotomy (yes/no) | 0/72 | 0/28 | 0/44 |
| Tracheal tube removal (yes/no) | 1/71 | 0/28 | 1/43 |
| CPR (yes/no) | 1/71 | 0/28 | 1/43 |
| Sputum suction (yes/no) | 11/61 | 2/26 | 9/35 |
| Fiber bronchoscopy (yes/no) | 1/71 | 0/28 | 1/43 |
| Laryngoscope (yes/no) | 0/72 | 0/28 | 0/44 |
| Unqualified hand-washing (yes/no) | 50/22 | 24/4 | 26/18 |
| Suboptimal hand hygiene before contact with patients (yes/no) | 39/33 | 22/6 | 17/27 |
| Suboptimal hand hygiene after contact with patients (yes/no) | 28/44 | 17/11 | 11/33 |
| Improper personal protective equipment (yes/no) | 49/23 | 24/4 | 25/19 |
| . | Total Cohort . | Infection . | Non-infection . |
|---|---|---|---|
| . | No./Median (IQR) . | No./Median (IQR) . | No./Median (IQR) . |
| Sex (male/female) | 22/50 | 14/14 | 8/36 |
| Age (years) | 31(28–40) | 39(31.25–46.75) | 30(26–34.50) |
| Occupation (clinician/nurse) | 38/34 | 19/9 | 19/25 |
| HRD/ GD | 33/39 | 18/10 | 15/29 |
| Isolation/Nonisolation ward | 6/66 | 1/27 | 5/39 |
| Worktime (hours/day) | 8(8–10) | 8(8–10) | 8(8–10) |
| Diagnosed family member (yes/no) | 3/69 | 3/25 | 0/44 |
| Suspected/Healthy family member (yes/no) | 2/70 | 1/27 | 1/43 |
| Diagnosed patient (yes/no) | 55/17 | 15/13 | 40/4 |
| Suspected patient (yes/no) | 41/31 | 11/17 | 30/14 |
| Huanan seafood market | 1/71 | 0/28 | 1/43 |
| Others (yes/no) | 0/72 | 0/0 | 0/72 |
| High-exposure operation (yes/no) | 13/59 | 3/25 | 10/34 |
| Tracheal intubation (yes/no) | 0/72 | 0/28 | 0/44 |
| Tracheotomy (yes/no) | 0/72 | 0/28 | 0/44 |
| Tracheal tube removal (yes/no) | 1/71 | 0/28 | 1/43 |
| CPR (yes/no) | 1/71 | 0/28 | 1/43 |
| Sputum suction (yes/no) | 11/61 | 2/26 | 9/35 |
| Fiber bronchoscopy (yes/no) | 1/71 | 0/28 | 1/43 |
| Laryngoscope (yes/no) | 0/72 | 0/28 | 0/44 |
| Unqualified hand-washing (yes/no) | 50/22 | 24/4 | 26/18 |
| Suboptimal hand hygiene before contact with patients (yes/no) | 39/33 | 22/6 | 17/27 |
| Suboptimal hand hygiene after contact with patients (yes/no) | 28/44 | 17/11 | 11/33 |
| Improper personal protective equipment (yes/no) | 49/23 | 24/4 | 25/19 |
Abbreviations: GD, general department; HRD, high-risk department; IQR, interquartile range.
Common Symptoms
Common symptoms were fever (85.71%), cough (60.71%), brachypnea (7.14%), chest distress (7.14%), headache (7.14%), diarrhea (7.14%), and hemoptysis (7.14%) among the 28 HCWs diagnosed with COVID-19.
Contact History
Table 2 demonstrated that diagnosed family member (DFM), diagnosed patient (DP), and suspected patient (SP) were related to infections of HCWs, separately with the relative risk of 2.76 (95% CI = 2.02–3.77, P < .01), 0.36 (95% CI = .22–.59, P < .01), and 0.49 (95% CI = .27–.89, P < .05).
The Relative Risk of Infection in Different Contact Histories and Medical Operation and Protection
| Exposure Factor . | Relative Risk . | 95% CI . | P value . |
|---|---|---|---|
| Contact history | |||
| Diagnosed family member | 2.76 | 2.02–3.77 | <.01** |
| Suspected family member | 1.30 | .31–5.35 | >.05 |
| Diagnosed patient | 0.36 | .22–.59 | <.01** |
| Suspected patient | 0.49 | .27–.89 | <.05* |
| Huanan seafood market | 0.63 | .06–7.08 | >.05 |
| Others | … | … | |
| Medical operation and protection | |||
| High exposure operation | 0.54 | .19–1.53 | >.05 |
| Tracheal intubation | … | … | |
| Tracheotomy | … | … | |
| Tracheal tube removal | 0.63 | .06–7.08 | >.05 |
| CPR | 0.63 | .06–7.08 | >.05 |
| Sputum suction | 0.43 | .12–1.55 | >.05 |
| Fiber bronchoscopy | 0.63 | .06–7.08 | >.05 |
| Laryngoscope | … | … | |
| Unqualified hand-washing | 2.64 | 1.04–6.71 | <.05* |
| Suboptimal hand hygiene before contact with patients | 3.10 | 1.43–6.73 | <.01** |
| Suboptimal hand hygiene after contact with patients | 2.43 | 1.34–4.39 | <.01** |
| Improper personal protective equipment | 2.82 | 1.11–7.18 | <.05* |
| Exposure Factor . | Relative Risk . | 95% CI . | P value . |
|---|---|---|---|
| Contact history | |||
| Diagnosed family member | 2.76 | 2.02–3.77 | <.01** |
| Suspected family member | 1.30 | .31–5.35 | >.05 |
| Diagnosed patient | 0.36 | .22–.59 | <.01** |
| Suspected patient | 0.49 | .27–.89 | <.05* |
| Huanan seafood market | 0.63 | .06–7.08 | >.05 |
| Others | … | … | |
| Medical operation and protection | |||
| High exposure operation | 0.54 | .19–1.53 | >.05 |
| Tracheal intubation | … | … | |
| Tracheotomy | … | … | |
| Tracheal tube removal | 0.63 | .06–7.08 | >.05 |
| CPR | 0.63 | .06–7.08 | >.05 |
| Sputum suction | 0.43 | .12–1.55 | >.05 |
| Fiber bronchoscopy | 0.63 | .06–7.08 | >.05 |
| Laryngoscope | … | … | |
| Unqualified hand-washing | 2.64 | 1.04–6.71 | <.05* |
| Suboptimal hand hygiene before contact with patients | 3.10 | 1.43–6.73 | <.01** |
| Suboptimal hand hygiene after contact with patients | 2.43 | 1.34–4.39 | <.01** |
| Improper personal protective equipment | 2.82 | 1.11–7.18 | <.05* |
Abbreviation: CI, confidence interval; CPR, cardiopulmonary resuscitation.
*P < .05, **P < .01.
The Relative Risk of Infection in Different Contact Histories and Medical Operation and Protection
| Exposure Factor . | Relative Risk . | 95% CI . | P value . |
|---|---|---|---|
| Contact history | |||
| Diagnosed family member | 2.76 | 2.02–3.77 | <.01** |
| Suspected family member | 1.30 | .31–5.35 | >.05 |
| Diagnosed patient | 0.36 | .22–.59 | <.01** |
| Suspected patient | 0.49 | .27–.89 | <.05* |
| Huanan seafood market | 0.63 | .06–7.08 | >.05 |
| Others | … | … | |
| Medical operation and protection | |||
| High exposure operation | 0.54 | .19–1.53 | >.05 |
| Tracheal intubation | … | … | |
| Tracheotomy | … | … | |
| Tracheal tube removal | 0.63 | .06–7.08 | >.05 |
| CPR | 0.63 | .06–7.08 | >.05 |
| Sputum suction | 0.43 | .12–1.55 | >.05 |
| Fiber bronchoscopy | 0.63 | .06–7.08 | >.05 |
| Laryngoscope | … | … | |
| Unqualified hand-washing | 2.64 | 1.04–6.71 | <.05* |
| Suboptimal hand hygiene before contact with patients | 3.10 | 1.43–6.73 | <.01** |
| Suboptimal hand hygiene after contact with patients | 2.43 | 1.34–4.39 | <.01** |
| Improper personal protective equipment | 2.82 | 1.11–7.18 | <.05* |
| Exposure Factor . | Relative Risk . | 95% CI . | P value . |
|---|---|---|---|
| Contact history | |||
| Diagnosed family member | 2.76 | 2.02–3.77 | <.01** |
| Suspected family member | 1.30 | .31–5.35 | >.05 |
| Diagnosed patient | 0.36 | .22–.59 | <.01** |
| Suspected patient | 0.49 | .27–.89 | <.05* |
| Huanan seafood market | 0.63 | .06–7.08 | >.05 |
| Others | … | … | |
| Medical operation and protection | |||
| High exposure operation | 0.54 | .19–1.53 | >.05 |
| Tracheal intubation | … | … | |
| Tracheotomy | … | … | |
| Tracheal tube removal | 0.63 | .06–7.08 | >.05 |
| CPR | 0.63 | .06–7.08 | >.05 |
| Sputum suction | 0.43 | .12–1.55 | >.05 |
| Fiber bronchoscopy | 0.63 | .06–7.08 | >.05 |
| Laryngoscope | … | … | |
| Unqualified hand-washing | 2.64 | 1.04–6.71 | <.05* |
| Suboptimal hand hygiene before contact with patients | 3.10 | 1.43–6.73 | <.01** |
| Suboptimal hand hygiene after contact with patients | 2.43 | 1.34–4.39 | <.01** |
| Improper personal protective equipment | 2.82 | 1.11–7.18 | <.05* |
Abbreviation: CI, confidence interval; CPR, cardiopulmonary resuscitation.
*P < .05, **P < .01.
Medical Operation and Protection
Illustrated in Table 2, the relative risks and their 95% CIs of unqualified hand-washing, suboptimal hand hygiene before and after contact with patients, and improper PPE were 2.64 (95% CI = 1.04–6.71, P < .05), 3.10 (95% CI = 1.43–6.73, P < .01), 2.43 (95% CI = 1.34–4.39, P < .01), and 2.82 (95% CI = 1.11–7.18, P < .05), respectively.
HRD and GD
It was indicated that the HRD group had 2.13 times higher risk in developing COVID-19 compared with the GD group (crude RR = 2.13, 95% CI: 1.45–3.95, P < .05). After a stratified analysis with the Mantel-Haenszel method to adjust confounding factors, sex (RRHM = 3.08, 95% CI: 1.09–8.71, Phomogeneity = .70), type of HCWs (RRHM = 3.56, 95% CI: 1.29–9.84, Phomogeneity = .27), and sex * type of HCWs (RRHM = 2.85, 95% CI: 1.03–7.90, Phomogeneity = .25) showed a homogeneity between layers.
Effect Interaction
The interaction effect between exposure and other factors was conducted with logistic regression. It revealed that: (1) male + HRD (RR = 2.45, 95% CI: 1.38–3.45, P < .01) with control for HCW; (2) clinician + HRD (RR = 2.00, 95% CI: 1.03–2.89, P < .05) with control for sex; and (3) unclean hand after contact with patients (UHA) + HRD (RR = 3.07, 95%CI: 1.14–5.15, P < .01), UHA + GD (RR = 2.45, 95% CI: 1.45–4.03, P < .05), and clean hand +HRD (RR = 2.30, 95% CI: 1.30–3.77, P < .05) with control for sex and HCW, were significant.
Time to Event
Figure 1 is a Kaplan-Meier curve of the whole 72 participants in the cohort. It revealed that the cumulative proportion of infection-free would be decreased with daily workhour, which is more obvious in HRD (P < .05). To be specific, all of the staff in HRD would be infected if they worked 15 hours per day.
Kaplan-Meier survival estimates for COVID-19 between HRD and GD. Abbreviations: CI, confidence interval; COVID-19, Coronavirus disease 2019; GD, general department; HRD, high-risk department.
DISCUSSION
Nosocomial infections of respiratory infectious diseases are common to see, and COVID-19 was found linked with the exposed department, duty hour, and hand hygiene in this study.
Similar to our findings, previous researches have proved the higher susceptibility of respiratory infectious disease for HRD workers [4]. This phenomenon has also been discovered in epidemics of SARS [5, 6]. For example, data from 7 hospitals in China showed an incidence of HCWs infected by SARS up to 13.53% in ICU [6]. We speculated that HRD experienced more exposures, such as a higher frequency of interventional medical operation and aerosol-generating procedure [7].
HCWs in China are generally working with long hours, with an average workweek exceeding 54 hours [8]. Moderate work hour benefits the health and safety of HCWs, whereas prolonged work (>10 hours/day) would possibly increase the risk of respiratory infections [9, 10]. An obvious COVID-19 infection ascending with daily work hours was found in this study. Consideration of duty hour restrictions (<10 hours/day) should be considered, depending on the medical staff’s specific role.
Contact transmission is one of the main routes of the SARS-CoV-2. Transmission from patients to HCWs usually follows contamination of the HCWs’ hands after touching either patients or fomites, whereas hand hygiene is considered the most important prevention measure for healthcare-associated infections. Our results highlight the importance of hand hygiene after contacting or caring for COVID-19 patients, which is highly consistent with other researchers [11, 12]. As we all know, washing hands can significantly reduce the residual viruses or bacteria on your hands.
Our research has some limitations. Recall bias on the part of HCWs is possible inherent in the survey study. To minimize the bias, investigators were required to verify the information using medical records in the hospital information system. Potential unmeasured confounding, especially with regards to gender differences was possibly another limitation. Hence, effect confounding was controlled as much as possible in the analysis. Limitations lie in small sample size, single-center aspect, and less representative research subjects, making the results difficult to be generalized. Nevertheless, the results support current recommendations for hand hygiene and duty hour reduction among HCWs.
CONCLUSION
HCWs who worked in HRD and with suboptimal hand hygiene after contacting patients had a higher risk of COVID-19. Higher risk with longer duty hours was found, especially in HRD. A call to confirm these risk factors in other larger cohorts, as well as work to mitigate these, would be appropriate.
Notes
Author contributions. L. R. designed the survey, analyzed data, and wrote the paper. X. y. C. designed the survey, collected and analyzed data, and wrote the paper. Y. W. collected data and wrote the paper. W. w. W. collected data and wrote the paper. L. Z. collected and analyzed data and wrote the paper. X. d. T. edited the paper. All authors have read and approved the manuscript in its final form.
Acknowledgments. The authors thank the designated hospital of Wuhan University and the teammates who completed the survey. We thank all medical staff who work on the frontline. We also thank Professor Tan and Wuhan University for making this study possible. The data sets supporting the conclusions of this article are available. The research is a designated hospital of Wuhan University and supported by Wuhan University. Due to the severe epidemic situation in Wuhan, the consent we obtained from study participants was verbal. We will upload a written ethics statement after the epidemic is over.
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
Author notes
L. R., X. C., and Y. W. contributed equally to this paper.




Comments