-
PDF
- Split View
-
Views
-
Cite
Cite
Lidia Morawska, Donald K Milton, It Is Time to Address Airborne Transmission of Coronavirus Disease 2019 (COVID-19), Clinical Infectious Diseases, Volume 71, Issue 9, 1 November 2020, Pages 2311–2313, https://doi.org/10.1093/cid/ciaa939
Close - Share Icon Share
We appeal to the medical community and to the relevant national and international bodies to recognize the potential for airborne spread of coronavirus disease 2019 (COVID-19). There is significant potential for inhalation exposure to viruses in microscopic respiratory droplets (microdroplets) at short to medium distances (up to several meters, or room scale), and we are advocating for the use of preventive measures to mitigate this route of airborne transmission.
Studies by the signatories and other scientists have demonstrated beyond any reasonable doubt that viruses are released during exhalation, talking, and coughing in microdroplets small enough to remain aloft in air and pose a risk of exposure at distances beyond 1–2 m from an infected individual ([1–4]). For example, at typical indoor air velocities [5], a 5-μm droplet will travel tens of meters, much greater than the scale of a typical room, while settling from a height of 1.5 m to the floor. Several retrospective studies conducted after the severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1) epidemic demonstrated that airborne transmission was the most likely mechanism explaining the spatial pattern of infections [6]. Retrospective analysis has shown the same for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [7–10]. In particular, a study in their review of records from a Chinese restaurant observed no evidence of direct or indirect contact between the 3 parties [10]. In their review of video records from the restaurant, they observed no evidence of direct or indirect contact between the 3 parties. Many studies conducted on the spread of other viruses, including respiratory syncytial virus (RSV) [11], Middle East Respiratory Syndrome Coronavirus (MERS-CoV) [8], and influenza [2, 4], show that viable airborne viruses can be exhaled [2] and/or detected in the indoor environment of infected patients [11, 12]. This poses the risk that people sharing such environments can potentially inhale these viruses, resulting in infection and disease. There is every reason to expect that SARS-CoV-2 behaves similarly, and that transmission via airborne microdroplets [10, 13] is an important pathway. Viral RNA associated with droplets <5 μm has been detected in air [14], and the virus has been shown to maintain infectivity in droplets of this size [9]. Other viruses have been shown to survive equally well, if not better, in aerosols compared to droplets on a surface [15].
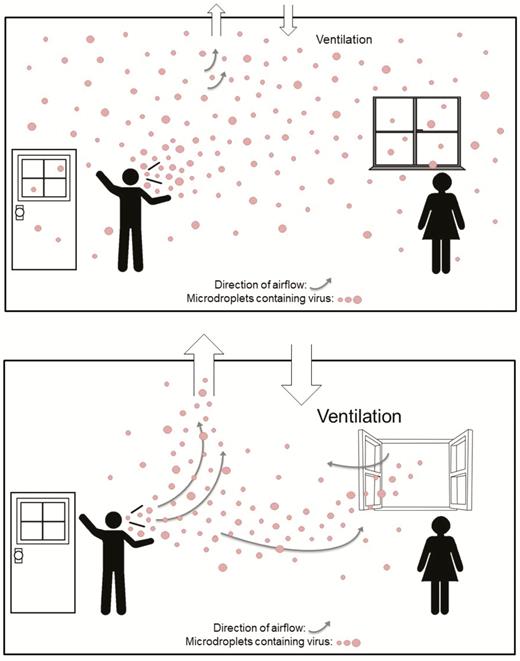
The current guidance from numerous international and national bodies focuses on hand washing, maintaining social distancing, and droplet precautions. Most public health organizations, including the World Health Organization (WHO) [16], do not recognize airborne transmission except for aerosol-generating procedures performed in healthcare settings. Hand washing and social distancing are appropriate but, in our view, insufficient to provide protection from virus-carrying respiratory microdroplets released into the air by infected people. This problem is especially acute in indoor or enclosed environments, particularly those that are crowded and have inadequate ventilation [17] relative to the number of occupants and extended exposure periods (as graphically depicted in Figure 1). For example, airborne transmission appears to be the only plausible explanation for several superspreading events investigated that occurred under such conditions [10], and others where recommended precautions related to direct droplet transmissions were followed.
Distribution of respiratory microdroplets in an indoor environment with (A) inadequate ventilation and (B) adequate ventilation.
The evidence is admittedly incomplete for all the steps in COVID-19 microdroplet transmission, but it is similarly incomplete for the large droplet and fomite modes of transmission. The airborne transmission mechanism operates in parallel with the large droplet and fomite routes [16] that are now the basis of guidance. Following the precautionary principle, we must address every potentially important pathway to slow the spread of COVID-19. The measures that should be taken to mitigate airborne transmission risk include:
- •
Provide sufficient and effective ventilation (supply clean outdoor air, minimize recirculating air) particularly in public buildings, workplace environments, schools, hospitals, and aged care homes.
- •
Supplement general ventilation with airborne infection controls such as local exhaust, high efficiency air filtration, and germicidal ultraviolet lights.
- •
Avoid overcrowding, particularly in public transport and public buildings.
Such measures are practical and often can be easily implemented; many are not costly. For example, simple steps such as opening both doors and windows can dramatically increase air flow rates in many buildings. For mechanical systems, organizations such as ASHRAE (the American Society of Heating, Ventilating, and Air-Conditioning Engineers) and REHVA (the Federation of European Heating, Ventilation and Air Conditioning Associations) have already provided guidelines based on the existing evidence of airborne transmission. The measures that we propose offer more benefits than potential downsides, even if they can only be partially implemented.
It is understood that there is not as yet universal acceptance of airborne transmission of SARS-CoV2; but in our collective assessment there is more than enough supporting evidence so that the precautionary principle should apply. In order to control the pandemic, pending the availability of a vaccine, all routes of transmission must be interrupted.
We are concerned that the lack of recognition of the risk of airborne transmission of COVID-19 and the lack of clear recommendations on the control measures against the airborne virus will have significant consequences: people may think that they are fully protected by adhering to the current recommendations, but in fact, additional airborne interventions are needed for further reduction of infection risk.
This matter is of heightened significance now, when countries are reopening following lockdowns: bringing people back to workplaces and students back to schools, colleges, and universities. We hope that our statement will raise awareness that airborne transmission of COVID-19 is a real risk and that control measures, as outlined above, must be added to the other precautions taken, to reduce the severity of the pandemic and save lives.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgment. Together with the authors, 239 scientists support this Commentary, and their affiliations and contact details are listed in the Supplementary Data.
The following scientists contributed to formulating this commentary. Linsey C. Marr, William Bahnfleth, Jose-Luis Jimenez, Yuguo Li, William W. Nazaroff, Catherine Noakes, Chandra Sekhar, Julian Wei-Tze Tang, Raymond Tellier, Philomena M. Bluyssen, Atze Boerstra, Giorgio Buonanno, Junji Cao, Stephanie J. Dancer, Francesco Franchimon, Charles Haworth, Jaap Hogeling, Christina Isaxon, Jarek Kurnitski, Marcel Loomans, Guy B. Marks, Livio Mazzarella, Arsen Krikor Melikov, Shelly Miller, Peter V. Nielsen, Jordan Peccia, Xavier Querol, Olli Seppänen, Shin-ichi Tanabe, Kwok Wai Tham, Pawel Wargocki, Aneta Wierzbicka, Maosheng Yao.
The following scientists reviewed the document. Jonathan Abbatt, John Adgate, Alireza Afshari, Kang-Ho Ahn, Francis Allard, Joseph Allen, Celia Alves, Meinrat O. Andreae, Isabella Annesi-Maesano, Ahmet Arısoy, Andrew P. Ault, Gwi-Nam Bae, Gabriel Bekö, Scott C. Bell, Allan Bertram, Mahmood Bhutta, Seweryn Bialasiewicz, Merete Bilde, Tami Bond, Joseph Brain, Marianna Brodach, David M. Broday, Guangyu Cao, Christopher D. Cappa, Annmarie Carlton, Paul K. S. Chan, Christopher Chao, Kuan-Fu Chen, Qi Chen, Qingyan Chen, David Cheong, Per Axcel Clausen, Ross Crawford, Derek Clements-Croome, Geo Clausen, Ian Clifton, Richard L. Corsi, Benjamin J. Cowling, Francesca Romana d’Ambrosio, Ghassan Dbaibo, Richard de Dear, Gianluigi de Gennaro, Peter DeCarlo, Philip Demokritou, Hugo Destaillats, Joanna Domagala-Kulawik, Neil M. Donahue, Caroline Duchaine, Marzenna R. Dudzinska, Dominic E. Dwyer, Greg Evans, Delphine K. Farmer, Kevin P. Fennelly, Richard Flagan, Janine Fröhlich-Nowoisky, Manuel Gameiro da Silva, Christian George, Marianne Glasius, Allen H. Goldstein, João Gomes, Michael Gormley, Rafal Górny, David Grimsrud, Keith Grimwood, Charles N. Haas, Fariborz Haghighat, Michael Hannigan, Roy Harrison, Ulla Haverinen-Shaughnessy, Philippa Howden-Chapman, Per Heiselberg, Daven K. Henze, Jean-Michel Heraud, Hartmut Herrmann, Philip K. Hopke, Ray Horstman, Wei Huang, Alex Huffman, David S. Hui, Tareq Hussein, Gabriel Isaacman-VanWertz, Jouni J.K. Jaakkola, Matti Jantunen, Lance Jennings, Dennis Johansson, Jan Kaczmarczyk, George Kallos, David Katoshevski, Frank Kelly, Søren Kjærgaard, Luke D. Knibbs, Henrik N. Knudsen, GwangPyo Ko, Evelyn S.C. Koay, Jen Kok, Nino Kuenzli, Markku Kulmala, Kazukiyo Kumagai, Prashant Kumar, Kazumichi Kuroda, Kiyoung Lee, Nelson Lee, Barry Lefer, Vincent Lemort, Xianting Li, Dusan Licina, Chao-Hsin Lin, Junjie Liu, Kam Lun E. Hon, John C. Little, Li Liu, Janet M. Macher, Ebba Malmqvist, Corinne Mandin, Ivo Martinac, Dainius Martuzevičius, Mark J. Mendell, David Miller, Claudia Mohr, Luisa T. Molina, Glenn Morrison, Roya Mortazavi, Edward Nardell, Athanasios Nenes, Mark Nicas, Zhi Ning, Jianlei Niu, Hidekazu Nishimura, Colin O’Dowd, Bjarne W. Olesen, Paula J. Olsiewski, Spyros Pandis, Daniel Peckham, Tuukka Petäjä, Zbigniew Popiolek, Ulrich Pöschl, Wayne R. Ott, Kimberly Prather, Andre S. H. Prevot, Hua Qian, Shanna Ratnesar-Shumate, James L. Repace, Tiina Reponen, Ilona Riipinen, Susan Roaf, Allen L. Robinson, Yinon Rudich, Manuel Ruiz de Adana, Masayuki Saijo, Reiko Saito, Paulo Saldiva, Tunga Salthammer, Joshua L. Santarpia, John H. Seinfeld, Gary S. Settles, Siegfried Schobesberger, Paul T. J. Scheepers, Max H. Sherman, Alan Shihadeh, Manabu Shiraiwa, Jeffrey Siegel, Torben Sigsgaard, Brett C. Singer, James N. Smith, Armin Sorooshian, Jerzy Sowa, Brent Stephens, Huey-Jen Jenny Su, Jordi Sunyer, Jason D. Surratt, Kazuo Takahashi, Nobuyuki Takegawa, Jørn Toftum, Margaret A. Tolbert, Euan Tovey, Barbara J. Turpin, Annele Virtanen, John Volckens, Claire Wainwright, Lance A. Wallace, Boguang Wang, Chia C. Wang, Michael Waring, John Wenger, Charles J. Weschler, Brent Williams, Mary E. Wilson, Armin Wisthaler, Kazimierz Wojtas, Douglas R. Worsnop, Ying Xu, Naomichi Yamamoto, Xudong Yang, Hui-Ling Yen, Hiroshi Yoshino, Hassan Zaraket, Zhiqiang (John) Zhai, Junfeng (Jim) Zhang, Qi Zhang, Jensen Zhang, Yinping Zhang, Bin Zhao, Tong Zhu.
Disclaimer. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any agency/institution.
Potential conflicts of interest. The authors: No reported conflicts of interest. Both authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.




Comments