-
PDF
- Split View
-
Views
-
Cite
Cite
Guilherme Pessoa-Amorim, Christian F Camm, Parag Gajendragadkar, Giovanni Luigi De Maria, Celine Arsac, Cecile Laroche, José Luis Zamorano, Franz Weidinger, Stephan Achenbach, Aldo P Maggioni, Chris P Gale, Athena Poppas, Barbara Casadei, Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology, European Heart Journal - Quality of Care and Clinical Outcomes, Volume 6, Issue 3, July 2020, Pages 210–216, https://doi.org/10.1093/ehjqcco/qcaa046
Close - Share Icon Share
Abstract
The COVID-19 pandemic required a significant redeployment of worldwide healthcare resources. Fear of infection, national lockdowns and altered healthcare priorities have the potential to impact utilisation of healthcare resources for non-communicable diseases. To survey health professionals’ views of the impact of the COVID-19 pandemic on the rate and timing of admission of patients with ST-elevation myocardial infarction (STEMI), the European Society of Cardiology (ESC) administered an internet-based questionnaire to cardiologists and cardiovascular nurses across 6 continents.
3101 responses were received from 141 countries across 6 continents. 88.3% responded that their country was in “total lockdown” and 7.1% in partial lockdown. 78.8% responded that the number of patients presenting with STEMI was reduced since the coronavirus outbreak and 65.2% indicated that the reduction in STEMI presentations was >40%. Approximately 60% of all respondents reported that STEMI patients presented later than usual and 58.5% that >40% of STEMI patients admitted to hospital presented beyond the optimal window for primary percutaneous intervention (PCI) or thrombolysis. Independent predictors of the reported higher rate of delayed STEMI presentation were a country in total lockdown, >100 COVID-19 cases admitted locally, and the complete restructuring of the local cardiology service.
The survey indicates that the impact of COVID-19 on STEMI presentations is likely to be substantial, with both lower presentations and a higher rate of delayed presentations occurring. This has potentially important ramifications for future healthcare and policy planning in the event of further waves of this pandemic.
Introduction
COVID-19, caused by the SARS-CoV2 virus, is a highly contagious condition, which may lead to severe respiratory failure and premature mortality.1 The present pandemic has required the rapid redeployment and mobilization of substantial healthcare resources worldwide,2 along with widespread ‘lockdown’, with estimates suggesting that by April over a third of the global population was under some form of restrictive measure.3 Over the same time, a reduction in hospital admissions for acute non-communicable conditions, such as myocardial infarction and stroke, has been reported in several countries.4–11
Globally, cardiovascular disease (CVD) remains the primary cause of death claiming the lives of 17.9 million people every year; of these deaths, 85% are due to heart attack and stroke and ∼38% are premature (below the age of 70).12–14 Whilst global healthcare delivery and policy are currently focused on the COVID-19 pandemic, we must not forget that other serious conditions, such as acute coronary syndromes (ACS)—for which we can deploy life-saving evidence-based treatments—not only continue to exist but may even increase in prevalence during an infectious disease pandemic.15
Here we present the results of a survey conducted by the ESC probing the perception of cardiologists and cardiovascular nurses with regards to ST-elevation myocardial infarction (STEMI) admissions to their hospitals.
Methods
An electronic questionnaire was designed to capture the perception of cardiologists and nurses with regards to the change in frequency (increase or decrease) and timing of STEMI admissions in their hospital or ward (Supplementary material online, Annex S1). The responders were also asked to self-report an estimate of the extent of any changes in STEMI admissions or delayed presentations according to predefined ranges, and to provide information on their place of work, presence of ‘lockdown’ in their country or region, concomitant number of COVID-19 admissions, and extent of COVID-19-related cardiology service restructuring (none, partial, total). The survey was in English and designed to be completed in <5 min (confirmed upon beta-testing in a sample of physicians whose mother tongue was not English).
A request to complete the questionnaire was sent to 186 000 ESC contacts (physicians and nurses). The first invitation was sent on 16 April 2020 and a reminder was emailed on 20 April 2020 to all contacts yet to click on the survey. The survey was closed on 26 April 2020.
Continuous variables were expressed as mean ± standard deviation (SD) or as median and interquartile range (IQR). Categorical variables were expressed as frequency and percentages.
A backward multivariable logistic regression analysis was performed to evaluate characteristics of respondents reporting STEMI patients presenting later than usual and outside of the optimal window for reperfusion (i.e. to explore possible local characteristics), including into the model all candidate variables (variables with P < 0.10 in univariate regression). A significance level of P < 0.05 was required for a variable to be retained in the model. To verify that the models were optimal, Hosmer and Lemeshow Goodness-of-Fit test and per cent concordance were calculated. A two-sided P < 0.05 was considered statistically significant. All analyses were performed using SAS statistical software version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
In total, there were 3101 responders to the questionnaire (1.7%) from 141 countries and 6 continents. Among the responders, 1800 (58.0%) were from Europe, 734 (23.7%) from Asia, 219 (7.1%) from South America, 163 (5.3%) from North America, 147 (4.7%) from Africa, and 38 (1.2%) from Oceania. Among the European responders, 45.7% were from Southern Europe, 18.8% from Western Europe, 18.7% from Northern Europe, and 16.8% from Eastern Europe. Data for the four European regions are reported in the Supplementary material online, Annex S2.
56.3% of responders defined themselves as ‘cardiologists’ and 33.6% as ‘interventional cardiologists’, the remaining 10.1% were nurses and population scientists. In Asia and North America, the proportion of responders identifying themselves as ‘interventional cardiologists’ was higher at 42.2% and 45.6%, respectively. 47.0% of respondents stated that they worked in a University Hospital, 35.8% in a district/regional or local hospital, and 17.2% in a private hospital. These proportions were similar across continents except in South America where 47.5% of responders worked in a private hospital.
Overall, 88.3% responded that their country was in ‘total lockdown’ (as defined by the closure of most shops, restaurants, etc., and the advice to work from home) and 7.1% in partial lockdown. The proportion of responders who said their country/region was in ‘total lockdown’ was highest in Europe (94.7%) and lowest in Africa (69.2%).
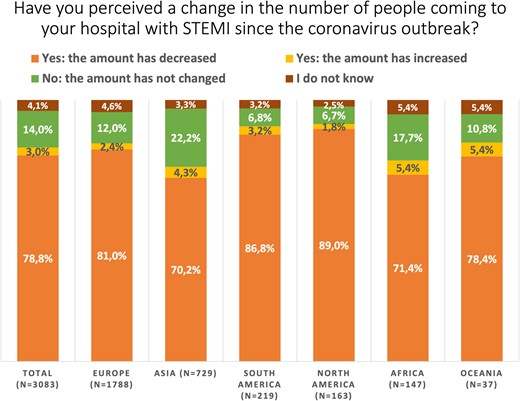
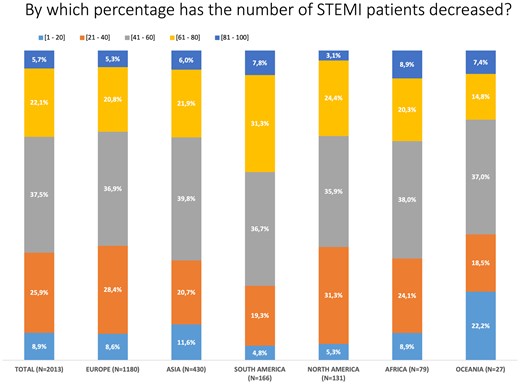
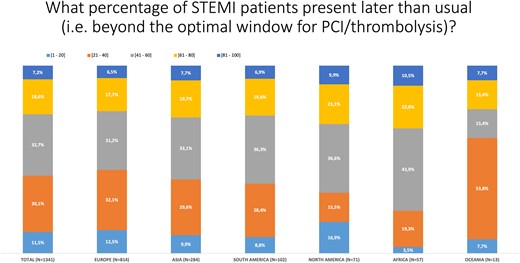
Overall, there was a perception that the number of admissions of patients with STEMI was substantially reduced (Figure 1) with 65.2% of those who reported a reduction indicating that it was >40% (Figure 2). Similarly, 62.2% of all respondents reported that patients with STEMI were admitted to hospital later than usual since the beginning of the COVID-19 outbreak; indeed, 58.5% of responders felt that the proportion of STEMI patients who presented beyond the optimal window for percutaneous coronary intervention or thrombolysis was >40% (Figure 3).
Distribution of responses overall and for each continent for those respondents who reported a lower number of ST-elevation myocardial infarction presentations since the COVID-19 outbreak.
Only 3.0% of responders reported an increase in STEMI admissions since the beginning of the COVID-19 outbreak; health anxiety and a true increase in the incidence of ACS during the pandemic were thought to be the most common reasons.
The extent of restructuring of cardiology wards, units, or departments varied across continents—no restructuring was most common in Africa (58.4%) and least common in Oceania (14.3%); however, the number of responders from these regions was the lowest. Overall, 31.8% reported no change, 54.9% a partial restructuring, and 13.3% a total restructuring.
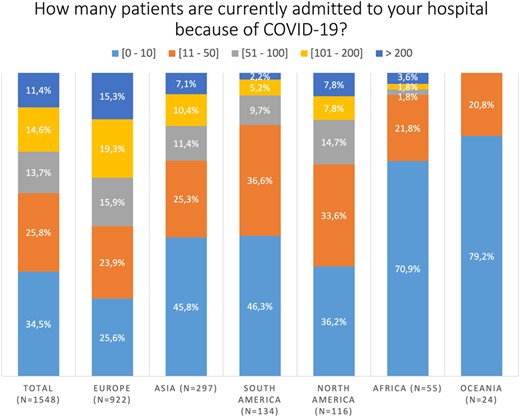
The proportion of responders reporting more than 200 COVID-19 patients admitted to their hospitals was highest in Europe (15.3%) and lowest in Oceania (0.0%) (Figure 4). Overall, about a quarter of the responders reported that there were more than 100 COVID-19 patients admitted to their hospitals.
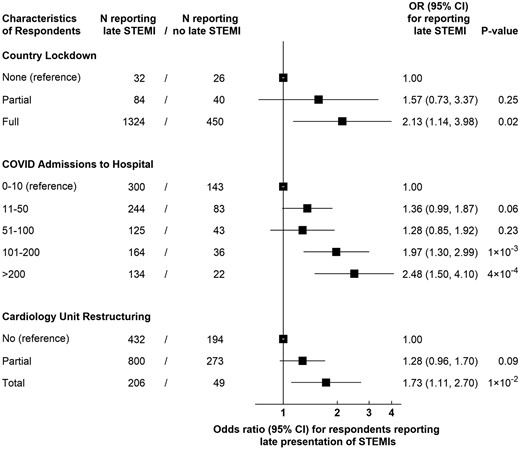
In multivariable analysis, respondents reporting late presentation of STEMI patients outside of the optimal reperfusion window (compared with those who did not) were more likely to be from a country with a total lockdown and working in a hospital with more than 100 COVID-related admissions and with restructured cardiology services (Figure 5).
National and hospital factors associated with a higher likelihood to report delays in ST-elevation myocardial infarction admissions.
Discussion
This international survey provides important insights on the impact of the COVID-19 pandemic on hospital admissions for a life-threatening cardiovascular emergency, such as STEMI, as reported by cardiologists (38% interventional) and cardiovascular nurses. The responses showed that most (∼80%) health professionals felt there had been a decrease in STEMI presentations, with the large majority of survey participants reporting at least a 40% reduction. These findings were largely consistent across six continents and, although based on self-reported perceptions, they are supported by objective evidence from European and the US registries suggesting a 25–40% average reduction in STEMI presentations during the COVID-19 outbreak. 4–8,11
Participants of this survey also reported an increase in time taken for those with STEMI to reach the hospital. This is similarly in keeping with data from Hong Kong showing an increased median time from onset of symptoms to ambulance arrival in STEMI patients from 82.5 to 318 min during the pandemic.16 Our multiple logistic regression model identified full country lockdown, higher numbers of COVID-19 patients in the hospital, and total cardiology unit restructuring as independent predictors of perceived late STEMI presentation. It is conceivable that STEMI patients in areas with high surges of COVID-19 cases and stricter lockdown enforcement may present later both because of changes in patient behaviour and perception of risk, and as a result of an increased demand on the ambulance service.17
The extent of restructuring of cardiology services was substantial, with two-thirds reporting at least some change in service setup. However, the extent varied between respondents suggesting heterogeneity in approaches to this pandemic. Importantly, the degree of this restructuring did not correlate with the number of admitted COVID-19 patients, suggesting it was driven by the desire to prepare for a possible surge of COVID-19 patients as well as by the actual need to front the increase in demand. However, the determinants of the extent of restructuring at a local or regional level cannot be inferred from the results of this survey.
It has been suggested that a state of lockdown might reduce triggers for acute decompensation, such as lower air pollution, lower commuting stress, or reduced exercise.18 However, these effects may be counterbalanced by the impact of additional psychological stress from social distancing, disruption of usual routine, fear of unemployment and uncertainty regarding the immediate and long-term future. Furthermore, individuals may not be presenting to emergency departments due to fear of acquiring COVID-19 whilst in hospital. In surveys undertaken by the Irish Cardiac Society (http://www.irishcardiacsociety.com/documents/618_PReleaseCovid-19.pdf) and the British Heart Foundation (https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2020/april/drop-in-heart-attack-patients-amidst-coronavirus-outbreak), fear of being exposed to COVID-19 was the reason mostly frequently reported for the decrease in ACS admissions, followed by worries of burdening the healthcare system, and patients not leaving their homes due to government restrictions. It has also been suggested that sensory neuropathy, already known to cause anosmia and ageusia in some COVID-19 patients,19 may reduce pain perception and thus the seeking of medical help. However, similar reductions in acute admissions have been reported for stroke9,10 (https://eso-stroke.org/likely-increase-in-the-risk-of-death-or-disability-from-stroke-during-the-covid-19 pandemic/), which is less dependent on pain perception, further suggesting behavioural changes, largely driven by fear of contracting an infectious disease that has caused the greater number of fatalities in elderly patients with a history of CVD, as the main reason underlying the observed trends.
Several limitations to this work need to be considered. The response rate to the survey was 1.7% and most of the responders (81.7%) were from Europe or Asia. Whilst we cannot be sure that the views of a minority will be representative of that of all cardiologists and nurses working in six continents nor exclude that health professionals witnessing the largest fall in ACS admission would be more likely to be responders, the results of the survey are in remarkable agreement with the findings of registries worldwide.4–8,11
The impact of reduced STEMI admissions and delayed presentations on mortality is difficult to quantify but likely to be substantial. Non-COVID-19 mortality has been shown to be higher during the coronavirus outbreak20; furthermore, it is conceivable that an excess of ACS may have been triggered by the infection, as it has been reported during seasonal influenza outbreaks15 leading to underestimation of the proportion of ACS patients who did not present to hospital and thus, of the actual impact of the pandemic on ischaemic deaths. Recently published data from the USA indicate that those who presented to hospital with ACS from 4 March to 14 April 2020 were less likely to have a history of ischaemic heart disease or a previous myocardial infarction compared with the 2019 ACS admissions over the same period,11 implying that those with the highest mortality risk for STEMI have been the least likely to seek help. As it has been widely reported that COVID-19 fatality rate is highest in elderly men with a history of ischaemic heart disease, their reluctance to come to hospital for fear of becoming infected is not surprising. It could be speculated that the large number of COVID-19 deaths amongst older males at a high risk of STEMI, may have contributed to the observed reduction in new STEMI admissions. However, at least in the USA, there was no indication that the age or gender distribution of STEMI patients differed during the coronavirus outbreak.11
In conclusion, the COVID-19 pandemic has impacted on the rate and timing of hospital admissions for ACS to an extent that would have been unimaginable just a few months ago. In the ESC survey, a large reduction in STEMI presentations has occurred on a background of significant restructuring of cardiology departments to deal with the COVID-19 pandemic. These self-reported perceptions are largely in line with registry data and suggest that the indirect adverse impact of COVID-19 on those with new or established cardiac disease or other non-communicable conditions is likely to be extensive.
Taken together, these observations must be taken into serious consideration in the event that a second pandemic wave develops as lockdown restrictions are eased worldwide. Medical societies, heart foundations, and governments have a responsibility to develop strategies to inform patients of the importance of seeking appropriate care, but also to ensure that a safe environment is provided for patients who are admitted to hospital because of a cardiovascular emergency. Lack of assurance on this front is likely to underpin our findings and to lead to unnecessary death and disability.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Supplementary material
Supplementary material is available at European Heart Journal – Quality of Care and Clinical Outcomes online.
Acknowledgements
We are indebted to all health professionals who took time from their busy schedule to fill in the ESC questionnaire.
Funding
B.C. is in receipt of a personal chair from the British Heart Foundation (CH/12/3/29609).
Conflict of interest: B.C. is the current President and SA the President-Elect of the European Society of Cardiology (ESC). A.P. is the President of the American College of Cardiology. J.L.Z. and F.W. are ESC Vice-Presidents for National Cardiac Societies. C.G. is the chair of the ESC EURObservational Research Programme. B.C. has received in-kind research support by Roche Diagnostics and iRhythm unrelated to this work. A.P.M. reports personal fees from Bayer, Fresenius, and Novartis unrelated to this work. All other authors declare none.
References
World Economic Forum. Nearly 3 billion people around the globe under COVID-19 lockdown—today’s coronavirus updates. https://www.weforum.org/agenda/2020/03/todays-coronavirus-updates/ (21 May 2020).
Atlas Writing Group, Esc Atlas of Cardiology is a compendium of cardiovascular statistics compiled by the European Heart Agency adotESoC, Developed in collaboration with the national societies of the European Society of Cardiology member countries,
GBD 2017 Causes of Death Collaborators.
World Health Organization. WHO cardiovascular disease factsheet. https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases (12 May