-
PDF
- Split View
-
Views
-
Cite
Cite
Massimo F Piepoli, Arno W Hoes, Stefan Agewall, Christian Albus, Carlos Brotons, Alberico L Catapano, Marie-Therese Cooney, Ugo Corrà, Bernard Cosyns, Christi Deaton, Ian Graham, Michael Stephen Hall, F D Richard Hobbs, Maja-Lisa Løchen, Herbert Löllgen, Pedro Marques-Vidal, Joep Perk, Eva Prescott, Josep Redon, Dimitrios J Richter, Naveed Sattar, Yvo Smulders, Monica Tiberi, H Bart van der Worp, Ineke van Dis, W M Monique Verschuren, Simone Binno, ESC Scientific Document Group , 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)
Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR), European Heart Journal, Volume 37, Issue 29, 1 August 2016, Pages 2315–2381, https://doi.org/10.1093/eurheartj/ehw106Close - Share Icon Share
Abbreviations and acronyms
- ABI
ankle–brachial (blood pressure) index
- ABPM
ambulatory blood pressure monitoring
- ACCORD
Action to Control Cardiovascular Risk in Diabetes
- ACE-I
angiotensin-converting enzyme inhibitor
- ACS
acute coronary syndromes
- ADVANCE
Action in Diabetes and Vascular disease: PreterAx and Diamicron MR Controlled Evaluation
- AF
atrial fibrillation
- AMI
acute myocardial infarction
- apoA1
apolipoprotein A1
- apoB
apolipoprotein B
- ARB
angiotensin receptor blocker
- BEUC
Bureau Européen des Unions de Consommateurs
- BMI
body mass index (weight (kg)/height (m2))
- BP
blood pressure
- CAC
coronary artery calcium
- CAD
coronary artery disease
- CAPRIE
Clopidogrel versus Aspirin in Patients at Risk for Ischaemic Events
- CARDS
Collaborative Atorvastatin Diabetes Study
- CHANCE
Clopidogrel in High-risk patients with Acute Non-disabling Cerebrovascular Events
- CHARISMA
Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilisation, Management, and Avoidance
- CI
confidence interval
- CKD
chronic kidney disease
- CR
cardiac rehabilitation
- CT
computed tomography
- CTT
Cholesterol Treatment Trialists' Collaboration
- CURE
Clopidogrel vs. Placebo in Patients with ACS without ST-segment elevation
- CV
cardiovascular
- CVD
cardiovascular disease
- DALYs
disability-adjusted life years
- DASH
Dietary Approaches to Stop Hypertension
- DBP
diastolic blood pressure
- DCCT
Diabetes Control and Complications Trial
- DHA
docosahexaenoic acid
- DM
diabetes mellitus
- DPP-4
dipeptidyl peptidase-4
- eGFR
estimated glomerular filtration rate
- ECDA
European Chronic Disease Alliance
- ECG
electrocardiogram
- ED
erectile dysfunction
- EHN
European Heart Network
- EMA
European Medicines Agency
- EPA
eicosapentaenoic acid
- EPIC
European Prospective Investigation into Cancer and Nutrition
- EPODE
Ensemble Prévenons l'Obésité des Enfants
- ESC
European Society of Cardiology
- EU
European Union
- FDA
Food and Drug Administration (USA)
- FDC
fixed dose combination
- FH
familial hypercholesterolaemia
- GLP-1
glucagon-like peptide 1
- GP
general practitioner
- GOSPEL
Global Secondary Prevention Strategies to Limit Event Recurrence After Myocardial Infarction
- HbA1c
glycated haemoglobin
- HBPM
home blood pressure measurements
- HDL-C
high-density lipoprotein cholesterol
- HF
heart failure
- HF-ACTION
Heart Failure: A Controlled Trial Investigating Outcomes of Exercise Training
- HOPE
Heart Outcomes Prevention Evaluation
- HPS
Heart Protection Study
- HRQoL
health-related quality of life
- HR
heart rate
- hsCRP
high-sensitivity C-reactive protein
- HYVET
Hypertension in the Very Elderly Trial
- ICD
International Classification of Diseases
- IMT
intima–media thickness
- INVEST
International Verapamil-Trandolapril Study
- LDL-C
low-density lipoprotein cholesterol
- Lp(a)
lipoprotein(a)
- LV
left ventricle/left ventricular
- LVH
left ventricular hypertrophy
- MET
metabolic equivalent
- MHO
metabolically healthy overweight/obesity
- MI
myocardial infarction
- MUFA
monounsaturated fatty acids
- NGO
non-governmental organization
- NHS
National Health Service (UK)
- NICE
National Institute for Health and Care Excellence
- NNT
number needed to treat
- NRI
net reclassification index
- NRT
nicotine replacement therapy
- OASIS
Organization to Assess Strategies in Acute Ischemic Syndromes
- ONTARGET
ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial
- OSAS
obstructive sleep apnoea syndrome
- OR
odds ratio
- PA
physical activity
- PAD
peripheral artery disease
- PLATO
Ticagrelor vs. Clopidogrel in Patients with ACS with and without ST-segment elevation
- PCOS
polycystic ovary syndrome
- PCSK9
proprotein convertase subtilisin/kexin type 9
- PROactive
Prospective Pioglitazone Clinical Trial in Macrovascular Events
- PROGRESS
Perindopril Protection Against Recurrent Stroke Study
- PROCAM
Prospective Cardiovascular Munster Study
- PWV
pulse wave velocity
- RA
rheumatoid arthritis
- RCT
randomized controlled trial
- RESPONSE
Randomised Evaluation of Secondary Prevention by Outpatient Nurse Specialists
- RM
repetition maximum
- ROS
reactive oxygen species
- RPE
rating of perceived exertion
- RR
relative risk
- SAVOR-TIMI 53
Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus – Trombolysis in Myocardial Infarction
- SBP
systolic blood pressure
- SGLT2
sodium-glucose co-transporter 2
- SNP
single nucleotide polymorphism
- SCORE
Systematic Coronary Risk Estimation
- SPARCL
Stroke Prevention by Aggressive Reduction in Cholesterol Levels
- TIA
transient ischaemic attack
- TRITON
Prasugrel vs. Clopidogrel in Patients with ACS
- UKPDS
United Kingdom Prospective Diabetes Study
- VADT
Veterans Affairs Diabetes Trial
- VALUE
Valsartan Antihypertensive Long-Term Use Evaluation
- VLDL
very low-density lipoprotein
- V̇O2
oxygen uptake
- WHO
World Health Organization
1. What is cardiovascular disease prevention?
1.1 Definition and rationale
Cardiovascular disease (CVD) prevention is defined as a coordinated set ofactions, at the population level or targeted at an individual, that are aimed ateliminating or minimizing the impact of CVDs and their relateddisabilities.1CVD remains a leading cause of morbidity and mortality, despite improvements inoutcomes. Age-adjusted coronary artery disease (CAD) mortality has declinedsince the 1980s, particularly in high-income regions.2 CAD rates are now less than half what theywere in the early 1980s in many countries in Europe, due to preventive measuresincluding the success of smoking legislation. However, inequalities betweencountries persist and many risk factors, particularly obesity3 and diabetes mellitus(DM),4 have beenincreasing substantially. If prevention was practised as instructed it wouldmarkedly reduce the prevalence of CVD. It is thus not only prevailing riskfactors that are of concern, but poor implementation of preventive measures aswell.5,6 Prevention should bedelivered (i) at the general population level by promoting healthy lifestylebehaviour7 and(ii) at the individual level, i.e. in those subjects at moderate to high risk ofCVD or patients with established CVD, by tackling unhealthy lifestyles (e.g.poor-quality diet, physical inactivity, smoking) and by optimising risk factors.Prevention is effective: the elimination of health risk behaviours would make itpossible to prevent at least 80% of CVDs and even 40% of cancers.8,9
1.2 Development of the 6th Joint Task Force guidelines
The present guidelines represent an evidence-based consensus of the 6th EuropeanJoint Task Force involving 10 professional societies.
By appraising the current evidence and identifying remaining knowledge gaps inmanaging CVD prevention, the Task Force formulated recommendations to guideactions to prevent CVD in clinical practice. The Task Force followed the qualitycriteria for development of guidelines, which can be found at http://www.escardio.org/Guidelines-&-Education/Clinical-Practice-Guidelines/Guidelines-development/Writing-ESC-Guidelines.For simplification and in keeping with other European Society of Cardiology(ESC) guidelines, the ESC grading system based on classes of recommendation andlevels of evidence has been maintained, recognising that this may be lesssuitable to measure the impact of prevention strategies, particularly thoserelated to behavioural issues and population-based interventions.
This document has been developed to support healthcare professionalscommunicating with individuals about their cardiovascular (CV) risk and thebenefits of a healthy lifestyle and early modification of their CV risk. Inaddition, the guidelines provide tools for healthcare professionals to promotepopulation-based strategies and integrate these into national or regionalprevention frameworks and to translate these in locally delivered healthcareservices, in line with the recommendations of the World Health Organization(WHO) global status report on non-communicable diseases 2010.10
As in the present guidelines, the model presented in the previous document fromthe Fifth European Joint Task Force11 has been structured around four core questions: (i)What is CVD prevention? (ii) Who will benefit from prevention? (iii) How tointervene? (iv) Where to intervene?
Compared with the previous guidelines, greater emphasis has been placed on apopulation-based approach, on disease-specific interventions and onfemale-specific conditions, younger individuals and ethnic minorities. Due tospace restrictions for the paper version, the chapter on disease-specificintervention is on the web, together with a few tables and figures (for moredetail see web addenda).
A lifetime approach to CV risk is important since both CV risk and prevention aredynamic and continuous as patients age and/or accumulate co-morbidities. Thisimplies that, apart from improving lifestyle and reducing risk factor levels inpatients with established CVD and those at increased risk of developing CVD,healthy people of all ages should be encouraged to adopt a healthy lifestyle.Healthcare professionals play an important role in achieving this in theirclinical practice.
1.3 Cost-effectiveness of prevention
Key messages
Prevention of CVD, either by implementation of lifestyle changes or useof medication, is cost effective in many scenarios, includingpopulation-based approaches and actions directed at high-riskindividuals.
Cost-effectiveness depends on several factors, including baseline CVrisk, cost of drugs or other interventions, reimbursement procedures andimplementation of preventive strategies.
Recommendation for cost-effective prevention of cardiovasculardisease
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendation for cost-effective prevention of cardiovasculardisease
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
In 2009, costs related to CVD amounted to €106 billion, representing ∼9% of thetotal healthcare expenditure across the European Union (EU).14 Thus, CVD represents aconsiderable economic burden to society and effective preventive measures arenecessary. There is consensus in favour of an approach combining strategies toimprove CV health across the population at large from childhood onward, withspecific actions to improve CV health in individuals at increased risk of CVD orwith established CVD.
Most studies assessing the cost-effectiveness of CVD prevention combine evidencefrom clinical research with simulation approaches, while cost-effectiveness datafrom randomized controlled trials (RCTs) are relatively scarce.15,16 Cost-effectiveness strongly depends onparameters such as the target population's age, the overall population risk ofCVD and the cost of interventions. Hence, results obtained in one country maynot be valid in another. Furthermore, changes such as the introduction ofgeneric drugs can considerably change cost-effectiveness.17 According to the WHO,policy and environmental changes could reduce CVD in all countries for less thanUS$1/person/year.18 A report from the National Institute for Health and CareExcellence (NICE) estimated that a UK national programme reducing population CVrisk by 1% would prevent 25 000 CVD cases and generate savings of €40million/year. CAD mortality rates could be halved by only modest risk factorreductions and it has been suggested that eight dietary priorities alone couldhalve CVD death.13
In the last three decades, more than half of the reduction in CV mortality hasbeen attributed to changes in risk factor levels in the population, primarilythe reduction in cholesterol and blood pressure (BP) levels and smoking. Thisfavourable trend is partly offset by an increase in other risk factors, mainlyobesity and type 2 DM.19,20 Aging of the populationalso increases CVD events.21
Several population interventions have efficiently modified the lifestyle ofindividuals. For example, increased awareness of how healthy lifestyles preventCVD has helped to reduce smoking and cholesterol levels. Lifestyle interventionsact on several CV risk factors and should be applied prior to or in conjunctionwith drug therapies. Also, legislation aimed at decreasing salt and the transfatty acid content of foods and smoking habits is cost effective in preventingCVD.12,13,19
Cholesterol lowering using statins15,16 andimprovement in BP control are cost effective if targeted at persons with high CVrisk.22Importantly, a sizable portion of patients on lipid-lowering or BP-lowering drugtreatment fails to take their treatment adequately or to reach therapeuticgoals,23,24 with clinical andeconomic consequences.
Gap in evidence
Most cost-effectiveness studies rely on simulation. More data, mainlyfrom RCTs, are needed.
2. Who will benefit from prevention? When and how to assess risk andprioritize
2.1 Estimation of total cardiovascular risk
All current guidelines on the prevention of CVD in clinical practice recommendthe assessment of total CVD risk since atherosclerosis is usually the product ofa number of risk factors. Prevention of CVD in an individual should be adaptedto his or her total CV risk: the higher the risk, the more intense the actionshould be.
The importance of total risk estimation in apparently healthy people beforemanagement decisions are made is illustrated in supplementary Figure A (see web addenda) and in Table 1 derived from the high-risk Systemic Coronary RiskEstimation (SCORE) chart (http://www.escardio.org/Guidelines-&-Education/Practice-tools/CVD-prevention-toolbox/SCORE-Risk-Charts).This shows that a person with a cholesterol level of 7 mmol/L can be at 10 timeslower risk than someone with a cholesterol level of 5 mmol/L if the former is afemale and the latter is a male hypertensive smoker.
Impact of combinations of risk factors on risk
 |
 |
CVD = cardiovascular disease; F = female; M = male; SBP = systolicblood pressure.
Impact of combinations of risk factors on risk
 |
 |
CVD = cardiovascular disease; F = female; M = male; SBP = systolicblood pressure.
A recent meta-analysis on CV risk reduction by treatment with BP-lowering drugsdoes, however, support the concept that absolute risk reduction is larger inthose individuals at higher baseline risk.25 This was confirmed in a furthermeta-analysis that also showed a greater residual risk during treatment in thoseat higher baseline risk, supporting earlier intervention.26,27
Although clinicians often ask for decisional thresholds to trigger intervention,this is problematic since risk is a continuum and there is no exact point abovewhich, for example, a drug is automatically indicated nor below which lifestyleadvice may not usefully be offered.
The risk categories presented later in this section are to assist the physicianin dealing with individual people. They acknowledge that although individuals atthe highest levels of risk gain most from risk factor interventions, most deathsin a community come from those at lower levels of risk, simply because they aremore numerous compared with high-risk individuals. Thus a strategy forindividuals at high risk must be complemented by public health measures toencourage a healthy lifestyle and to reduce population levels of CV riskfactors.
It is essential for clinicians to be able to assess CV risk rapidly and withsufficient accuracy. This realization led to the development of the risk chartused in the 1994 and 1998 Guidelines. This chart, developed from a conceptpioneered by Anderson,28used age, sex, smoking status, blood cholesterol and systolic BP (SBP) toestimate the 10- year risk of a first fatal or non-fatal CAD event. There wereseveral problems with this chart, which are outlined in the Fourth JointEuropean Guidelines on prevention.11,29 Thisled to the presently recommended SCORE system, estimating an individual's 10year risk of fatal CVD.30 The SCORE charts have been developed to estimate risk inboth high- and low-risk European populations; its applicability to non-Caucasianpopulations has not been examined.
2.2 When to assess total cardiovascular risk?
Recommendations for cardiovascular risk assessment
 |
 |
BP = blood pressure; CV = cardiovascular; CVD = cardiovasculardisease;
DM = diabetes mellitus.
aClass of recommendation.
bLevel of evidence.
Recommendations for cardiovascular risk assessment
 |
 |
BP = blood pressure; CV = cardiovascular; CVD = cardiovasculardisease;
DM = diabetes mellitus.
aClass of recommendation.
bLevel of evidence.
Screening is the identification of unrecognized disease or, in this case, of anunknown increased risk of CVD in individuals without symptoms. CV riskassessment or screening can be done opportunistically or systematically.Opportunistic screening means without a predefined strategy, but is done whenthe opportunity arises [e.g. when the individual is consulting his or hergeneral practitioner (GP) for some other reason]. Systematic screening can bedone in the general population as part of a screening programme or in targetedsubpopulations, such as subjects with a family history of premature CVD orfamilial hyperlipidaemia.
While the ideal scenario would be for all adults to have their risk assessed,this is not practical in many societies. The decision about who to screen mustbe made by individual countries and will be resource dependent.
In a meta-analysis, GP-based health checks on cholesterol, BP, body mass index(BMI) and smoking were effective in improving surrogate outcomes, especially inhigh-risk patients.31 Alarge study of CV risk assessment in the general population found that althoughthere were overall improvements in risk factors, there was no impact on CVoutcomes at the population level.32 A Cochrane review of RCTs using counselling oreducation to modify CV risk factors in adults from the general population,occupational groups or those with specific risk factors (i.e. DM, hypertension)concluded that risk factor improvements were modest and interventions did notreduce total or CV mortality in general populations, but reduced mortality inhigh-risk hypertensive and DM populations.33 Although the benefits of treatingasymptomatic conditions such as hypertension, DM and dyslipidaemia on morbidityand mortality outcomes have been documented, a Cochrane review of the existingtrials concluded that general health checks (including screening for theseconditions) do not reduce all-cause or CV morbidity or mortality.34 However, most studieswere performed three to four decades ago, and thus risk factor interventionswere not contemporary. Perhaps application of medical treatment in addition tothe lifestyle interventions that were the core component of most trials wouldimprove efficacy.
Most guidelines recommend a mixture of opportunistic and systematicscreening.11,35–38 Screeningin people at relatively low risk of CVD is not particularly effective inreducing the risk of CV events. The costs of such screening interventions arehigh and these resources may be better used in people at higher CV risk or withestablished CVD. In many countries, GPs have a unique role in identifyingindividuals at risk of but without established CVD and assessing theireligibility for intervention (see section 4a.1.1). A modelling study based onthe European Prospective Investigation of Cancer–Norfolk (EPIC-Norfolk) cohortdata concluded that, compared with the National Health Service (NHS) nationalstrategy to screen all adults 40–74 years of age for CV risk, inviting the 60%of the population at the highest risk according to an integrated risk score wasequally effective in preventing new cases of CVD and had potential costsavings.39
A general concern in screening, including CV risk assessment, is its potential todo harm. False positive results can cause unnecessary concern and medicaltreatment. Conversely, false negative results may lead to inappropriatereassurance and a lack of lifestyle changes. However, current data suggest thatparticipating in CV screening in general does not cause worry in those who arescreened.40–43 More research is needed on how certain subgroups,such as older people, the socially deprived and ethnic minorities, react toscreening.
Despite limited evidence, these guidelines recommend a systematic approach to CVrisk assessment targeting populations likely to be at higher CV risk, such asthose with a family history of premature CVD. Thus systematic CV risk assessmentin men <40 years of age and women <50 years of age with no known CV riskfactors is not recommended. Additionally, screening of specific groups with jobsthat place other people at risk, e.g. bus drivers and pilots, may be reasonable,as is screening for CV risk factors in women before prescribing combined oralcontraception, although there are no data to support the beneficial effects.Beyond this, systematic CV risk assessment in adults <40 years of age with noknown CV risk factors is not recommended as a main strategy due to the lowcost-effectiveness. Systematic CV assessment may be considered in adult men>40 years of age and in women >50 years of age or post-menopausal with noknown CV risk factors. Risk assessment is not a one-time event; it should berepeated, for example, every 5 years.
2.3 How to estimate total cardiovascular risk?
Key messages
In apparently healthy persons, CV risk in general is the result ofmultiple, interacting risk factors. This is the basis for the total CVrisk approach to prevention.
SCORE, which estimates the 10 year risk of fatal CVD, is recommended forrisk assessment and can assist in making logical management decisionsand may help to avoid both under- and overtreatment. Validated localrisk estimation systems are useful alternatives to SCORE.
Individuals automatically at high to very high CV risk(Table 5) do not need the use of a risk score and requireimmediate attention to risk factors.
In younger persons, a low absolute risk may conceal a very high relativerisk and use of the relative risk chart or calculation of their “riskage” may help in advising them of the need for intensive preventiveefforts.
While women are at lower CV risk than men, their risk is deferred by ∼10years rather than avoided.
The total risk approach allows flexibility; if perfection cannot beachieved with one risk factor, trying harder with others can stillreduce risk.
Recommendation for how to estimate cardiovascular risk
 |
 |
CV = cardiovascular; DM = diabetes mellitus; SCORE = SystematicCoronary Risk Estimation.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendation for how to estimate cardiovascular risk
 |
 |
CV = cardiovascular; DM = diabetes mellitus; SCORE = SystematicCoronary Risk Estimation.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
2.3.1 Ten-year cardiovascular risk
Many CV risk assessment systems are available for use in apparently healthyindividuals (Table 2), including Framingham,44 SCORE,30 ASSIGN (CV risk estimation modelfrom the Scottish Intercollegiate Guidelines Network),45 Q-Risk,46,47 PROCAM (Prospective CardiovascularMunster Study),48CUORE,49 thePooled Cohort equations,50 Arriba51 and Globorisk.52 In practice, most risk estimationsystems perform rather similarly when applied to populations recognizablycomparable to those from which the risk estimation system was derived. Since2003, the European Guidelines on CVD prevention in clinical practicerecommend use of the SCORE system, because it is based on large,representative European cohort datasets. The SCORE risk function has beenexternally validated.53
 |
 |
 |
 |
(continued)
 |
 |
ACC = American College of Cardiology; AHA = American HeartAssociation; ARIC = Atherosclerosis Risk in Communities; ATP =Adult Treatment Panel; BMI = body mass index; BP = bloodpressure; CAD = coronary artery disease; CARDIA = CoronaryArtery Risk Development in Young Adults; CHS = CardiovascularHealth Study; CVD = cardiovascular disease; DM = diabetesmellitus; HDL-C = high-density lipoprotein cholesterol; JBS =Joint British Societies; LDL-C = low-density lipoproteincholesterol; NCEP = National Cholesterol Education Program; NICE= National Institute for Health and Care Excellence; no. cigs =number of cigarettes; PROCAM = Prospective CardiovascularMunster Study; SBP = systolic blood pressure; SIGN = ScottishIntercollegiate Guidelines Network; SHHEC = Scottish HeartHealth Extended Cohort.
(continued)
 |
 |
ACC = American College of Cardiology; AHA = American HeartAssociation; ARIC = Atherosclerosis Risk in Communities; ATP =Adult Treatment Panel; BMI = body mass index; BP = bloodpressure; CAD = coronary artery disease; CARDIA = CoronaryArtery Risk Development in Young Adults; CHS = CardiovascularHealth Study; CVD = cardiovascular disease; DM = diabetesmellitus; HDL-C = high-density lipoprotein cholesterol; JBS =Joint British Societies; LDL-C = low-density lipoproteincholesterol; NCEP = National Cholesterol Education Program; NICE= National Institute for Health and Care Excellence; no. cigs =number of cigarettes; PROCAM = Prospective CardiovascularMunster Study; SBP = systolic blood pressure; SIGN = ScottishIntercollegiate Guidelines Network; SHHEC = Scottish HeartHealth Extended Cohort.
Table 3 liststhe advantages of the SCORE risk charts.
Advantages and limitations in using the SCORE risk charts
 |
 |
CVD = cardiovascular disease; SCORE = Systematic Coronary RiskEstimation.
Advantages and limitations in using the SCORE risk charts
 |
 |
CVD = cardiovascular disease; SCORE = Systematic Coronary RiskEstimation.
The SCORE system estimates the 10 year risk of a first fatalatherosclerotic event. All International Classification of Diseases (ICD)codes that could reasonably be assumed to be atherosclerotic are included,including CAD, stroke and aneurysm of the abdominal aorta. Traditionallymost systems estimated CAD risk only; however, more recently a number ofrisk estimation systems have changed to estimate the risk of allCVDs.44,47,50,58
The choice of CV mortality rather than total (fatal plus non-fatal) eventswas deliberate, although not universally popular. Non-fatal event rates arecritically dependent upon definitions and the methods used in theirascertainment. Critically, the use of mortality allows recalibration toallow for time trends in CV mortality. Any risk estimation system willoverpredict in countries in which mortality has fallen and underpredict inthose in which it has risen. Recalibration to allow for secular changes canbe undertaken if good quality, up-to-date mortality and risk factorprevalence data are available. Data quality does not permit this fornon-fatal events. For these reasons, the CV mortality charts were producedand have been recalibrated for a number of European countries.
Naturally, the risk of total fatal and non-fatal events is higher, andclinicians frequently ask for this to be quantified. The SCORE data indicatethat the total CV event risk is about three times higher than the risk offatal CVD for men, so that a SCORE risk of fatal CVD of 5% translates into afatal plus non-fatal CV risk of ∼15%; the multiplier is about four in womenand somewhat lower than three in older persons, in whom a first event ismore likely to be fatal.61
As noted in the introduction, thresholds to trigger certain interventions areproblematic since risk is a continuum and there is no threshold at which,for example, a drug is automatically indicated. Obviously, decisions onwhether treatment is initiated should also be based on patientpreferences.
A particular problem relates to young people with high levels of riskfactors, where a low absolute risk may conceal a very high relative riskrequiring intensive lifestyle advice. Several approaches to communicatingabout risk to younger people are presented below (refer also to section2.5.1). These include use of the relative risk chart or ‘risk age’ or‘lifetime risk’. The aim is to communicate that lifestyle changes can reducethe relative risk substantially as well as reduce the increase in risk thatoccurs with ageing.
Another problem relates to older people. In some age categories, the vastmajority, especially of men, will have estimated CV death risks exceedingthe 5–10% level, based on age (and gender) only, even when other CV riskfactor levels are low. This could lead to excessive use of drugs in theelderly. This issue is dealt with later (see section 2.3.5). It should benoted that RCT evidence to guide drug treatments in older persons is limited(refer to section 2.5.2).
The role of high-density lipoprotein cholesterol (HDL-C) in risk estimationhas been systematically re-examined using the SCORE database.62–64Overall HDL-C has a modest but useful effect in redefining riskestimation,63,64 butthis may not be seen in some low-risk populations.65 Assessing HDL-C is particularlyimportant at levels of risk just below the threshold for intensive riskmodification of 5%, where many of these subjects will qualify for intensiveadvice if their HDL-C is low.63 SCORE charts incorporating HDL-C are illustrated insupplementary FiguresB–I (see web addenda). In these charts, HDL-C is usedcategorically. The electronic version of SCORE, HeartScore (http://www.HeartScore.org),has been modified to take HDL-C into account on a continuous basis and istherefore more accurate.
The role of a plasma triglyceride as a predictor of CVD has been debated formany years. Fasting triglycerides relate to risk in univariable analyses,but the effect is attenuated by adjustment for other factors, especiallyHDL-C.66
Dealing with the impact of additional risk factors such as body weight,family history and newer risk markers is difficult within the constraint ofa paper chart. It should be stressed, however, that although many other riskfactors have been identified, their contribution is generally very modest toboth absolute CV risk estimations and in terms of reclassification of anindividual to another risk category67 (Table 4).
Examples of risk modifiers that are likely to have reclassificationpotential (see following sections for details)
 |
 |
ABI = ankle–brachial blood pressure index; BMI = body mass index;CVD = cardiovascular disease; CT = computed tomography.
Examples of risk modifiers that are likely to have reclassificationpotential (see following sections for details)
 |
 |
ABI = ankle–brachial blood pressure index; BMI = body mass index;CVD = cardiovascular disease; CT = computed tomography.
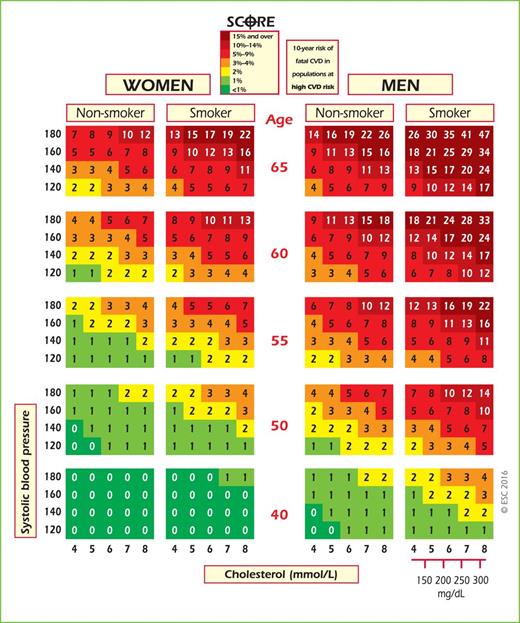
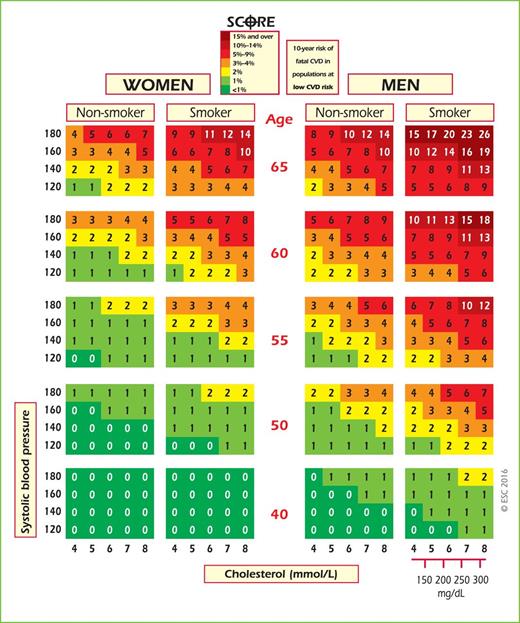
The SCORE risk charts are shown in Figures 1–4, including a chart ofrelative risks (Figure 3). Instructions on their use follow.
SCORE chart: 10-year risk of fatal cardiovascular disease inpopulations of countries at high cardiovascular risk based on thefollowing risk factors: age, sex, smoking, systolic blood pressure,total cholesterol. CVD = cardiovascular disease; SCORE = SystematicCoronary Risk Estimation.
SCORE chart: 10-year risk of fatal cardiovascular disease inpopulations of countries at low cardiovascular risk based on thefollowing risk factors: age, sex, smoking, systolic blood pressure,total cholesterol. CVD = cardiovascular disease; SCORE = SystematicCoronary Risk Estimation.
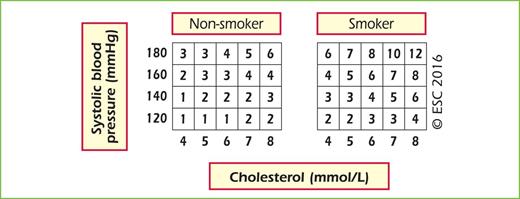
Relative risk chart, derived from SCORE Conversion of cholesterolmmol/L → mg/dL: 8 = 310; 7 = 270; 6 = 230; 5 = 190; 4 = 155.
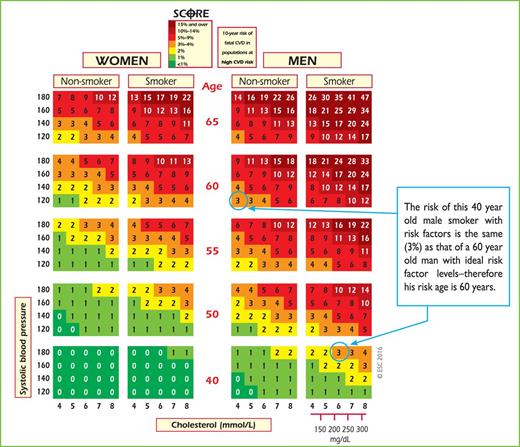
SCORE chart (for use in high-risk European countries) illustratinghow the approximate risk age can be read off the chart. SCORE =Systematic Coronary Risk Estimation.
Please note that Figure 3 shows relative not absolute risk. Thus a person inthe top right-hand box, with multiple CV risk factors, has a risk that is 12times greater than a person in the bottom left with normal risk factorlevels. This may be helpful when advising a young person with a low absolutebut high relative risk of the need for lifestyle change.
2.3.2 Cardiovascular risk age
The risk age of a person with several CV risk factors is the age of a personof the same gender with the same level of risk but with ideal levels of riskfactors. Thus a 40-year-old with high levels of some risk factors may havethe risk age of a 60-year-old (Figure 4), because the risk equals that of a60-year-old with ideal risk factor levels (i.e. non-smoking, totalcholesterol of 4 mmol/L and BP of 120 mmHg).68 Risk age is an intuitive and easilyunderstood way of illustrating the likely reduction in life expectancy thata young person with a low absolute but high relative risk of CVD will beexposed to if preventive measures are not adopted.68Table A showing different risk factor combinations isincluded in the web addenda to provide a more accurate estimation of riskages. Risk age is also automatically calculated as part of the latestrevision of HeartScore.
Risk age has been shown to be independent of the CV endpoint used,68 which bypasses thedilemma of whether to use a risk estimation system based on CV mortality oron total CV events. Risk age can be used in any population regardless ofbaseline risk and secular changes in mortality, and therefore avoids theneed for recalibration.69 At present, risk age is recommended to help communicateabout risk, especially to younger people with a low absolute risk but a highrelative risk.
2.3.3 Lifetime vs. 10-year cardiovascular risk estimation
Conventional CV risk prediction schemes estimate the 10 year risk of CVevents. Lifetime CV risk prediction models identify high-risk individualsboth in the short and long term. Such models account for predicted risk inthe context of competing risks from other diseases over the remainingexpected lifespan of an individual.
Notably, 10 year risk identifies individuals who are most likely to benefitfrom drug therapy in the near term. Drug treatment starts to work quiterapidly, and drug treatment can be largely informed by short-term risk, suchas 10 year risk. One problem with short-term risk is that it is mostlygoverned by age and consequently few younger individuals, in particularwomen, reach treatment thresholds. It has therefore been argued thatlifetime risk estimation may enhance risk communication, particularly amongyounger individuals and women.
Evidence for the role of lifetime risk in treatment decisions is lacking.Sufficient data for robust lifetime risk estimations, as well as meaningfulrisk categorization thresholds, are also lacking. Providing lifetime CV riskestimates for some groups at high risk of mortality due to competing non-CVDcauses can be difficult to interpret. Importantly, evidence of the benefitsof lifelong preventive therapy (e.g. BP- or lipid-lowering drugs) in youngerindividuals with low short-term but higher lifetime risks is lacking. Forthese reasons, we do not recommend that risk stratification for treatmentdecisions be based on lifetime risk. However, like risk age and relativerisk, it may be a useful tool in communicating about risk to individualswith high risk factor levels but who are at a low 10 year absolute risk ofCV events, such as some younger people. Whatever approach is used, ifabsolute risk is low, a high relative risk or risk age signals the need foractive lifestyle advice and awareness that drug treatment may needconsideration as the person ages. Both risk age and lifetime risk are closerto relative than absolute risk, and none provides an evidence base for drugtreatment decisions.
2.3.4 Low-risk, high-risk and very-high-risk countries
The countries considered here are those with national cardiology societiesthat belong to the ESC, both European and non-European.
2.3.4.1 What are low-risk countries?
The fact that CVD mortality has declined in many European countries meansthat more now fall into the low-risk category. While any cut-off pointis arbitrary and open to debate, in these guidelines the cut-off pointsfor calling a country ‘low risk’ are based on age-adjusted 2012 CVDmortality rates in those 45–74 years of age (<225/100 000 in men and<175/100 000 in women).70 Thus the following countries are defined as lowrisk: Andorra, Austria, Belgium, Cyprus, Denmark, Finland, France,Germany, Greece, Iceland, Ireland, Israel, Italy, Luxembourg, Malta,Monaco, The Netherlands, Norway, Portugal, San Marino, Slovenia, Spain,Sweden, Switzerland and the United Kingdom.
2.3.4.2 What are high-risk and very-high-risk countries?
High-risk countries are Bosnia and Herzegovina, Croatia, Czech Republic,Estonia, Hungary, Lithuania, Montenegro, Morocco, Poland, Romania,Serbia, Slovakia, Tunisia and Turkey.
Very-high-risk countries present levels of risk that are more than doublethat of low-risk countries (i.e. CVD mortality >450/100 000 for menand >350/100 000 for women). Additionally, the male:female ratio issmaller than in low-risk countries, suggesting a major problem forwomen. The very high-risk countries are Albania, Algeria, Armenia,Azerbaijan, Belarus, Bulgaria, Egypt, Georgia, Kazakhstan, Kyrgyzstan,Latvia, former Yugoslav Republic of Macedonia, Moldova, RussianFederation, Syrian Arab Republic, Tajikistan, Turkmenistan, Ukraine andUzbekistan.
2.3.5 How to use the risk estimation charts
Use of the risk charts should be qualified by knowledge of the followingaspects:
The SCORE charts are used in apparently healthy people, not for thosewith established CVD or at very high risk or high risk for otherreasons [e.g. DM (see section 3a.8) or chronic kidney disease (CKD;see section 2.4.5.1)], who need intensive risk advice anyway.
Use of the low-risk chart is recommended for the countries listedabove. Use of the high-risk chart is recommended for all otherEuropean and Mediterranean countries, taking into account that thehigh-risk charts may underestimate the risk in very-high-riskcountries (see above). Note that several countries have undertakennational recalibrations to allow for time trends in mortality andrisk factor distributions. Such charts are likely to betterrepresent risk levels.
To estimate a person's 10 year risk of CV death, find the table fortheir gender, smoking status and (nearest) age. Within the table,find the cell nearest to the person's BP and total cholesterol. Riskestimates will need to be adjusted upwards as the person approachesthe next age category.
While no threshold is universally applicable, the intensity of adviceshould increase with increasing risk. The effect of interventions onthe absolute probability of developing a CV event increases with anincreasing baseline risk; that is, the number of individuals neededto treat (NNT) to prevent one event decreases with increasing risk.
– Low- tomoderate-risk persons (calculated SCORE<5%): should be offered lifestyle adviceto maintain their low- to moderate-riskstatus.
– High-riskpersons (calculated SCORE ≥5% and <10%):qualify for intensive lifestyle advice and may becandidates for drugtreatment.
– Very-high-riskpersons (calculated SCORE ≥10%): drugtreatment is more frequently required. In persons >60years of age, these thresholds should be interpretedmore leniently, because their age-specific risk isnormally around these levels, even when other CV riskfactor levels are ‘normal’. In particular, uncriticalinitiation of drug treatments of all elderly with risksgreater than the 10% threshold should bediscouraged.
The charts assist in risk estimation but must be interpreted in lightof the clinician's knowledge and experience and in view of thefactors that may modify the calculated risk (see below).
Relative risks may be high in young persons, even if 10 year absoluterisks are low, because events usually occur later in life. Therelative risk chart or estimating risk age may be helpful inidentifying and counselling such persons.
The lower risk in women is explained by the fact that risk isdeferred by 10 years—the risk of a 60-year-old woman is similar tothat of a 50-year-old man. Ultimately, more women than men die ofCVD.
The charts may be used to give some indication of the effects ofreducing risk factors, given that there will be a time lag beforerisk reduces and that the results of RCTs in general give betterestimates of the benefits of interventions. Those who stop smokinggenerally halve their risk.
2.3.6 Modifiers of calculated total cardiovascular risk
Apart from the conventional major CV risk factors included in the riskcharts, there are other risk factors that could be relevant for assessingtotal CVD risk. The Task Force recommends additional risk factor assessmentif such a risk factor improves risk classification [e.g. by calculation of anet reclassification index (NRI)] and if the assessment is feasible in dailypractice. In general, reclassification is of most value when theindividual's risk lies close to a decisional threshold, such as a SCORE riskof 5%. In very-high-risk or very-low-risk situations, the impact ofadditional risk factors is unlikely to alter management decisions. While thepresence of risk modifiers may move an individual's estimated risk upward,absence of these modifiers should lead to lowering an individual's estimatedrisk.
Table 4 listsexamples of factors that fulfil the aforementioned criteria. Several otherfactors that are frequently discussed in the literature, but may not havethe ability to reclassify subjects, are discussed in subsequent paragraphs.Also discussed further in this section are the roles of ethnicity and ofspecific conditions or diseases that may be associated with a higher thancalculated risk, such as CKD, autoimmune diseases, etc. The way modifiersare related to CV risk may be very different. Social deprivation and beingoverweight, for example, are important as ‘causes of the causes’ of CVD, inthat they may be associated with higher levels of conventional risk factors.Family history may reflect a shared environment, genetic factors or both.Markers such as computed tomography (CT) calcium scoring are indicators ofdisease rather than risk factors for future disease.
2.3.7 Risk categories: priorities
Individuals at highest risk gain most from preventive efforts, and thisguides the priorities, which are detailed in Table 5.
Risk categories
 |
 |
ACS = acute coronary syndrome; AMI = acute myocardial infarction;BP = blood pressure; CKD = chronic kidney disease; DM = diabetesmellitus; GFR = glomerular filtration rate; PAD = peripheralartery disease; SCORE = systematic coronary risk estimation; TIA= transient ischaemic attack.
Risk categories
 |
 |
ACS = acute coronary syndrome; AMI = acute myocardial infarction;BP = blood pressure; CKD = chronic kidney disease; DM = diabetesmellitus; GFR = glomerular filtration rate; PAD = peripheralartery disease; SCORE = systematic coronary risk estimation; TIA= transient ischaemic attack.
2.3.8 Risk factor targets
Risk factor goals and target levels for important CV risk factors arepresented in Table 6.
Risk factor goals and target levels for important cardiovascular riskfactors
 |
 |
BMI = body mass index; HbA1c = glycated haemoglobin; HDL-C =high-density lipoprotein cholesterol; LDL-C = low densitylipoprotein cholesterol.
aBlood pressure <140/90 mmHg is the general target.The target can be higher in frail elderly, or lower in mostpatients with DM (see chapter 3.a.8) and in some (very)high-risk patients without DM who can tolerate multiple bloodpressure lowering drugs (see chapter 3.a.9).
bNon-HDL-C is a reasonable and practical alternativetarget because it does not require fasting. Non HDL-C secondarytargets of <2.6, <3.3 and <3.8 mmol/L (<100, <130and <145 mg/dL) are recommended for very high, high and lowto moderate risk subjects, respectively. See section 3a.7.10 formore details.
cA view was expressed that primary care physiciansmight prefer a single general LDL-C goal of 2.6 mmol/L (100mg/dL). While accepting the simplicity of this approach and thatit could be useful in some settings, there is better scientificsupport for the three targets matched to level of risk.
dThis is the general recommendation for those at veryhigh-risk. It should be noted that the evidence for patientswith CKD is less strong.
Risk factor goals and target levels for important cardiovascular riskfactors
 |
 |
BMI = body mass index; HbA1c = glycated haemoglobin; HDL-C =high-density lipoprotein cholesterol; LDL-C = low densitylipoprotein cholesterol.
aBlood pressure <140/90 mmHg is the general target.The target can be higher in frail elderly, or lower in mostpatients with DM (see chapter 3.a.8) and in some (very)high-risk patients without DM who can tolerate multiple bloodpressure lowering drugs (see chapter 3.a.9).
bNon-HDL-C is a reasonable and practical alternativetarget because it does not require fasting. Non HDL-C secondarytargets of <2.6, <3.3 and <3.8 mmol/L (<100, <130and <145 mg/dL) are recommended for very high, high and lowto moderate risk subjects, respectively. See section 3a.7.10 formore details.
cA view was expressed that primary care physiciansmight prefer a single general LDL-C goal of 2.6 mmol/L (100mg/dL). While accepting the simplicity of this approach and thatit could be useful in some settings, there is better scientificsupport for the three targets matched to level of risk.
dThis is the general recommendation for those at veryhigh-risk. It should be noted that the evidence for patientswith CKD is less strong.
2.3.9 Conclusions
Estimation of total CV risk remains a crucial part of the present guidelines.The priorities (risk categories) defined in this section are for clinicaluse and reflect the fact that those at highest risk of a CVD event gain mostfrom preventive measures. This approach should complement public actions toreduce community risk factor levels and promote a healthy lifestyle. Theprinciples of risk estimation and the definition of priorities reflect anattempt to make complex issues simple and accessible. Their very simplicitymakes them vulnerable to criticism. Above all, they must be interpreted inlight of the physician's detailed knowledge of his/her patient and in lightof local guidance and conditions.
Gaps in evidence
There are no recent RCTs of a total risk approach to risk assessmentor risk management.
The young, women, older people and ethnic minorities continue to beunderrepresented in clinical trials.
A systematic comparison of current international guidelines is neededto define areas of agreement and the reasons for discrepancies.
2.4 Other risk markers
2.4.1 Family history/(epi)genetics
Key messages
Family history of premature CVD in first-degree relatives, before 55years of age in men and 65 years of age in women, increases the riskof CVD.
Several genetic markers are associated with an increased risk of CVD,but their use in clinical practice is not recommended.
Recommendations for assessment of family history/(epi)genetics
 |
 |
CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for assessment of family history/(epi)genetics
 |
 |
CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
2.4.1.1 Family history
Familial history of premature CVD is a crude but simple indicator of therisk of developing CVD, reflecting both the genetic trait and theenvironment shared among household members.71 A positive family history ofpremature CV death is associated with an increased risk of early andlifetime CVD.74In the few studies that simultaneously assessed and reported the effectsof family history and genetic scores, family history remainedsignificantly associated with the incidence of CVD after adjusting forthe genetic scores.75,76Limited data exist regarding the ability of family history to improvethe prediction of CVD beyond conventional CV risk factors.77–79One possible explanation is the varying definitions of family historyapplied80 and that conventional CV risk factors can partlyexplain the impact of family history.
A family history of premature CVD is simple, inexpensive information thatshould be part of the CV risk assessment in all subjects. Family historycan be a risk modifier to optimal management after the calculated riskusing SCORE lies near a decisional threshold: a positive family historywould favour more intensive interventions, while a negative familyhistory would translate into less intensive treatment.77
2.4.1.2 Genetic markers
Genetic screening and counselling is effective in some conditions, suchas familial hypercholesterolaemia (FH) (see section 3a.7.9). Thisparagraph will focus on genetic screening for high CV risk in thegeneral population.
Several recent genome-wide association studies have identified candidategenes associated with CVD. Since the effect of each genetic polymorphismis small, most studies have used genetic scores to summarize the geneticcomponent. There is a lack of consensus regarding which genes and theircorresponding single nucleotide polymorphisms (SNPs) should be includedin a genetic risk score and which method should be used to calculate thegenetic score.
The association of genetic scores with incident CVD has beenprospectively studied, adjusting for the main CV risk factors, and moststudies have found a significant association, with the relative risksvarying between 1.02 and 1.49 per increase in one score unit.77 The ability ofgenetic scores to predict CV events beyond traditional CV risk factors(i.e. defined by the NRI) was found in about half of the studies. TheNRI is a statistical measure quantifying the usefulness of adding newvariables to a risk prediction equation.77 The biggest improvements in theNRI were observed in participants at intermediate risk, while little orno improvement was observed in participants at high risk.75,81 One study estimated that oneadditional CAD event for every 318 people screened at intermediate riskcould be prevented by measuring the CAD-specific genetic score inaddition to established risk factors.81 Importantly, since the frequencyof polymorphisms might differ, the results may vary betweenpopulations.76,82,83 Recently, agenetic risk score based on 27 genetic variants enabled theidentification of subjects at increased risk of CAD, who would benefitthe most from statin therapy, even after adjustment for familyhistory.84 Still, it is likely that some reported associationsmight be due to chance,85 and replication studies are needed to confirmpositive findings.
Currently, many commercial tests are available, allowing an almostcomplete assessment of an individual's genome, and strong pressure isbeing applied to use this information to predict genetic risk and tomake genetic testing a routine measure.86 Given the lack of agreementregarding which genetic markers should be included, how genetic riskscores should be calculated and uncertainties about improvement in CVrisk prediction, the use of genetic markers for the prediction of CVD isnot recommended.
2.4.1.3 Epigenetics
Epigenetics studies the chemical changes in DNA that affect geneexpression. Methylation of genes related to CV risk factors isassociated with variation in CV risk factor levels,87,88 and lower DNA methylation levelsare associated with an increased risk of CAD or stroke.89 No informationexists, however, regarding the effect of epigenetic markers in improvingCVD risk prediction beyond conventional risk factors. Thus, epigeneticscreening of CVD is not recommended.
Gaps in evidence
The impact of adding family history to the current SCORE riskequation should be assessed.
Future studies should assess the power of different genetic riskscores to improve CVD risk prediction in several differentpopulations, the number of events prevented and thecost-effectiveness of including genetic data in the riskassessment.
2.4.2 Psychosocial risk factors
Key messages
Low socio-economic status, lack of social support, stress at work andin family life, hostility, depression, anxiety and other mentaldisorders contribute to the risk of developing CVD and a worseprognosis of CVD, with the absence of these items being associatedwith a lower risk of developing CVD and a better prognosis ofCVD.
Psychosocial risk factors act as barriers to treatment adherence andefforts to improve lifestyle, as well as to promoting health inpatients and populations.
Recommendation for assessment of psychosocial risk factors
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendation for assessment of psychosocial risk factors
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Low socio-economic status, defined as low educational level, low income,holding a low-status job or living in a poor residential area, confer anincreased risk of CAD; the relative risk (RR) of CAD mortality risk is1.3–2.0.93,94 Compared with theFramingham risk score, adding social deprivation to CV risk assessment wasable to reduce unattributed risk substantially.45
People who are isolated or disconnected from others are at increased risk ofdeveloping and dying prematurely from CAD. Similarly, a lack of socialsupport increases CAD risk and worsens the prognosis of CAD.95
Acute mental stressors may act as triggers of acute coronary syndrome (ACS).These stressors include exposure to natural catastrophes, as well aspersonal stressors (e.g. defeat or other serious life events) resulting inacute strong negative emotions (e.g. outbursts of anger or grief).96 After the death of asignificant person, the incidence rate of acute myocardial infarction (AMI)is elevated 21-fold during the first 24 hours, declining steadily during thesubsequent days.97
Chronic stress at work (e.g. long working hours, extensive overtime work,high psychological demands, unfairness and job strain) predicts prematureincident CAD in men [relative risk (RR) ∼1.2–1.5].98 In addition, long-term stressfulconditions in family life increase CAD risk (RR ∼2.7–4.0).99,100
Clinical depression and depressive symptoms predict incident CAD (RR 1.6 and1.9, respectively)101 and worsen its prognosis (RR 1.6 and 2.4,respectively).92,96,101,102 Vital exhaustion, most likelyrepresenting somatic symptoms of depression, significantly contributed toincident CAD (population attributable risk 21.1% in women and 27.7% in men).The NRI improved significantly.103 Panic attacks also increase the risk of incidentCAD (RR 4.2).104Anxiety is an independent risk factor for incident CAD (RR 1.3),92 for cardiacmortality following AMI [odds ratio (OR) 1.2]105 and cardiac events (OR1.7).106
Meta-analyses reported a 1.5-fold risk of CVD incidence, a 1.2-fold risk ofCAD and 1.7-fold risk for stroke in patients with schizophrenia,107 and a 1.3-foldrisk for incident CAD, even after adjustment for depression, in patientswith post-traumatic stress disorder.108
Hostility is a personality trait, characterized by extensive experience ofmistrust, rage and anger and the tendency to engage in aggressive,maladaptive social relationships. A meta-analysis confirmed that anger andhostility are associated with a small but significant increased risk for CVevents in both healthy and CVD populations (RR 1.2).109 The type D(‘distressed’) personality involves an enduring tendency to experience abroad spectrum of negative emotions (negative affectivity) and to inhibitself-expression in relation to others (social inhibition). The type Dpersonality has been shown to predict poor prognosis in patients with CAD(RR 2.2).110
In most situations, psychosocial risk factors cluster in individuals andgroups. For example, both women and men of lower socio-economic statusand/or with chronic stress are more likely to be depressed, hostile andsocially isolated.111 The INTERHEART study has shown that a cluster ofpsychosocial risk factors (i.e. social deprivation, stress at work or infamily life and depression) is associated with increased risk for myocardialinfarction (MI) (RR 3.5 for women and 2.3 for men). The populationattributable risk was 40% in women and 25% in men.112
Mechanisms that link psychosocial factors to increased CV risk includeunhealthy lifestyle [more frequent smoking, unhealthy food choices and lessphysical activity (PA)] and low adherence to behaviour changerecommendations or CV medication.93,113In addition, depression and/or chronic stress are associated withalterations in autonomic function, in the hypothalamic–pituitary axis and inother endocrine markers, which affect haemostatic and inflammatoryprocesses, endothelial function and myocardial perfusion.111 Enhanced risk inpatients with depression may also be due in part to adverse effects oftricyclic antidepressants.91
Assessment of psychosocial factors in patients and persons with CV riskfactors should be considered for use as risk modifiers in CV riskprediction, especially in individuals with SCORE risks near decisionalthresholds. In addition, psychosocial factors can help identify possiblebarriers to lifestyle changes and adherence to medication. Standardizedmethods are available to assess psychosocial factors in many languages andcountries.90Alternatively, a preliminary assessment of psychosocial factors can be madewithin the physicians' clinical interview, as shown in Table 7.
Core questions for the assessment of psychosocial risk factors inclinical practice
 |
 |
Core questions for the assessment of psychosocial risk factors inclinical practice
 |
 |
No more than a minimum education according to the requirement of the countryand/or a ‘yes’ for one or more items indicate an increased CV risk and couldbe applied as a modifier of CV risk (see Chapter 2.3.6). The management ofpsychosocial risk factors should be addressed according to Chapter 3a.2.
Gap in evidence
It remains unknown whether routine screening for psychosocial riskfactors contributes to fewer future cardiac events.
2.4.3 Circulating and urinary biomarkers
Key messages
CV circulating and urinary biomarkers have either no or only limitedvalue when added to CVD risk assessment with the SCORE system.
There is evidence of publication bias in the field of novelbiomarkers of CV risk, leading to inflated estimates of strength ofassociation and potential added value.
Recommendation for assessment of circulating and urinarybiomarkers
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendation for assessment of circulating and urinarybiomarkers
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
In general, biomarkers can be classified into inflammatory (e.g.high-sensitivity C-reactive protein (hsCRP, fibrinogen), thrombotic (e.g.homocysteine, lipoprotein-associated phospholipase A2), glucose- andlipid-related markers (e.g. apolipoproteins) and organ-specific markers(e.g. renal, cardiac). However, for the purpose of overall CV riskestimation, these distinctions are generally not relevant. Also, from theperspective of risk stratification (i.e. prediction of future CV events),the question of whether a biomarker is causally related to CVD or may be amarker of preclinical disease is equally irrelevant.
Among the most extensively studied and discussed biomarkers is hsCRP. Thisbiomarker has shown consistency across large prospective studies as a riskfactor integrating multiple metabolic and low-grade inflammatory factors,with RRs approaching those of classical CV risk factors. However, itscontribution to the existing methods of CV risk assessment is probablysmall.116
Meta-analyses and systematic reviews suggest that the vast majority of othercirculating and urinary biomarkers have no or limited proven ability toimprove risk classification. However, the extent to which they have beentested for their ability to add value to risk stratification variesconsiderably,114,115with strong evidence of reporting bias.117 Organ-specific biomarkers may beuseful to guide therapy in specific circumstances (e.g. albuminuria inhypertension or DM may predict kidney dysfunction and warrant renoprotectiveinterventions) (see section 3a).
If, despite these recommendations, biomarkers are used as risk modifiers, itis important to note that having an unfavourable biomarker profile may beassociated with a somewhat higher risk, but also that a favourable profileis associated with a lower risk than calculated. The degree to which thecalculated risk is affected by biomarkers is generally unknown, but almostuniversally smaller than the (adjusted) RRs reported for these biomarkers inthe literature.118Hence, in these patients, particularly with a moderate risk profile, onlyrelatively small adjustments in calculated risk are justifiable, andpatients who are clearly at high or low risk should not be reclassifiedbased on biomarkers.119
Gaps in evidence
Not all potentially useful circulatory and urinary biomarkers haveundergone state-of-the-art assessment of their added value in CVrisk prediction on top of conventional risk factors.
Biomarkers may be useful in specific subgroups, but this has beenaddressed in only a limited number of studies.
The role of metabolomics as risk factors for CVD and to improve CVrisk prediction beyond conventional risk factors should be furtherassessed.
2.4.4 Measurement of preclinical vascular damage
Key messages
Routine screening with imaging modalities to predict future CV eventsis generally not recommended in clinical practice.
Imaging methods may be considered as risk modifiers in CV riskassessment, i.e. in individuals with calculated CV risks based onthe major conventional risk factors around the decisionalthresholds.
Recommendations for imaging methods
 |
 |
ABI = ankle–brachial index; CV = cardiovascular; IMT =intima–media thickness.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for imaging methods
 |
 |
ABI = ankle–brachial index; CV = cardiovascular; IMT =intima–media thickness.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Although most CVD can be explained by traditional risk factors, there issubstantial variation in the amount of atherosclerosis. Thus interest hascontinued in the use of non-invasive imaging techniques to improve CV riskassessment. In individuals with calculated CV risks based on the majorconventional risk factors near the decisional thresholds, some imagingtechniques may be considered as risk modifiers to improve risk predictionand decision making.
2.4.4.1 Coronary artery calcium
Coronary artery calcium (CAC) is examined through electron beam ormultislice CT. Calcifications indicate late-stage subclinical coronaryatherosclerosis.134 Atherosclerotic coronary arteries do notnecessarily always show calcifications. The extent of the calcificationcorrelates with the extent of total coronary plaque burden.134 CAC is not anindicator of the (in)stability of an atherosclerotic plaque.135 In patientswith ACS, the extent of CAC is more pronounced than in those withoutCAD.136
The quantification of CAC scoring is fairly consistent across studies.Most studies use the Agatston score.137 The value of the score can befurther increased if the age and sex distribution within percentiles aretaken into account. A CAC score ≥300 Agatston units or ≥75th percentilefor age, sex and ethnicity is considered to indicate increased CVrisk.
CAC has shown a very high negative predictive value, since an Agatstonscore of 0 has a negative predictive value of nearly 100% for ruling outsignificant coronary narrowing.120 However, studies havequestioned the negative predictive value of CAC because significantstenosis in the absence of CAC is possible.121 Many prospective studies haveshown the association of CAC with CAD, and the Agatston score is anindependent predictor of CAD.122 Importantly, including CAC may improve CV riskprediction in addition to conventional risk factors.123 Thus, CACscoring may be considered in individuals with calculated SCORE risksaround the 5% or 10% thresholds.124,125
Although recent studies also showed the presence of CAC in low-riskpopulations, the added predictive value on CV events remains to bedemonstrated.138–140
There are concerns regarding costs and radiation exposure. For CACscoring, the radiation exposure with properly selected techniques is ±1mSv.
2.4.4.2 Carotid ultrasound
Population-based studies have shown correlations between the severity ofatherosclerosis in one arterial territory and the involvement of otherarteries.126 Therefore, early detection of arterial disease inapparently healthy individuals has focused on peripheral arteries, andin particular on the carotid arteries. Risk assessment using carotidultrasound focuses on the measurement of the intima–media thickness(IMT) and the presence and characteristics of plaques.
The IMT is not only a measure of early atherosclerosis, but also ofsmooth muscle hypertrophy/hyperplasia. There is a graded increase in CVrisk with increasing IMT,126 and a value >0.9 mm is considered abnormal.The risk of stroke associated with IMT is non-linear, with hazardsincreasing more rapidly at lower IMTs than at higher IMTs. TheIMT-associated risk of cardiac events is also non-linear.127 The extent ofcarotid IMT is an independent predictor of CVD, but seems to be morepredictive in women than in men.
The lack of standardization regarding the definition and measurement ofIMT, its high variability and low intra-individual reproducibility haveraised concerns. A recent meta-analysis failed to demonstrate any addedvalue of IMT compared to the Framingham Risk Score in predicting futureCVD, even in the intermediate risk group.128 Thus, the systematic use ofcarotid ultrasound IMT to improve risk assessment is notrecommended.
Plaque is usually defined as the presence of a focal wall thickening thatit is at least 50% greater than the surrounding vessel wall or as afocal region with an IMT measurement ≥1.5 mm that protrudes into thelumen.141 Plaques may be characterized by their number,size, irregularity and echodensity (echolucent vs. calcified). Plaquesare related to both coronary and cerebrovascular events, and echolucent(as opposed to calcified) plaques increase ischaemic cerebrovascularevents.127 Many studies emphasize the greater value ofmeasures that include plaque area and thickness, rather than IMT alone,in predicting CVD. Therefore, even though formal reclassificationanalyses have not been undertaken, carotid artery plaque assessmentusing ultrasonography may be considered to be a risk modifier in CV riskprediction in some cases.
2.4.4.3 Arterial stiffness
Arterial stiffness is commonly measured using either aortic pulse wavevelocity (PWV) or arterial augmentation index. An increase in arterialstiffness is usually related to damage in the arterial wall, as has beenshown in hypertensive patients.142 Although the relationshipbetween aortic stiffness and CVD is continuous, a PWV threshold of 12m/s has been suggested as a conservative estimate of significantalterations of aortic function in middle-aged hypertensive patients. Ameta-analysis showed that arterial stiffness predicts future CVD andimproves risk classification.142 However, the validity of this conclusion isoffset by evidence of substantial publication bias.117 The Task Forceconcludes that arterial stiffness may serve as a useful biomarker toimprove CV risk prediction for patients close to decisional thresholds,but its systematic use in the general population to improve riskassessment is not recommended.
2.4.4.4 Ankle–brachial index
The ankle–brachial index (ABI) is an easy-to-perform and reproducibletest to detect asymptomatic atherosclerotic disease. An ABI <0.9indicates ≥50% stenosis between the aorta and the distal leg arteries.Because of its acceptable sensitivity (79%) and specificity(90%),131 an ABI <0.90 is considered to be a reliablemarker of peripheral artery disease (PAD).129 An ABI value indicatingsignificant PAD adds value to the medical history, because 50–89% ofpatients with an ABI <0.9 do not have typical claudication130 and it ispresent in 12–27% of asymptomatic individuals >55 years of age.
The ABI is inversely related to CV risk,132 but there is controversyregarding its potential to reclassify patients into different riskcategories.131,143
2.4.4.5. Echocardiography
Echocardiography is more sensitive than electrocardiography in diagnosingleft ventricular hypertrophy (LVH) and it precisely quantifies leftventricular (LV) mass and geometric LVH patterns. Cardiac abnormalitiesdetected by echocardiography have an additional predictivepower.144,145 In view of the lack of convincing evidence thatechocardiography improves CV risk reclassification, and because of thelogistical challenges in performing it, this imaging tool is notrecommended to improve CV risk prediction.
Gaps in evidence
Currently, most imaging techniques have not been rigorouslytested as screening tools in CV risk assessment; more evidenceon calibration, reclassification and cost-effectiveness is stillneeded.
The reduction of CVD risk in patients treated with lipid- orBP-lowering drugs because of reclassification with, for example,CAC or ABI remains to be demonstrated.
2.4.5 Clinical conditions affecting cardiovascular disease risk
2.4.5.1 Chronic kidney disease
Key message Hypertension, dyslipidaemia and DM are commonamong patients with CKD. In addition, inflammatory mediators andpromoters of calcification cause vascular injury and may explain why CKDis associated with CVD even after adjustment for conventional riskfactors.146 A decreasing estimated glomerular filtration rate(eGFR) is an important sign of a gradually increasing risk forCVD-related mortality, starting at <75 mL/min/1.73 m2 andgradually increasing to an approximate three-fold risk in patients withvalues of 15 mL/min/1.73 m2. End-stage renal disease isassociated with a very high CV risk. Independent of eGFR, increasedalbumin excretion is also associated with CV mortality risk; the RR is ∼2.5 in overt proteinuria.147 Studies assessing whether the accuracy of CVrisk stratification improves with the addition of eGFR levels areemerging,148 but there is no consensus on which measure ofrenal function (i.e. which formula, and creatinine- orcystatine-C-based) best predicts CVD.149,150 Based on the evidence, theTask Force decided to classify patients with severe CKD (GFR <30mL/min/1.73 m2) as ‘very high risk’ and those with moderateCKD (GFR 30–59 mL/min/1.73 m2) as ‘high risk’ (seeTable 5).
CKD is associated with an increased risk of CVD, independent ofconventional CVD risk factors.
Gap in evidence
The contribution of various CKD markers to CVD riskstratification remains unclear.
2.4.5.2 Influenza
Key message
There is an association between acute respiratory infections,especially those occurring at times of peak influenza viruscirculation, and AMI.
Recommendation for influenza vaccination
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendation for influenza vaccination
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Influenza can trigger a CV event. Studies show an increase in rates of MIduring the annual influenza season. The risk of MI or stroke was morethan four times higher after a respiratory tract infection, with thehighest risk in the first 3 days.151 A recent meta-analysissuggests that preventing influenza, particularly by means ofvaccination, can prevent influenza-triggered AMI,154 but there isconcern that some studies are biased.151–153,155
Gap in evidence
Large-scale RCTs are needed to assess the efficacy of influenzavaccination in preventing influenza-triggered AMI.
2.4.5.3 Periodontitis
Studies have linked periodontal disease to both atherosclerosis andCVD,156,157 andserological studies have linked elevated periodontal bacteria antibodytitres to atherosclerotic disease.158 A longitudinal study hassuggested that an improvement in clinical and microbial periodontalstatus is related to a decreased rate of carotid artery IMT progressionduring a 3 year follow-up period,159 but IMT progression does notseem to be associated with CV events.133 Thus, if active treatment orprevention of periodontitis improves, clinical prognosis is stillunclear.
2.4.5.4 Patients treated for cancer
Key messages
Patients surviving cancer after treatment with chemotherapy orradiotherapy are at increased risk for CVD.
The increased incidence of CVD is correlated with the(combination of) treatments given and the administered dose.
The presence of traditional CV risk factors in cancer patientsfurther increases CV risk.
Recommendations for patients treated for cancer
 |
 |
CV = cardiovascular; LV = left ventricular.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dHigh-risk patients are mainly those individualsreceiving high cumulative doses of type I chemotherapyand/or combined treatment with other chemotherapic agentsand radiotherapy, and/or with CV uncontrolled riskfactors.
Recommendations for patients treated for cancer
 |
 |
CV = cardiovascular; LV = left ventricular.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dHigh-risk patients are mainly those individualsreceiving high cumulative doses of type I chemotherapyand/or combined treatment with other chemotherapic agentsand radiotherapy, and/or with CV uncontrolled riskfactors.
Survivors of cancer represent an increasingly large population, most ofwhom have received chemotherapy and/or radiotherapy. Cardiotoxicity dueto chemotherapy is related to a direct effect on the cell(anthracycline-like) through the generation of reactive oxygen species(ROS). It can be mediated by topoisomerase IIβ in cardiomyocytes throughthe formation of ternary complexes (topoisomerase IIβ–anthracycline–DNA)inducing DNA double-strand breaks and transcriptome changes responsiblefor defective mitochondrial biogenesis and ROS formation. Some agents(fluorouracil, bevacizumab, sorafenib and sunitinib) can induce a directischaemic effect not related to the premature development ofatherosclerotic lesions. Moreover, they can increase risk factors suchas hypertension and accelerate atherosclerosis, especially in olderpatients. These effects can be irreversible (type I agents) or partiallyreversible (type II agents) and can develop many years after treatmentexposure. Typically, anthracyclines are the prototype of type I agentsand trastuzumab of type II agents.162
Cardiotoxicity due to chest radiotherapy can induce micro- andmacrovascular injury. It can accelerate atherosclerosis, but this mayoccur many years after the initial exposure.163–169 The latencyand severity of radiotherapy cardiotoxicity is related to multiplefactors, including the dose (total per fraction), the volume of theheart irradiated, concomitant administration of other cardiotoxic drugsand patient factors (younger age, traditional risk factors,170 history ofheart disease).
The first step in the identification of higher risk for cardiotoxicityconsists of a careful baseline assessment of CV risk factors. Primarycare, cardiology and oncology should work together to deliver optimalsurvivorship care that addresses CVD risk factors as well as prevalentdisease. Positive health-promoting behaviour, including lifestylefactors (healthy diet, smoking cessation, regular exercise, weightcontrol) should be strongly advised. In particular, aerobic exercise isconsidered as a promising non-pharmacological strategy to prevent and/ortreat chemotherapy-induced cardiotoxicity.171
Signs or symptoms of cardiac dysfunction should be monitored before andperiodically during treatment for early detection of even asymptomaticabnormalities in patients receiving potentially cardiotoxicchemotherapy, and heart failure (HF) guideline recommendations should befollowed if indicated.172 Thus, pretreatment evaluation of LV functionis required.173A targeted approach to treat patients with early LV dysfunction, incombination with global longitudinal strain abnormalities and biomarker(notably troponin) elevation, has been proposed.173,174
In the case of a decrease in LV function during or after chemotherapy,the use of cardiotoxic agents should be avoided or delayed, if possible,until after discussion with the oncology team. This calls for adequatecommunication between oncology and cardiology.
To reduce chemotherapy type I cardiotoxicity, a variety of prophylactictreatments, including β-blockers, angiotensin-converting enzymeinhibitors (ACE-Is), dexrazozane and statins, has been tested andcompiled in a recent meta-analysis.161 It has been stressed thatearly preventive treatment is mandatory to exert a maximumeffect.173–176
Gaps in evidence
Evidence on the effect of early preventive measures to reducetype I cardiotoxicity is inconclusive.
The most appropriate strategy to improve risk stratification andprevent CVD in patients treated for cancer needs to be testedprospectively.
2.4.5.5 Autoimmune disease
Key messages
Rheumatoid arthritis (RA) enhances CV risk independently oftraditional risk factors, with an RR of 1.4 and 1.5 in men andwomen, respectively.
There is mounting evidence that other immune diseases, such asankylosing spondylitis or early severe psoriasis, also increaseCV risk, with RRs approaching those in RA.
Post hoc analysis of two statin trials suggests that the relativereduction in CVD incidence in autoimmune diseases is comparableto that seen in the other conditions.
Recommendations for autoimmune disease
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for autoimmune disease
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
There is now clear evidence implicating high-grade inflammation as apathway for accelerated vascular disease.178 Systemic inflammation appearsto enhance CV risk directly and indirectly via accentuation of existingrisk pathways.178 While early small studies suggested RA increasesCV risk beyond other risk markers, the recent analysis of the nationalQRESEARCH database in 2.3 million people provides the best availableevidence for this.47 Such evidence has now been implemented in somenational risk scores58 and European guidelines.177
Evidence in psoriasis is less rigorous, but a recent paper demonstratesbroadly comparable CV risks in RA and in early severepsoriasis.179 Robust data for independently elevated CV risks inother autoimmune conditions are generally lacking. Hence, clinicaljudgment should be applied on a case-by-case basis. There is evidencefrom post hoc analysis of randomized trials to support astatin-associated reduction in CV risk in autoimmuneconditions.180 Finally, in all autoimmune diseases, druginteractions of anti-inflammatory and immunosuppressive drugs with, forexample, statins, antiplatelet agents and antihypertensive agentsdeserve attention.
Gaps in evidence
The association between non-RA immune inflammatory disease andCVD is less clear than for RA.
The relationship between anti-rheumatic drugs and CV risk isunknown.
2.4.5.6 Obstructive sleep apnoea syndrome
Key message OSAS is characterized by recurrent partial orcomplete collapse of the upper airway during sleep. It affects anestimated 9% of adult women and 24% of adult men and has been associatedwith an RR of 1.7 for CV morbidity and mortality.181 Repetitivebursts of sympathetic activity, surges of BP and oxidative stressbrought on by pain and episodic hypoxaemia associated with increasedlevels of mediators of inflammation are thought to promote endothelialdysfunction and atherosclerosis.181 Screening for OSAS can beperformed using the Berlin Questionnaire and daytime sleepiness can beassessed by the Epworth Sleepiness Scale and overnightoximetry.182 Definitive diagnosis often requirespolysomnography, usually during a night in a sleep laboratory duringwhich multiple physiological variables are continuously recorded.Treatment options include behavioural changes, such as avoiding alcohol,caffeine or other stimulants of wakefulness before sleep, increased PA,discontinuation of sedating drugs and obesity control. Continuouspositive airway pressure is the gold-standard therapy and reduces CVmortality and events.183
There is evidence of a positive relationship between obstructivesleep apnoea syndrome (OSAS) and hypertension, CAD, atrialfibrillation (AF), stroke, and HF.
Gap in evidence
More studies are needed to determine whether routine screeningreduces (non)fatal CVD.
2.4.5.7 Erectile dysfunction
Key message
Erectile dysfunction (ED) is associated with future CV events inmen without and with established CVD.
Recommendation for erectile dysfunction
 |
 |
CV = cardiovascular; CVD = cardiovascular disease; ED =erectile dysfunction.
aClass of recommendation.
bLevel of evidence.
Recommendation for erectile dysfunction
 |
 |
CV = cardiovascular; CVD = cardiovascular disease; ED =erectile dysfunction.
aClass of recommendation.
bLevel of evidence.
ED, defined as the consistent inability to reach and maintain an erectionsatisfactory for sexual activity, is common, affecting almost 40% of men>40 years of age (with varying degrees of severity), and increases infrequency with age. ED and CVD share common risk factors, including age,hypercholesterolaemia, hypertension, insulin resistance and DM, smoking,obesity, metabolic syndrome, sedentary lifestyle and depression. CVD andED also share a common pathophysiological basis of aetiology andprogression.184 Numerous studies have established that ED isassociated with asymptomatic CAD.185,186 ED precedes CAD, stroke andPAD by a period that usually ranges from 2 to 5 years (average 3 years).A meta-analysis showed that patients with ED compared with subjectswithout ED have a 44% higher risk for total CV events, 62% for AMI, 39%for stroke and 25% for all-cause mortality.186 The predictive ability of EDis higher in younger ED patients despite the fact that the probabilityof ED increases with age, and it most likely identifies a group ofpatients with early and aggressive CVD. Thorough history taking,including CV symptoms and the presence of risk factors and co-morbidconditions, assessment of ED severity and physical examination aremandatory first-line elements of investigation. Lifestyle changes areeffective in improving sexual function in men: these include physicalexercise, improved nutrition, weight control and smokingcessation.184
Gap in evidence
The benefit of routine screening for ED and the most effectivetool to assess it are still unclear.
2.5 Relevant groups
2.5.1 Individuals <50 years of age
Key messages
Some people <50 years of age have high relative or lifetime CVrisk and should be offered lifestyle advice as a minimum.
Some younger people will have high single CV risk factors that, ofthemselves, warrant intervention, such as cholesterol levels >8mmol/L or BP ≥180/110 mmHg.
The most important group of people <50 years of age to identifyare those with a family history of premature CVD, who should betested for FH and treated accordingly.
Recommendation for individuals <50 years of age
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendation for individuals <50 years of age
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
The most powerful driver of risk in all short-term (5 or 10 year) CV riskalgorithms is age. As a consequence, all standard CV risk calculators showpeople <50 as low CVD risk, regardless of underlying risk factors.However, some younger individuals are at very high relative risk comparedwith individuals of a similar age and may have high lifetime risk: they aremore likely to develop CVD early and may prematurely suffer fatal ornon-fatal CV events. So trying to identify who may be at such risk is animportant challenge.
2.5.1.1 Assessing cardiovascular disease risk in people <50 years ofage
Information on CV risk factors should be routinely collected in alladults <50 years of age with a first-degree family history (i.e.<55 years of age for male and <65 years of age for femalerelatives) of premature CVD. There are no data on the right age to begincollecting such information in the general population, but someguidelines advocate starting at age 40 years.190 Repeating such assessmentsoccasionally, such as every 5 years, is recommended, but there are nodata to guide this interval.
People <50 years of age should be assessed using the standardalgorithm in terms of treatment decisions. However, in the absence of avery high individual risk factor level or diagnosis of FH, their 10-yearrisk will never be high enough to warrant BP- or lipid-lowering therapy.Physicians may want to further differentiate CV risk in younger peopleby using a relative risk chart (Figure 3, section 2.3.1); this might beuseful in assisting people <50 years of age to judge their risk inrelation to someone of the same age with low levels of risk factors.
Alternatively, physicians should consider using a risk age calculator(Figure 4, section 2.3.2) or a lifetime risk calculator,such as the JBS3 web-based tool (Figure J in webaddenda),58 which might act as an educational tool in terms ofhow changing risk factors might change the lifetime risk score as wellas illustrate long-term CVD risk.
People <50 years of age with a positive family history of prematureCVD should be screened for FH (see section 2.4.1) by clinical criteria(or occasionally genetic testing), such as those defined by the DutchLipid Clinic Network.187 Alternatives are the Simon Broome Registrycriteria188 or the US MedPed Program.189
2.5.1.2 Management of cardiovascular disease risk in people <50 years ofage
All people <50 years of age with elevated CVD risk factors should becounselled on lifestyle factors (with emphasis on avoiding smoking,overweight and sedentary behaviour) and the relationship between riskfactors and subsequent disease. There are no data on what are the mosteffective methods of changing health behaviours in younger people.However, smoking cessation, healthy weight maintenance and regularaerobic activity are all important behaviours on which to provide adviceand support.
Younger people with very high BP levels warranting treatment should bemanaged in the same way as older people with hypertension. In youngerpeople who are judged eligible for a statin on the grounds of either FHor very high lipid levels, the management offered is the same as forolder people. Very importantly, for all patients deemed to suffer withFH, the physician making the management decisions should arrange for FHscreening for family members (see section 3a.7.9).
Gaps in evidence
Age to commence formal CV risk estimation.
Whether and how to screen populations for FH.
2.5.2 Elderly
Age is the dominant driver of cardiovascular risk, and most individuals arealready at (very) high risk at the age of 65 years (see section 2.3.1).Especially in the oldest old, cardiovascular risk management iscontroversial. Opponents argue that risk should not be treated when it isessentially age-driven. Proponents, on the other hand, point out that manypreventive treatments are still effective at advanced age in terms ofpostponing morbidity and mortality.
The Task Force has taken the position that epidemiological evidence ofabsolute risk reduction in clinical trials is the main driver forrecommendations in this guideline. Still, we encourage a discussion withpatients regarding quality of life and life potentially gained, as well asregarding the ethical dilemmas of treating risk inherent to ageing, thetotal burden of drug treatment and the inevitable uncertainties ofbenefit.
In this guideline, sections on treatment of the main risk factors containrecommendations or considerations specific to the elderly when evidence isavailable.
2.5.2.1 Hypertension
Most of the elderly-specific evidence is available for BP (section 3a.9).In general, more lenient treatment targets are advocated in the elderly.The hypertension literature also contains increasing evidence thatbiological rather than calendar age is important.191
2.5.2.2 Diabetes mellitus
Evidence supporting more lenient glycaemic control targets in the elderlyis also available for DM (section 3a.8). The role of biologicalage/frailty is less well established than for BP, but nonetheless, aClass IIa recommendation is given to relax glycaemic targets in elderlyor frail patients.
2.5.2.3 Hyperlipidaemia
Few areas in CVD prevention are more controversial than the mass use ofstatins in the elderly. As the section on lipid control points out,there is no evidence of decreasing effectiveness of statins in patients>75 years of age (section 3a.7). On the other hand, thecost-effectiveness of statins in these patients is offset by even smallgeriatric-specific adverse effects.192 Also, evidence supportingeffectiveness in the oldest old (i.e. >80 years of age) is verylimited. A recent trial suggested no harm of stopping statins in theelderly with a limited life expectancy.193 Taken together, therecommendations of cholesterol-lowering treatment in the elderly shouldbe followed with caution and common sense, adverse effects should bemonitored closely and treatment should be reconsidered periodically.
2.5.3 Female-specific conditions
Key messages
Several obstetric complications, in particular pre-eclampsia andpregnancy-related hypertension, are associated with a higher risk ofCVD later in life. This higher risk is explained, at least partly,by hypertension and DM.
Polycystic ovary syndrome (PCOS) confers a significant risk forfuture development of DM.
Recommendations for female-specific conditions
 |
 |
DM = diabetes mellitus; PCOS = polycystic ovary syndrome.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for female-specific conditions
 |
 |
DM = diabetes mellitus; PCOS = polycystic ovary syndrome.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Specific conditions that may occur in females only and may have an impact onCVD risk can be separated into obstetric and non-obstetric conditions.
2.5.3.1 Obstetric conditions
Pre-eclampsia (defined as pregnancy-related hypertension accompanied byproteinuria) occurs in 1–2% of all pregnancies. Studies suggest thatpre-eclampsia is associated with an increase in CV risk by a factor1.5–2.5,194,195 while the RR of developing hypertension is ∼3196and DM ∼2.194,197 Because moststudies did not adjust the elevated risk of future CVD for thedevelopment of conventional risk factors, it cannot be establishedwhether the increased CV risk after pre-eclampsia occurs independent ofCV risk factors. The rationale for screening these women for theoccurrence of hypertension and DM is, however, quite strong.
Pregnancy-related hypertension affects 10–15% of all pregnancies. Theassociated risk of later CVD is lower than for pre-eclampsia, but isstill elevated (RR 1.9–2.5).202 Also, the risk for sustained or futurehypertension is elevated (RRs vary widely, from 2.0 to 7.2 or evenhigher).196,204 Again, however, there was incomplete adjustmentfor conventional risk factors. The risk of developing DM is probablyalso elevated in these women, but exact estimates are not available.
There are no data to suggest that recurrent pregnancy loss is associatedwith an increased CV risk. A history of premature birth is possiblyassociated with an increased risk of CVD in offspring (RR1.5–2.0),202,203 which may be partially explained by an increasedincidence of hypertension and DM.
Finally, gestational diabetes confers a sharply elevated risk of futureDM, with up to 50% developing DM within 5 years afterpregnancy.200 Previously, oral glucose tolerance testing wasadvocated to screen for DM in such patients, but screening by fastingglucose or glycated haemoglobin may be preferable.201
2.5.3.2 Non-obstetric conditions
PCOS affects ∼5% of all women in their fertile years. PCOS has beenassociated with an increased risk for future development of CVD, butlarger studies have produced conflicting results.198,205 The risk ofdeveloping hypertension is probably somewhat increased, but again thedata are conflicting.205 PCOS does seem to be associated with a higherrisk of developing DM (RR 2–4),198,199 suggesting that periodicscreening for DM is appropriate.
Premature menopause, better defined as primary ovarian insufficiency,occurs in roughly 1% in women ≤40 years of age. It has been reported tobe associated with an increased risk of CVD (RR ∼1.5),206 but studiesare sparse. There are insufficient data to draw conclusions on apossible increased risk of hypertension or DM.
Gaps in evidence
The degree to which increased CVD risk associated with several ofthe female-specific conditions occurs independent ofconventional CVD risk factors is unknown.
Information on whether female-specific conditions improve riskclassification in women is unknown.
2.5.4 Ethnic minorities
Key messages
CVD risk varies considerably between immigrant groups. South Asiansand sub-Saharan Africans have a higher risk, while Chinese and SouthAmericans have a lower risk.
South Asians are characterized by a high prevalence and inadequatemanagement of DM.
Current risk estimation equations do not provide adequate estimationsof CVD risk in ethnic minorities.
Recommendation for ethnic minorities
 |
 |
CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendation for ethnic minorities
 |
 |
CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Europe welcomes a large number of non-EU immigrants per year, mainly fromIndia, China, North Africa and Pakistan. One of 25 Europeans comes fromoutside Europe, but data regarding CVD risk or CVD risk factors amongimmigrants are scarce and of differing quality.209
First-generation migrants usually display lower CVD mortality rates thannatives of the host country,210 but with time, migrants tend to approach the CVDrisk in their host country.210,211Relative to natives of the host country, CVD mortality risk, as well as theprevalence and management of CVD risk factors among migrants, variesaccording to country of origin and host country.211–213 Given theconsiderable variability in CVD risk factors between immigrant groups, nosingle CVD risk score performs adequately in all groups and the use ofethnic-specific scores might be necessary.207
Immigrants from South Asia (notably India and Pakistan) present high CVDrates214–216 and have a much higher prevalence ofDM,217,218 while theprevalence of other CV risk factors is slightly lower than or comparable tonatives of the host country.217,219Interestingly, the increased prevalence of DM increases the CVD risk inSouth Asians in some studies214 but not in others. Management of DM is alsosignificantly worse, while management of high BP and hypercholesterolaemiais better among South Asians than host country natives.220 The higher CVDrisk among South Asians makes screening more cost effective than in otherimmigrant groups, but risk prediction using SCORE might not beoptimal.221
Immigrants from China and Vietnam present lower CVD risk than natives of thehost country,214although this finding has been challenged.215 This lower risk seems attributableto lower levels of CV risk factors217 and higher HDL-C levels.222
Immigrants from Turkey have higher estimated CVD risk and higher CVDmortality rates212than host country natives. This seems mainly due to the higher prevalence ofsmoking, DM, dyslipidaemia, hypertension and obesity rates.222–224Management of CVD risk factors also varies according to the host country;there are no differences in hypertension control compared with natives inThe Netherlands,224but there is worse control in Denmark.225
Immigrants from Morocco present lower CVD rates than natives from the hostcountry.212Possible explanations include lower BP and cholesterol levels and smokingrates,223,224 although a higherprevalence of DM and obesity has also been found.224 No differences between Moroccanimmigrants and Dutch natives were found regarding hypertensioncontrol.223
Immigrants from sub-Saharan Africa and the Caribbean present higher CVD ratesthan natives from the host country in some studies,213,214,226 but not all.214 African immigrants have higher DMrates218but smoke less219than natives from the host country. Management of CVD risk factors was worsethan among natives in one study,220 but not in another.227
Immigrants from South America have lower CVD mortality rates than natives inSpain,228while no difference was found in Denmark.229 South American immigrants in Spainhave a lower prevalence of CV risk factors and CVD rates than natives inSpain, but these differences decrease with increasing length ofstay.230
Based on available mortality and prospective data,208 the following correction factorscould be applied when assessing CVD risk using SCORE among first-generationimmigrants only. These values reflect the best estimations from availabledata and should be interpreted with caution, but can be used to guide CVrisk management.
Southern Asia: multiply the risk by 1.4
Sub-Saharan Africa and the Caribbean: multiply the risk by 1.3
Western Asia: multiply the risk by 1.2
Northern Africa: multiply the risk by 0.9
Eastern Asia or South America: multiply the risk by 0.7
Gaps in evidence
Studies focusing on CVD risk and the prevalence of CVD risk factorsamong minorities in Europe are needed.
Validation of the SCORE risk estimation among ethnic minorities isneeded.
Ethnicity-specific thresholds to define high risk (based on the SCOREevaluation) should be identified. Alternatively, ethnicity-specificCVD risk equations should be developed.
3a. How to intervene at the individual level: risk factor intervention
3a.1 Behaviour change
Key message
Cognitive behavioural methods are effective in supporting persons inadopting a healthy lifestyle.
Recommendations for facilitating changes in behaviour
 |
 |
CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for facilitating changes in behaviour
 |
 |
CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
‘Lifestyle’ is usually based on long-standing behavioural patterns that aremaintained by social environment. Individual and environmental factors impedethe ability to adopt a healthy lifestyle, as does complex or confusing advicefrom caregivers. Friendly and positive interaction enhances an individual'sability to cope with illness and adhere to recommended lifestyle changes(‘empowerment’). It is important to explore each patient's experiences,thoughts, worries, previous knowledge and circumstances of everyday life.Individualized counselling is the basis for motivation and commitment.Decision-making should be shared between the caregiver and patient (includingalso the individual's spouse and family).232,235 Use of the principles of effectivecommunication236 (Table 8) will facilitate treatment and prevention of CVD.
In addition, caregivers can build on cognitive behavioural strategies to assessthe individual's thoughts, attitudes and beliefs concerning the perceivedability to change behaviour, as well as the environmental context. Behaviouralinterventions such as ‘motivational interviewing’ increase motivation andself-efficacy.231
Previous unsuccessful attempts often affect self-efficacy for future change. Acrucial step is to help set realistic goals combined with self-monitoring of thechosen behaviour.232Moving forward in small, consecutive steps is key to changing long-termbehaviour.232Communication training is important for health professionals. The ‘ten strategicsteps’ listed in Table 9 can enhance counselling of behavioural change.237
Combining the knowledge and skills of caregivers (such as physicians, nurses,psychologists, experts in nutrition, cardiac rehabilitation and sports medicine)into multimodal behavioural interventions can optimize preventiveefforts.232–234 Multimodal behavioural interventions areespecially recommended for individuals at very high risk.232–234 Theseinterventions include promoting a healthy lifestyle through behaviour changes,including nutrition, PA, relaxation training, weight management and smokingcessation programmes for resistant smokers.233,234 They enhance coping with illness and improve adherenceand CV outcome.238,239 Psychosocial riskfactors (stress, social isolation, and negative emotions) that may act asbarriers against behaviour change should be addressed in tailored individual orgroup counselling sessions.233,234
There is evidence that more extensive/longer interventions lead to betterlong-term results with respect to behaviour change and prognosis.232 Individuals of lowsocio-economic status, older age or female sex may need tailored programmes inorder to meet their specific needs regarding information and emotionalsupport.232,240,241
Gap in evidence
There is limited evidence to determine which interventions are mosteffective in specific groups (e.g. young–old, male–female, high vs. lowsocio-economic status).
3a.2 Psychosocial factors
Key messages
Treatment of psychosocial risk factors can counteract psychosocialstress, depression and anxiety, thus facilitating behaviour change andimproving quality of life and prognosis.
The caregiver–patient interaction should follow the principles ofpatient-centred communication. Age- and sex-specific psychosocialaspects should be considered.
Recommendations for psychosocial factors
 |
 |
CAD = coronary artery disease; CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for psychosocial factors
 |
 |
CAD = coronary artery disease; CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Caregivers in clinical practice are in a unique position to directly supporttheir patients regarding psychosocial risk factors in individuals with high CVrisk or with established disease. Empathic, patient-centred communication helpsto establish and maintain a trustful relationship and is a powerful source ofemotional support and professional guidance in coping with psychosocialstressors, depression, anxiety, CV risk factors and CVD.247,248 The principles of a supportivecaregiver–patient interaction are247,248Specialized psychological interventions have additional beneficial effects ondistress, depressiveness and anxiousness, even when added to standardrehabilitation.242 These interventions include individual or groupcounselling on psychosocial risk factors and coping with illness, stressmanagement programmes, meditation, autogenic training, biofeedback, breathing,yoga and/or muscular relaxation.
Spend enough time with the patient, listen carefully and repeat essentialkeywords.
Consider age- and sex-specific psychosocial aspects.
Encourage expression of emotions, do not trivialize psychosocial burdensand worries.
Explain essential medical facts in the patient's own language, conveyhope and relief from feelings of guilt and reinforce adaptive thoughtsand actions.
In the case of severe mental symptoms, obtain treatment preferences andperform shared decision-making regarding further diagnostic andtherapeutic steps.
Summarize important aspects of the consultation to confirm that thepatient has been understood.
Offer regular follow-up contacts.
Large and consistent effects on depression have been shown in ‘collaborativecare’, which may involve a systematic assessment of depression, a(non-physician) care manager to perform longitudinal symptom monitoring,treatment interventions and care coordination and specialist-provided steppedcare recommendations and treatment.244 Collaborative care for depression resulted in a 48%lower risk for developing first CAD events 8 years after treatment compared withusual care [RR 0.52 (95% CI 0.31, 0.86)].245 Internet-delivered cognitivebehavioural therapy in depressed patients with high CVD risk produced small, butrobust, improvement of depressive symptoms, adherence and some healthbehaviours.246
In patients with established CAD, mental health treatments for depression(psychotherapy and/or medication) have moderate efficacy for reducing cardiacevents (NNT 34), but do not reduce total mortality.243 Collaborative care is especiallyeffective on depressive symptoms and partially effective on cardiacprognosis.249,250 Furthermore, there isevidence that PA can effectively improve depression in patients withCAD.251
In addition to the treatment of mood symptoms, there are several other approachesto psychosocial intervention that have proved useful. Two RCTs252,253 have shown the favourable impact ofstress management and social support groups on the prognosis of clinical CAD.Nurse-led interventions reveal beneficial effects on anxiety, depression andgeneral well-being in CAD patients.254,255
In hostile CAD patients, a group-based hostility-control intervention may leadnot only to decreases in behaviourally assessed hostility levels, but also todecreased levels of depression, resting heart rate (HR) and CV reactivity tomental stress, as well as to increased social support and satisfaction withlife.256 Workreorganizations aimed at improving autonomy and increasing control at work mayresult in improved social support and a reduction in physiological stressresponses. Hence, a reduction of work stress in managers and supervisors mayhave beneficial health effects on the target individuals and may also improveperceived social support in their subordinates.257
Gap in evidence
Evidence that treatment of clinically significant depression and anxietyalone will prevent CVD and improve outcomes is inconclusive.
3a.3 Sedentary behaviour and physical activity
Key messages
Regular PA is a mainstay of CV prevention; participation decreasesall-cause and CV mortality.
PA increases fitness and improves mental health.
Sedentary subjects should be encouraged to start light-intensity aerobicPA.
Recommendations for physical activity
 |
 |
CV = cardiovascular; PA = physical activity.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dVolume is the total weekly dose of PA.
Recommendations for physical activity
 |
 |
CV = cardiovascular; PA = physical activity.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dVolume is the total weekly dose of PA.
3a.3.1 Introduction
Regular PA reduces the risk of many adverse health outcomes over a wide agerange: all-cause and CVD mortality are reduced in healthy individuals by20–30% in a dose–response fashion,258–260,267,269 in subjects with coronary risk factors269 and in cardiacpatients.270 PA has a positive effect on many risk factors,including hypertension, low-density lipoprotein cholesterol (LDL-C) andnon-HDL-C, body weight and type 2 DM.267 This applies to both men and womenand across a broad range of ages from childhood to the very elderly. Asedentary lifestyle is one of the major risk factors for CVD independent ofparticipation in PA.271
3a.3.2 Physical activity prescription
Health providers should assess the PA level in any subject (how many days andminutes per day are spent on average doing PA at moderate or vigorousintensity). They should warn against inactivity and help add PA to dailylife. Subjects should be advised on appropriate types of activities and waysof progressing and should be helped to set personal goals to achieve andmaintain the benefits. To this end, individuals should be encouraged to findsome activity they either enjoy and/or that they can include in their dailyroutines, as such activities are more likely to be sustainable. For a moreeffective behaviour change, clinicians should explore practical ways toovercome barriers to exercise. For this reason, the link between primarycare and local community-based structures for activity, recreation and sportis crucial.262 Theamount of time spent being sedentary should be minimized by activetravelling (cycling or walking), taking breaks from extended periods ofsitting and reducing screen time.272 Brief exercises are more cost effective thansupervised gym-based exercise classes or instructor-led walkingprogrammes.264
3a.3.2.1 Aerobic physical activity
Aerobic PA, the most studied and recommended modality, with a beneficialdose–response effect on prognosis,259,260,268 consists of movements of largemuscle mass in a rhythmic manner for a sustained period. It includeseveryday activity, including active travel (cycling or walking), heavyhousehold work, gardening, occupational activity and leisure timeactivity or exercise such as brisk walking, Nordic walking, hiking,jogging or running, cycling, cross-country skiing, aerobic dancing,skating, rowing or swimming.
Similar to all other interventions, its prescription can be adjusted interms of frequency, duration and intensity. However, practising PA belowthe lowest recommended levels should be encouraged in individuals unableto meet the minimum or in those sedentary individuals who have juststarted, with a gradual increase in activity level.
Moderate or vigorous aerobic exercise should be recommended. This can beexpressed either in absolute or relative terms.
Absolute intensity is the amount of energy expended perminute of activity, assessed by oxygen uptake per unit of time (mL/minor L/min) or by metabolic equivalent (MET), which is estimated as therate of energy expenditure while sitting at rest. By convention thiscorresponds to 3.5 mL O2/kg/min).273 A list of PA intensities inMET values is available.274 An absolute measure does not take into accountindividual factors such as body weight, sex, and fitness level: olderpersons exercising at a vigorous intensity of 6 METs may be exercisingat their maximum intensity, while a younger person working at the sameabsolute intensity may be exercising moderately.
Relative intensity is the level of effort required toperform an activity. Less fit individuals generally require a higherlevel of effort than fitter people to perform the same activity. It isdetermined relative to an individual's level of cardiorespiratoryfitness (V̇O2max) or as a percentage of a person's measuredor estimated maximum HR (%HRmax), which is 220 − age. It also can beexpressed as an index of individual rate of effort (how hard the personfeels he/she is exercising), that is, the rating of perceived exertion(RPE) or by frequency of breathing (the so-called Talk Test). Forindividuals on medication, it is important to consider possiblemodification of HR response and to refer to other relative intensityparameters. Especially for older and deconditioned individuals, arelative measure of intensity is more appropriate. Classification forboth absolute and relative intensity and examples are presented inTable 10.
Classification of physical activity intensity and examples ofabsolute and relative intensity levels
 |
 |
MET (metabolic equivalent) is estimated as the energy cost ofa given activity divided by resting energy expenditure: 1MET = 3.5 mL O2 kg-1 min-1 oxygen consumption(VO2).
RPE, rating of perceived exertion (20 value Borg score).
%HRmax, percentage of measured or estimated maximum heartrate (220-age).
Modified from Howley.275
Classification of physical activity intensity and examples ofabsolute and relative intensity levels
 |
 |
MET (metabolic equivalent) is estimated as the energy cost ofa given activity divided by resting energy expenditure: 1MET = 3.5 mL O2 kg-1 min-1 oxygen consumption(VO2).
RPE, rating of perceived exertion (20 value Borg score).
%HRmax, percentage of measured or estimated maximum heartrate (220-age).
Modified from Howley.275
PA should occur at a frequency of at least three to five sessions perweek, but preferably every day.
It is recommended that individuals accumulate at least 30 min/day, 5days/week of moderate intensity PA (i.e. 150 min/week) or 15 min/day, 5days/week of vigorous intensity PA (75 min/week), or a combination ofboth, performed in sessions with a duration of at least 10 min. Shorterexercise sessions (i.e. <10 min) may also be appropriate, especiallyin very deconditioned individuals.267,276,277 For lipid control or bodyweight management, longer durations of exercise, 40 and 60–90 min/day,respectively, have been proposed.278
Aerobic interval training and high-intensity interval training cannot yetbe broadly recommended until further data on safety and efficacy areavailable.266
3a.3.2.2 Muscle strength/resistance physical activity
Isotonic PA stimulates bone formation and reduces bone loss; it preservesand enhances muscle mass, strength, power and functional ability, withsome evidence of benefit in lipid and BP control and insulinsensitivity, especially in combination with aerobic exercise.267,279 It shouldtarget the major muscle groups (agonist and antagonist) and includemultijoint or compound movements through the full range of motion of thejoints, such as working with resistance bands, calisthenics using bodyweight for resistance, carrying heavy loads and heavy gardening. Foreach exercise session, the suggested prescription is two to three setsof 8–12 repetitions at the intensity of 60–80% of the individual's 1repetition maximum (1 RM, the maximum load that can be lifted one time)at a frequency of least 2 days a week. For older adults or verydeconditioned individuals, it is suggested to start with one set of10–15 repetitions at 60–70% of 1 RM.280
3a.3.2.3 Neuromotor physical activity
For older adults at risk of falls, neuromotor exercise helps to maintainand improve balance and motor skills (balance, agility, coordination andgait). This includes multifaceted activities such as tai chi and yoga,and recreational activities using paddles or sport balls to challengehand–eye coordination. The optimal volume is not known.276
3a.3.2.4 Phases and progression of physical activity
PA sessions should include the following phases: warm-up, conditioning(aerobic, muscle strength/resistance and neuromotor exercise), cool-downand stretching/flexibility. Progressive warm-up before and cool-downafter exercise may prevent injuries and adverse cardiac events. Inactiveadults should start gradually, at light or moderate intensity for shortperiods of time (even <10 min), with sessions spread throughout theweek. With the improvement in exercise tolerance, each subjectprogresses in the level of PA, but increases in any components (i.e.frequency, duration and intensity) should be gradual, to minimize risksof muscle soreness, injury, fatigue and the long-term risk ofovertraining.276 Following any adjustments, the individualshould check for adverse effects (e.g. excessive shortness of breath)and if there are any such effects, downward adjustments should bemade.276
3a.3.3 Risk assessment
The risk of an adverse CV response during PA is extremely low for apparentlyhealthy adults (5–17 sudden deaths/million population/year).281 The risk ofparticipation is outweighed by the substantial health benefits conferred byPA.267 Riskduring light- or moderate-intensity exercise is lower than during vigorousactivity,267 thus in healthy individuals who wish to undertakemoderate PA, such as a walking programme, a preliminary medical evaluationis not needed.266
Before starting more intensive leisure time activities (i.e. structured orcompetitive activity, amateur sports, exercise and fitness training), a riskassessment should be tailored to the individual's clinical (i.e. metabolic,musculoskeletal condition/disease) and cardiac risk profile, the currentlevel of habitual PA and the intended level of PA.265 Individuals who exercise onlyoccasionally seem to have an increased risk of acute coronary events andsudden cardiac death during or after exercise.282 Sedentary subjects and those withCV risk factors should start aerobic PA at low-intensity activity andprogress gradually. Clinical evaluation, including exercise testing, may beconsidered for sedentary people with CV risk factors who intend to engage invigorous PA and sports. The information gathered from exercise tests may beuseful in establishing a safe and effective exercise prescription. Validatedself-assessment questionnaires have been proposed for sedentary individualsentering low-intensity leisure time sports activity or startingmoderate-intensity activities265 (see Table B in web addenda).
Gaps in evidence
The lower and upper limit of aerobic PA intensity, duration andfrequency to exert a beneficial effect is unknown.
The effectiveness of PA monitoring vs. simple counselling to optimizethe motivation of patients to adhere to active lifestyle isunknown.
The role and sustainability of modern technology (such as wearabletechnology, ‘exergaming’ and smartphone apps) for motivating peopleto undertake more PA has not been established.
3a.4 Smoking intervention
Key messages
Stopping smoking is the most cost-effective strategy for CVDprevention.
There is a strong evidence base for brief interventions with advice tostop smoking, all types of nicotine replacement therapy (NRT),bupropion, varenicline and greater effectiveness of drugs incombination, except for NRT plus varenicline. The most effective arebrief interventions plus assistance with stopping using drug therapy andfollow-up support.
Electronic cigarettes (e-cigarettes) may help in smoking cessation butshould be covered by the same marketing restrictions as cigarettes.
Passive secondary smoking carries significant risk, with the need toprotect non-smokers.
Recommendations for smoking intervention strategies
 |
 |
CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for smoking intervention strategies
 |
 |
CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
3a.4.1 Introduction
Smoking is a lethal addictive disorder. A lifetime smoker has a 50%probability of dying due to smoking, and on average will lose 10 years oflife,287contrasting with <3 years with severe hypertension and <1 year withmild hypertension.288 Smoking is an established cause of a plethora ofdiseases and is responsible for 50% of all avoidable deaths in smokers, halfof these due to CVD. The 10-year fatal CVD risk is approximately doubled insmokers. The RR in smokers <50 years of age is five-fold higher than innon-smokers.289
Slightly less than half of lifetime smokers will continue smoking untildeath. Approximately 70% of UK smokers want to stop smoking at some time inthe future,290 with ∼43% trying to stop in the past year; however, only 2–3% of the populationsucceed in stopping.291 Even modest and low levels of smoking confer vascularrisk.294
Although the rate of smoking is declining in Europe, it remains very commonand is increasing in women, adolescents and the sociallydisadvantaged.295 Widening education-related inequalities in smokingcessation rates have been observed in many European countries. In theEUROASPIRE IV survey among CAD patients, 16% smoked after a mean follow-uptime of 16 months, and nearly half of the participants who smoked at thetime of their coronary event were persistent smokers. The survey also foundthat evidence-based treatment for smoking cessation was underused.6
3a.4.2 Dosage and type
The risks associated with smoking show a dose–response relationship with nolower limit for deleterious effects.296 Duration also plays a role, andwhile cigarette smoking is the most common, all types of smoked tobacco,including low-tar (‘mild’ or ‘light’) cigarettes, filtered cigarettes,cigars and pipes, are harmful.292 Smoking is deleterious regardless of how it isdone, including by water pipe. Tobacco smoke is more harmful when inhaled,but smokers who claim not to inhale the smoke (e.g. pipe smokers) are alsoat increased risk of CVD. Smokeless tobacco is also associated with a smallbut statistically significant increased risk of MI and stroke.
3a.4.3 Passive smoking
Passive smoking increases the risk of CAD.293,297 A smoking spouse or workplace exposure increasesCVD risk by an estimated 30%. Major health benefits result from reducedenvironmental tobacco smoke, with public smoking bans in various differentgeographical locations leading to significant decreases in MI rates (seesection 3c.4).
3a.4.4 Mechanisms by which tobacco smoking increases risk
Smoking enhances the development of both atherosclerosis and superimposedthrombotic phenomena. Smoking affects endothelial function, oxidativeprocesses, platelet function, fibrinolysis, inflammation, lipid oxidationand vasomotor function. In experimental studies, several of these effectsare fully or partly reversible within a very short time. Plaque formation isnot thought to be fully reversible and thus smokers would never be expectedto reach the risk level of never smokers concerning CVD. Nicotinereplacement shows no adverse effect on outcomes in patients with cardiacdisease.298,299
3a.4.5 Smoking cessation
The benefits of smoking cessation have a large evidence base. Some advantagesare almost immediate; others take more time. CVD risk in former smokers isin between that of current and never smokers.
Stopping smoking after an MI is potentially the most effective of allpreventive measures: a systematic review and meta-analysis showed reductionsin MIs and in the composite endpoints of death/MI (RR 0.57 and 0.74,respectively) compared with continued smoking.300 The benefit is consistent overgender, duration of follow-up, study site and time period. Significantmorbidity reductions occur within the first 6 months.301 Randomized trialsalso support smoking cessation, with the risk of CVD approaching (but neverequalling) the risk of never smokers within 10–15 years.
Smoking reduction has not been shown to increase the probability of futuresmoking cessation, but some advocate nicotine-assisted smoking reduction insmokers unable or unwilling to quit. Quitting must be encouraged in allsmokers (Table 11). There is no age limit to the benefits of smokingcessation. Passive smoking should also be avoided.
Professional support can increase the odds of stopping [RR 1.66 (95% CI 1.42,1.94)].302An impetus for smoking cessation occurs at the time of diagnosing or(invasive) treatment of CVD. Prompting a person to try to quit, briefreiteration of CV and other health hazards and agreeing on a specific planwith a follow-up arrangement are evidence-based interventions (seeFigure K in web addenda).
Smoking cessation programmes initiated during hospital admission shouldcontinue for a prolonged period after discharge. A smoking history includingdaily tobacco consumption and degree of addiction (most commonly assessed bythe Fagerström test302) may guide the degree of support and pharmacologicalaids. Smokers should be advised about expected weight gain of, on average, 5kg and that the health benefits of tobacco cessation far outweigh the risksfrom weight gain.
3a.4.6 Evidence-based drug interventions
Following the failure of advice, encouragement and motivationalinterventions, or in addition to them, NRT, varenicline or bupropion shouldbe offered to assist cessation.285 All forms of NRT (chewing gum, transdermalnicotine patches, nasal spray, inhaler, sublingual tablets) are effective:in a systematic review, the RR for abstinence with NRT vs. control was 1.60;NRTs increase the rate of quitting by 50–70%, regardless ofsetting.303
The antidepressant bupropion aids long-term smoking cessation with a similarefficacy to NRT.286A meta-analysis of 44 trials comparing long-term cessation rates usingbupropion vs. control yielded a relative success rate of 1.62.283 Bupropion carriesa known risk of seizures (reported as ∼1/1000 users),286 without increasedrisks of neuropsychiatric or heart and circulatory problems. Overall, NRTand bupropion help ∼80% more people to quit than placebo; this means thatfor every 10 people who quit with placebo, ∼18 could be expected to quitwith NRT or with bupropion.285
The partial nicotine receptor agonist varenicline at the standard doseincreases the chances of quitting more than two-fold compared with placebo(14 trials, 6166 people).283 The number of people stopping smoking withvarenicline is higher than with bupropion (three trials, 1622 people).Varenicline more than doubles the chances of quitting compared with placebo,so that for every 10 who quit with placebo, ∼28 could be expected to quitwith varenicline. Varenicline helps ∼50% more people to quit than nicotinepatch and ‘other’ NRTs (tablets, sprays, lozenges and inhalers) and ∼70%more people than nicotine gum. So for every 10 people who quit with an NRTpatch or with ‘other’ NRTs, ∼15 would be expected to quit with varenicline,and for every 10 who quit with NRT gum, ∼17 would be expected to quit withvarenicline.285
Low-dose varenicline (four trials, 1272 people) roughly doubles the chancesof quitting and reduces the number and severity of side effects. The mainside effect of varenicline is nausea, but this is mostly mild or moderateand usually subsides over time.285 Although concerns have been raised, retrospectivecohort studies and an RCT304 indicate no severe adverse events with vareniclinein the setting of ACS patients, with the large EVITA trial in ACSongoing.
Clonidine has helped people to quit, but causes side effects and is thereforea second-line agent. It is not clear whether mecamylamine used with NRThelps people to quit. Other treatments did not seem to help. So far,nicotine vaccines are not licensed for use anywhere in the world.285
Combining two types of NRT is as effective as using varenicline, and helpsmore people to quit than a single type of NRT.285
3a.4.7 Electronic cigarettes
Electronic cigarettes (e-cigarettes) are battery-operated devices thatsimulate combustible cigarettes by heating nicotine and other chemicals intoa vapour that is inhaled. Electronic cigarettes deliver the addictivenicotine without the vast majority of tobacco chemicals, and are probablyless harmful than tobacco.305
Evidence on the effectiveness of e-cigarettes is limited due to the smallnumber of trials, low event rates and wide confidence intervals.306 Data from someobservational studies and a randomized trial suggest that the efficacy offirst-generation e-cigarettes is similar to that of transdermal NRTpatches307or NRT inhalers.308The benefit may come from low nicotine delivery or just the non-nicotinebehavioural components of e-cigarette use. About 6% of former smokers whoused e-cigarettes daily relapsed to smoking after 1 month and 6% after 1year, and nearly half of dual users of both tobacco and e-cigarettes stoppedsmoking after 1 year, indicating that e-cigarette use might be effective inrelapse prevention and smoking cessation.309 These studies and real-world dataindicate that e-cigarettes are moderately effective as smoking cessation andharm reduction aids, but that a significant component of that effect is dueto changes in behaviour rather than in nicotine delivery. Recent evidenceindicates that e-cigarettes, as currently being used, are associated withsignificantly less quitting among smokers.310 Although no safety issues havebeen observed in the short term (2 years), determining the long-term healtheffects of e-cigarettes (and in particular dual use with cigarettes) willrequire more research.305
3a.4.8 Other smoking cessation interventions
Both individual and group behavioural interventions are effective in helpingsmokers quit. Support from the individual's partner and family is important.There are no reliable data that acupuncture, acupressure, laser therapy,hypnotherapy or electrostimulation are effective for smoking cessation.
Gap in evidence
More efficient, safe and cost-effective smoking cessation aids arerequired.
3a.5 Nutrition
Key messages
Dietary habits influence the risk of CVD and other chronic diseases suchas cancer.
Energy intake should be limited to the amount of energy needed tomaintain (or obtain) a healthy weight, that is, a BMI >20.0 but<25.0 kg/m².
In general, when following the rules for a healthy diet, no dietarysupplements are needed.
Recommendation on nutrition
 |
 |
CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendation on nutrition
 |
 |
CVD = cardiovascular disease.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
3a.5.1 Introduction
Dietary habits influence CV risk, either through an effect on risk factorssuch as cholesterol, BP, body weight and DM, or through othereffects.311Table 12summarizes the characteristics of a healthy diet.
Most evidence on the relation between nutrition and CVD is based onobservational studies; randomized clinical trials estimating the impact ofdiet on endpoints are scarce. The impact of diet is studied on three levels:specific nutrients, specific foods/food groups and specific dietarypatterns, of which the Mediterranean diet is the most studied.
The nutrients of interest with respect to CVD are fatty acids (which mainlyaffect lipoprotein levels), minerals (which mainly affect BP), vitamins andfibre.
3a.5.2 Fatty acids
For prevention of CVD, the types of fatty acids consumed are more importantthan the total fat content.
The risk of CAD is reduced by 2–3% when 1% of energy intake from saturatedfatty acids is replaced by polyunsaturated fatty acids. The same has notbeen clearly shown for replacement with carbohydrates and monounsaturatedfatty acids (MUFAs). Saturated fatty acid intake should be reduced to amaximum of 10% of energy intake by replacing it with polyunsaturated fattyacids.312
MUFAs have a favourable effect on HDL-C levels when they replace saturatedfatty acids or carbohydrates,313 but there is little evidence that MUFAs lower CADrisk.
Polyunsaturated fatty acids lower LDL-C levels, and to a lesser extent HDL-Clevels, when they replace saturated fatty acids. The polyunsaturated fattyacids can be divided into two subgroups: omega-6 fatty acids, mainly fromplant foods, and omega-3 fatty acids, mainly from fish oils and fats. Withinthe subclass of omega-3 fatty acids, eicosapentaenoic acid anddocosahexaenoic acid (EPA/DHA) are especially important. They do not changeserum cholesterol levels and, with currently available cardioprotectivetherapies, it is debatable whether they exert a favourable effect onall-cause, CAD, and stroke mortality.314,315
The trans fatty acids, a subclass of unsaturated fatty acids, have been shownto be especially harmful due to their unfavourable impact on both totalcholesterol (increase) and HDL-C (decrease). These fatty acids are formedduring industrial processing (hardening) of fats and are present in, forexample, margarine and bakery products. A meta-analysis of prospectivecohort studies has shown that, on average, a 2% increase in energy intakefrom trans fatty acids increases CAD risk by 23%.316 It is recommended to derive <1%of total energy intake from trans fatty acids—the less the better.
The impact of dietary cholesterol on serum cholesterol levels is weakcompared with that of the fatty acid composition of the diet. Whenguidelines are followed to lower saturated fat intake, this usually alsoleads to a reduction in dietary cholesterol intake. Therefore, someguidelines (including this one) on healthy diet do not give specificguidelines on the intake of dietary cholesterol; others recommend a limitedintake of <300 mg/day.
3a.5.3 Minerals
A meta-analysis estimated that even a modest reduction in sodium intake of 1g/day reduces SBP by 3.1 mmHg in hypertensive patients and 1.6 mmHg innormotensive patients.317 The Dietary Approaches to Stop Hypertension (DASH)trial showed a dose–response relation between sodium reduction and BPreduction.318 In most western countries, salt intake is high (∼9–10g/day), whereas the recommended maximum intake is 5 g/day. Optimal intakelevels might be as low as ∼3 g/day. Although the relation between saltintake and BP remains controversial, the totality of evidence warrants saltreduction as an important way to prevent CAD and stroke. On average, 80% ofsalt intake comes from processed foods, while only 20% is added later on.Salt reduction can be achieved by making different dietary choices (fewerprocessed foods, more basic foods) and the reformulation of foods (loweringsalt content) (see Chapter 3c.2).
Potassium has favourable effects on BP. The main sources of potassium arefruits and vegetables. An inverse statistically significant associationexists between potassium intake and the risk of incident stroke [RR 0.76(95% CI 0.66, 0.89)].319 Apart from reducing sodium intake, increasingpotassium intake contributes to the lowering of BP.
3a.5.4 Vitamins
Many case–control and prospective observational studies have observed inverseassociations between levels of vitamin A and E and the risk of CVD. However,intervention trials have failed to confirm these observational studies.Also, for the B vitamins (B6, folic acid and B12) and vitamin C, trials haveshown no beneficial effects.
In the bottom tertile of serum levels of vitamin D, CV and total mortality is35% higher [RR 1.35 (95% CI 1.13, 1.61)] than in the highesttertile.320A 41% higher risk of CV mortality [RR 1.41 (95% CI 1.18, 1.68)] and 57%higher risk of all-cause mortality [RR 1.57 (95% CI 1.36, 1.81)] has beenreported in the lowest vs. highest quintile.321 A much smaller effect was observedin RCTs: an 11% risk reduction in all-cause mortality was observed forvitamin D3 supplementation [RR 0.89 (95% CI 0.80, 0.99)], but not forvitamin D2 supplementation.320 Due to a lack of power, it was not possible tolook at CV mortality specifically. Therefore, conclusions about vitamin Dsupplementation [type of supplement (D2 or D3), dosage and duration] for CVprevention cannot yet be drawn.
3a.5.5. Fibre
Recent meta-analyses of prospective cohort studies show that a 7 g/day higherintake of total fibre is associated with a 9% lower risk of CAD [RR 0.91(95% CI 0.87, 0.94)]322 and a 10 g/day higher fibre intake is associated witha 16% lower risk of stroke [RR 0.84 (95% CI 0.75, 0.94)]323 and a 6% lowerrisk of type 2 DM [RR 0.94 (95% CI 0.91, 0.97)].324 There is no evidence yet for asimilar association with fibre from fruits and vegetables. Although themechanism has not been elucidated completely, it is known that a high fibreintake reduces postprandial glucose responses after carbohydrate-rich mealsand lowers total cholesterol and LDL-C levels.
3a.5.6 Foods and food groups
3a.5.6.1 Fruits and vegetables
Prospective cohort studies have shown a protective effect of theconsumption of fruits and vegetables on CVD, but RCTs are scarce. Ameta-analysis reported a decrease of 4% [RR 0.96 (95% CI 0.92, 0.99)] inCV mortality for each additional serving of fruits (equivalent to 77 g)and vegetables (equivalent to 80 g) per day, while all-cause mortalitydid not reduce further with intakes of more than fiveservings.325 A meta-analysis reported a risk reduction forstroke of 11% [RR 0.89 (95% CI 0.83, 0.97)] for three to five dailyservings of fruits and vegetables and of 26% [RR 0.74 (95% CI 0.69,0.79)] for more than five servings compared with less than threeservings.326 A meta-analysis on CAD reported a 4% decrease inCAD risk [RR 0.96 (95% CI 0.93, 0.99)] for each additional serving offruits and vegetables per day.327
3a.5.6.2 Nuts
A meta-analysis of prospective cohort studies has shown that dailyconsumption of 30 g of nuts reduces the risk of CVD by ∼30% [RR 0.71(95% CI 0.59, 0.85)].328 It must be noted that the energy density ofnuts is high.
3a.5.6.3 Fish
The protective effect of fish on CVD is attributed to the n-3 fatty acidcontent. Pooled risk estimates from prospective cohort studies show thateating fish at least once a week results in a 16% reduction in the riskof CAD [RR 0.85 (95% CI 0.75, 0.95)] compared with eating lessfish.329 A recent meta-analysis showed that eating fish twoto four times a week reduces the risk of stroke by 6% [RR 0.94 (95% CI0.90, 0.98)] compared with eating fish less than once a week.330 The relationbetween fish intake and CV risk is not linear. Especially in the rangeof no or very low intake, risk is increased. The public health impact ofa small increase in fish consumption in the general population istherefore potentially large.
For fish oil, three randomized controlled prevention trials have beenpublished. All three trials, in post-AMI or CAD patients who received anextra amount of 400–1000 g EPA/DHA daily, did not observe a reduction inCV events in the intervention group. A recent meta-analysis of 20trials, mostly prevention of recurrent CV events and mostly using fishoil supplements, showed no benefit of fish oil supplementation on CVoutcomes.315
3a.5.6.4 Alcoholic beverages
Drinking three or more alcoholic beverages per day is associated withelevated CVD risk. Results from epidemiological studies suggest a lowerrisk of CVD occurring with moderate (one to two units per day) alcoholconsumption compared with non-drinkers. This association appears not tobe explained by special characteristics of abstainers,331 although thepotential for residual confounding and reverse causality cannot be fullyexcluded. Moreover, a recent Mendelian randomization study includinganalyses from 59 epidemiological studies has shed doubt on anybeneficial effect of moderate alcohol consumption,332 suggestingthat the lowest risks for CV outcomes were in abstainers and that anyamount of alcohol is associated with elevated BP and BMI.
3a.5.6.5 Soft drinks and sugar
Sugar-sweetened soft drinks are the largest single food source ofcalories in the US diet and are important in Europe. In children andadolescents, beverages may now even account for 10–15% of the caloriesconsumed. Regular consumption of soft drinks has been associated withoverweight, metabolic syndrome and type 2 DM. Substitution ofsugar-sweetened soft drinks with artificially sweetened drinks resultedin less weight gain in children over an 18-month period.333Sugar-sweetened beverages also cause weight gain in adults. Regularconsumption of sugar-sweetened beverages (i.e. two servings per daycompared with one serving per month) was associated with a 35% higherrisk of CAD in women, even after other unhealthy lifestyle and dietaryfactors were accounted for, whereas artificially sweetened beverageswere not associated with CAD. The WHO guideline recommends a maximumintake of 10% of energy from sugar (mono- and disaccharides), whichincludes added sugars as well as sugars present in fruits and fruitjuices.334
3a.5.7 Functional foods
Functional foods containing phytosterols (plant sterols and stanols) areeffective in lowering LDL-C levels by an average of 10% when consumed inamounts of 2 g/day. The cholesterol-lowering effect is in addition to thatobtained with a low-fat diet or use of statins. Further cholesterolreduction can be obtained with higher doses of phytosterols.335 No studies withclinical endpoints have been performed yet.
3a.5.8 Dietary patterns
Studying the impact of a total dietary pattern theoretically shows the fullpreventive potential of diet since it yields a combined estimate of theimpact of several favourable dietary habits. The Mediterranean dietcomprises many of the nutrients and foods that have been discussedpreviously: high intake of fruits, vegetables, legumes, wholegrain products,fish and unsaturated fatty acids (especially olive oil); moderateconsumption of alcohol (mostly wine, preferably consumed with meals) and lowconsumption of (red) meat, dairy products and saturated fatty acids. Ameta-analysis of prospective cohort studies has demonstrated that greateradherence to a Mediterranean diet is associated with a 10% reduction in CVincidence or mortality [pooled RR 0.90 (95% CI 0.87, 0.93)] and an 8%reduction in all-cause mortality [pooled RR 0.92 (95% CI 0.90,0.94)].336An RCT in high-risk individuals suggested that following a Mediterraneandiet over a 5 year period, compared with a control diet, was related to a29% lower risk of CVD [RR 0.71 (95% CI 0.56, 0.90)].337
Gaps in evidence
The biggest challenge in dietary prevention of CVD is to develop moreeffective strategies to make people change their diet (bothquantitatively and qualitatively) and to maintain that healthy dietand a normal weight.
Research into the substances in foods that underlie the protectiveeffects is ongoing.
3a.6 Body weight
Key messages
Both overweight and obesity are associated with an increased risk of CVDdeath and all-cause mortality. All-cause mortality is lowest with a BMIof 20–25 kg/m2 (in those <60 years of age); further weightreduction cannot be considered protective against CVD.
Healthy weight in the elderly is higher than in the young andmiddle-aged.
Achieving and maintaining a healthy weight has a favourable effect onmetabolic risk factors (BP, blood lipids, glucose tolerance) and lowerCV risk.
Recommendation for body weight
 |
 |
BP = blood pressure; CVD = cardiovascular disease; DM = diabetesmellitus.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dBMI 20–25 kg/m2. There is evidence thatoptimal weight in elderly is higher than in the young andmiddle-aged.339
Recommendation for body weight
 |
 |
BP = blood pressure; CVD = cardiovascular disease; DM = diabetesmellitus.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dBMI 20–25 kg/m2. There is evidence thatoptimal weight in elderly is higher than in the young andmiddle-aged.339
3a.6.1 Introduction
In many countries, favourable trends in major risk factors such as bloodcholesterol, BP and smoking prevalence have been observed, translating intoreduced CV mortality. However, BMI has greatly increased in all countriesover recent decades, resulting in a concomitant increase in the prevalenceof type 2 DM. In the USA, it has been projected that if obesity trends from2005 to 2020 continue, obesity will increasingly offset the positive effectsof declining smoking rates.340 The main clinical complications of increasing bodyweight are increases in BP, dyslipidaemia, insulin resistance, systemicinflammation and prothrombotic state and albuminuria and the development ofDM and CV events (HF, CAD, AF, stroke).
3a.6.2 Which index of obesity is the best predictor of cardiovascularrisk?
BMI [weight (kg)/height (m2)] can be measured easily and is usedextensively to define categories of body weight (see TableC in the web addenda).341 In addition to the amount of bodyfat, its distribution is important. Body fat stored in the abdomen(intra-abdominal fat) carries a higher risk than subcutaneous fat.
Several measures of body fatness are available (see Table Din the web addenda). Most data are available for BMI, waist:hipcircumference ratio and simple waist circumference. The optimal level formeasurement of waist circumference is midway from the lower rib margin tothe anterior superior iliac crest, in the standing position. The WHOthresholds for waist circumference are the most widely accepted in Europe.Based on these thresholds, two action levels are recommended:
(i) waist circumference ≥94 cm in men and ≥80 cm in women represents thethreshold at which no further weight should be gained and
(ii) waist circumference ≥102 cm in men and ≥88 cm in women represents thethreshold at which weight reduction should be advised.
These thresholds have been calculated based on Caucasians, and it is apparentthat different cut-offs for anthropometric measurements are required indifferent races and ethnicities. A meta-analysis concluded that both BMI andwaist circumference are similarly strong and continuously associated withCVD and type 2 DM.342 Therefore, BMI generally suffices in routinepractice.
3a.6.3 Does ‘metabolically healthy obesity’ exist?
The phenotype of ‘metabolically healthy obesity’ (MHO), defined by thepresence of obesity in the absence of metabolic risk factors, has gained alot of interest. Some studies argue that a specific subgroup of obeseindividuals is resistant to metabolic complications such as arterialhypertension and insulin resistance. However, MHO individuals present ahigher all-cause mortality compared with normal weight metabolically healthyindividuals.343,344Long-term results from the Whitehall study support the notion that MHO is atransient phase345moving towards glucometabolic abnormalities rather than a specific‘state’.
3a.6.4 The obesity paradox in established heart disease
At the population level, obesity is associated with CVD risk. However, amongthose with established CAD, the evidence is contradictory. Systematicreviews of patients with CAD or undergoing percutaneous coronaryintervention have suggested an ‘obesity paradox’ whereby obesity appearsprotective.338,346This is also the case for HF patients. However, this evidence should not bemisinterpreted to recommend higher target BMIs for those with establishedCVD since reverse causality may be operating. Cardiorespiratory fitnessmight influence relationships between adiposity and clinical prognosis inthe obesity paradox. Normal weight unfit individuals have a higher risk ofmortality than fit individuals, regardless of their BMI. Overweight andobese fit individuals have mortality risks similar to normal weight fitindividuals.347 Furthermore, the results of the EPIC study suggestthat the influence of physical inactivity on mortality appears to be greaterthan that of high BMI.348
3a.6.5 Treatment goals and modalities
CVD risk has a continuous positive relationship with BMI and other measuresof body fat. Because all-cause mortality appears to increase at BMI levels<20,339we do not recommend such low BMI levels as treatment goals.
Although diet, exercise and behaviour modifications are the mainstaytherapies for overweight and obesity, they are often unsuccessful forlong-term treatment. Medical therapy with orlistat and/or bariatric surgeryare additional options. A recent meta-analysis indicates that patientsundergoing bariatric surgery have a reduced risk of MI, stroke, CV eventsand mortality compared with non-surgical controls.349
Gaps in evidence
Knowledge and implementation of effective strategies to achieveweight loss and maintain a long-term healthy weight.
Identification of the relative roles of diet, exercise and behaviourmodification in the management of overweight and obese people.
The optimal level of BMI over the life course (at older ages andafter a CV event).
3a.7 Lipid control
Key messages
Elevated levels of plasma LDL-C are causal to atherosclerosis.
Reduction of LDL-C decreases CV events.
Low HDL-C is associated with increased CV risk, but manoeuvres toincrease HDL-C have not been associated with a decreased CV risk.
Lifestyle and dietary changes are recommended for all.
Total CV risk should guide the intensity of the intervention.
Total cholesterol and HDL-C are adequately measured on non-fastingsamples, thus allowing non-HDL-C to be derived.
Recommendations for lipid control
 |
 |
CV = cardiovascular; HDL-C = high-density lipoproteincholesterol;
LDL-C = low-density lipoprotein cholesterol.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dNon-HDL-C is a reasonable and practical alternativetarget because it does not require fasting. Non HDL-C secondarytargets of <2.6, <3.3 and <3.8 mmol/L (<100, <130 and<145 mg/dL) are recommended for very high, high and low tomoderate risk subjects, respectively See section 3a.7.10 for moredetails.
eA view was expressed that primary care physicians mightprefer a single LDL-C goal of 2.6 mmol/L (100 mg/dL). Whileaccepting the simplicity of this approach and that it could beuseful in some settings, there is better scientific support for thethree targets matched to level of risk.
fThis is the general recommendation for those at veryhigh-risk. It should be noted that the evidence for patients withCKD is less strong.
Recommendations for lipid control
 |
 |
CV = cardiovascular; HDL-C = high-density lipoproteincholesterol;
LDL-C = low-density lipoprotein cholesterol.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dNon-HDL-C is a reasonable and practical alternativetarget because it does not require fasting. Non HDL-C secondarytargets of <2.6, <3.3 and <3.8 mmol/L (<100, <130 and<145 mg/dL) are recommended for very high, high and low tomoderate risk subjects, respectively See section 3a.7.10 for moredetails.
eA view was expressed that primary care physicians mightprefer a single LDL-C goal of 2.6 mmol/L (100 mg/dL). Whileaccepting the simplicity of this approach and that it could beuseful in some settings, there is better scientific support for thethree targets matched to level of risk.
fThis is the general recommendation for those at veryhigh-risk. It should be noted that the evidence for patients withCKD is less strong.
3a.7.1 Introduction
The crucial role of dyslipidaemia, especially hypercholesterolaemia, in thedevelopment of CVD is documented beyond any doubt by genetic, pathology,observational and intervention studies.
In blood plasma, lipids such as cholesterol and triglycerides circulate aslipoproteins in association with various proteins (apolipoproteins). Themain carrier of cholesterol in plasma (LDL-C) is atherogenic. The role oftriglyceride-rich lipoproteins is currently under active investigation:chylomicrons and large very-low-density lipoproteins (VLDLs) appear not tobe atherogenic, but very high concentrations of these triglyceride-richlipoproteins can cause pancreatitis. Remnant lipoproteins [total cholesterol− (LDL-C + HDL-C)] have recently been identified in Mendelian randomizationstudies as pro-atherogenic lipoproteins.
3a.7.2 Total and low-density lipoprotein cholesterol
Most cholesterol is normally carried in LDL-C. Over a wide range of plasmacholesterol concentrations, there is a strong and graded positiveassociation between total as well as LDL-C and risk of CVD.354 This associationapplies to men and women, and to those without CVD as well as withestablished CVD.
The evidence that reducing plasma LDL-C reduces CVD risk is unequivocal; theresults of epidemiological studies and trials with and without statins usingangiographic or clinical endpoints confirm that the reduction of LDL-C is ofprime concern in the prevention of CVD.38
Meta-analyses of many statin trials show a dose-dependent relative reductionin CVD with LDL-C lowering. Every 1.0 mmol/L reduction in LDL-C isassociated with a corresponding 20–25% reduction in CVD mortality andnon-fatal MI.350
3a.7.3 Apolipoprotein B
Apolipoprotein B (apoB; the main apoprotein of atherogenic lipoproteins)levels have also been measured in outcome studies in parallel withLDL-C.355Based on the available evidence, it appears that apoB is a similar riskmarker to LDL-C.356Also, there appears to be less laboratory error in the determination of apoBthan LDL-C, particularly in patients with marked hypertriglyceridaemia[>3.4 mmol/L (>300 mg/dL)], but there is no evidence that apoB is abetter predictor of CVD than LDL-C.357
3a.7.4 Triglycerides
Hypertriglyceridaemia is a significant independent CVD risk factor, but theassociation is far weaker than for hypercholesterolaemia.358 The risk isassociated more strongly with moderate than with very severehypertriglyceridaemia [>10 mmol/L (>∼900 mg/dL)], which is a riskfactor for pancreatitis. There are, however, no randomized trials to providesufficient evidence to derive target levels for triglycerides. Meta-analysessuggest that targeting triglycerides may reduce CVD in specific subgroupswith high triglycerides and low HDL-C. At present, fasting triglycerides>1.7 mmol/L (> ∼150 mg/dL) continue to be considered a marker ofincreased risk, but concentrations ≤1.7 mmol/L are not evidence-based targetlevels for therapy.
3a.7.5 High-density lipoprotein cholesterol
Low HDL-C is independently associated with higher CVD risk.359 Low HDL-C may evenrival hypercholesterolaemia (due to high concentrations of LDL-C) as a riskfactor for CAD.360The combination of moderately elevated triglycerides and low concentrationsof HDL-C is very common in patients with type 2 DM, abdominal obesity andinsulin resistance and in those who are physically inactive. This lipidpattern is also characterized by the presence of small, dense, atherogenicLDL particles. An HDL-C level <1.0 mmol/L (<40 mg/dL) in men and<1.2 mmol/L (<45 mg/dL) in women may be regarded as a marker ofincreased risk. Recent Mendelian randomization studies, however, cast doubton the causal role of HDL-C in CVD.361 Physical activity and otherlifestyle factors, rather than drug treatment, remain important means ofincreasing HDL-C levels.
3a.7.6 Lipoprotein(a)
Lipoprotein(a) [Lp(a)] is a low-density lipoprotein to which an additionalprotein called apolipoprotein(a) is attached. High concentrations of Lp(a)are associated with increased risk of CAD and ischaemic stroke and Mendelianrandomization studies support a causal role in CVD for Lp(a). There is norandomized intervention study showing that reducing Lp(a) decreases CVDrisk.362 Atpresent there is no justification for screening the general population forLp(a), but it may be considered in patients at moderate risk to refine riskevaluation or in subjects with a family history of early CVD.
3a.7.7 Apolipoprotein B/apolipoprotein A1 ratio
Apolipoprotein A1 (apoA1) is the major apoprotein of high-densitylipoprotein. It is beyond doubt that the apoB:apoA1 ratio is one of thestrongest risk markers.112,355However, there is insufficient evidence to support this variable as atreatment goal. Since the measurement of apolipoproteins is not available toall physicians in Europe, is more costly than currently used lipid variablesand only adds moderately to the information derived from currently appliedlipid parameters, its use is not recommended.
3a.7.8 Calculated lipoprotein variables
3a.7.8.1 Low-density lipoprotein cholesterol
LDL-C can be measured directly, but in most studies and in manylaboratories LDL-C is calculated using the Friedewald formula:363 Thecalculation is valid only when the concentration of triglycerides is<4.5 mmol/L (< ∼400 mg/dL). Similar problems may be faced whenLDL-C is low [< ∼1.3 mmol/L (<50 mg/dL)]. Direct methods may beless sensitive to plasma triglyceride levels. However, recent data showthat the direct methods may also be biased when triglyceride levels arehigh. Also, the values obtained with the different direct methods arenot necessarily identical, especially for low and high LDL-C values.
In mmol/L: LDL-C = total cholesterol − HDL-C − (0.45 ×triglycerides)
In mg/dL: LDL-C = total cholesterol − HDL-C − (0.2 ×triglycerides)
3a.7.8.2 Non-high-density lipoprotein cholesterol (accurate in non-fastingsamples)
Non-HDL-C comprises the cholesterol in low-density lipoprotein,intermediate-density lipoprotein, remnant and VLDL, thus capturing allthe information regarding pro-atherogenic lipoproteins. Non-HDL-Cpredicts CVD risk even better than LDL-C.351 LDL-C limits may betransferred to non-HDL-C limits by adding 0.8 mmol/L (30 mg/dL).Calculated by simply subtracting HDL-C from total cholesterol,non-HDL-C, unlike LDL-C, does not require the triglyceride concentrationto be <4.5 mmol/L (<400 mg/dL). Therefore, it is certainly abetter measure than calculated LDL-C for patients with increased plasmatriglyceride concentrations, but also has an additional advantage of notrequiring patients to fast before blood sampling. There is evidence fora role of non-HDL-C as a treatment target.364 Since non-HDL-C is capturingthe information regarding all the atherogenic apoB-containinglipoproteins, we suggest that it is a reasonable alternative treatmentgoal while acknowledging that it has not been an endpoint in therapeutictrials.
3a.7.8.3 Remnant cholesterol
Recently the remnant cholesterol [total cholesterol − (HDL-C + LDL-C)]has been shown to be causally related to atherosclerosis in Mendelianrandomization studies. This parameter, however, is not suggested as apredictor or main target for therapy and further population data andclinical studies are awaited.
3a.7.9 Exclusion of secondary and familial dyslipidaemia
The presence of dyslipidaemias secondary to other conditions must be excludedbefore beginning treatment, as treatment of underlying disease improveshyperlipidaemia without requiring antilipidaemic therapy. This isparticularly true for hypothyroidism. Secondary dyslipidaemias can also becaused by alcohol abuse, DM, Cushing's syndrome, diseases of the liver andkidneys and several drugs (e.g. corticosteroids). Patients who could havegenetic dyslipidaemias, such as FH, can be identified by extreme lipidabnormalities and/or family history. If possible, these patients should bereferred for specialist evaluation. The treatment recommendations in thisguideline may not apply to these specific patients, who are dealt with indetail in the ESC/European Atherosclerosis Society guidelines ondyslipidaemias.38,352An LDL-C >5.1 mmol/L (>200 mg/dL) in therapy-naive patients requirescareful evaluation for possible FH. However, in the presence of prematureCVD or family history, possible FH should be considered at lower LDL-Clevels.
3a.7.10 Who should be treated and what are the goals?
In general, RCTs are the ideal evidence base for decisional thresholds andtreatment goals. For treatment goals, this requires RCTs randomly allocatingsubjects to different lipid goal levels. However, most evidence in terms oftreatment goals is derived from observational studies and from post hocanalyses of RCTs (and meta-regression analyses thereof) randomly allocatingdifferent treatment strategies (and not treatment goals). Hence,recommendations reflect consensus based on large-scale epidemiological dataand RCTs comparing treatment regimens, not on RCTs comparing different lipidgoal levels.
In the past, an LDL-C of 2.6 mmol/L (100 mg/dL) has been considered atreatment threshold and goal. This goal remains reasonable for most patientswho have an indication for LDL-C-lowering therapy based on calculation ofthe CV risk (see section 2).
Evidence from trials has suggested that lowering LDL-C to ≤1.8 mmol/L (<70mg/dL) is associated with a lower risk of recurrent CVD events.365 Therefore, anLDL-C level of 1.8 mmol/L (70 mg/dL) appears to be a reasonable goal forprevention of recurrent CV events and in other very-high-risk subjects. Atreatment goal of an LDL-C reduction of at least 50% is also recommended ifthe baseline LDL-C level is 1.8–3.5 mmol/L (70–135 mg/dL).
Non-HDL-C target values may be an alternate target if non-fasting samples areobtained, and goals should be <2.6, <3.3 and <3.8 mmol/L (<100,<130 and <145 mg/dL) with very high, high and low to moderate CV risk,respectively. In addition, this is a secondary goal in people with elevatedtriglycerides. In the same subjects, although not generally recommended,apoB levels at <80 and <100 mg/dL can be reasonable goals for subjectswith very high and high CV risk, respectively.
The benefit of cholesterol-lowering therapy depends on initial levels ofrisk: the higher the risk, the greater the benefit in absolute riskreduction (Table 13). There are no differences in the relative reductionbetween men and women and between younger and older age or between thosewith and without DM.366
Possible intervention strategies as a function of totalcardiovascular risk and low-density lipoprotein cholesterollevel
 |
 |
CV = cardiovascular;; LDL-C = low-density lipoproteincholesterol; SCORE = Systematic Coronary Risk Estimation.
aClass of recommendation.
bLevel of evidence.
Guidance on the use of drug treatment must be interpreted in thelight of the physician’s judgement and knowledge with regards tohis or her individual patient. Note that risk stratification isnot applicable in familial hypercholesterolaemia, where drugtreatment is recommended, and that, in this table, drugtreatment may be considered at risks lower than the generictreatment thresholds indicated in paragraph 2.3.5. Thustreatment may occasionally be considered in moderate risk (1–5%)individuals, provided that patients are well-informed of thelimited absolute risk reduction, and high numbers needed totreat. In higher risk (5–10%), drug therapy is associated withsomewhat larger absolute benefits, and should at least beconsidered. Drug therapy is strongly advised in those at veryhigh risk (≥10%). If baseline LDL-C in this category is alreadybelow the target level of 1.8 mmol/L, benefit of statin therapyinitiation is less certain, but may still be present.
Possible intervention strategies as a function of totalcardiovascular risk and low-density lipoprotein cholesterollevel
 |
 |
CV = cardiovascular;; LDL-C = low-density lipoproteincholesterol; SCORE = Systematic Coronary Risk Estimation.
aClass of recommendation.
bLevel of evidence.
Guidance on the use of drug treatment must be interpreted in thelight of the physician’s judgement and knowledge with regards tohis or her individual patient. Note that risk stratification isnot applicable in familial hypercholesterolaemia, where drugtreatment is recommended, and that, in this table, drugtreatment may be considered at risks lower than the generictreatment thresholds indicated in paragraph 2.3.5. Thustreatment may occasionally be considered in moderate risk (1–5%)individuals, provided that patients are well-informed of thelimited absolute risk reduction, and high numbers needed totreat. In higher risk (5–10%), drug therapy is associated withsomewhat larger absolute benefits, and should at least beconsidered. Drug therapy is strongly advised in those at veryhigh risk (≥10%). If baseline LDL-C in this category is alreadybelow the target level of 1.8 mmol/L, benefit of statin therapyinitiation is less certain, but may still be present.
3a.7.11 Patients with kidney disease
CKD can be characterized by mixed dyslipidaemia (high triglycerides, highLDL-C and low HDL-C).367 Statin therapy has a beneficial effect on CVD outcomesin CKD368 and insome studies slows the rate of kidney function loss.369,370 Similar data have been observedfor combination therapy of a statin with ezetimibe, but not for ezetimibealone.368For patients with end-stage renal disease, we recommend that hypolipidaemictherapy should not be initiated. If patients with CKD already on ahypolipidaemic therapy enter end-stage renal disease, the therapy may bemaintained.368
3a.7.12 Drugs
The currently available lipid-lowering drugs include inhibitors of3-hydroxy-3-methylglutaryl-coenzyme A reductase (statins), fibrates, bileacid sequestrants (anion exchange resins), niacin (nicotinic acid),selective cholesterol absorption inhibitors (e.g. ezetimibe) and, morerecently, proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors.Response to all therapy varies widely among individuals and thereforemonitoring the effect on LDL-C levels is recommended.
Statins, by decreasing LDL-C, reduce CV morbidity and mortality as well asthe need for coronary artery interventions.371,372 Statins at doses that effectively reduce LDL-C byat least 50% also seem to halt progression or even contribute to regressionof coronary atherosclerosis.373 Statins also lower triglycerides, andmeta-analysis evidence shows statins may also lower pancreatitisrisk.374Therefore, they should be used as the drugs of first choice in patients withhypercholesterolaemia or combined hyperlipidaemia.
Data indicate that combination therapy with ezetimibe also brings a benefitthat is in line with the Cholesterol Treatment Trialists' (CTT)Collaboration meta-analysis supporting the notion that LDL-C reduction iskey to the achieved benefit independent of the approach used.353,375
Increased levels of liver enzymes in plasma occur occasionally during statintherapy, and in most cases are reversible. Routine monitoring of liverenzyme values is not indicated. In addition, 5–10% of patients receivingstatins complain of myalgia, but rhabdomyolysis is extremely rare. The riskof myopathy (severe muscular symptoms) can be minimized by identifyingvulnerable patients and/or by avoiding statin interactions with specificdrugs376(see Table E in web addenda). Because statins are prescribed on a long-termbasis, possible interactions with other drugs deserve particular andcontinuous attention, as many patients will receive pharmacological therapyfor concomitant conditions.377 In practice, management of a patient with myalgiabut without a major creatinine kinase increase is based on trial and errorand usually involves a trial of a different statin or the use of a very lowdosage several days a week with a gradual increase.376
In general, the safety profile of statins is acceptable, and earlierobservations that lipid-lowering treatment may contribute to an increase innon-CV mortality (e.g. cancers, suicides, depression) or mental disorderswere not confirmed in a large meta-analysis.378 Increased blood sugar and glycatedhaemoglobin (HbA1c) levels (i.e. increased risk of type 2 DM) occur afterstatin treatment and are dose dependent, in part linked to very slightweight gain, but the benefits of statins outweigh the risks for the vastmajority of patients.377–379 Patients should be reminded that adhering tolifestyle changes when prescribed a statin should lessen any modest DMrisk.379–382
For non-statin treatments, selective cholesterol absorption inhibitors (e.g.ezetimibe) are not usually used as monotherapy to decrease LDL-Cconcentrations, unless patients are intolerant to statins. They arerecommended as combination therapy with statins in selected patients when aspecific goal is not reached with the maximal tolerated dose of astatin.
Bile acid sequestrants also decrease total cholesterol and LDL-C but arepoorly tolerated and tend to increase plasma triglyceride concentrations.They are therefore not recommended for routine use in CVD prevention.
Fibrates and niacin are used primarily for triglyceride lowering andincreasing HDL-C, while fish oils (n-3 fatty acids) in doses of 2–4 g/dayare used for triglyceride lowering.360 Evidence supporting the use ofthese drugs for CVD event reduction is limited and, given the strongevidence favouring statins, routine use of these drugs in CVD prevention isnot recommended. In order to prevent pancreatitis, when triglycerides are>10 mmol/L (>900 mg/dL) they must be reduced not only by drugs butalso by restriction of alcohol, treatment of DM, withdrawal of oestrogentherapy, etc. In those rare patients with severe primaryhypertriglyceridaemia, specialist referral must be considered.
Regarding new therapies, recent data from phase I–III trials show that PCSK9inhibitors sharply decrease LDL-C by up to 60%, either as monotherapy or inaddition to the maximal statin dose. Whether this approach results in thepredicted reduction in CV events is being addressed in large outcome trials;preliminary evidence suggests that this is the case.383–385
3a.7.13 Drug combinations
Patients with dyslipidaemia, particularly those with established CVD, DM orasymptomatic high-risk individuals, may not always reach treatment goals,even with the highest tolerated statin dose. Therefore, combinationtreatment may be needed. It must be stressed, however, that the onlycombination that has evidence of clinical benefit (one large RCT) is that ofa statin combined with ezetimibe.353 Based on the relatively limited body of evidence,clinicians may restrict the use of this combination to patients at high orvery-high risk of CVD.
Combinations of niacin and a statin increase HDL-C and decrease triglyceridesbetter than either of these drugs alone, but flushing is the main adverseeffect of niacin, which may affect compliance. Furthermore, there is noevidence of clinical benefit for this combination.386
Fibrates, particularly fenofibrate, may be useful, not only for decreasinghigh triglyceride concentrations and increasing low HDL-C, but for loweringLDL-C further when used with a statin. There is limited evidence for thiscombination in terms of a reduction in CVD events. In selected cases,however, this approach may be considered, such as when, during statintreatment, triglycerides remain high and/or HDL-C is very low. Other drugsmetabolized through cytochrome P450 should be avoided when this combinationis prescribed. Fibrates should preferably be taken in the morning andstatins in the evening to minimize peak dose concentrations and decrease therisk of myopathy. Patients have to be instructed about warning symptoms(myalgia), even though such adverse effects are very rare. Gemfibrozilshould not be added to a statin treatment, because of the high potential forinteractions.
If target levels cannot be reached even on maximal doses of lipid-loweringtherapy or drug combinations, patients will still benefit from treatment tothe extent that the dyslipidaemia has been improved. In these patients,increased attention to other risk factors may help to reduce total risk.
Gaps in evidence
Triglyceride or HDL-C values as a target for therapy.
Whether Lp(a) lowering against background statin therapy can reducethe risk of CVD.
How to increase adoption of non-HDL-C and non-fasting samples inclinical practice.
Whether functional foods and food supplements with a lipid-loweringeffect can safely reduce the risk of CVD.
3a.8 Diabetes mellitus (type 2 and type 1)
Key messages
The multifactorial approach is very important in patients with type 2DM.
Lifestyle management to aid weight control by sustainable dietary changesand increased PA levels should be central in the management of patientswith type 2 DM.
Intensive management of hyperglycaemia reduces the risk of microvascularcomplications and, to a lesser extent, the risk of CVD. However, targetsshould be relaxed in the elderly, frail, those with long-duration DM andthose with existing CVD.
Intensive treatment of BP in DM, with a target of 140 mmHg systolic forthe majority, reduces the risk of macrovascular and microvascularoutcomes. A lower SBP target of 130 mmHg further lessens the risks forstroke, retinopathy and albuminuria and should be applied to selectedpatients.
Lipid lowering is a key mechanism to lower CVD risk in both type 2 andtype 1 DM. All patients >40 years of age and selected youngerpatients at elevated risk are recommended for statin therapy.
In DM patients with existing CVD, the use of a sodium-glucoseco-transporter-2 (SGLT2) inhibitor substantially lessened CVD and totalmortality and HF hospitalisation without major adverse effects. SGLT2inhibitors should be considered early in the course of DM management insuch patients.
Recent evidence points to sizeable reductions in CVD mortality in DMpatients via improvements in risk factor management, although theincreasing worldwide DM prevalence will create major challenges. Moreshould be done to prevent DM.
People with DM are on average at double the risk of CVD.399 A simple DM riskquestionnaire can guide which patients without CVD should be tested forDM.400
Keeping close to the recommended targets for BP, lipid control, glycaemia andHbA1c is important for the prevention of CVD. Clear reductions have occurred inCVD death rates in DM consistent with better management of risk factors,although the increasing prevalence of DM continues to create pressures on allhealth care systems.
The targets, especially the glycaemic and in some cases lipids, should be lessstringently implemented in older people with DM, those with a longer duration ofDM, those with evidence of CVD and the frail.401
There is mounting evidence for a very high relative risk in younger individualswith type 2 DM (age <40 years),402 and additional guidance on care is needed.
Except for glucose management, prevention of CVD follows the same generalprinciples as for people without DM. Achieving low BP levels and low LDL-C andtotal cholesterol concentrations is particularly important. Many treatmenttargets are more stringent for patients with DM. Typically, patients with type 2DM have multiple CVD risk factors, each requiring treatment according toexisting guidelines.
3a.8.1 Lifestyle intervention
The ESC and European Association for the Study of Diabetes scientificstatements advocate lifestyle management as a first measure for theprevention and management of DM.387 Most patients with DM are obese, so weight controlis a central component. Several dietary patterns can be adopted where thepredominance of fruits, vegetables, wholegrain cereals and low-fat proteinsources is more important than the precise proportions of total energyprovided by the major macronutrients. Salt intake should be restricted.Specific dietary recommendations include limiting saturated and trans fatsand alcohol intake, monitoring carbohydrate consumption and increasingdietary fibre. A Mediterranean-type diet is acceptable, where fat sourcesare derived primarily from monounsaturated oils.
A combination of aerobic and resistance exercise training is effective in theprevention of the progression of DM and for the control of glycaemia. Littleis known about how to promote and sustain PA; however, reinforcement byhealth care providers to patients to find sustainable ways to increase PA iscrucial. Smoking increases the risk of DM, CVD and premature death andshould be strongly discouraged (see section 3a.4.5).387,403 Lifestyle intervention can alsoprevent DM development in those at elevated risk and, in turn, lowers futuremicrovascular and macrovascular risks.404
3a.8.2 Cardiovascular risk
At diagnosis or in those with a short duration of disease, DM is not a CADrisk equivalent state.405,406In general, risk levels approach CAD risk equivalence after about a decadeor in those with proteinuria or low eGFR.406–408 Emerging datasuggest that patients who develop DM at a younger age have a highcomplication burden.402 People with DM with existing CAD have a vascular riskwell in excess of those with CAD but without DM and a substantially lowerlife expectancy.409
Statins are recommended for all those newly diagnosed with type 2 DM beyond acertain age (>40 years is currently recommended). This recommendationreflects greater lifetime vascular risk trajectories in these individuals.However, a proportion of DM patients at 40–50 years of age may have a low 10year risk of CVD due to normal BP and lipid levels and being non-smokers,and in such cases there remains a role for physician judgement. Equally, insome patients <40 years of age with type 2 DM with evidence of end-organdamage or significant risk factors, statins may be indicated.
3a.8.3 Glucose control
The UK Prospective Diabetes Study (UKPDS) established the importance ofintensive glucose lowering with respect to CVD risk reduction in newlydiagnosed patients with DM but not treated with modern BP- or lipid-loweringtherapies, with the best evidence to support metformin, leading to itsposition as first-line therapy. Three trials were conducted to see if CVevents could be reduced further with more intensive glycaemia treatment andlower target HbA1c levels.389,393,410 However, theresults were surprising, with unexpected increases in total and CVD deathsin the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial anda trend towards an increase in CVD death in the Veterans Affairs DiabetesTrial (VADT). The results prompted concerns about the safety of intensiveglucose lowering and the appropriateness of pursuing tight glucose control,particularly in older people with DM and in those with existing CVD.Subsequent meta-analyses of intensive glucose control, including data fromUKPDS, Prospective Pioglitazone Clinical Trial in Macrovascular Events(PROactive), ACCORD, Action in Diabetes and Vascular disease: PreterAx andDiamicron MR Controlled Evaluation (ADVANCE) and VADT,411 showed significantreductions in non-fatal AMI and CAD events, but no effect on stroke or totalmortality.412,413The additional analyses of these trials suggested that CVD benefits for anaverage HbA1c reduction of ∼0.9% over 5 years were far less than via usualreductions in cholesterol and BP seen with statins and available BP-loweringagents. Four recent trials of newer DM therapies (DPP-4 and GLP-1)414–417 inpatients with DM and existing CVD or at high risk demonstratednon-inferiority (i.e. safety) but not superiority with respect to CVD risk.There was, however, an increase in the rate of hospitalization for HF withsaxagliptin in the Saxagliptin Assessment of Vascular Outcomes Recorded inPatients with Diabetes Mellitus – Trombolysis in Myocardial Infarction(SAVOR-TIMI 53) trial.416
Very recently, the SGLT2 inhibitor empagliflozin demonstrated substantialreductions in CVD death (by 38%) and all-cause mortality (by 32%), as wellas in hospitalisation for HF (by 35%), as compared with standard care,suggesting use of an SLGT2 inhibitor should come very early in the course ofmanagement of patients with DM and CVD.394 The pattern of trial resultswhereby non-fatal MI and stroke were not reduced by active treatment, aswell as the rapid separation of mortality curves, suggest that the mechanismof benefit was likely to relate more to cardio-renal haemodynamic effectsthan to atherothrombotic actions or effects of glucose lowering per se. Moreresearch on understanding the trial results is needed.
3a.8.4 Blood pressure
In people with type 2 DM, apart from lifestyle interventions, the reductionof BP (along with cholesterol) should be targeted as strictly as targetingglucose/HbA1c levels. BP targets should be considered regardless of overallCV risk score in patients with type 2 DM.
Hypertension is more common in patients with type 2 DM compared with thegeneral population. A recent systematic review and meta-analysis ofrandomized trials of BP-lowering agents in >100 000 patients with type 2DM confirmed that lowering BP reduces the risk of all-cause mortality, CVevents, CAD events, stroke, HF, retinopathy, new or worsening albuminuriaand renal failure.418 The results were similar when trials with low risk ofbias were selected. Furthermore, a systolic target <140 mmHg lessens therisk of total mortality and most separate outcomes. Further reductions inthe risk for albuminuria, retinopathy and stroke, but not in overallsurvival or aggregate clinical endpoints, were achieved with a systolictarget <130 mmHg. In people >80 years of age, targets should be sethigher, aiming for <150/90 mmHg, unless renal impairment is present.
Combination treatment is commonly needed to lower BP effectively in DM. AnACE-I or an angiotensin receptor blocker (ARB), where tolerated, shouldalways be included as first-line therapy because of the evidence of superiorprotective effects against initiation or progression of nephropathy.
3a.8.5 Lipid-lowering therapy
The Heart Protection Study (HPS) demonstrated that treatment with simvastatin40 mg reduced the risk of CAD and stroke in people with DM and individualswithout DM who had no prior AMI or angina pectoris.372 Further robustsupport for statin benefit came from the Collaborative Atorvastatin DiabetesStudy (CARDS), which compared 10 mg atorvastatin with placebo,371 and from the CTTmeta-analysis in DM patients.419 There is also trial evidence to show greater CVDrisk reduction with more intense statin therapy in DM patients.395 More recent trialevidence shows a clear CVD benefit of lowering LDL-C with ezetimibe on topof a statin in patients with type 2 DM.353 Emerging evidence also shows thatPCSK9 inhibitors are equally efficacious in lowering LDL-C in type 2 DMpatients, although results of CV outcome trials are awaited. Lower treatmenttargets should be pursued in patients with type 2 DM who have overt CVD orCKD.
While the most common lipid abnormality in type 2 DM is elevated triglycerideand low HDL-C, trials examining possible CVD benefits of lipid (mainlytriglyceride) lowering with fibrates in DM have not been positive. The USFood and Drug Administration (FDA) states that the current evidence base isinsufficient to support fibrates for CVD protection and that more trialevidence is needed.420
Prescribing of lipid-lowering agents in older people with DM (>85 years)requires special consideration because exposure to higher doses (or higherpotency) may not increase life expectancy, but may increase the risk ofadverse effects.
3a.8.6 Antithrombotic therapy
Patients with type 1 or type 2 DM have an increased tendency to developthrombotic phenomena. The Antiplatelet Trialists' Collaborationmeta-analysis demonstrated the benefits of antithrombotic therapy (mainlyaspirin) in patients with DM with clinically established CAD,cerebrovascular disease or other forms of thrombotic disease, with a 25%reduction in risk of CV events.421
The role of aspirin in patients without CVD remains unproven. A meta-analysisof six RCTs found no statistically significant reduction in the risk ofmajor CV events or all-cause mortality when aspirin was compared withplacebo or no aspirin in people with DM and no pre-existing CVD.398 Further trials areongoing.
3a.8.7 Microalbuminuria
Microalbuminuria (urinary albumin excretion from 30 to 300 mg/24 h) predictsthe development of overt nephropathy in patients with type 1 or type 2 DM,while the presence of overt proteinuria (300 mg/24 h) generally indicatesestablished renal parenchymal damage. In patients with DM and hypertension,microalbuminuria—even below the current threshold values—predicts CV events,and a continuous relationship between CV as well as non-CV mortality andurinary protein:creatinine ratios has been reported. Microalbuminuria can bemeasured from spot urine samples (due to inaccuracy in sampling, 24 h ornight-time urine collection is discouraged) by indexing the urinary albuminconcentration to the urinary creatinine concentration (2.5/3.5–25/35mg/mmol). Patients with DM and microalbuminuria or proteinuria should betreated with an ACE-I or ARB regardless of baseline BP.
Gaps in evidence
There is a need to examine whether a type 2 DM CV risk score based oneither 10 year or lifetime risk helps to improve targeting ofpreventative therapies and leads to a reduction in CV risk or a gainin lifetime years free from disease.
Further trial data are needed to establish if the empagliflozinoutcome findings hold for other classes of SGLT2 inhibitors and tobetter understand the mechanisms of benefit. It would also be usefulto know if SGLT2 inhibitors lessen CV mortality and HF risks inpatients with DM but without CVD.
More research on the benefits of glucagon-like peptide 1 (GLP-1)receptor agonists on CVD risk is needed and trials are due to bereported in subsequent years. Early evidence suggests no CVD benefitwith short-term use of dipeptidyl peptidase 4 (DPP-4) inhibitors inpeople at high risk for CVD, as reviewed.422
3a.8.8 Type 1 diabetes
Key messages Type 1 DM is the result of a lack of insulinproduction in the pancreas, confirmed by absent or virtually absentC-peptide levels. The average age of onset is ∼14 years, although persons ofany age can develop type 1 DM. Type 1 DM should be suspected in any patientwho progresses to insulin within the first year of diagnosis. A largecontemporary study in Scotland observed a relative risk for CVD events of2.3 in men and 3 in women with type 1 DM compared with the generalpopulation,423 suggesting CVD risks may have declined over time,commensurate with improvements in life expectancy.424 Another report from Swedendemonstrated CVD mortality rates in type 1 DM to be twice the rates of thegeneral population in those with HbA1c levels <6.9% (52 mmol/mol),whereas risk was especially high (∼10-fold) in those with very poor control[≥9.7% (≥83 mmol/mol)].425 In the majority of studies, the risk of CVD eventsor mortality was highest among those with diabetic nephropathy,macroalbuminuria or CKD. The presence of proliferative retinopathy andautonomic neuropathy also signalled an elevated CVD risk.
CVD and mortality risks have decreased in type 1 DM patients butremain unacceptably elevated in those with very poor glycaemiccontrol or any evidence of kidney disease.
Intensive management of hyperglycaemia in DM reduces the risk ofmacrovascular complications and premature mortality; a target of6.5–7.5% (48–58 mmol/mol) HbA1c is recommended.
The recommended BP target in the majority of patients with type 1 DMis 130/80 mmHg.
Lipid-lowering agents targeting LDL-C reduction should be recommendedto the majority of patients >40 years of age and to those youngerthan this with evidence of nephropathy or with multiple riskfactors.
The Diabetes Control and Complications Trial (DCCT) established theimportance of tight glucose control to lessen the risks of bothmicrovascular and macrovascular disease. A 27 year follow-up of this trialshowed that 6.5 years of initial intensive DM therapy in type 1 DM wasassociated with a modestly lower all-cause mortality rate when compared withconventional therapy.426 A glycaemic target for HbA1c of 6.5–7.5% (48–58mmol/mol) appears to be a balanced approach for long-term care of patientswith type 1 DM. The use of insulin analogues, insulin pumps and continuousglucose monitoring to improve glycaemic control while minimizinghypoglycaemia is the subject of intense research, as is the use of agents(e.g. metformin, GLP-1 agonists) commonly used in type 2 DM.
The CTT suggested lipid lowering with statins is as equally effective in type1 patients as in type 2.427 All patients >40 years of age with type 1 DMshould be recommended for statins unless they have a short duration of DMand no other risk factors. Younger patients with multiple risk factors orevidence of end organ damage (albuminuria, low eGFR, proliferativeretinopathy or neuropathy) should be considered for statin therapy.
A target BP of 130/80 mmHg is accepted practice in type 1 DM, with evidenceof specific benefits of ACE-Is or ARBs on the early development and laterprogression of microvascular disease in younger type 1 DM patients. A lowertarget BP of 120/75–80 mmHg may be helpful in younger type 1 DM patients(<40 years of age) with persistent microalbuminuria. Studies supportingimproved CVD outcome in type 1 DM through BP reduction are lacking. As morepatients with type 1 DM are living to older age, SBP targets may need to berelaxed (140 mmHg) in some to avoid side effects.
Current evidence suggests many patients with type 1 DM >40 years of agecontinue to smoke, are still not receiving statins and, perhaps mostimportantly, have very poor glucose control.423 Further efforts to target theseestablished risk factors are needed.
Gaps in evidence
Further studies are needed on metformin and GLP-1 receptor agonistsin (subgroups of) patients with type 1 DM to determine whether theyimprove glycaemic control, aid in weight reduction and improveclinical outcomes.
There is a need for a CVD risk score in type 1 DM to better guideinitiation of preventative therapies in younger patients.
3a.9 Hypertension
Key messages
Elevated BP is a major risk factor for CAD, HF, cerebrovascular disease,PAD, CKD and AF.
The decision to start BP-lowering treatment depends on the BP level andtotal CV risk.
Benefits of treatment are mainly driven by BP reduction per se, not bydrug type.
Combination treatment is needed to control BP in most patients.
Recommendations for management of diabetes
 |
 |
BP = blood pressure; CV = cardiovascular; DM = diabetes mellitus;HbA1c = glycated haemoglobin; HDL-C = high-density lipoproteincholesterol; LDL-C = low-density lipoprotein cholesterol; SGLT2 =Sodium-glucose co-transporter-2.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dNon-HDL-C is a reasonable and practical alternativetarget because it does not require fasting. Non HDL-C secondarytargets of <2.6 and <3.3 mmol/L (<100 and <130 mg/dL)are recommended for very high, and high-risk subjects, respectivelySee section 3a.7.10 for more details.
Recommendations for management of diabetes
 |
 |
BP = blood pressure; CV = cardiovascular; DM = diabetes mellitus;HbA1c = glycated haemoglobin; HDL-C = high-density lipoproteincholesterol; LDL-C = low-density lipoprotein cholesterol; SGLT2 =Sodium-glucose co-transporter-2.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dNon-HDL-C is a reasonable and practical alternativetarget because it does not require fasting. Non HDL-C secondarytargets of <2.6 and <3.3 mmol/L (<100 and <130 mg/dL)are recommended for very high, and high-risk subjects, respectivelySee section 3a.7.10 for more details.
3a.9.1. Introduction
High BP is a leading risk factor for disease burden globally, accounting for9.4 million deaths and 7.0% of global disability-adjusted life-years (DALYs)in 2010.439Compared with 1990, the impact of high BP has increased by ∼2.1 milliondeaths.439Overall, the prevalence of hypertension is ∼30–45% in adult persons ≥18years of age, with a steep increase with ageing.
Elevated BP is a risk factor for CAD, HF, cerebrovascular disease, PAD, CKDand AF. The risk of death from either CAD or stroke increases progressivelyand linearly from BP levels as low as 115 mmHg systolic and 75 mmHgdiastolic upwards,440 although for absolute risk the curves flatten in thelower BP ranges.
3a.9.2 Definition and classifications of hypertension
The definition and classifications of hypertension are shown inTable 14.11
Definition and classification of blood pressurelevelsa
 |
 |
BP = blood pressure.
aBP levels in untreated individuals.
Definition and classification of blood pressurelevelsa
 |
 |
BP = blood pressure.
aBP levels in untreated individuals.
3a.9.3 Blood pressure measurement
Office BP is recommended for screening and diagnosis of hypertension, whichshould be based on at least two BP measurements per visit and on at leasttwo visits. If the BP is only slightly elevated, repeated measurementsshould be made over a period of several months to achieve an acceptabledefinition of the individual's ‘usual’ BP and to decide about initiatingdrug treatment. If BP is more markedly elevated or accompanied by targetorgan damage, other CV factors or established CV or renal disease, repeatedBP measurements are required within a shorter period in order to maketreatment decisions.
3a.9.4 Office or clinic blood pressure measurement
Auscultatory or oscillometric semi-automatic sphygmomanometers should bevalidated and checked periodically.441 Measurement of BP at the upper armis preferred, and cuff and bladder dimensions should be adapted to the armcircumference. If feasible, automated recording of multiple BP readings inthe office, with the patient seated in an isolated room, might be consideredas a means of improving reproducibility and matching office BP values closerto those provided by daytime ambulatory BP monitoring (ABPM) or home BPmeasurements (HBPMs).442 Note that automated devices are not validated for BPmeasurement in patients with AF.
3a.9.5 Out-of-office blood pressure monitoring
Out-of-office BP is commonly assessed by ABPM or HBPM, usually byself-measurement; it is usually lower than the office BP and the differenceincreases as office BP increases (Table 15).443
Blood pressure thresholds for definition of hypertension withdifferent types of BP measurement
 |
 |
DPB = diastolic blood pressure; SBP = systolic bloodpressure.
Blood pressure thresholds for definition of hypertension withdifferent types of BP measurement
 |
 |
DPB = diastolic blood pressure; SBP = systolic bloodpressure.
The following general principles and remarks should be taken into account:(i) the procedure should be adequately explained to the patient, with verbaland written instructions; (ii) interpretation of the results should takeinto account that the reproducibility of out-of-office BP measurements isreasonably good for 24 h, day and night BP averages, but less so for shorterperiods; (iii) ABPM and HBPM provide somewhat different information on thesubject's BP status and risk, and the two methods should thus be regarded ascomplementary rather than competitive; (iv) devices should be validated andregularly calibrated, at least every 6 months.
Both ABPM and HBPM values are closely related to prognosis.444 Night-time BPseems to be a stronger predictor than daytime BP. Out-of-office measurementmay be useful not only in untreated subjects, but also in treated patients,with the aim of monitoring the effects of treatment and increasingcompliance with drug therapy (Table 16).
Clinical indications for the use of out-of-office blood pressuremeasurements (home blood pressure measurement, ambulatory bloodpressure measurement)
 |
 |
ABPM = ambulatory blood pressure monitoring; BP = bloodpressure;
CKD = chronic kidney disease; CV = cardiovascular.
Clinical indications for the use of out-of-office blood pressuremeasurements (home blood pressure measurement, ambulatory bloodpressure measurement)
 |
 |
ABPM = ambulatory blood pressure monitoring; BP = bloodpressure;
CKD = chronic kidney disease; CV = cardiovascular.
3a.9.6 Diagnostic evaluation in hypertensive patients
Laboratory tests should include haemoglobin, fasting plasma glucose (HbA1c ifnot fasting) and serum tests for total cholesterol, HDL-C, triglycerides,potassium, uric acid, creatinine (and calculated renal function) andthyrotropin (in postmenopausal women). Urinalysis should includealbumin:creatinine ratio, dipstick test, sediment and quantitativeproteinuria if the dipstick test is positive. Echocardiography andfundoscopy can be considered. The routine measurement of additionalbiomarkers and/or the use of vascular imaging methods is notrecommended.
3a.9.7 Risk stratification in hypertension
The decision to start pharmacological treatment depends not only on the BPlevel but also on total CV risk, outlined in section 2. However, evensubclinical hypertensive organ damage predicts CV death independently ofSCORE, and the combination may improve risk prediction, especially insubjects at moderate risk (SCORE 1–4%).445,446 Echocardiography is more sensitive than ECG indiagnosing LVH and in predicting CV risk, and may help in more precisestratification of the overall risk and in directing therapy.447 Analbumin:creatine ratio >30 mg/g in urine is also a marker of subclinicaldamage in hypertensive patients.
3a.9.8 Who to treat, and when to initiate antihypertensive treatment
The decision to start antihypertensive treatment depends on the BP level andtotal CV risk. Lifestyle changes are recommended in all patients withsuboptimal BP, including masked hypertension. Prompt initiation of drugtreatment is recommended in individuals with grade 3 hypertension with anylevel of CV risk.431 Lowering BP with drugs is more frequently requiredwhen the total CV risk is very high and should also be considered when therisk is high (section 2.3.5).431 Initiation of BP-lowering drug treatment may alsobe considered in grade 1 or 2 hypertensive patients at low to moderate riskwhen BP is within this range at several repeated visits or elevated byambulatory BP criteria and remains within this range despite a reasonableperiod of time with lifestyle changes.447 However, the NNT in this patientcategory is very high, and patients should be informed and their preferencemust be considered.
Lifestyle changes only with close BP monitoring should be the recommendationin young individuals with isolated moderate elevation of brachialSBP448 andin individuals with high-normal BP who are at low or moderaterisk.447Also, in white coat hypertensive patients without additional risk factors,therapeutic intervention should be limited to lifestyle changes, accompaniedby close follow-up. Drug treatment may also be considered in white coathypertensive patients with a higher CV risk because of metabolicderangements or in the presence of organ damage.
3a.9.9 How to treat
3a.9.9.1 Lifestyle changes
Lifestyle interventions, weight control and regular PA alone may besufficient for patients with high-normal and grade 1 hypertension, andshould always be advised for patients receiving BP-lowering drugs, asthese may reduce the dosage of BP-lowering drugs needed to achieve BPcontrol. The lifestyle intervention specific to hypertension is saltrestriction. At the individual level, effective salt reduction is by nomeans easy to achieve. As a minimum, advice should be given to avoidadded salt and high-salt food. As the BP-lowering effect of increasedpotassium has been well documented in the DASH diet (rich in fruits,vegetables and low-fat dairy products with a reduced content of dietarycholesterol as well as saturated and total fat), patients withhypertension should generally be advised to eat more fruits andvegetables and to reduce their intake of saturated fat andcholesterol.447
3a.9.9.2 Blood pressure-lowering drugs
The large number of randomized trials of BP-lowering therapy, both thosecomparing active treatment vs. placebo and those comparing differentcompounds, confirm that (i) the main benefits of BP-lowering treatmentare due to lowering of BP per se, and are largely independent of thedrugs employed; and (ii) thiazide and thiazide-like diuretics(chlorthalidone and indapamide), β-blockers, calcium antagonists, ACE-Isand ARBs can adequately lower BP and reduce the risk of CV death andmorbidity.431,432 Thus these drugs are all recommended forinitiation and maintenance of BP control, either as monotherapy or incombination. Some aspects should be considered for each of theBP-lowering drug groups.
The position of β-blockers as first-choice BP-lowering drugs has beenquestioned. A meta-analysis of 147 randomized trials431 reports only aslight inferiority of β-blockers in preventing stroke (17% reductionrather than 29% reduction with other agents), but a similar effect inpreventing CAD and HF, and higher efficacy in patients with a recentcoronary event. However, since β-blockers induce weight gain, haveadverse effects on lipid metabolism and increase (compared with otherdrugs) the incidence of DM, they are not preferred in hypertensivepatients with multiple metabolic risk factors and conditions thatincrease the risk of new-onset DM (such as obesity, impaired fastingglucose). However, this may not apply to vasodilating β-blockers such ascarvedilol and nebivolol, which have less or no dysmetabolic action, aswell as a reduced incidence of new-onset DM compared with conventionalβ-blockers.
Thiazide diuretics also have dyslipidaemic and diabetogenic effects,particularly when used in high doses. Thiazides have often beenadministered together with β-blockers in trials showing a relativeexcess of new-onset DM.
ACE-Is and ARBs are particularly effective in reducing LVH, reducingmicroalbuminuria and proteinuria, preserving renal function and delayingend-stage renal disease.
Evidence concerning the benefits of other classes of agents is much morelimited. The α1 blockers, centrally acting agents(α2 adrenoreceptor agonists and imidazoline-receptoragonists), anti-aldosterone drugs and the renin inhibitor aliskireneffectively lower BP in hypertension, but there are no data documentingtheir ability to improve CV outcome. All of these agents have frequentlybeen used as added drugs in trials documenting CV protection and canthus be used for combination treatment in addition to the recommendedcombinations (see below).
Drugs with 24 h efficacy are preferred. Simplification of treatmentimproves adherence to therapy, and effective 24 h BP control isprognostically important in addition to office BP control. Long-actingdrugs also minimize BP variability, which may offer protection againstprogression of organ damage and the risk of CV events.
Any all-purpose ranking of drugs for general BP lowering is infeasibleand no evidence is available that different choices should be made basedon age or sex (except for caution in using ACE-Is and ARBs in women ofchildbearing age because of possible teratogenic effects).449 Some agentsshould be considered as the preferred choice in specific conditionsbecause they have been used in trials that included patients with thoseconditions or because of greater effectiveness in specific types oforgan damage (Table 17).447
Drugs to be preferred in specific conditions
 |
 |
ACE-I = angiotensin-converting enzyme inhibitor; ARB =angiotensin receptor blocker; BP = blood pressure; CV =cardiovascular; Diuretic = thiazide or thiazide-like; ESRD =end-stage renal disease; ISH = isolated systolichypertension; LVH = left ventricular hypertrophy; MI =myocardial infarction.
Drugs to be preferred in specific conditions
 |
 |
ACE-I = angiotensin-converting enzyme inhibitor; ARB =angiotensin receptor blocker; BP = blood pressure; CV =cardiovascular; Diuretic = thiazide or thiazide-like; ESRD =end-stage renal disease; ISH = isolated systolichypertension; LVH = left ventricular hypertrophy; MI =myocardial infarction.
3a.9.9.3 Combination treatment
Combination treatment is needed to control BP in most patients. Theaddition of a drug from another class should thus be regarded as arecommended treatment strategy unless the initial drug needs to bewithdrawn because of side effects or the absence of any BP-loweringeffects. The extra BP reduction from combining drugs from two differentclasses is approximately five times greater than doubling the dose ofone drug450 andmay reduce the side effects associated with either drug. The combinationof two drugs may also offer advantages for treatment initiation,particularly in patients at (very) high risk in whom early BP controlmay be desirable. Trial evidence of outcome reduction has been obtained,particularly for the combination of a diuretic with an ACE-I, an ARB ora calcium antagonist.451
Despite the trial evidence of outcome reduction, the β-blocker/diureticcombination favours the development of DM and should thus be avoidedunless required for other reasons. The combination of ACE-I and ARB isnot recommended.452 Specific benefits of such a combination innephropathic patients with proteinuria (because of a superioranti-proteinuric effect) await confirmation in event-based trials, andif used, should be monitored closely.
In 15–20% of hypertensive patients, a combination of three drugs isneeded to achieve BP control, thus a combination of three BP-loweringdrugs at fixed doses in a single tablet may be favoured, becausereducing the number of daily pills improves adherence, which is low inpatients with hypertension. The most rational combinations appear to bea blocker of the renin–angiotensin system, a calcium antagonist and adiuretic at effective doses.
3a.9.10 Blood pressure goals
There are only a few randomized clinical trials comparing different treatmenttargets. Hence any recommendation on target levels largely derives fromobservational studies and post hoc analyses of RCTs, which have mostlycompared different treatment regimens and reported achieved BP levels.
There is sufficient evidence to recommend that SBP be lowered to <140 mmHgand DBP to <90 mmHg in all non-elderly hypertensive patients. Evidence ismissing in the elderly hypertensive patient, in whom the benefit of loweringSBP to <140 mmHg has not been tested in randomized trials.
A DBP target <90 mmHg is always recommended, except in patients with DM,in whom values <85 mmHg are recommended. Nevertheless, it should beconsidered that DBP values between 80 and 85 mmHg are generally safe andwell tolerated.396,397
Post hoc analyses of large-scale trials (e.g. ONTARGET, INVEST and VALUE),although suffering from the limitation posed by comparisons ofnon-randomized groups, suggest that, at least in high-risk hypertensivepatients, there may be no advantage in lowering SBP to <130 mmHg, exceptperhaps for risk of stroke. A J-curve phenomenon for achieved SBP <130mmHg cannot be excluded,447 mainly in patients with advanced atheroscleroticdiseases and/or frailty.
The publication of the primary results of the Systolic Blood PressureIntervention Trial (SPRINT), which compared the benefit of treatment of SBPto a target of <120 mmHg with treatment to a target of <140 mmHg,challenged the above goal recommendations in high-risk patients withoutDM.435Frail elderly were underrepresented in this trial. Targeting an SBP <120mmHg compared with <140 mmHg (average values 121 mmHg and 136 mmHg,respectively, at the first year) resulted in lower rates of a combinedoutcome of fatal and non-fatal major CV events and death from any cause.However, significantly higher rates of serious adverse events, hypotension,syncope, electrolyte abnormalities and acute kidney injury or failure, butnot injurious falls, were observed in the intensive-treatment group. Thefact that the study was open label in a strategy close to usual care withfrequent visits may have helped to adjust the antihypertensive treatment ifserious side effects occurred and thus minimized the risk of events.Generalizability of the findings of SPRINT to patients with DM and to frailelderly is problematic.
Based on current data, it may still be prudent to recommend lowering SBP/DBPto values within the range 130–139/80–85 mmHg, and possibly close to thelower values in this range, in all hypertensive patients.
3a.9.11 Hypertension in special groups
3a.9.11.1 Diabetes mellitus
See section 3a.8.4.
3a.9.11.2 Elderly
Large meta-analyses confirm that treatment is highly beneficial in theelderly hypertensive patient. The proportional benefit in patients>60 years of age is no less than that for younger patients.
In patients >60 years of age with SBP ≥160 mmHg, there is solidevidence to recommend reducing SBP to 140–150 mmHg. However, in fitpatients <80 years of age, BP-lowering treatment may be considered atSBP values ≥140 mmHg, with a target SBP <140 mmHg if treatment iswell tolerated.
Evidence is now available from an outcome trial that BP-loweringtreatment also has benefits in patients ≥80 years of age. Becausepatients in the Hypertension in the Very Elderly Trial (HYVET) weregenerally in good condition, the extent to which HYVET data can beextrapolated to more frail octogenarians is uncertain. In individuals>80 years of age with an initial SBP ≥160 mmHg, it is recommended toreduce SBP to 140–150 mmHg, provided the individual is in good physicaland mental condition.436 The decision to treat should be made on anindividual basis, and patients should always be carefully monitoredduring treatment, with BP also measured in the standing position. Infrail elderly patients, it is recommended to be careful and reach adecision based on monitoring of the clinical effects of treatment.
3a.9.12 Resistant hypertension
The definition of hypertension resistant to treatment is when a therapeuticstrategy that includes appropriate lifestyle measures plus a diuretic andtwo other BP-lowering drugs belonging to different classes at adequate doses(but not necessarily including a mineralocorticoid receptor antagonist)fails to lower SBP and DBP values to <140 mmHg and <90 mmHg,respectively. Depending on the population examined and the level of medicalscreening, the prevalence of resistant hypertension has been reported torange from 5 to 30% of the overall hypertensive population, with figures<10% probably representing the true prevalence. Resistant hypertension isassociated with a high risk of CV and renal events.453 Before a patientis considered treatment resistant, consideration should be given to a lackof treatment adherence, white coat syndrome or high salt or alcohol intake,as well as drug intake with a potential pressor effect, the use ofrecreational drugs or secondary hypertension. In these patients, physiciansshould check whether the drugs included in the existing multiple drugregimen have any BP-lowering effect and withdraw them if their effect isabsent or minimal. Anti-aldosterone drugs, amiloride or the α1blocker doxazosin should be considered as the fourth or fifth drug, if nocontraindication exists (eGFR <45 mL/min/m2 and/or serumpotassium >4.5 mmol/L for mineralocorticoid receptor antagonists).
In the case of drug treatment ineffectiveness (i.e. resistant hypertension),specialist referral should be considered. Any invasive approach in thesepatients should be considered only for truly resistant hypertensivepatients, with clinic values ≥160 mmHg SBP or ≥110 mmHg DBP and with BPelevation confirmed by ABPM.
3a.9.13 Duration of treatment and follow-up
Generally, BP-lowering therapy should be maintained indefinitely. Cessationof therapy in hypertensive patients is mostly followed by the return of BPto pretreatment levels. In some patients, in whom treatment is accompaniedby effective BP control for an extended period, it may be possible to reducethe number and/or dosage of drugs. This may be particularly the case if BPcontrol is accompanied by healthy lifestyle changes. A reduction ofmedications should be made gradually and the patient should be checkedfrequently because of the risk of reappearance of hypertension.
Patient follow-up should be carried out by the health care team, which shouldinclude physicians, nurses and pharmacists in a concerted activity, althoughwide variations exist in the organization of health care systems acrossEurope. In some countries, the task relies more on physicians, while inothers, specially educated and trained nurses play a more prominent role.Once the target is reached, a visit interval of a few months is reasonable;there is no difference in BP control between 3 and 6 month intervals. Theregression of asymptomatic organ damage occurring during treatment reflectsthe treatment-induced reduction of morbid and fatal CV events;454 however, acost-effectiveness analysis in which signs of organ damage should best beassessed in the follow-up has never been done.447
Gaps in evidence
Drug treatment in white coat hypertension.
If and when drug treatment should be started in the high-normal BPrange.
The optimal office BP values (i.e. the most protective and safe) forpatients to achieve by treatment in different demographic andclinical conditions.
The optimal out-of-office (home and ambulatory) BP targets andwhether the treatment strategies based on control of out-of-officeBP provide an advantage over strategies based on conventional(office) BP control.
3a.10 Antiplatelet therapy
Key messages
Antiplatelet therapy is not recommended in individuals free from CVD, dueto the increased risk of major bleeding.
Recommendations for antiplatelet therapy
 |
 |
ACS = acute coronary syndrome; CAD = coronary artery disease; DES =drug-eluting stent; MI = myocardial infarction; TIA = transientischaemic attack.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for antiplatelet therapy
 |
 |
ACS = acute coronary syndrome; CAD = coronary artery disease; DES =drug-eluting stent; MI = myocardial infarction; TIA = transientischaemic attack.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for management of hypertension
 |
 |
ACE-I = angiotensin-converting enzyme inhibitor; ARBs = angiotensinreceptor blockers; BP = blood pressure; CKD = chronic kidneydisease; CV = cardiovascular; CVD = cardiovascular disease; DBP =diastolic blood pressure; SBP = systolic blood pressure; SCORE =Systematic Coronary Risk Estimation.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dOverweight, obesity, dyslipidaemia, impaired glucosetolerance.
Recommendations for management of hypertension
 |
 |
ACE-I = angiotensin-converting enzyme inhibitor; ARBs = angiotensinreceptor blockers; BP = blood pressure; CKD = chronic kidneydisease; CV = cardiovascular; CVD = cardiovascular disease; DBP =diastolic blood pressure; SBP = systolic blood pressure; SCORE =Systematic Coronary Risk Estimation.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
dOverweight, obesity, dyslipidaemia, impaired glucosetolerance.
3a.10.1 Antiplatelet therapy in individuals without cardiovasculardisease
Prevention in individuals without overt CV or cerebrovascular disease wasinvestigated using long-term aspirin vs. control in a systematic review ofsix trials including 95 000 individuals. A risk reduction from 0.57% to0.51%/year of serious vascular events was found by the AntithromboticTrialists' Collaboration.464 Major gastrointestinal and extracranial bleedsincreased by 0.03%/year. The risk of vascular mortality was not changed bytreatment with aspirin. In a recent Japanese study,470 patients 60–85years of age presenting with hypertension, dyslipidaemia or DM wererandomized to treatment with 100 mg aspirin or placebo. The 5 yearcumulative primary outcome event rate (death from CV causes) was notsignificantly different between the groups, but treatment with aspirinsignificantly increased the risk of extracranial haemorrhage requiringtransfusion or hospitalization (P = 0.004). In individualswith multiple risk factors, clopidogrel in combination with aspirin vs.aspirin alone was tested in the Clopidogrel for High Atherothrombotic Riskand Ischemic Stabilisation, Management, and Avoidance (CHARISMA) trial andwas not of significant benefit.471 The results of the four major ongoing primaryprevention trials—two in DM patients,472,473 one in individuals of advanced age474 and one inindividuals with moderate CV risk475—are expected to become available over the next 5years.
3a.10.2 Antiplatelet therapy in individuals with cardiovascular orcerebrovascular disease
In the acute state of cerebral ischaemia, aspirin reduced the risk of newvascular events within 2–4 weeks by preventing four recurrent strokes andfive vascular deaths per 1000 patients treated.476
Following an episode of ACS, dual antiplatelet therapy given for a period of12 months is a standard treatment based on results from the CURE,455 TRITON456 andPLATO457studies, whereas no clinical studies support the use of prasugrel andticagrelor in patients with stable CAD.
In long-term prevention after MI, stroke or PAD, aspirin is the most studieddrug. In a meta-analysis of 16 trials comprising 17 000 individuals, theAntithrombotic Trialists' Collaboration,464 aspirin treatment was associatedwith serious vascular events in 6.7% of patients/year vs. 8.2% of controls.The risk of total stroke was 2.08%/year vs. 2.59% (P =0.002) and coronary events was 4.3%/year vs. 5.3% (P =0.0001). Aspirin was associated with a 10% reduction in total mortality,with a significant excess of major bleeds; nevertheless, the benefits ofaspirin exceeded the bleeding hazards.
In patients with prior MI, stroke or PAD, clopidogrel showed a slightsuperiority with respect to aspirin; the rate of serious vascular events was5.32%/year with clopidogrel vs. 5.83% with aspirin (P =0.043). There were slightly more bleeds with aspirin.477
Adding aspirin to clopidogrel in high-risk patients with recent ischaemicstroke or transient ischaemic attack (TIA) was associated with anon-significant difference in reducing major vascular events. However, therisk of life-threatening or major bleeding was significantly increased bythe addition of aspirin.478
On the other hand, the Clopidogrel in High-risk patients with AcuteNon-disabling Cerebrovascular Events (CHANCE) trial showed that the combinedtreatment of clopidogrel and aspirin decreased the 90 day risk of strokewithout increasing haemorrhage compared with aspirin alone in 5170 Chinesepatients randomized within 24 h after symptom onset of minor stroke or TIAto clopidogrel–aspirin or to aspirin alone.479
In patients with prior non-cardioembolic ischaemic stroke, dual antiplatelettherapy with dipyridamole plus aspirin showed superiority overaspirin.465In such patients, oral vitamin K antagonists are not superior to aspirin andare associated with a higher bleeding risk.468,469
In patients with ischaemic stroke, a direct comparison of dipyridamole plusaspirin vs. clopidogrel alone466 showed similar rates of recurrent stroke,including haemorrhagic stroke. There was a higher frequency of majorhaemorrhagic events with dipyridamole plus aspirin (4.1% vs. 3.6%).
Vorapaxar is a novel antiplatelet agent that selectively inhibits thecellular actions of thrombin through antagonism of PAR-1. In 26 449 patientswho had a history of MI, ischaemic stroke or PAD, the primary compositeendpoint—CV death, MI or stroke—was significantly reduced with vorapaxar inaddition to standard antiplatelet therapy, but with increased risk ofmoderate or severe bleeding.480 Vorapaxar cannot be recommended systematically inpatients with stable atherosclerotic disease.
Gap in evidence
Experience with the new antiplatelet drugs in patients with stableCAD is still limited and so is their use in combination withanticoagulant treatment.
3a.11 Adherence to medication
Key messages
Adherence to medication in individuals at high risk and in patients withCVD is low.
Several types of interventions are effective in improving medicationadherence.
The polypill may increase adherence to treatment and improve CV riskfactor control.
Recommendations for achieving medication adherence
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for achieving medication adherence
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Adherence to medication in individuals at high risk and in patients with CVD islow, resulting in worse outcomes and higher health care costs.487 One month after AMI,25–30% of patients stop at least one drug, with a progressive decline inadherence over time. After 1 year, only 50% of patients report persistent use ofstatins, β-blockers or BP-lowering therapy.483,484 The reasons for poor adherence are multifactorial(Table F in web addenda).483
Cost-related non-adherence is a relevant problem in many health care systems. Forexample, in American veterans, adherence to lipid-lowering medication decreasedas co-payments increased.488 Depression also independently doubles the risk fornon-adherence.489 Reasons for non-adherence tend to cluster; for example,complex medication regimens may be important in individuals with chronic diseaseor multiple risk factors. This places high demands on caregivers to provideclear advice and continuous care.484 Physicians often fail to communicate critical elementsof medication use (e.g. possible adverse effects, how long to take themedication and the frequency or timing of dosing).490 Thus there is a need to trainphysicians to identify risk factors for non-adherence and promote adherence tomedication.
Several interventions are effective in improving adherence in chronicconditions.481Solely reducing dosage demands resulted in strong effects, but otherinterventions such as repetitive monitoring and feedback, multisessioninformation and combined behavioural interventions have shown effects rangingfrom minor to strong.481 Collaboration with pharmacists or pharmacist-directed carewas superior to standard care with respect to BP, total cholesterol and LDL-Clevels.491Knowledge of one's CAC score may increase risk perception and adherence tomedication.492
In clinical practice, physicians should assess adherence to medication, identifyreasons for possible non-adherence and promote adherence according to thefollowing established principles:
Provide clear advice regarding the benefits and possible adverse effectsof the medication and the duration and timing of dosing.
Consider patients' habits and preferences (shared decision-making).
Simplify the treatment regimen to the lowest feasible level.
Ask patients in a non-judgmental way how the medication works for themand discuss possible reasons for non-adherence (e.g. side effects,worries).
Implement repetitive monitoring and feedback.
Introduce physician assistants and/or trained nurses or pharmacistswhenever it is necessary and feasible.
In case of persistent non-adherence, offer multisession or combinedbehavioural interventions [e.g. for patients after myocardialrevascularization in a cardiac rehabilitation (CR) setting].
3a.11.1 Polypill
More than a decade ago, Wald and Law quantified the efficacy and adverseeffects of a fixed dose combination (FDC) from published trials and proposedthat an FDC consisting of a statin, BP-lowering agents, aspirin and folatecould potentially reduce CVD by 80% in individuals >55 years ofage.493
A recent systematic review and meta-analysis485 summarizes nine randomized trials(n = 7047) on FDCs, largely conducted in higher-riskpopulations and primarily designed to evaluate changes in CV risk factorsand adherence. However, FDCs included in the analysis were single pills ofdiverse composition and doses (although all contained a statin and at leastone BP-lowering agent) and had a range of comparators (placebo, single-drugactive component or ‘usual care’). No convincing evidence of either benefitor risk for FDCs in terms of all-cause mortality or CV events was found. FDCtherapy improved adherence (only one trial) compared with a multidrugstrategy by 33% (95% CI 26%, 41%) compared with usual care.
In another international study, not included in the previous meta-analysis,695 CAD patients were randomized to test the effect of an FDC polypillcontaining aspirin, simvastatin and ramipril, or the three drugs separately.The study showed that FDC improved adherence compared with separatemedications after 9 months of follow-up (adherence 63% vs. 52%;P = 0.006).486
The polypill should not be considered in isolation, but as an integral partof a comprehensive CVD prevention strategy that includes efforts to reducetobacco use, increase PA and increase consumption of a heart-healthydiet.494However, potential adverse effects of a single drug component of the FDCcannot be specifically corrected and therefore may also affect treatmentadherence to the other components. Until we have the results of ongoingtrials with major CVD as the endpoint, the polypill cannot be recommendedfor prevention of CVD and cannot be prescribed to all individuals.
Gaps in evidence
There is limited evidence about which interventions for improvingadherence to medication are the most effective and in whom (e.g.young–old, male–female, high vs. low socio-economic status).
The effect of the polypill as a global strategy to reduce CVD remainsuncertain.
3b. How to intervene at the individual level: disease-specific intervention—atrialfibrillation, coronary artery disease, chronic heart failure, cerebrovasculardisease, peripheral artery disease (web addenda)
3c. How to intervene at the population level
3c.1 Introduction (healthy lifestyle promotion)
The population level approach follows the Geoffrey Rose paradigm: small shifts inthe risk of disease (or risk factor) across a whole population consistently leadto greater reductions in disease burden than a large shift in high-riskindividuals only. This population-wide approach has further advantages: itaddresses CV health over the entire life course and reduces healthinequalities.
Individual behaviour is enacted in an environment with hierarchical levels, whichencompass individual choice, family influence, cultural and ethnic grouping,workplace, health care and policy at the state and global levels (e.g. EUpolicies and international trade agreements).The aim of this section is toprovide stakeholders with evidence-based suggestions for the most effectiveinterventions to improve CVD risk that can be implemented at a group, community,regional, national or global level. Health care professionals play an importantrole in advocating evidence-based population-level interventions.
Strategies such as ‘nudging’ (to push mildly) and ‘default’ have been proposed astools. By changing the context to make healthy decisions the default, theindividual is nudged in the healthy direction. The task for both national andlocal authorities is to create social environments that provide healthierdefaults.
The evidence presented here builds on recent comprehensive reviews311,495–497 and individual studiesand summarizes the ‘totality of evidence’. It is rarely feasible to use an RCTto evaluate population-level interventions (in contrast to individual-levelinterventions). The guidelines committee has chosen to follow the definition of‘level of evidence’ for population-level approaches. Thus consistent findingsfrom several high-quality studies were considered sufficient to merit strongrecommendations.
3c.2 Population-based approaches to diet
Key messages
Structural measures such as product reformulation, limitations onmarketing and taxes on unhealthy foods, subsidizing the costs ofhealthier foods and consumer-friendly nutrition labelling will improvehealthy food choices.
Healthy environments in the community, at schools and in workplaces willstimulate a healthy lifestyle.
Recommendations for population-based approaches to diet
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for population-based approaches to diet
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Diet is a powerful determinant of obesity, hypertension, dyslipidaemia, DM and CVhealth. Rapid reductions in CV events can be seen after changes in diet at thepopulation level.497,510 Stakeholders,including health care professionals, have a shared responsibility forpopulation-based approaches and can help to promote healthy diets andenvironments495,498 (FigureL in web addenda504).
Many EU countries recognize the health benefits of reducing the energy densityand salt and sugar content as well as replacement of trans and saturated fat byunsaturated fat in foods and drinks.311,495,498 These have led tosuccessful reductions in trans fats499 and salt,495,499–501 the latter likely leading to decreases inBP.501Mandatory upper limits harmonized across the EU will ensure that all EUconsumers are equally protected.498
Governments can facilitate nationwide cooperation between (local) governments,non-governmental organizations (NGOs), the food industry, retail, catering,schools, workplaces and other stakeholders. The French Ensemble Prévenonsl'Obésité des Enfants (EPODE) project is an example of a multistakeholdercooperation that can help decrease childhood obesity.502 Similar projects are in place inBelgium, Spain, The Netherlands, Greece and Australia.
Educational tools and intervention in the media may lead to a reduction inchildhood obesity (e.g. limiting children's exposure to advertising of unhealthyfoods).311,495,497,502,503 In2013, the European Heart Network (EHN) published a report summarizing recentdevelopments in relation to the marketing of unhealthy foods tochildren.504Accompanying consumer awareness campaigns on healthy foods505 and nutritionlabelling can be effective. Consumers understand different systems of labellingand their use has a positive impact on sales.506 The EHN is calling for a simplified,colour-coded, front-of-pack scheme indicating high, medium and low levels ofnutrients.311,495,497 This scheme can be applied to allfoods and could be expanded to certain restaurants.311 Labelling also stimulates thereformulation of foods,504 and thus it has the potential to improve dietary intakeand reduce diet-related chronic diseases.
Pricing strategies can lead to a decline in the sales of unhealthy foods and anincrease in the sales of fruits and vegetables. Modelling studies havedemonstrated that food taxes could improve energy and nutrient intake, BMI andhealth.495,507,508 An increasing number of countries haveintroduced taxes on unhealthy foods and drinks [e.g. the fat tax in Denmark(caused a 10–15% decrease in consumption; now repealed) and the junk food tax inHungary (sales declined by 27%)].504
Consideration should be given to balanced economic incentives: subsidies andtaxes to counteract any unbalanced effect on the socially disadvantaged.
To tackle obesity, every school and workplace should have a policy to promote ahealthy environment and provide healthy foods and meals.495,504 Ideally, health education should bepart of the school curriculum. Workplace dietary modification interventionsalone and in combination with nutrition education or environmental changes haveshown improvements in the consumption of fruits and vegetables and/orfats.509
In the community, planning the location and density of fast food outlets and goodaccess to supermarkets is needed, especially in deprived areas.495–497
Gaps in evidence
Scientific evidence of the impact of food and nutrition policyinstruments on outcome measures such as food intake and CV health islargely lacking.
Cost-effectiveness studies of the impact of different policy options arealso limited.
3c.3 Population-based approaches to physical activity
Key messages
A sedentary lifestyle and physical inactivity affects more than half ofthe population worldwide.
Regular PA is recommended for all men and women as a lifelong part oflifestyle, with at least 150 min/week of moderate activity or at least75 min/week of vigorous activity or an equivalent combination thereof.Any activity is better than none and more activity is better thansome.
Population-based interventions are effective in promoting PA.
Early childhood education in PA and movement should start atpreschool/kindergarten.
Daily PA at school should be at least 30 minutes, and preferably 60minutes.
Good neighbourhoods and a safe environment enhances and encourages PA ineveryday life.
Recommendations for population-based approaches to physical activity(continued)
 |
 |
GPs = general practitioners; PA = physical activity.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for population-based approaches to physical activity(continued)
 |
 |
GPs = general practitioners; PA = physical activity.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
In most countries, the majority of adults and children do not achieve the minimumactivity levels recommended by health organizations: every person should engagein moderate exercise for at least 150 min/week and/or vigorous activity for atleast 75 min/week or an equivalent thereof.258,520 For population-based prevention, the statement of‘seven best investments’512 gives the universal and comprehensive advice to promotePA.512
Specific national guidelines developed for PA include frequency, intensity, time(duration) and type of activity (FITT), which can influence legislativeinitiatives, such as ‘active cities’ with bicycle lanes and walking paths andreallocation of road space.
Focused media and educational campaigns can initiate physicalactivities.519Recent campaigns from sports medicine societies have endorsed PA prescriptionsfrom GPs (http://www.efsma.net). The PA shouldbe assessed at every medical encounter.
A simple strategy for increasing daily exercise is to encourage the use of stairsrather than the elevator or escalator, along with signage directing people tothe stairs and health promotion materials endorsing the positive effects ofstair climbing.516
Interestingly, an increase in fuel prices may reduce car driving and increaseactive commuting for those who live within reasonable walking or bikingdistances, with the exception of diseased or disabled persons.496
PA education should be started in preschool/kindergarten and continue for alllevels of primary and secondary education. For school education, amulticomponent intervention should focus on improving lifelong PA by trainedteachers. At least 3 h/week, and preferably 60 min/day, of sports or PA shouldbe performed during school time.511 Regular activity also improves cognitive competencefor learning.513,521 This activity can besupplemented with active commuting to school and supervised walking routes toand from school, with less reliance on buses.514
Workplaces can offer different opportunities for PA promotion. Some largercompanies offer a fitness centre on company grounds without fees for employees.Workplace-based interventions may increase regular physical exercise foremployees, but results demonstrate that a high proportion of workers do notparticipate.522Therefore, supervisors and managers should endorse workplace interventions byencouraging employees to undertake PA.
Improved accessibility to recreation and exercise facilities with increasedoperating hours and utilizing community resources such as school playgrounds mayincrease regular PA in all age groups and reduce socio-economic inequality ofaccess.517
Gap in evidence
Sustainability and long-term outcomes of population-based actions topromote PA.
3c.4 Population-based approaches to smoking and other tobacco use
Key messages
Adolescence is the most vulnerable period for uptake of smoking, withlifelong consequences.
High taxes on all tobacco products is the most effective policy measureto reduce smoking uptake by the young.
Restrictions on smokeless tobacco due to strong evidence of harm.
Restrictions on e-cigarettes due to uncertainty regarding safety andeffect.
Plain packaging is effective in reducing tobacco consumption.
Restrictions on advertising, promotion and sponsorship by the tobaccoindustry.
A goal would be to make a common European decision to achieve asmoking-free Europe by 2030.
Recommendations for population-based approaches to smoking and othertobacco use
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for population-based approaches to smoking and othertobacco use
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
The WHO Framework Convention on Tobacco Control recommends smoke-free laws:protecting people from tobacco smoke and banning smoke in public places, warningabout the dangers of tobacco, raising taxes on tobacco and enforcing advertisingbans.523Children and low socio-economic groups are sensitive to population-based tobaccointervention. Passive smoking increases CVD risk,495,496 more so in women than in men.529 All smoking, includingsmoking a water pipe, is deleterious. Smokeless tobacco (in Europe usually snus,a moist powder tobacco placed under the upper lip) increases the risk of fatalCVD events,525–527 and the use of snus during pregnancy increases therisk of stillbirth.530There is no evidence that snus increases smoking cessation more than nicotinereplacement products or medication. Many smokers use e-cigarettes to quit. Thereare many unanswered questions about their safety, efficacy for harm reductionand cessation and impact on public health. International legislation should beharmonized to prevent a new tobacco epidemic.495
Multicomponent strategies are best. Advertising bans reduce tobacco consumption,and mass media campaigns reduce smoking uptake by teenagers and increase adultquitting.495Media and educational campaigns in schools reduce smoking and promote smokingcessation. Editors should increase the coverage of tobacco and health in themedia.531Telephone or Internet-based cessation support reduces tobacco use.496
Packs with pictorial and text warnings raise awareness of tobaccodangers.495Plain and standardized packaging without brand labels enhances theeffectiveness.
Higher taxes reduce tobacco consumption and encourage quitting, particularlyamong young and lower socio-economic groups.495,496
School-based smoking bans should be implemented.496 Smoking bans at workplaces reduceexposure to passive smoking, decrease smoking and increase quittingrates.495Tobacco outlet density near homes, hospitals and schools should be reduced.Pregnant women should avoid tobacco, and parents should be tobacco free whenchildren are present. Health personnel, caregivers and teachers must set anexample by not using tobacco products at work.
Gaps in evidence
Effect of school-based smoking restrictions.
Health harm of e-cigarettes.
More evidence on environmental smoking is needed, as smoke particles mayremain in rooms for many years.
3c.5 Alcohol abuse protection
Key messages
Excessive alcohol intake is associated with increased CV mortality, andalcohol ranks as the second-leading cause of DALYs lost in high-incomecountries.
The interventions for addressing the harmful use of alcohol are costeffective, with good return (i.e. increasing alcoholic beverage excisetaxes, restricting access to alcoholic beverages and implementingcomprehensive restrictions and bans on advertising and promotion ofalcoholic beverages).
Recommendations for protecting against alcohol abuse
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for protecting against alcohol abuse
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
At the population level, alcohol consumption is associated with multiple healthrisks that clearly outweigh any potential benefits. In 2012, ∼3.3 million deaths(5.9% of all global deaths) and 139 million DALYs (5.1% of the global burden ofdisease and injury) were attributable to alcohol consumption. The highestnumbers of deaths are from CVDs, with 33.3% of the alcohol-attributable deathsdue to CVDs.534Ischaemic heart disease mortality is 65% higher in male heavy drinkers and morethan double in female heavy drinkers.540
The relationship between alcohol consumption and CAD and cerebrovascular diseasesis complex. It depends on both the level and pattern of alcohol consumption. Lowalcohol consumption, ranging from one to three alcohol units per day (a unitequates to about 80 mL of wine, 250 mL of normal strength beer or 30–50 mL ofspirits) in some segments of the population is associated with the lowestall-cause mortality, largely due to lower coronary mortality.541
SBP and DBP levels increase as alcohol consumption increases to >3 units/day,as does the risk of cardiac arrhythmias, cardiomyopathy, sudden death andhaemorrhagic stroke.542The pattern of alcohol use has an effect on CVD risk; binge drinking isassociated with a higher risk of sudden death and stroke.543
The following strategies and interventions have the highest level ofeffectiveness to prevent the harmful use of alcohol: age limits for sale andserving;535drink-driving strategies;537 government retail monopolies on the sale of alcohol andreducing the hours of sale;536 banning alcohol advertising, promotion and sponsorshipof events532 and anincrease in retail prices.533,538
In the absence of other population-level measures, such as taxation andadvertising restrictions, labelling alcohol with information on caloric contentand health warning messages of the harmful effects of alcohol has been shown tohave a limited effect.538
Alcohol regulations in the policies of workplaces, educational centres andschools are effective.532
Brief intervention in primary care to prevent alcohol abuse has been shown to beeffective.539
In the community, excessive alcohol intake can be limited by restrictions in thenumber and opening hours of outlets and by increasing the minimum age for salesand servings.495
Gap in evidence
Better quality evidence is needed with regard to potential confounding instudies on the effects of alcohol consumption.
3c.6 Healthy environment
Air pollution contributes to the risk of respiratory and CV diseases.544 Important sources offine particles in the EU are motorized road traffic, power plants and industrialand residential heating using oil, coal or wood. Up to a third of Europeansliving in urban areas are exposed to levels exceeding EU air quality standards.In particular, young and old individuals and subjects with a high risk of CVDare more prone to the detrimental effects of air pollution on the circulationand the heart.
The EU Commission released a policy package to be implemented by the year 2030with measures to reduce harmful emissions from traffic, energy plants andagriculture. Further efforts to reduce air pollution should be encouraged andtaken up by national governments (e.g. through appropriate and effectivelegislation). Patient organizations and health professionals have an importantrole to play in supporting education and policy initiatives and provide a strongvoice in the call for action at the governmental level.544
The media can inform the population on air quality (e.g. by apps) and byproviding smog alerts. Information on patients' behaviour during smog is needed.Economic incentives such as reduced taxes on electric and hybrid cars cancontribute to the improvement of air quality. New houses and schools can bebuilt in areas remote from highways and polluting industries.
4a. Where to intervene at the individual level
The question of ‘where’ prevention should take place requires only a simple answer:everywhere! Prevention of CVD should be valued and implemented at all levels ofsociety and in all health care settings. This should include increased spending onprevention in health care and on actions that make communities healthier. Allclinicians should consider prevention and promotion of healthy lifestyles aprofessional responsibility with individual patients and should support policiesthat promote healthier lifestyles. Patients should also be empowered and have theknowledge and support to make informed decisions and to demand robust preventionefforts from health care groups and society.
4a.1 Clinical settings and stakeholders
4a.1.1 Cardiovascular disease prevention in primary care
Key messages
The prevention of CVD should be delivered in all health caresettings, including primary care.
Where appropriate, all health professionals should assess CV riskfactors to determine the individual's total CV risk score.
GPs and nurses should work together as a team to provide the mosteffective multidisciplinary care.
Recommendation for cardiovascular disease prevention in primarycare
 |
 |
aClass of recommendation.
bLevel of evidence.
Recommendation for cardiovascular disease prevention in primarycare
 |
 |
aClass of recommendation.
bLevel of evidence.
The physician in general practice is the key person to initiate, coordinateand provide long-term follow-up for CVD prevention. In most countries, GPsdeliver >90% of consultations and provide most public health medicine,including preventive care and chronic disease monitoring. In the case of CVDprevention, they have a unique role in identifying individuals at risk ofCVD and assessing their eligibility for intervention based on their riskprofile. How to maximize attendance rates and adherence, particularly inthose who are at highest risk, remains an issue.
As mentioned in section 2.2, a systematic approach is recommended to riskassessment, giving priority to persons with a priori higher risk (such asfamily history of premature CVD, presence of hypertension, etc.);opportunistic screening of persons <40 years of age without CV riskfactors is not recommended.
Intensive and structured intervention in general practice contributes to theprevention of recurrent CV events and reduces hospital admissions in CADpatients.545
The successful implementation of CVD prevention guidelines relies heavily onGPs providing risk factor evaluation, intervention and patient education.However, CV targets in general practice are often not achieved. TheEUROASPIRE III survey (primary prevention arm) showed that the lifestyle ofpeople being treated as high CV risk—defined as patients treated with BP-and lipid-lowering drugs as well as anti-diabetes drugs—showed muchpersistent smoking and a high prevalence of both obesity and centralobesity. BP, lipid and glucose control is poor, with most patients notachieving the targets defined in the prevention guidelines.5
Surveys done among GPs and physicians in several European regions found thatmost were aware of the European guidelines on CVD prevention, but that only36–57% were using the guidelines in practice, and less than half performedcomprehensive risk assessments. The main barrier was time, but GPs alsocited that there were too many guidelines, unrealistic targets for riskfactor control, a preference for using their own experience and a lack ofknowledge regarding comprehensive risk assessment.546–549 Online resources,mobile apps, pocket guidelines and summary cards may contribute as a meansto overcome the implementation challenge.
Evidence for an effective role for nurses in primary care exists. A study ofnurse-coordinated preventive cardiology programmes for primary prevention ofCVD compared with routine practice conducted in a matched, paired-clusterRCT in six pairs of general practices in six European countries showed morehigh-risk patients achieved the lifestyle and risk factor targets in thenurse-coordinated arm compared with usual care.550
In 2009, a randomized trial in The Netherlands on CVD risk management andpreventive care found that practice nurses achieved results equal to GPsafter 1 year of follow-up.551 A clinical trial (n = 525) in theUSA also showed that advanced practice nurses working with community healthworkers can achieve significant improvements in CV risk factors (BP,cholesterol, DM control) in underserved inner-city populations compared withenhanced usual care, and it was cost-effective.552
Gap in evidence
Further research is needed in order to explore what is the beststrategy to improve implementation of CVD prevention guidelines ingeneral practice, taking into account the heterogeneity amongcountries in terms of health systems and local resources.
4a.1.2 Acute hospital admission setting
Recommendation for CVD prevention strategies in the acute hospitaladmission setting
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendation for CVD prevention strategies in the acute hospitaladmission setting
 |
 |
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
The importance of starting appropriate prevention before hospital dischargecannot be overemphasized, as prevention treatment tends to decrease ratherthan increase post-hospitalization, with proportions of patients onappropriate therapy declining over time and patients not reaching riskfactor targets.295,554
The acute care team should emphasize the importance of the preventivemeasures directly to the patient, because failure to do so may suggest thatthese measure are valueless; and they interact with other healthprofessionals (e.g. physicians, nurses) to ensure that prevention strategiesinitiated during hospitalization are sustained and supported in othersettings.
Thus patients, while in acute care, should receive appropriate interventionsto optimize prevention strategies. These include full clinical assessment toguide optimization of medical therapy, individualized behavioural educationfor risk factor modification and referral to exercise-based CR.
Education should be person-centred with full participation of patients andcaregivers, providing explanations for each intervention, while earlymobilization and physical conditioning programmes should vary according tothe individual's clinical status.
4a.1.3 Specialized prevention programmes
Recommendations for specialized prevention programmes
 |
 |
CR = cardiac rehabilitation; CVD = cardiovascular disease; HF =heart failure.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Recommendations for specialized prevention programmes
 |
 |
CR = cardiac rehabilitation; CVD = cardiovascular disease; HF =heart failure.
aClass of recommendation.
bLevel of evidence.
cReference(s) supporting recommendations.
Specialized prevention programmes are delivered as CR or other preventionprogrammes for all patients with CVD or at high risk for CVD. The corecomponents and goals of CR have been standardized,562 but the structure, length and typeof programme offered differs widely by country, affected by nationalguidelines and standards, legislation and payment factors.563
CR is a comprehensive programme involving exercise training, risk factormodification, education and psychological support. An overview of sixCochrane systematic reviews of CR (148 RCTs with 98 093 subjects) concludedthat for low- to moderate-risk patients with HF, or who are post-MI orrevascularization, exercise-based CR decreased hospital admissions andimproved health-related quality of life (HRQoL) compared with usual care,and may reduce mortality longer term.555 A limitation of current reviews isthe inclusion of trials prior to modern treatment, differing patients groupsand heterogeneous programmes of CR. Thus more research is needed todetermine the optimal intervention. A number of recent controlled cohortstudies have found a survival benefit for patients receiving CR comparedwith no CR. An ongoing meta-analysis of CR in the modern era may providemore definitive results regarding patient programmes and outcomes. Atpresent, the benefit of CR appears to be through direct physiologicaleffects of exercise training and through CR's effects on risk factors,behaviour and mood.555 CR also provides an opportunity for social support andto screen patients for psychosocial risk factors.
Referral and participation in CR varies widely across countries: many CRprogrammes do not include unstable patients or patients with HF, devices orPAD, and referral and retention of women and older, higher-risk patientsremains suboptimal.563,564Referrals to CR can be increased through electronic prompts or automaticreferrals, while patient uptake may be improved with structured follow-up bynurses or therapists and early starts to programmes afterdischarge.557,558,565
Nurse-led programmes can also deliver effective preventive programmes inpatients with CVD. The EUROACTION trial used a 16 week family-centredapproach that led to healthier lifestyle changes in activity and diet andmore effective control of risk factors in patients and their partnerscompared with usual care.550 The Randomised Evaluation of Secondary Preventionby Outpatient Nurse Specialists (RESPONSE) trial randomized patients afterACS to usual care or to nurse-coordinated prevention intervention ofoutpatient visits over 6 months: at 1 year, patients in the interventiongroup had better control of risk factors, fewer readmissions and emergencydepartment visits and a predicted RR of mortality (using SCORE) 17% lowerthan the control group.561
4a.1.4 Alternative rehabilitation models
Key message CR has predominantly been implemented in hospitalsor in community centres with trained staff. Home-based rehabilitationprogrammes have the potential to increase patient participation by offeringgreater flexibility and options for activities. A systematic review of 12trials (with 1978 patients) of home- vs. centre-based rehabilitation foundno difference in outcomes, adherence or cost between the two in the shortterm and up to 24 months.566 The majority of studies recruited low-risk,predominantly male patients, and activities were self-regulated withintermittent support, usually by telephone. Home-based rehabilitation thusoffers an alternative for some patients, although relatively few programmesin Europe offer it.563
Home-based rehabilitation with and without telemonitoring holdspromise for increasing participation and supporting behaviouralchange.
4a.1.4.1 Telerehabilitation
Telerehabilitation, i.e. the use of electronic communication andinformation technologies to provide and support remote clinical careafter an acute event, has been found to be more effective than usualcare in achieving behavioural change, and equally effective as a CRprogramme.557,567 Simple telemonitoring, including ECG transmissionby telephone in patients with CVD, has been found to be safe andacceptable to patients and results in improvements in physicalcapacity.568 Recent studies are also using smartphoneapplications for monitoring and delivery of content and support, withimprovements in uptake, adherence and completion of rehabilitation inyounger patients.569
Thus telerehabilitation could further widen participation to morepatients and provide monitoring and greater individualized behaviouralsupport, but large-scale randomized trials are needed.
4a.1.5 Maintaining lifestyle changes
Maintaining healthy behaviours after a specialized prevention programme isproblematic for many patients.
Specialized prevention programmes and patient consultations should use apatient-centred approach that focuses on the patient's priorities and goalsand incorporates lifestyle changes within the context of the patient's life.Behavioural change of personal value to the individual is more likely to bemaintained (see section 3a.1).
Longer-term support for behaviour change may be needed and communitymaintenance programmes may be useful. In the Global Secondary PreventionStrategies to Limit Event Recurrence After MI (GOSPEL) trial, 3241 patientswere randomized post-CR programme to an intensive multifactorialintervention over 3 years or usual care. Patients in the intervention groupreceived monthly exercise and counselling sessions for 6 months, then every6 months for 3 years. Compared with usual care, the intervention group hadimproved PA, diet and total cholesterol maintained throughout the study. Theintervention significantly decreased several combined endpoints, such as CVmortality plus non-fatal MI and stroke by 33%, cardiac death plus non-fatalMI by 36% and non-fatal MI by 48% compared with usual care.570
Gaps in evidence
The optimal CR programme in the era of modern cardiology and theincremental benefits of various components of CR programmes,especially for underserved patient groups.
Alternative and cost-effective models of CR are needed to ensureparticipation globally, including low- and middle-incomecountries.
4a.2 How to monitor preventive activities
Key message
Standards of performance in CVD prevention may serve as vehicles toaccelerate appropriate translation of scientific evidence into clinicalpractice.
Recommendation for monitoring preventive strategies
 |
 |
aClass of recommendation.
bLevel of evidence.
Recommendation for monitoring preventive strategies
 |
 |
aClass of recommendation.
bLevel of evidence.
Candidates for measures of performance are some of those processes of care thatare recommended by the guideline either as class I, which identifies recommendedprocedures/treatments, or class III, which identifies procedures/treatments thatare not recommended.
The development of standards of performance involves identification of a set ofmeasures that target a specific patient population observed over a particulartime period. Thus these performance measures are aimed at any clinician orhealth care professional who sees adult subjects (≥18 years of age) at risk forCVD. Table 18provides examples of performance measurements of CVD prevention. Detailedspecifications for each performance measure, including the numerator,denominator, period of assessment, method of reporting and sources of data,should be developed at the local level. An optimal target of 100% is recommendedfor all standards. If this is not achievable, an interim local target could beset.
Examples of performance measurements of CVD prevention
 |
 |
BMI = body mass index; BP = blood pressure; CR = cardiacrehabilitation; HbA1c = glycated haemoglobin; PA = physicalactivity.
Examples of performance measurements of CVD prevention
 |
 |
BMI = body mass index; BP = blood pressure; CR = cardiacrehabilitation; HbA1c = glycated haemoglobin; PA = physicalactivity.
4b. Where to intervene at the population level
Key message
Governmental and non-governmental organizations (NGOs) such as heartfoundations and other health-promoting organizations can be a powerful forcein promoting a healthy lifestyle and healthy environments in CVDprevention.
4b.1 Government and public health
Recommendations for population-based interventions to promote CV health aredescribed in section 3c. These preventive strategies to address unhealthy diets,smoking and physical inactivity must take place at different levels. At eachlevel, different clusters of stakeholders are concerned and responsible for theinterventions:495 At the EU level as well as at the level of nationalgovernments, legislation should be developed regarding, for example, thenutritional composition of foods; nutrition labelling; smoke-free policies andenvironments; restrictions on marketing of unhealthy foods, alcohol and tobaccoproducts and promoting environments that encourage PA in everydaylife.311 Also,policy measures to reduce air pollution should be developed. Both levels may useeconomic instruments such as taxes and subsidies to support strategies on foodand nutrition, tobacco and alcohol. It is not necessarily exclusively theresponsibility of governments to ensure the availability of and accessibility toPA opportunities and healthy foods; this should be a joint effort by government,industry and businesses. Health authorities should monitor improvements, and ifvoluntary efforts by industry prove inadequate, governments must intervene.
International level— WHO, World Trade Organization, EU
National level—government departments, health authorities,health-promoting agencies, consumer organizations, health NGOs,industries
Regional and local level—local governmental departments, communities,schools, workplaces, health professionals, catering sector, retailers,NGOs.
4b.2 Non-governmental organizations
NGOs are important stakeholders in advocating the development and maintenance ofpublic health policies and are important partners with health care workers inpromoting CV prevention.
Several Brussels-based NGOs aim at improving the CV health of the public andpatients, including EHN, health and medical professionals [ESC, European ChronicDisease Alliance (ECDA)] and consumer organizations [Bureau Européen des Unionsde Consommateurs (BEUC)].
CV patients' organizations provide their patient members with the opportunity toobtain support from their peers. They produce patient information in the form ofbooklets and web-based materials and promote CR.
Stakeholders such as NGOs and health professionals (e.g. cardiologists,internists and GPs) have a responsibility in agenda setting and monitoringinterventions, and can initiate mass media campaigns to improve health.
In creating healthy and active environments, especially in schools, workplacesand the community, stakeholders such as teachers and parent organizations, thecatering sector, employer organizations, trade unions, sport clubs and fitnesscentres and organizations promoting cycling, walking, public transport orinvolved in urban planning and mobility can play a role. An example is theFrench EPODE project, aimed at reducing overweight in children.502
5. To do and not to do messages from the Guidelines
To do and not to do messages from the Guidelines (continued)
 |
 |
ACE-I = angiotensin-converting enzyme inhibitor; ACS = acute coronarysyndrome; ARBs = angiotensin receptor blockers; BP = blood pressure; CAD= coronary artery disease; CKD = chronic kidney disease; CV =cardiovascular; CVD = cardiovascular disease; DBP = diastolic bloodpressure; DM = diabetes mellitus; GPs = general practitioners; HbA1c =glycated haemoglobin; HDL-C = high-density lipoprotein cholesterol; HF =heart failure; IMT = intima–media thickness; LDL-C = low-densitylipoprotein cholesterol; PA = physical activity; SBP = systolic bloodpressure; SCORE = Systematic Coronary Risk Estimation; TIA = transientischaemic attack.
aClass of recommendation.
bLevel of evidence.
To do and not to do messages from the Guidelines (continued)
 |
 |
ACE-I = angiotensin-converting enzyme inhibitor; ACS = acute coronarysyndrome; ARBs = angiotensin receptor blockers; BP = blood pressure; CAD= coronary artery disease; CKD = chronic kidney disease; CV =cardiovascular; CVD = cardiovascular disease; DBP = diastolic bloodpressure; DM = diabetes mellitus; GPs = general practitioners; HbA1c =glycated haemoglobin; HDL-C = high-density lipoprotein cholesterol; HF =heart failure; IMT = intima–media thickness; LDL-C = low-densitylipoprotein cholesterol; PA = physical activity; SBP = systolic bloodpressure; SCORE = Systematic Coronary Risk Estimation; TIA = transientischaemic attack.
aClass of recommendation.
bLevel of evidence.
6. Appendix
ESC Committee for Practice Guidelines (CPG): Jose Luis Zamorano (Chairperson) (Spain), Victor Aboyans (France), Stephan Achenbach (Germany), Stefan Agewall (Norway), Lina Badimon (Spain), Gonzalo Barón-Esquivias (Spain), Helmut Baumgartner (Germany), Jeroen J. Bax (The Netherlands), Héctor Bueno (Spain), Scipione Carerj (Italy), Veronica Dean (France), Çetin Erol (Turkey), Donna Fitzsimons (UK), Oliver Gaemperli (Switzerland), Paulus Kirchhof (UK/Germany), Philippe Kolh (Belgium), Patrizio Lancellotti (Belgium), Gregory Y.H. Lip (UK), Petros Nihoyannopoulos (UK), Massimo F. Piepoli (Italy), Piotr Ponikowski (Poland), Marco Roffi (Switzerland), Adam Torbicki (Poland), António Vaz Carneiro (Portugal), Stephan Windecker (Switzerland).
ESC National Cardiac Societies actively involved in the review process of the 2016 European Guidelines on cardiovascular disease prevention in clinical practice:
Austria: Austrian Society of Cardiology, Bernhard Metzler; Azerbaijan: Azerbaijan Society of Cardiology, Ruslan Najafov; Belarus: Belorussian Scientific Society of Cardiologists, Valeriy Stelmashok; Belgium: Belgian Society of Cardiology, Catherine De Maeyer; Bosnia and Herzegovina: Association of Cardiologists of Bosnia and Herzegovina, Mirza Dilić; Bulgaria: Bulgarian Society of Cardiology, Ivan Gruev; Croatia: Croatian Cardiac Society, Davor Miličić; Czech Republic: Czech Society of Cardiology, Helena Vaverkova; Denmark: Danish Society of Cardiology, Ida Gustafsson; Egypt: Egyptian Society of Cardiology, Ihab Attia; Estonia: Estonian Society of Cardiology, Davit Duishvili; Former Yugoslav Republic of Macedonia: Macedonian FYR Society of Cardiology, Nela Kostova; France: French Society of Cardiology, Jean Ferrières; Georgia: Georgian Society of Cardiology, Zurab Klimiashvili; Germany: German Cardiac Society,Rainer Hambrecht; Greece: Hellenic Cardiological Society,Konstantinos Tsioufis; Hungary: Hungarian Society of Cardiology,Eszter Szabados; Iceland: Icelandic Society of Cardiology, KarlAndersen; Ireland: Irish Cardiac Society, Carl Vaughan;Israel: Israel Heart Society, Barak Zafrir; Italy:Italian Federation of Cardiology, Salvatore Novo; Kazakhstan:Association of Cardiologists of Kazakhstan, Kairat Davletov;Kosovo: Kosovo Society of Cardiology, Fisnik Jashari;Kyrgyzstan: Kyrgyz Society of Cardiology, Alina Kerimkulova,Latvia: Latvian Society of Cardiology, Iveta Mintale;Lebanon: Lebanese Society of Cardiology, Georges Saade;Lithuania: Lithuanian Society of Cardiology, ZanetaPetrulioniene; Luxembourg: Luxembourg Society of Cardiology,Charles Delagardelle; Malta: Maltese Cardiac Society, Caroline J.Magri; Moldova: Moldavian Society of Cardiology, Victor Rudi;Morocco: Moroccan Society of Cardiology, Latifa Oukerraj;The Netherlands: Netherlands Society of Cardiology, B. ErsenÇölkesen; Norway: Norwegian Society of Cardiology, Henrik Schirmer;Poland: Polish Cardiac Society, Piotr Jankowski;Portugal: Portuguese Society of Cardiology, Roberto Palma dosReis; Romania: Romanian Society of Cardiology, Daniel Gherasim;Russian Federation: Russian Society of Cardiology, SergeyNedogoda; San Marino: San Marino Society of Cardiology, MarcoZavatta; Serbia: Cardiology Society of Serbia, Vojislav Giga;Slovakia: Slovak Society of Cardiology, Slavomira Filipova;Spain: Spanish Society of Cardiology, Luis Rodríguez Padial;Sweden: Swedish Society of Cardiology, Anna Kiessling;Switzerland: Swiss Society of Cardiology, François Mach;Tunisia: Tunisian Society of Cardiology and Cardio-VascularSurgery, Abdallah Mahdhaoui; Turkey: Turkish Society of Cardiology,Dilek Ural; Ukraine: Ukrainian Association of Cardiology, ElenaNesukay; United Kingdom: British Cardiovascular Society, ChrisGale.
7. References
Author notes
The disclosure forms of all experts involved in the development of these guidelines are available on the ESC website http://www.escardio.org/guidelines.
ESC Committee for Practice Guidelines (CPG) and National Cardiac Societies document reviewers: listed in the Appendix.
ESC entities having participated in the development of this document:
Associations: European Association for Cardiovascular Prevention & Rehabilitation (EACPR), European Association of Cardiovascular Imaging (EACVI), European Association of Percutaneous Cardiovascular Interventions (EAPCI), Heart Failure Association (HFA).
Councils: Council on Cardiovascular Nursing and Allied Professions, Council for Cardiology Practice, Council on Cardiovascular Primary Care.
Working Groups: Cardiovascular Pharmacotherapy
The content of these European Society of Cardiology (ESC) Guidelines has been published for personal and educational use only. No commercial use is authorized. No part of the ESC Guidelines may be translated or reproduced in any form without written permission from the ESC. Permission can be obtained upon submission of a written request to Oxford University Press, the publisher of the European Heart Journal and the party authorized to handle such permissions on behalf of the ESC.
Disclaimer. The ESC Guidelines represent the views of the ESC and were produced after careful consideration of the scientific and medical knowledge and the evidence available at the time of their publication. The ESC is not responsible in the event of any contradiction, discrepancy and/or ambiguity between the ESC Guidelines and any other official recommendations or guidelines issued by the relevant public health authorities, in particular in relation to good use of healthcare or therapeutic strategies. Health professionals are encouraged to take the ESC Guidelines fully into account when exercising their clinical judgment, as well as in the determination and the implementation of preventive, diagnostic or therapeutic medical strategies; however, the ESC Guidelines do not override, in any way whatsoever, the individual responsibility of health professionals to make appropriate and accurate decisions in consideration of each patient's health condition and in consultation with that patient and, where appropriate and/or necessary, the patient's caregiver. Nor do the ESC Guidelines exempt health professionals from taking into full and careful consideration the relevant official updated recommendations or guidelines issued by the competent public health authorities, in order to manage each patient's case in light of the scientifically accepted data pursuant to their respective ethical and professional obligations. It is also the health professional's responsibility to verify the applicable rules and regulations relating to drugs and medical devices at the time of prescription.