-
PDF
- Split View
-
Views
-
Cite
Cite
Hanno L Tan, Nikolaos Dagres, Bernd W Böttiger, Peter J Schwartz, ESCAPE-NET Investigators, European Sudden Cardiac Arrest network: towards Prevention, Education and New Effective Treatments (ESCAPE-NET): A major European Horizon 2020 project focused on cardiac arrest, European Heart Journal, Volume 39, Issue 2, 07 January 2018, Pages 86–88, https://doi.org/10.1093/eurheartj/ehx758
Close - Share Icon Share
Sudden cardiac arrest (SCA) is a public health problem, accounting for 50% of cardiovascular deaths and 20% of all natural deaths in Western societies. This problem is expected to rise further as the population ages, since SCA mostly strikes individuals of advanced age (median age 65 years). Sudden cardiac arrest is caused by acute myocardial infarction, myocardial ischaemia and/or cardiac arrhythmia [ventricular fibrillation (VF)], which results from various, often interacting, causes. Sudden cardiac arrest is lethal within minutes if left untreated, yet mostly occurs in the community (out-of-hospital), where treatment is usually not immediately available. Accordingly, survival rates across Europe are presently only 10% on average.
While improvements in primary and secondary prevention have resulted in substantial declines in overall mortality from heart disease in general and coronary heart disease over the past 30 years, SCA rates have declined to a lesser extent. Clearly, SCA prevention is a major opportunity to further reduce mortality from heart disease. This requires early recognition of individuals at risk and an understanding of the causative factors on an individual’s level. This knowledge is still lacking, and the majority of SCA now occurs unexpectedly in individuals who are unaware of their increased risk. Much improvement must be gained here. Also, new treatment strategies for SCA have shown to increase survival rates. Further improvements in this area are also crucial.
Studies into the causes of SCA have so far focused on single causative factors, including traditional risk factors such as coronary artery disease and heart failure. These studies have yielded crude and imperfect risk stratification schemes that may result in failure to recognize individuals at risk or, conversely, unnecessary treatment associated with high complication risk and cost [e.g. implantable cardioverter-defibrillators (ICDs)] in individuals who do not need them.
Moreover, while great strides have been made in our identification and understanding of causative genes and variants therein which are associated with increased SCA risk, thanks to studies at Cardiogenetic clinics worldwide, these studies also have limited scope. These studies have shown that DNA information is not only highly useful to identify individuals at increased SCA risk, but also actionable: carriers of risk DNA profiles may receive timely treatment (ranging from lifestyle advice and drug use to prophylactic ICD implantations) to reduce their risk of death from SCA. Yet, such studies typically involve young individuals with monogenic diseases, in which a single rare DNA variant (mutation) is sufficient to cause SCA.
However, the majority of SCA victims in the general population have a private set of acquired and inherited risk factors (including polymorphisms, i.e. common DNA variants), that, in isolation, increase SCA risk only marginally, but whose interaction may culminate in SCA. Identifying these risk factors and understanding their interactions often has immediate therapeutic implications. For instance, drug use is hampered by the fact that various drugs (including drugs prescribed for non-cardiac disease) have the potential to increase SCA risk in vulnerable individuals because they impact on electrical properties of the heart. Being able to identify individuals with increased vulnerability to this adverse effect would increase the overall therapeutic benefit of these drugs, as they could be withheld only from vulnerable individuals, while they could be prescribed with more liberty (and greater therapeutic effect) to non-vulnerable individuals. Clearly, designing a risk score that takes multiple interacting risk factors into account may lead to tailored therapy which saves lives and is more cost-efficient.
Studies in resuscitation science have also yielded the exciting insight that various improvements in resuscitation care have incrementally increased survival rates from out-of-hospital SCA. At present, great efforts are aimed at shortening the delay between onset of VF and defibrillation. These efforts are centred on lay resuscitation by bystanders, fast deployment of automated external defibrillators (AEDs) by trained volunteer lay rescuers. This requires a concerted effort of the resuscitation science community, policy makers, and the general population, because various critical steps must be taken to ensure their overall efficacy.
These include dissemination to the general population and their training in basic life support and the use of AED, strategic placement of AEDs at locations where SCA is most likely to occur, and sophisticated telecommunication technologies to alert the nearest volunteer lay rescuer of an ongoing SCA and to guide him/her to the scene of SCA and/or the nearest AED (‘First Responder’). Clearly, these efforts have paid off, as survival rates after SCA in regions where these strategies have been implemented have risen sharply. While there is proven direct benefit in elucidating the causes of SCA and establishing the best resuscitation efforts, these efforts are greatly hampered by the fact that collection of data and biosamples for DNA analysis of out-of-hospital SCA victims is very challenging and costly.
For instance, because VF turns into asystole within minutes if left untreated, SCA victims must be identified within minutes after VF onset to ascertain that their collapse resulted from VF (individuals who died suddenly without ECG documentation of VF may have died from non-cardiac causes, e.g. pulmonary embolism or stroke). Also, DNA collection in many countries is only allowed while the SCA victim is still alive. Yet, identifying SCA victims so rapidly is challenging because SCA usually occurs unexpectedly. Moreover, to fully understand the interacting factors that caused SCA, painstaking collection of highly detailed information (including clinical factors and drug use information) is required. These difficulties have resulted in the situation that SCA researchers, even after collecting SCA cases for many years, have each collected SCA cohorts that still lack the size and statistical power for the identification of all interacting risk factors for SCA which is needed to design risk scores for SCA occurrence.
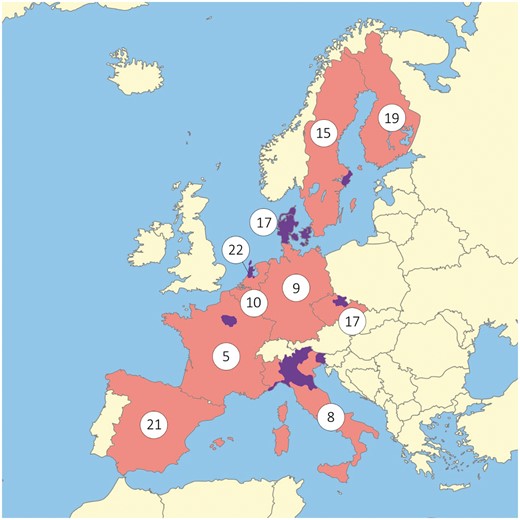
To overcome these difficulties, a public-private consortium of 16 partners across 10 European countries (The Netherlands, Denmark, France, Italy, Czech Republic, Sweden, Germany, Spain, Belgium, and Finland) have joined their forces in the European Sudden Cardiac Arrest network: towards Prevention, Education and New Effective Treatments project (ESCAPE-NET, www.escape-net.eu, Figure 1, Supplementary material online, Tables 1–3), funded by the European Union’s Horizon 2020 program, which has begun on 1 January 2017. This 5 years’ project will bring together 11 cohorts of SCA victims (n = 85 790 in total), along with detailed clinical and drug use information, and DNA samples (n = 15 000), in one joint harmonized database. In addition, five observational prospective population cohorts (n = 53 060 subjects) will be studied to obtain additional insights into the factors that contribute to SCA occurrence.
Large differences in survival rates after sudden cardiac arrest across Europe. Countries in orange indicate study sites of ESCAPE-NET; the catchment areas in these countries are indicated in purple. Numbers indicate survival rates (%) at hospital discharge of patients in whom cardiopulmonary resuscitation was attempted as reported in the EuReCa One Registry (survival rates in that registry were analysed in entire countries or parts thereof).
The increased power of this effort is expected to allow the researchers to identify the relevant risk factors for SCA occurrence, and to design risk scores for SCA occurrence based on them. Moreover, the ESCAPE-NET consortium is designed to achieve a comprehensive understanding of SCA in the general population by including researchers with complementary expertise. For instance, it brings researchers who study the causes of SCA at one table with resuscitation scientists. This synergy is expected to provide additional gains. For instance, resuscitation scientists mostly focus on situational factors that determine survival chances after resuscitation from SCA, but study patient characteristics less. Yet, recent reports indicate that patient characteristics also determine survival chances. By joining forces with scientists who study patient characteristics in detail to unravel the causes of SCA, resuscitation scientists may use these characteristics to develop tailored resuscitation strategies.
Various other elements will be studied in the ESCAPE-NET project that have received less attention in SCA research, but are likely to be of additional relevance. Studies into the role of socio-economic and environmental stress in SCA occurrence and survival after SCA will be conducted, along with cost-effectiveness analyses of various prevention and resuscitation strategies. Finally, the fact that large cohorts containing sensitive patient information will be brought together and shared across various European countries provides an opportunity to develop methods that ensure data protection in accordance with the European Union’s General Data Protection Regulation (Regulation EU 2016/679) that will come into effect in 2018.
One specific aim of the ESCAPE-NET project is to maximize its own impact. This will be achieved by implementing intensive dissemination efforts. Such efforts are aimed at education of basic scientists and clinicians who study and treat SCA. Moreover, the ESCAPE-NET consortium will reach out to other stakeholders (scientists, clinicians, and policy makers) involved in SCA, who are interested in collaborating with the ESCAPE-NET consortium and joining its efforts. To achieve these aims, the ESCAPE-NET consortium includes the key European organizations that are dedicated to research into the causes of SCA (European Heart Rhythm Association; EHRA—representing the European Society of Cardiology; ESC) and research into the optimal resuscitation strategies for SCA (European Resuscitation Council; ERC).
Through the creation of this extensive European network dedicated to SCA research and its open invitation to other stakeholders to join its efforts, the ESCAPE-NET consortium aims to fulfil its mission to reduce the burden of SCA in the community, and to continue these efforts even beyond the completion of the ESCAPE-NET project.
Hanno L. Tan (Coordinator of ESCAPE-NET)1, Nikolaos Dagres2, Bernd W. Böttiger3, Peter J. Schwartz4, on behalf of the ESCAPE-NET Investigators5
1Department of Cardiology, Heart Center, Academic Medical Center, Amsterdam, The Netherlands; 2European Heart Rhythm Association, representing the European Society of Cardiology, Sophia Antipolis, France; 3European Resuscitation Council, Nil, Belgium, and Department of Anaesthesiology and Intensive Care Medicine, University Hospital of Cologne, Germany; 4Center for Cardiac Arrhythmias of Genetic Origin, IRCCS Istituto Auxologico Italiano, Milan, Italy; and 5A full list of the ESCAPE-NET Investigators is provided in the Acknowledgements (supplementary material online).
Address for correspondence: Peter J. Schwartz, MD Center for Cardiac Arrhythmias of Genetic Origin IRCCS Istituto Auxologico Italiano Via Pier Lombardo, 22 20135 Milan, Italy Tel. +390255000408 Fax +390255000411 e-mail: peter.schwartz@unipv.it; p.schwartz@auxologico.it
Supplementary material
Supplementary material is available at European Heart Journal online.
Acknowledgement
Bernd Böttiger is supported by the ERC Research NET.
Funding
The ESCAPE-NET project has received funding from the European Union’s Horizon 2020 research and innovation programme under (Grant Agreement No. 733381).
Conflict of interest: none declared.
Author notes
A full list of the ESCAPE-NET Investigators is provided in Acknowledgements Supplementary material online.