-
PDF
- Split View
-
Views
-
Cite
Cite
Luka Nicin, Wesley Tyler Abplanalp, Hannah Mellentin, Badder Kattih, Lukas Tombor, David John, Jan D Schmitto, Jörg Heineke, Fabian Emrich, Mani Arsalan, Tomas Holubec, Thomas Walther, Andreas M Zeiher, Stefanie Dimmeler, Cell type-specific expression of the putative SARS-CoV-2 receptor ACE2 in human hearts, European Heart Journal, Volume 41, Issue 19, 14 May 2020, Pages 1804–1806, https://doi.org/10.1093/eurheartj/ehaa311
Close - Share Icon Share
See page 1807 for the editorial comment on this article (doi: 10.1093/eurheartj/ehaa410)
The coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 infections imposes a major threat for the world’s healthcare systems and is leading to thousands of deaths. Angiotensin-converting enzyme 2 (ACE2) has been identified as a potential receptor for SARS coronavirus1 and is also considered the main receptor for SARS-CoV-2.2 SARS-CoV-2 binds to ACE2 via its glycosylated outer membrane spike proteins. ACE2 is highly expressed in the lung and heart, and is known for its vital role in the cardiovascular system.3–5 Although SARS-CoV-2 mainly invades alveolar epithelial cells, it can also cause myocardial injury, as assessed by increased troponin T and NT-proBNP levels accompanying increased cardiovascular symptoms in COVID-19-infected patients.6 , 7 It is unclear whether elevated biomarkers of cardiac injury (or long-term effects on the cardiovascular system) are directly caused by viral infection of cardiac tissue or are secondary to hypoxia and systemic inflammation. However, patients with underlying cardiovascular disease represent a significant proportion of the patients who may suffer from a severe course after COVID-19 infection.8 This situation may be aggravated by findings showing that ACE inhibitors, which are often used to treat cardiovascular diseases, augment the expression of the SARS-CoV-2 receptor ACE2 in lung cells.9 This is probably mediated by an effect on angiotensin II, which is known to reduce ACE2 expression.9 Thus, ACE inhibition decreases angiotensin II, leading to an indirect up-regulation of ACE2.9 The effect of angiotensin II receptor blockers (ARBs), which primarily target the angiotensin receptor 1, is unclear. One may speculate that ARBs indirectly reduce ACE2 levels by augmenting free angiotensin II levels, which in turn is expected to down-regulate ACE2 via activating the angiotensin receptor 2. However, the effect of the two different treatments on the expression of ACE2 in the heart requires further investigation.
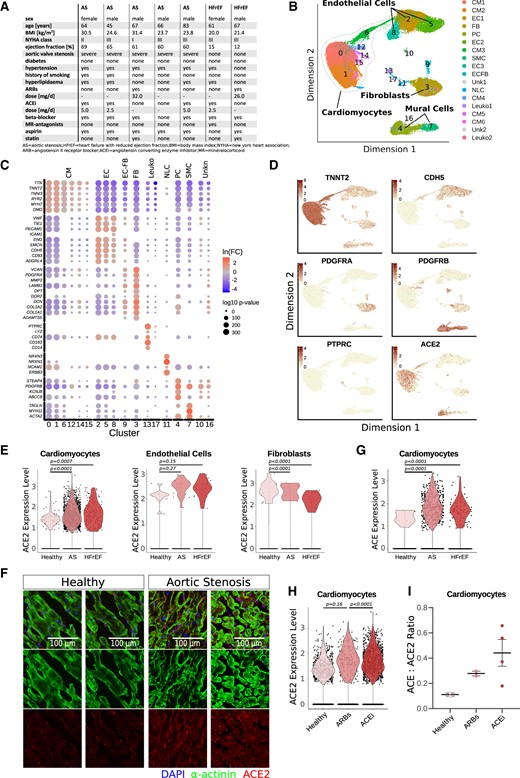
Therefore, we used single nuclei RNA sequencing to determine the expression of ACE and ACE2 in the different cell types of the human heart. Gene expression signatures were detected in cardiac tissues of five patients with aortic stenosis (AS) and two patients with heart failure with reduced ejection fraction (HFrEF) (Figure 1A) and compared with with samples of one healthy donor heart (age: 63 years, male) that was not used for transplantation. After single nuclei RNA sequencing, data were pooled, and unsupervised clustering was performed with a total of 57 601 nuclei. We found 18 distinct clusters. Using cell type-specific gene markers, major cell types were annotated, including cardiomyocytes (six clusters), fibroblasts (one cluster), endothelial cells (three clusters), leucocytes (two clusters), pericytes (one cluster), and smooth muscle cells (one cluster) (Figure 1B–D). ACE2 was expressed in cardiomyocytes (Cluster 0 and 1) and mural cells, particularly pericytes (Cluster 4), and was detected at a lower expression level in fibroblasts, endothelial cell, and leucocytes (Figure 1D). Comparison of ACE2 in a pooled analysis of nuclei of the different groups showed that ACE2 was significantly elevated in cardiomyocytes of patients with heart disease compared with healthy controls (Figure 1E). ACE2 was also slightly, but not significantly, increased in endothelial cells, and the expression was lower in fibroblasts of patients with heart disease compared with healthy controls (Figure 1E). Immunostaining confirmed an increased expression of ACE2 in cardiomyocytes of patients with aortic stenosis (Figure 1F).
Regulation of ACE and ACE2 expression in human hearts. (A) Baseline characteristics of patients. (B and C) Single nuclei RNA sequencing of left ventricular cardiac tissue of two samples from a healthy donor and seven patients with heart disease. Uniform manifold approximation and projection (UMAP) plot. CM, cardiomyocytes; EC, endothelial cell; FB, fibroblast; PC, pericytes; SMC, smooth muscle cells; ECFB, endothelial and fibroblast marker-expressing cluster; NLC, neuronal like cells; Unk, unknown (B); and representative marker gene expression in each cluster (C) are shown. (D) Representative cardiac (troponin T2, TNNT2), endothelial (VE-cadherin, CDH5), fibroblast (PDGFRA), mural cell (PDGFRB), and leucocyte (CD45, PTPRC) markers and expression of ACE2 are shown in UMI (unique molecular identifier) counts per cell. (E) Expression of ACE2 in clusters annotated in (B). (F) Immunostaining against ACE2 (ab15348, Abcam) in healthy human hearts and in patients with AS (representative images of n = 7 patients with AS are shown). (G) Expression of ACE in cardiomyocytes. (H and I) Expression of ACE2 and ACE/ACE2 ratios in cardiomyocytes of healthy donor patients treated with ARBs (n = 2) and ACE inhibitors (n = 4). Data are shown as mean ± SEM. Statistical analysis was performed using the unpaired, two-sided Student’s t-test. For comparisons of >2 groups, multiple-group ANOVA with a post-hoc Tukey’s test was used.
In addition, ACE was augmented in cardiomyocytes of patients with AS and HFrEF (Figure 1G). Interestingly, cardiomyocytes of patients who were treated with ACE inhibitors showed a significantly higher ACE2 expression compared with ARB-treated patients (Figure 1H). Moreover, patients treated with ACE inhibitors had an imbalance of ACE to ACE2 expression, with a more than four-fold higher ACE/ACE2 ratio compared with healthy control cells (Figure 1I).
In conclusion, these data provide novel insights into the cell type-specific expression and regulation of ACE2 in the heart. Patients with varying heart disease aetiology show augmented expression of ACE2 levels particularly in cardiomyocytes. Treatment with ACE inhibitors tends to be associated with increased ACE2 mRNA and unfavourable ACE/ACE2 ratios, which are believed to be a driver of cardiovascular pathologies.9 This study is limited by its small sample size and therefore is only hypothesis-generating. However, these novel data suggest that it will be important to monitor SARS-CoV-2-infected patients for cardiovascular complications and assess the impact of ARB/ACE inhibitor therapy.
Conflict of interest: none declared.
Acknowledgements
The authors acknowledge support by the DFG (Exc2026) and the Rolf M. Schwiete Foundation.
References
Author notes
ThomasWalther, Andreas M. Zeiher and Stefanie Dimmeler contributed equally to this work.