-
PDF
- Split View
-
Views
-
Cite
Cite
Thomas F Lüscher, Current management of supraventricular tachycardias: the 2019 ESC Guidelines, European Heart Journal, Volume 41, Issue 5, 1 February 2020, Pages 607–609, https://doi.org/10.1093/eurheartj/ehaa056
Close - Share Icon Share

For the podcast associated with this article, please visit https://academic.oup.com/eurheartj/pages/Podcasts.
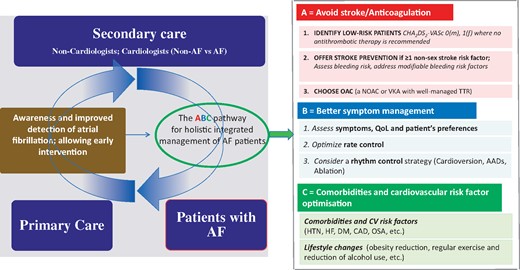
Arrythmias are an important symptom of a variety of cardiac diseases and are associated with significant morbidity and mortality. Supraventricular tachycardias are mostly not life threatening, but cause considerable symptoms impairing quality of life and—in the case of atrial fibrillation—are an important cause of embolic stroke1 and dementia.2 As outlined in ‘The year in cardiology: arrhythmias and pacing’ by A. John Camm from the St. George’s University London in the UK, and colleagues,3 this last year we have seen much progress with regard to the use of anticoagulants4–6 and the prevention of stroke and dementia,7 as well as ablation therapy for atrial fibrillation (Figure 18,9). Apart from recently issued European Society of Cardiology Guidelines for the management of patients with supraventricular arrhythmias—which are part of this Focus Issue—there has been little research progress in this field. Ventricular arrhythmias and device therapy, on the other hand, have seen modest progress, particularly as regards ventricular fibrosis and fatal arrythmias,10,11 which may become an important decision maker for device therapy in heart failure patients.
Managing atrial fibrillation—Easy as ABC (from Camm AJ, Lip GYH, Schilling R, Calkins H, Steffel J. The year in cardiology: arrhythmias and pacing. See pages 619–625).
Episodes of fast atrial fibrillation are highly symptomatic and often require direct-current cardioversion. Although quite safe, cardioversion is associated with thrombo-embolic events,5 even with anticoagulation, particularly vitamin K antagonists.5 Low-escalating energy shocks are common practice, but the optimal energy selection is unknown. In their FAST TRACK manuscript entitled ‘Maximum-fixed energy shocks for cardioverting atrial fibrillation’, Bo Løfgren and colleagues from the Aarhus University Hospital in Denmark compared maximum-fixed and low-escalating energy shocks for cardioverting atrial fibrillation.12 In a single-centre, single-blinded, randomized trial they allocated 276 elective atrial fibrillation patients to cardioversion using maximum-fixed (360–360–360 J) or low-escalating (125–150–200 J) biphasic truncated exponential shocks. Sinus rhythm 1 min after cardioversion was achieved in 88% in the maximum-fixed energy group, and in 66% in the low-escalating energy group. Sinus rhythm after first shock occurred in 75% in the maximum-fixed energy group compared with 34% in the low-escalating energy group. Thus, maximum-fixed energy shocks are more effective compared with low-escalating energy shocks for cardioverting atrial fibrillation, with similar safety. These clinically important findings are further discussed in an Editorial by Helmut Klein from the University of Rochester Medical Center in the USA.13
Patients with atrial fibrillation are usually seen by a cardiologist, but nurse-led care is increasingly common, and also in the management of other cardiac disease such as heart failure. Nurse-led care is expected to be more patient centred with the potential to reduce events. In their FAST TRACK ‘Nurse-led vs. usual care for atrial fibrillation’ Harry Crijns from the University Medical Centre Maastricht in the Netherlands and the RACE 4 Investigators randomized 1375 patients with atrial fibrillation to receive nurse-led care or usual care by specialized nurses.14 With nurse-led care, 81% patients received anticoagulation in accordance with the guidelines, as did 82% of the usual care patients. The cumulative adherence to guidelines-based recommendations was 61% under nurse-led care and 26% under usual care. Over 37 months, the primary endpoint occurred in 9.7% per year under nurse-led care and in 11.6% per year under usual care. There were 7.0% and 9.4% hospitalizations for arrhythmia events per year, and 0.7% and 1.1% per year for heart failure, respectively. Crijns et al. conclude that their trial failed to show that nurse-led care was superior to usual care. These results are put into context in an Editorial by Justin Ezekowitz from the University of Alberta in Edmonton, Alberta, Canada.15
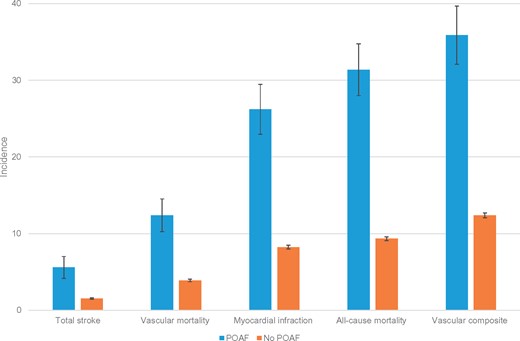
Perioperative atrial fibrillation is a common event and is most probably related to inflammation due to wound healing and/or infection.16 In their manuscript entitled ‘Risk of stroke and other adverse outcomes in patients with perioperative atrial fibrillation 1 year after non-cardiac surgery’, David Conen from the McMaster University in Hamilton, Canada and the CLIMA Investigators determined the 1-year risk of stroke and other adverse outcomes in patients with a new diagnosis of perioperative atrial fibrillation after non-cardiac surgery.17 The PeriOperative ISchemic Evaluation (POISE)-1 Trial compared metoprolol vs. placebo in 8351 patients, and POISE-2 compared aspirin vs. placebo, and clonidine vs. placebo in 10 010 patients with, or at risk of, cardiovascular disease undergoing non-cardiac surgery. Among 18 117 patients, 2.2% experienced perioperative atrial fibrillation. The stroke incidence 1 year after surgery was 5.58 vs. 1.54 per 100 patient-years in patients with and without perioperative atrial fibrillation, with an adjusted hazard ratio of 3.43 (Figure 2). Patients with perioperative atrial fibrillation also had an increased risk of death, with an adjusted hazard ratio of 2.51, and myocardial infarction, with an adjusted hazard ratio of 5.10 (Figure 2). Thus, although less common than anticipated, perioperative atrial fibrillation is associated with a significantly increased risk of stroke, infarction, and death at 1 year. Whether and what intervention studies might now be necessary is further discussed in an Editorial by Dipak Kotecha from the University of Birmingham College of Medical and Dental Sciences in Birmingham, UK.18
Incidence of adverse events among patients with and without perioperative atrial fibrillation Data are incidence rates per 100 patient-years of follow-up. Error bars indicate 95% confidence intervals. POAF, perioperative atrial fibrillation (from Conen D, Alonso-Coello P, Douketis J, Chan MTV, Kurz A, Sigamani A, Parlow JL, Wang CY, Villar JC, Srinathan SK, Tiboni M, Malaga G, Guyatt G, Sivakumaran S, Funes M-VR, Cruz P, Yang H, Dresser GK, Alvarez-Garcia J, Schricker T, Jones PM, Drummond LW, Balasubramanian K, Yusuf S, Devereaux PJ. Risk of stroke and other adverse outcomes in patients with perioperative atrial fibrillation 1 year after non-cardiac surgery. See pages 645–651).
This issue also contains the ‘2019 ESC Guidelines for the management of patients with supraventricular tachycardia. The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC): Developed in collaboration with the Association for European Paediatric and Congenital Cardiology (AEPC)’ by Josep Brugada and colleagues from the ESC Scientific Document Group.19
Lastly, the issue is complemented by two Discussion Forum contributions. In a first one entitled ‘Bang for the buck: the importance of modifiable factors for electrical cardioversion of atrial fibrillation’, David Birnie and colleagues from the University of Ottawa Heart Institute in Canada comment on the study published in this issue entitled ‘Maximum-fixed energy shocks for cardioverting atrial fibrillation’.12,20 Løfgren and colleagues respond to it in their contribution.21
The editors hope that this issue of the European Heart Journal will be of interest to its readers.
With thanks to Amelia Meier-Batschelet for help with compilation of this article.