-
PDF
- Split View
-
Views
-
Cite
Cite
Zhongyou Li, Wentao Jiang, Yu Chen, Guanshi Wang, Fei Yan, Tao Zeng, Haidong Fan, Acute and short-term efficacy of sauna treatment on cardiovascular function: Ameta-analysis, European Journal of Cardiovascular Nursing, Volume 20, Issue 2, February 2021, Pages 96–105, https://doi.org/10.1177/1474515120944584
Close - Share Icon Share
Abstract
The role of sauna bathing in cardiovascular function treatment has been increasingly explored, but insufficient attention has been paid to its efficacy. We performed a meta-analysis to provide more evidence for the efficacy of sauna treatment in cardiovascular nursing.
Sixteen peer-reviewed journal articles were screened to summarize the efficacy of the sauna on cardiovascular function. Both acute (0–30 min after the sauna) and short-term (2–4 weeks following the sauna treatment) efficacies were investigated.
For pooled acute efficacy, body temperature and heart rate significantly (p < 0.001) grew by 0.94°C and 17.86 beats/min, respectively; reductions of 5.55 mmHg (p < 0.001) and 6.50 mmHg (p < 0.001) were also observed in systolic blood pressure and diastole blood pressure, respectively. For combined short-term efficacy, left ventricular ejection fraction (LVEF), 6-min walk distance, and flow-mediated dilation (p < 0.001) increased by 3.27%, 48.11 m, and 1.71%, respectively; greater amelioration in LVEF was observed in participants with lower LVEF. The proportion of patients with New York Heart Association class III and IV decreased by 10.9% and 12.2%, respectively. Systolic blood pressure, diastolic blood pressure, brain natriuretic peptide concentration, left ventricular end-diastolic dimension, cardiothoracic ratio, and left atrial dimension reduced by 5.26 mmHg (p < 0.001), 4.14 mmHg (p < 0.001), 116.66 pg/mL (p < 0.001), 2.79 mm (p < 0.001), 2.628% (p < 0.05), and 1.88 mm (p < 0.05), respectively, while the concentration of norepinephrine in the plasma remained unchanged.
Sauna treatment was found to play a positive role in improving cardiovascular function and physical activity levels, especially in patients with low cardiovascular function. These findings reveal that thermal intervention may be a promising means for cardiovascular nursing.
Introduction
Individualized exercise training is a crucial component of cardiovascular nursing, but target heart rate, an empirical assessment method for training intensity,1,2 may not be applicable to some special populations, such as high-risk patients and patients who have recently been discharged from the hospital. Therefore, there is an urgent requirement for additional strategies for cardiovascular nursing which can be utilized in a wider population. As opposed to exercise training, sauna treatment with no strenuous individualized program may be a rewarding strategy for cardiovascular nursing due to its potential efficacy and mild intensity. For example, the sauna contributed to the amelioration of vascular endothelial function,3–5 left ventricular ejection fraction (LVEF)4,6–9 and exercise tolerance.5,6 Moreover, a long-term follow-up study10 also concluded that the prevalence of cardiovascular disease declined with increasing sauna frequency.
However, there is limited research and evidence for the role of sauna in cardiovascular function. Through an analysis of physiology, a strong relationship between human cardiovascular fitness and ambient temperature is coming into focus, as vasoconstriction and vasodilation are regulated by temperature. For example, previous studies found a higher cardiovascular risk caused by vasoconstriction in winter,11–14 while recent research15 revealed that the risk of myocardial infarction decreased by 2.8% for every 7.4°C increase in temperature, which was strongly correlated with vasodilation. Specifically, noradrenaline, secreted from the sympathetic vasoconstrictor when the human body is stimulated by low temperature, binds to alpha-receptors in the vascular smooth muscle cells, resulting in vasoconstriction. Thus, blood perfusion decreases and the hemodynamic environment worsens. Inversely, through stimulus by heat, the reduction in peripheral vascular resistance resulting from the opening of plentiful arteriovenous anastomoses allowed for an improvement in hemodynamic status. Consequently, it appears that thermal intervention, such as sauna treatment, plays a key role in cardiovascular function.
To date, insufficient attention has been paid to the contribution of sauna treatment. In particular, the link with cardiovascular nursing is unclear as thermal-induced vasodilation is rarely used in nursing practice or as a dedicated treatment for nursing or rehabilitation. Although recent studies16,17 have summarized the effects of sauna treatment on heart failure and have drawn some valuable conclusions, the analyses were not sufficiently comprehensive. For example, the amount of data included in these works is relatively small; a sub-analysis of the duration of sauna treatment is lacking; acute efficacy has not been clearly identified and the relationship between acute and chronic efficacy has not been discussed. The effects of sauna treatment on physical activity were also not ascertained, and its association with cardiovascular function recovery remains unclear. Therefore, we reviewed the acute and short-term efficacy of sauna treatment on cardiovascular function via related citations, with the objective of providing more comprehensive evidence for its efficacy in cardiovascular nursing and prevention.
Methods
Purpose and definitions
This meta-analysis was performed by summarizing data from citations to explore more detailed efficacy of sauna treatment in cardiovascular function, including acute and short-term efficacy. Acute efficacy corresponded to acute response (0–30 min after the sauna) including body temperature, heart rate (HR), systolic blood pressure (SBP) and diastolic blood pressure (DBP). Short-term efficacy was denoted as the effect of 2–4 weeks treatment on cardiovascular indicators and physical activity levels, such as LVEF, HR, SBP, DBP, brain natriuretic peptide (BNP), left ventricular end-diastolic dimension (LVEDD), cardiothoracic ratio (CTR), left atrial dimension (LAD), norepinephrine, flow-mediated dilation (FMD), 6-min walk distance (6MWD) and New York Heart Association (NYHA) class
Literature search strategy
Automatic searches of literature databases including Scopus, PubMed, Ovid Medline and Embase were used to analyze the relationship between the sauna treatment and cardiovascular function (search strategies are shown in the Supplementary Material online). Medical Subject Headings were also used in PubMed, Medline and Embase. All records included in this work were English publications. Identified citations were first screened based on title and abstract and then based on full text. Reviews, conference abstracts and other studies without useful data were excluded. The data were collected from 20 January 2019 to 25 April 2019 and were analyzed from 1 May 2019 to 10 June 2019.
Inclusion criteria
The inclusion criteria were as follows: (1) participants with cardiovascular diseases (such as heart failure) or asymptomatic individuals at risk for cardiovascular disease (such as smoking, hypertension or obesity); (2) acute efficacy including SBP, DBP, body temperature and HR; (3) related indicators of cardiovascular function were included in the records. For example, the primary outcomes of short-term efficacy included LVEF, HR, SBP and DBP, while secondary outcomes of short-term efficacy included concentration of plasma BNP, LVEDD, CTR, LAD, norepinephrine, FMD and 6MWD; (4) to ensure comparability of results, intervention conditions remained the same. Namely, patients in the sauna group were treated with sauna for 15 min, 5–10 times per week for 2–4 weeks. Following each sauna treatment, participants were kept warm for 30 min using a blanket.
Data collection and quality assessment
Data were gathered independently by one author (ZL) and verified by another author (TZ). The data extraction included author, year, efficacy (acute or short-term), follow-up duration (weeks), sample size and indicators of cardiovascular function. A Cochrane18 risk of bias assessment was applied to check the quality of included publications, and risk level was judged as low, unclear or high.19
Publication bias assessment
Publication bias was assessed using Egger’s test,20 Begg’s test21 and funnel plot.22 More than three articles were considered in the publication bias analysis. Dual and Tweedie’s ‘Trim and Fill’ method23 was utilized to avoid publication bias.
Data analysis
The pooled effects were described by forest plots generated by R software (version 3.6.1). Differences between the sauna and control groups were reflected using the weighted mean difference and a 95% confidence interval. Cochrane’s Q test24 was then used to determine the heterogeneity with an I2 value greater than 50% or p-value lower than 0.05, and a random-effect model was used to treat heterogeneity.25 Furthermore, the primary outcomes of short-term efficacy such as LVEF, HR, SBP and DBP were composed of three subgroups (2–4 weeks), and two subgroups (0 and 30 min) were taken into consideration for the acute response.
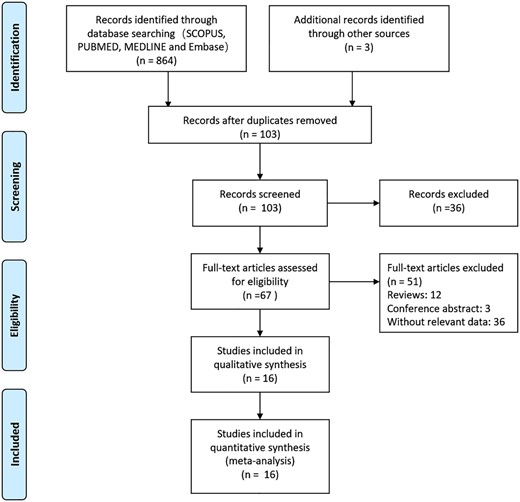
Characteristics of selection studies
The screening process of citations is illustrated in Figure 1. First, a total of 864 studies were searched, and 103 studies remained after duplicates were removed. Sixty-seven articles remained eligible for a full-text check. Finally, 16 articles were incorporated into the analysis after excluding the reviews, conference abstracts and studies without relevant data. Basic information showed that there were seven randomized controlled trials3,26–31 and nine non-randomized controlled trials5,6,32–38 (Table 1), which included 968 participants of 38–69 years of age. The majority of participants (at least 72%) were elderly and presented with chronic heart failure or risks for coronary artery disease (smoking, hypertension or obesity). There were 13 articles investigating short-term efficacy3,5,6,26–31,33,34,36,37 and three investigating acute efficacy.32,35,38
Basic information of included studies
| Author . | Year . | Design . | Efficacy . | Followed up, week . | Control group . | Sauna group . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n . | Mean age (SD) . | NYHA I/II/III/IV . | Population . | n . | Mean age (SD) . | NYHA I/II/III/IV . | Population . | |||||
| Kihara3 | 2002 | RCT | Chronic | 2 | 10 | 64 (16) | 0/5/5/0 | CHF | 20 | 62 (15) | 1/14/5/0 | CHF |
| Kihara26 | 2004 | RCT | Chronic | 2 | 10 | 59 (4) | 0/2/8/0 | CHF | 20 | 59 (3) | 0/5/15/0 | CHF |
| Miyata27 | 2008 | RCT | Chronic | 2 | 76 | 66 (14) | 2.51 | CHF | 112 | 63 (13) | 2.61 | CHF |
| Kuwahata28 | 2011 | RCT | Chronic | 4 | 27 | 64 (16) | 0/13/10/4 | CHF | 27 | 63 (15) | 0/12/11/4 | CHF |
| Fujita29 | 2011 | RCT | Chronic | 4 | 20 | 65 (13) | 0/18/2/0 | CHF | 20 | 64 (14) | 0/17/3 | CHF |
| Ichiki30 | 2017 | RCT | Chronic | 2 | 73 | _ | _ | CHF | 76 | _ | _ | CHF |
| Tei31 | 2016 | RCT | Chronic | 2 | 73 | 66 (15) | 0/30/33/10 | CHF | 76 | 66 (16) | 0/33/35/8 | CHF |
| Tei32 | 1995 | NRCT | Acute | 20 | _ | _ | CHF | 20 | _ | _ | CHF | |
| Tei33 | 1996 | NRCT | Chronic | 4 | 56 | _ | 0/0/23/33 | CHF | 53 | _ | 0/0/23/33 | CHF |
| Imamura34 | 2001 | NRCT | Chronic | 2 | 10 | 38 (7) | _ | APs | 25 | 38 (7) | _ | APRCADs |
| Miyamoto6 | 2005 | NRCT | Chronic | 4 | 15 | 63 (14) | 0/3/12/0 | CHF | 15 | 63 (14) | 0/3/12/0 | CHF |
| Kisanuki35 | 2007 | NRCT | Acute | 10 | 62 (16) | 0/2/8/0 | CHF | 10 | 62 (16) | 0/2/8/0 | CHF | |
| Sohn36 | 2010 | NRCT | Chronic | 2 | 10 | 62 (9) | 0/7/3/0 | CHF | 10 | 62 (9) | 0/7/3/0 | CHF |
| Ohori5 | 2012 | NRCT | Chronic | 3 | 41 | 68 (14) | 4/15/22/0 | CHF | 41 | 68 (14) | 4/15/22/0 | CHF |
| Sobajima37 | 2015 | NRCT | Chronic | 3 | 49 | 69 (14) | 6/15/28/0 | CHF | 49 | 69 (14) | 6/15/28/0 | CHF |
| Laukkanen38 | 2018 | NRCT | Acute | 102 | 52 (9) | _ | APRCADs | 102 | 52 (9) | _ | APRCADs | |
| Author . | Year . | Design . | Efficacy . | Followed up, week . | Control group . | Sauna group . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n . | Mean age (SD) . | NYHA I/II/III/IV . | Population . | n . | Mean age (SD) . | NYHA I/II/III/IV . | Population . | |||||
| Kihara3 | 2002 | RCT | Chronic | 2 | 10 | 64 (16) | 0/5/5/0 | CHF | 20 | 62 (15) | 1/14/5/0 | CHF |
| Kihara26 | 2004 | RCT | Chronic | 2 | 10 | 59 (4) | 0/2/8/0 | CHF | 20 | 59 (3) | 0/5/15/0 | CHF |
| Miyata27 | 2008 | RCT | Chronic | 2 | 76 | 66 (14) | 2.51 | CHF | 112 | 63 (13) | 2.61 | CHF |
| Kuwahata28 | 2011 | RCT | Chronic | 4 | 27 | 64 (16) | 0/13/10/4 | CHF | 27 | 63 (15) | 0/12/11/4 | CHF |
| Fujita29 | 2011 | RCT | Chronic | 4 | 20 | 65 (13) | 0/18/2/0 | CHF | 20 | 64 (14) | 0/17/3 | CHF |
| Ichiki30 | 2017 | RCT | Chronic | 2 | 73 | _ | _ | CHF | 76 | _ | _ | CHF |
| Tei31 | 2016 | RCT | Chronic | 2 | 73 | 66 (15) | 0/30/33/10 | CHF | 76 | 66 (16) | 0/33/35/8 | CHF |
| Tei32 | 1995 | NRCT | Acute | 20 | _ | _ | CHF | 20 | _ | _ | CHF | |
| Tei33 | 1996 | NRCT | Chronic | 4 | 56 | _ | 0/0/23/33 | CHF | 53 | _ | 0/0/23/33 | CHF |
| Imamura34 | 2001 | NRCT | Chronic | 2 | 10 | 38 (7) | _ | APs | 25 | 38 (7) | _ | APRCADs |
| Miyamoto6 | 2005 | NRCT | Chronic | 4 | 15 | 63 (14) | 0/3/12/0 | CHF | 15 | 63 (14) | 0/3/12/0 | CHF |
| Kisanuki35 | 2007 | NRCT | Acute | 10 | 62 (16) | 0/2/8/0 | CHF | 10 | 62 (16) | 0/2/8/0 | CHF | |
| Sohn36 | 2010 | NRCT | Chronic | 2 | 10 | 62 (9) | 0/7/3/0 | CHF | 10 | 62 (9) | 0/7/3/0 | CHF |
| Ohori5 | 2012 | NRCT | Chronic | 3 | 41 | 68 (14) | 4/15/22/0 | CHF | 41 | 68 (14) | 4/15/22/0 | CHF |
| Sobajima37 | 2015 | NRCT | Chronic | 3 | 49 | 69 (14) | 6/15/28/0 | CHF | 49 | 69 (14) | 6/15/28/0 | CHF |
| Laukkanen38 | 2018 | NRCT | Acute | 102 | 52 (9) | _ | APRCADs | 102 | 52 (9) | _ | APRCADs | |
NYHA: New York Heart Association; RCT: randomized controlled trial; NRCT non-randomized controlled trial; CHF: chronic heart failure; AP: asymptomatic participant; APRCAD: asymptomatic participant with risks for coronary artery disease (smoking, hypertension or obesity)
Basic information of included studies
| Author . | Year . | Design . | Efficacy . | Followed up, week . | Control group . | Sauna group . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n . | Mean age (SD) . | NYHA I/II/III/IV . | Population . | n . | Mean age (SD) . | NYHA I/II/III/IV . | Population . | |||||
| Kihara3 | 2002 | RCT | Chronic | 2 | 10 | 64 (16) | 0/5/5/0 | CHF | 20 | 62 (15) | 1/14/5/0 | CHF |
| Kihara26 | 2004 | RCT | Chronic | 2 | 10 | 59 (4) | 0/2/8/0 | CHF | 20 | 59 (3) | 0/5/15/0 | CHF |
| Miyata27 | 2008 | RCT | Chronic | 2 | 76 | 66 (14) | 2.51 | CHF | 112 | 63 (13) | 2.61 | CHF |
| Kuwahata28 | 2011 | RCT | Chronic | 4 | 27 | 64 (16) | 0/13/10/4 | CHF | 27 | 63 (15) | 0/12/11/4 | CHF |
| Fujita29 | 2011 | RCT | Chronic | 4 | 20 | 65 (13) | 0/18/2/0 | CHF | 20 | 64 (14) | 0/17/3 | CHF |
| Ichiki30 | 2017 | RCT | Chronic | 2 | 73 | _ | _ | CHF | 76 | _ | _ | CHF |
| Tei31 | 2016 | RCT | Chronic | 2 | 73 | 66 (15) | 0/30/33/10 | CHF | 76 | 66 (16) | 0/33/35/8 | CHF |
| Tei32 | 1995 | NRCT | Acute | 20 | _ | _ | CHF | 20 | _ | _ | CHF | |
| Tei33 | 1996 | NRCT | Chronic | 4 | 56 | _ | 0/0/23/33 | CHF | 53 | _ | 0/0/23/33 | CHF |
| Imamura34 | 2001 | NRCT | Chronic | 2 | 10 | 38 (7) | _ | APs | 25 | 38 (7) | _ | APRCADs |
| Miyamoto6 | 2005 | NRCT | Chronic | 4 | 15 | 63 (14) | 0/3/12/0 | CHF | 15 | 63 (14) | 0/3/12/0 | CHF |
| Kisanuki35 | 2007 | NRCT | Acute | 10 | 62 (16) | 0/2/8/0 | CHF | 10 | 62 (16) | 0/2/8/0 | CHF | |
| Sohn36 | 2010 | NRCT | Chronic | 2 | 10 | 62 (9) | 0/7/3/0 | CHF | 10 | 62 (9) | 0/7/3/0 | CHF |
| Ohori5 | 2012 | NRCT | Chronic | 3 | 41 | 68 (14) | 4/15/22/0 | CHF | 41 | 68 (14) | 4/15/22/0 | CHF |
| Sobajima37 | 2015 | NRCT | Chronic | 3 | 49 | 69 (14) | 6/15/28/0 | CHF | 49 | 69 (14) | 6/15/28/0 | CHF |
| Laukkanen38 | 2018 | NRCT | Acute | 102 | 52 (9) | _ | APRCADs | 102 | 52 (9) | _ | APRCADs | |
| Author . | Year . | Design . | Efficacy . | Followed up, week . | Control group . | Sauna group . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n . | Mean age (SD) . | NYHA I/II/III/IV . | Population . | n . | Mean age (SD) . | NYHA I/II/III/IV . | Population . | |||||
| Kihara3 | 2002 | RCT | Chronic | 2 | 10 | 64 (16) | 0/5/5/0 | CHF | 20 | 62 (15) | 1/14/5/0 | CHF |
| Kihara26 | 2004 | RCT | Chronic | 2 | 10 | 59 (4) | 0/2/8/0 | CHF | 20 | 59 (3) | 0/5/15/0 | CHF |
| Miyata27 | 2008 | RCT | Chronic | 2 | 76 | 66 (14) | 2.51 | CHF | 112 | 63 (13) | 2.61 | CHF |
| Kuwahata28 | 2011 | RCT | Chronic | 4 | 27 | 64 (16) | 0/13/10/4 | CHF | 27 | 63 (15) | 0/12/11/4 | CHF |
| Fujita29 | 2011 | RCT | Chronic | 4 | 20 | 65 (13) | 0/18/2/0 | CHF | 20 | 64 (14) | 0/17/3 | CHF |
| Ichiki30 | 2017 | RCT | Chronic | 2 | 73 | _ | _ | CHF | 76 | _ | _ | CHF |
| Tei31 | 2016 | RCT | Chronic | 2 | 73 | 66 (15) | 0/30/33/10 | CHF | 76 | 66 (16) | 0/33/35/8 | CHF |
| Tei32 | 1995 | NRCT | Acute | 20 | _ | _ | CHF | 20 | _ | _ | CHF | |
| Tei33 | 1996 | NRCT | Chronic | 4 | 56 | _ | 0/0/23/33 | CHF | 53 | _ | 0/0/23/33 | CHF |
| Imamura34 | 2001 | NRCT | Chronic | 2 | 10 | 38 (7) | _ | APs | 25 | 38 (7) | _ | APRCADs |
| Miyamoto6 | 2005 | NRCT | Chronic | 4 | 15 | 63 (14) | 0/3/12/0 | CHF | 15 | 63 (14) | 0/3/12/0 | CHF |
| Kisanuki35 | 2007 | NRCT | Acute | 10 | 62 (16) | 0/2/8/0 | CHF | 10 | 62 (16) | 0/2/8/0 | CHF | |
| Sohn36 | 2010 | NRCT | Chronic | 2 | 10 | 62 (9) | 0/7/3/0 | CHF | 10 | 62 (9) | 0/7/3/0 | CHF |
| Ohori5 | 2012 | NRCT | Chronic | 3 | 41 | 68 (14) | 4/15/22/0 | CHF | 41 | 68 (14) | 4/15/22/0 | CHF |
| Sobajima37 | 2015 | NRCT | Chronic | 3 | 49 | 69 (14) | 6/15/28/0 | CHF | 49 | 69 (14) | 6/15/28/0 | CHF |
| Laukkanen38 | 2018 | NRCT | Acute | 102 | 52 (9) | _ | APRCADs | 102 | 52 (9) | _ | APRCADs | |
NYHA: New York Heart Association; RCT: randomized controlled trial; NRCT non-randomized controlled trial; CHF: chronic heart failure; AP: asymptomatic participant; APRCAD: asymptomatic participant with risks for coronary artery disease (smoking, hypertension or obesity)
Results
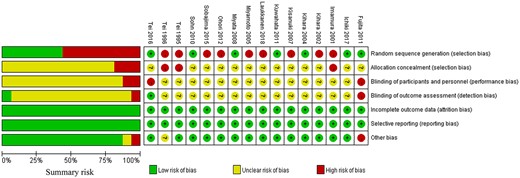
Quality assessment
The score of the quality assessment is presented in Figure 2. More than half of the citations were scored as having a high risk of bias due to a non-randomized design. Most of the publications were evaluated as having an unclear risk of bias for allocation concealment, blinding of participants, personnel and outcome assessment because insufficient information was supplied. All studies scored a low risk of bias for attrition and reporting biases because there were no incomplete outcome data or selective reporting. Additionally, most of the citations were assessed as having a low risk of other biases.
Risk of bias graph. Both summary risk (left panel) and risk for each study (right panel) are presented.
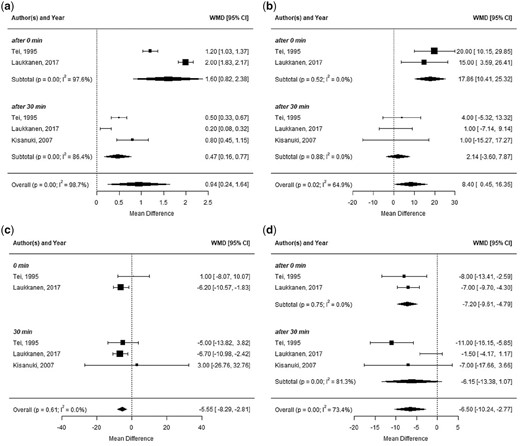
Acute efficacy of sauna treatment
Acute effect estimates (Figure 3) suggested that the combined effects of the sauna treatment resulted in significant (p < 0.001) increases in body temperature and HR, and greater (p < 0.001) reductions in SBP and DBP. No evidence for publication bias provided by Begg’s test, Egger’s test and funnel plot (Supplementary Material Figure 8) was observed.
Relationship between sauna treatment and acute response. (a), (b), (c) and (d) correspond to body temperature, heart rate, systolic blood pressure and diastolic blood pressure, respectively. WMD: weighted mean difference; CI: confidence interval.
Short-term efficacy of sauna treatment
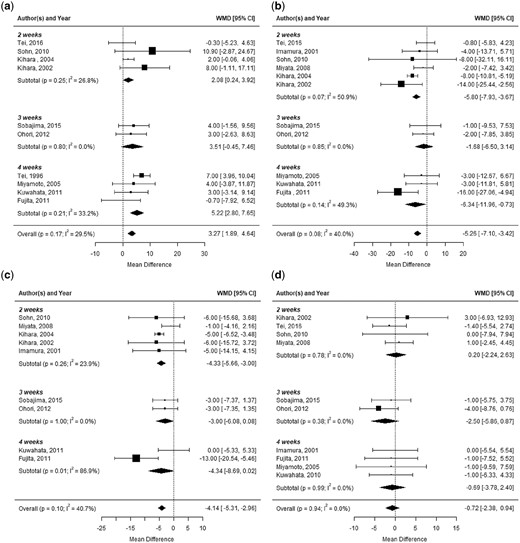
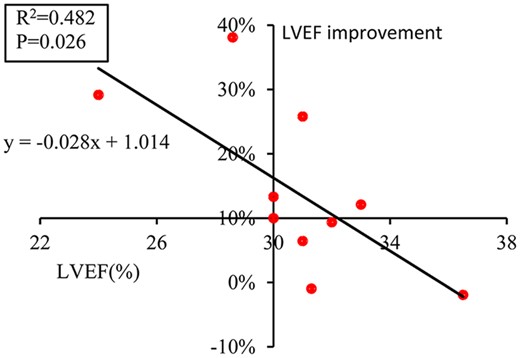
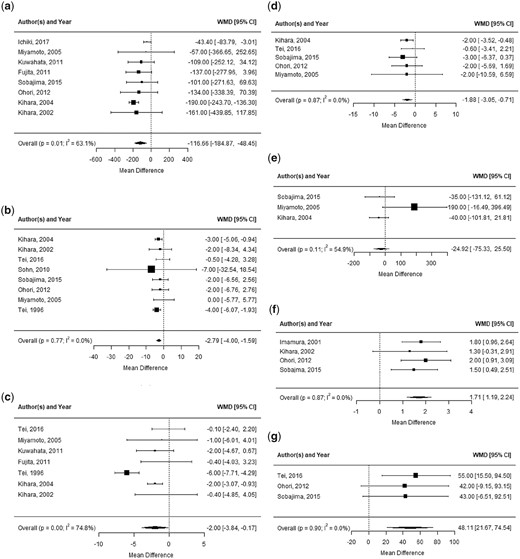
Primary outcomes (Figure 4) revealed that the pooled effect of LVEF significantly (p < 0.001) increased after the sauna intervention. Intriguingly, a more evident (p < 0.05) improvement in LVEF was noted in patients with lower LVEF (Figure 5). The summary effect of SBP notably decreased, and an apparent reduction in DBP was observed. Additionally, there was a slight (p=0.396) effect of sauna treatment on HR. Through the sub-analysis, the increment value of LVEF rose with increase in sauna duration, and the efficacy of SBP and DBP was more obvious with the four-week sauna intervention than with the 2–3 week sauna intervention. Among secondary indicators (Figure 6), the concentration of plasma BNP significantly (p < 0.001) decreased, while no significant (p=0.923) change in the concentration of norepinephrine was observed. The pooled effect showed that the intervention of the sauna treatment led to a striking (p < 0.05) decrease in cardiac geometry, including LVEDD, CTR and LAD. Additionally, the assessment of vascular function showed a significant elevation in FMD, and the exercise tolerance of patients achieved a satisfactory improvement in 6MWD. For publication bias, two ‘missing’ citations were added into CTR analysis through the ‘Trim and Fill’ method due to the asymmetric funnel plot (Supplementary Figure 8), while no publication bias was noted and no missing citation was required for possible bias in the analysis of other indicators.
Sauna and primary indicators. (a), (b), (c) and (d) correspond to left ventricular ejection fraction, systolic blood pressure, diastolic blood pressure and heart rate, respectively. Three subgroups were divided by intervention duration of two, three and four weeks, respectively. WMD: weighted mean difference; CI: confidence interval.
The relationship between left ventricular ejection fraction (LVEF) and ratio of LVEF improvement.
Sauna and secondary indicators. (a) to (g) correspond to brain natriuretic peptide, left ventricular end-diastolic dimension, cardiothoracic ratio, left atrial dimension, norepinephrine, % flow-mediated dilation and 6-min walk distance, respectively.
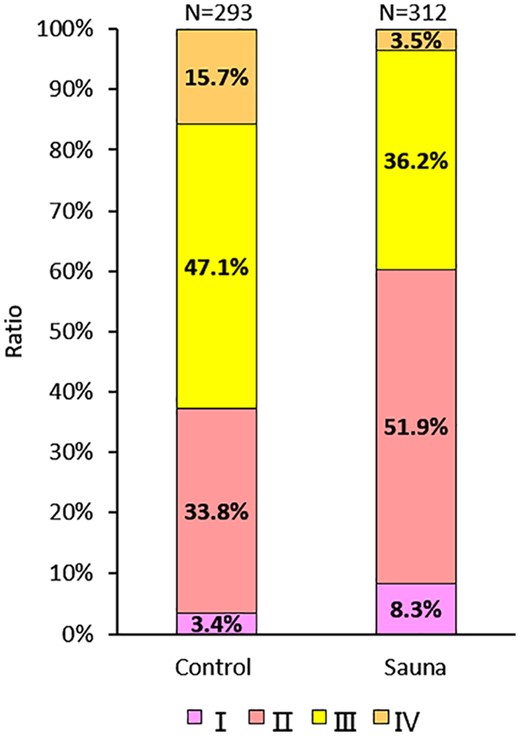
In addition, a total of 293 and 312 patients were diagnosed as NYHA class for the sauna and control groups, respectively, and the majority were in classes II and III (Figure 7). After the short-term sauna intervention, the proportion of patients with NYHA classes III and IV decreased by 10.9% and 12.2%, respectively.
Proportion of New York Heart Association functional class in the control and sauna groups.
Discussion
Sauna treatment with satisfactory efficacy and no complex individualized program may be a rewarding, convenient and low-cost strategy for cardiovascular nursing, especially for some special populations (high-risk patients and patients who have recently been discharged from the hospital) who are unable to participate in physical activity.
For acute efficacy of sauna treatment, our results showed that an increase in body temperature helped to keep the arteriovenous anastomoses open, resulting in a sustainable reduction in peripheral vascular resistance, to relieve the cardiac load and to promote blood circulation. Furthermore, the acute effect of HR in the sauna group was higher than that in the control group because the cardiac sympathetic nerve was dominated by heat stress,39 which is beneficial to the growth of cardiac output. Although beta-blockers are a factor in HR reduction, it may be inferred that the cardiac sympathetic nerve stimulated by heat stress released more neurotransmitters than beta-blockers originating from drugs, a factor that requires further exploration. Additionally, since peripheral vascular resistance decreased greatly at high temperatures, an acute reduction in blood pressure (BP) was observed.
The short-term efficacy of sauna treatment correlated well with the acute response to 45 min sauna therapy. Our summarized results highlighted that LVEF significantly increased after 2–4 weeks of the sauna treatment, which demonstrated that it was a beneficial strategy for promoting blood perfusion of organs and tissues. The mechanism of the efficacy of the sauna treatment is closely related to the self-regulation of the cardiovascular system induced by heat stress. Physiologically, a multitude of arteriovenous anastomoses start opening at higher temperatures, resulting in a reduction in peripheral vascular resistance. Previous studies4,8,32 discovered that the hemodynamic response to the sauna treatment was strongly evoked by peripheral vascular resistance reduction, which led to an increase in cardiac output. Furthermore, as peripheral vascular resistance declined, BP declined concomitantly. As with the acute efficacy, our short-term results exhibited a reduction of 5 mmHg and 4 mmHg in SBP and DBP, respectively. However, research4,40,41 on sauna treatment and hypertension found that excellent antihypertensive efficacy can be achieved. Their results (with ranges of 10–23 mmHg and 9–11 mmHg reduction in SBP and DBP respectively) reported a larger antihypertensive amplitude than our results, probably due to the inclusion of patients with lower BP in this study. Other than BP, a more evident improvement of LVEF was noted in patients with lower LVEF, indicating that the sauna treatment had a greater effect on participants with lower cardiovascular function, which provided strong support for the long-term follow-up observation of previous work.42,43 Furthermore, the consensus is that the cardiac output is related to blood pressure and peripheral resistance(Q = P/R, where Q, P and R represent cardiac output, blood pressure and resistance, respectively). Although both the blood pressure and resistance declined after 2–4 weeks of the sauna treatment, cardiac output still increased because resistance decreased more than blood pressure4 did (10.5–41.5% vs. 3.0–9.3%). Additionally, cardiac output also depends on HR but our results indicated that there was no significant change in HR after 2–4 weeks of the sauna treatment, demonstrating that the short-term improvement of cardiac output induced by the sauna treatment was independent of HR.
BNP and norepinephrine in the plasma are two biochemical indicators of cardiovascular function. Considering that more BNP is secreted by myocardial cells as the cardiac load increases, a high-concentration of BNP in plasma corresponds to weak cardiac function.44,45,46 Our results showed a significant reduction in BNP after 2–4 weeks of the sauna treatment because it relieved the cardiac load to inhibit the expression of the natriuretic peptide system. Norepinephrine binds to the alpha-receptor in vascular smooth muscle cells, resulting in vasoconstriction to decrease blood perfusion.47 However, there was minimal change in the concentration of norepinephrine after 2–4 weeks of the sauna treatment, which suggested that there was no vasoconstriction at high temperatures; namely, the improvement in cardiac output provoked by the sauna was independent of norepinephrine.
Cardiac geometry including LVEDD, CTR and LAD decreased significantly after 2–4 weeks of the sauna treatment, which revealed an improvement in cardiac function. For example, a reduction in LVEDD represented an enhancement in cardiac contractility, manifesting an increase in cardiac output. As CTR and LAD decreased, the sauna also played a positive role in cardiomegaly prevention because the cardiac load decreased with a decrease in peripheral vascular resistance.
Additionally, the mechanism of sauna treatment in cardiovascular function was also correlated with the improvement of arterial compliance. FMD has been widely used as a predictor of endothelium function.48,49 Our results indicated that FMD increased after 2–4 weeks of the sauna treatment, which could be interpreted as a hemodynamic factor: as the peripheral vascular resistance reduced, the wall shear stress inside blood vessels grew with increasing blood flow, leading to more nitric oxide being produced by endothelium cells to improve arterial function.50,51,52 Thermal intervention may be a promising strategy for preventing arterial stenosis or delaying restenosis.
Consequently, indicators including LVEF, SBP, DBP, BNP, LVEDD, CTR, LAD and FMD showed that cardiovascular function improved via the sauna, which may be beneficial for enhancing physical activity levels. After 2–4 weeks of the sauna treatment, the 6MWD was significantly improved, indicating that sauna treatment is a beneficial method for improving the level of physical activity of the participants. The effects of the sauna treatment on physical activity can be interpreted as being due, in part, to three factors: (1) as blood perfusion increased with the growth of cardiac output, the metabolism was enhanced; (2) cardiac tolerance improved with increasing cardiovascular function; (3) the blood supply to limb muscles increased with cardiac output growth, leading to an enhancement of muscular strength. Meanwhile, our results showed an evident change in the distribution of the NYHA class, illustrating that nearly 23% of patients with severe heart failure were able to restore their physical activities within 2–4 weeks.
Limitation
This work is important for an understanding of the potential efficacy of sauna treatment of cardiovascular function, but there remain some limitations. First, the absence of methods including randomization, blinding and allocation concealment implementation in most citations led to an effect on the total credibility of this work, and thus more scientific trials are still required. Second, as most of the participants included in this study were elderly, the applicability of the conclusion to more populations with different ages still has yet to be explored. Third, only three publications in terms of acute efficacy were involved, suggesting that additional studies of sauna treatment in acute efficacy are also required. Finally, since most patients had chronic heart failure and only a few asymptomatic participants with risks for coronary artery disease were studied, the sauna treatment provided more data for the treatment of heart failure, and further research is needed in other populations.
Conclusion
With a reduction in peripheral vascular resistance and an increase in blood flow, sauna treatment actively promotes the amelioration of cardiovascular function, which improves physical activity levels. Additionally, the sauna treatment had a greater effect on patients with lower cardiovascular function. Consequently, thermal therapy may be developed as a common means of cardiovascular nursing.
Supplemental material
Supplementary material is available at European Journal of Cardiovascular Nursing online.
Declaration of conflicting interests
The authors have no conflicts of interest to declare.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by Grants-in-Aid from the National Natural Science Foundation of China (Nos.11772210 and 11272224) and the National Key Research and Development Program (No.2017YFB0702500).



Comments