-
PDF
- Split View
-
Views
-
Cite
Cite
Tiange Wang, Zhiyun Zhao, Yu Xu, Lu Qi, Min Xu, Jieli Lu, Mian Li, Yuhong Chen, Meng Dai, Wenhua Zhao, Guang Ning, Weiqing Wang, Yufang Bi, Insulin Resistance and β-Cell Dysfunction in Relation to Cardiometabolic Risk Patterns, The Journal of Clinical Endocrinology & Metabolism, Volume 103, Issue 6, June 2018, Pages 2207–2215, https://doi.org/10.1210/jc.2017-02584
Close - Share Icon Share
Abstract
Insulin resistance (IR) and β-cell dysfunction are two major defects synergistically inducing the development of diabetes and related cardiometabolic disorders.
To investigate the independent and joint associations of IR and β-cell dysfunction with the prevalence of multiple cardiometabolic disorders, including obesity, central obesity, diabetes, dyslipidemia, and hypertension.
A nationally representative population of 93,690 Chinese adults.
IR and β-cell dysfunction were assessed by the homeostasis model assessment of IR (HOMA-IR) and of β-cell function (HOMA-B), respectively.
High HOMA-IR was independently associated with high prevalence of all estimated cardiometabolic disorders, whereas low HOMA-B was independently associated with high prevalence of diabetes, dyslipidemia, and hypertension but low prevalence of obesity and central obesity. When examined jointly, the associations of HOMA-IR and HOMA-B with multiple cardiometabolic disorders showed different patterns with varying magnitudes. The strongest joint associations were observed for diabetes, with low HOMA-B associated with high prevalence of diabetes regardless of HOMA-IR; joint associations with dyslipidemia and hypertension prevalence appeared to be additive and had moderate changing trends; and low HOMA-B was not associated with high prevalence of obesity or central obesity unless combined with high HOMA-IR.
IR was associated with more prevalent cardiometabolic disorders than was β-cell dysfunction, and combinations of IR and β-cell dysfunction showed distinct relations with cardiometabolic risk patterns in Chinese adults.
Diabetes is the leading cause of cardiometabolic morbidity and mortality (1). Globally, 415 million people are living with diabetes, and it is estimated the prevalence will increase to 642 million in 2040 (1). Of note, China already has the world’s largest diabetes epidemic (1). According to our previous investigation, the prevalence of diabetes in China was 11.6% in 2010, with up to 114 million people estimated to be affected by the disease (2).
Insulin resistance (IR) and β-cell dysfunction are two major features in the pathogenesis of type 2 diabetes (3, 4). Both pathological states synergistically exacerbate type 2 diabetes and increase cardiometabolic risk (5–7). It is noteworthy that compared with European people, Chinese people tend to have higher insulin sensitivity but more vulnerable β-cell function in the progression of type 2 diabetes (8, 9), and these features may translate into varying susceptibilities to diabetes-related cardiometabolic disorders such as obesity, dyslipidemia, and hypertension (10). However, national data on the features of IR and β-cell dysfunction and their relationships with cardiometabolic disorders are still lacking in the Chinese population.
In a nationally representative sample of 93,690 Chinese adults with comprehensive measures of glucose and insulin metabolism, we examined the characteristics of IR and β-cell dysfunction, and the independent and joint associations of the two pathological states with established cardiometabolic disorders.
Methods
Study population
China Noncommunicable Disease Surveillance 2010 is a cross-sectional survey including all 162 study sites from the Chinese Center for Disease Control and Prevention National Disease Surveillance Point System in 2010. This system was designed to select a nationally representative sample of the general population, covering the major geographic areas of all 31 provinces, autonomous regions, and municipalities in mainland China (2, 11). At each site, a complex, multistage, probability sampling design was used to select participants who were representative of civilian and noninstitutionalized Chinese adults. Only individuals who had been living in their current residence ≥6 months were eligible. In the first stage, four subdistricts in urban areas or townships in rural areas were selected from each site with probability proportional to size. In the second stage, three neighborhood communities or administrative villages were selected with probability proportional to size. In the third stage, households within each neighborhood community or administrative village were listed, and 50 households were randomly selected. In the final stage, one individual aged ≥18 years was randomly selected from each household by using a Kish selection table (12). All replacements were successfully recruited by the third sampling. A total of 109,023 subjects were selected; among them, 98,658 participated in the survey, with an overall response rate of 90.5%. The final analysis included 93,690 participants aged ≥18 years who had no missing data on fasting plasma glucose or serum insulin and did not use antidiabetic medications.
The study protocol was approved by the Ethical Review Committee of the Chinese Center for Disease Control and Prevention, and other participating institutes approved the study’s protocol. Written informed consent was obtained from all study participants.
Data collection
Data collection was conducted by trained staff in examination centers at local health stations or community clinics in the participants’ residential area. Demographic characteristics, education attainment, family history of diseases, lifestyle factors, and medical history were collected by a questionnaire. Current smoking was defined as having smoked 100 cigarettes in one’s lifetime and currently smoking cigarettes. Current drinking was defined as alcohol intake more than once per month during the past 12 months. The Global Physical Activity Questionnaire was applied to assess physical activity, which included household- and work-related activities, as well as activities during transportation and leisure time (13), and weekly energy expenditure in metabolic equivalent (MET) hours based on the information was calculated. Weight and height were measured according to a standard protocol, and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Waist circumference was measured on standing participants midway between the lower edge of the costal arch and the upper edge of the iliac crest. Using an automated device (model HEM-7071; Omron), blood pressure was measured at the nondominant arm three times consecutively with a 1-minute interval between the measurements, with the participant in a seated position after a 5-minute rest. The average of the three readings was used in analysis.
Blood samples were collected in all participants after an overnight fast of at least 10 hours. Participants without a self-reported history of diabetes underwent a standard 75-g oral glucose tolerance test (OGTT), and the plasma glucose level was measured at 0 and 2 hours after administration during the test. Blood specimens for the glucose test were collected using vacuum blood-collection tubes containing anticoagulant sodium fluoride and were centrifuged on site within 2 hours of collection. Plasma glucose concentration was measured within 24 hours at local laboratories under a standardization and certification program using glucose oxidase or hexokinase methods.
Capillary blood samples were collected using the Hemoglobin Capillary Collection System (Bio-Rad Laboratories). The capillary blood specimens were shipped and stored at 2°C to 8°C until glycated hemoglobin A1c (HbA1c) was measured within 4 weeks after collection by high-performance liquid chromatography using the VARIANT II Hemoglobin Testing System (Bio-Rad Laboratories) at the central laboratory in the Shanghai Institute of Endocrine and Metabolic Diseases, which was certificated by the National Glycohemoglobin Standardization Program.
The capillary HbA1c value was converted to venous values using a validated formula. HbA1c values from capillary whole-blood samples prepared with the Hemoglobin Capillary Collection System showed high agreement with the venous whole-blood samples collected in EDTA tubes (2).
Serum samples were aliquoted and frozen at −80°C within 2 hours of collection and shipped in dry ice to the central laboratory, which was accredited by the College of American Pathologists. Serum insulin was measured by an autoanalyzer (ARCHITECT ci16200 analyzer; Abbott Laboratories). Levels of serum total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides were measured using an autoanalyzer (Abbott Laboratories).
A stringent quality assurance and quality control program was implemented to ensure the validity and reliability of the data. All research staff underwent a training session on the use of standardized protocols and instruments for data collection, all laboratory equipment was calibrated, and blinded duplicate samples were used. All data were double-entered into a database and then compared and corrected for errors.
IR, β-cell dysfunction and cardiometabolic disorders
The homeostasis model assessment of insulin resistance (HOMA-IR) index was calculated according to the following formula (14): fasting insulin (mIU/L) × fasting glucose (mg/dL)/405, and IR was defined as HOMA-IR within the highest quintile. HOMA of β-cell function (HOMA-B) index was calculated as follows: (360 × fasting insulin [mIU/L])/(fasting glucose [mg/dL] − 63), and β-cell dysfunction was defined as HOMA-B within the lowest quintile.
Overweight was defined as BMI between 25.0 and 29.9 kg/m2, and obesity was defined as BMI ≥30 kg/m2 (15). Central obesity was defined as waist circumference ≥90 cm in men and ≥80 cm in women (16). Diabetes was defined as (1) a self-reported previous diagnosis by health care professionals, (2) fasting plasma glucose level ≥126 mg/dL, (3) 2-hour plasma glucose level ≥200 mg/dL, or (4) HbA1c concentration ≥6.5% (17). Dyslipidemia was defined as taking lipid-lowering medications, levels of total cholesterol ≥240 mg/dL, triglycerides ≥200 mg/dL, HDL cholesterol <40 mg/dL, or LDL cholesterol ≥160 mg/dL (18). Hypertension was defined as taking blood pressure–lowering medications, systolic blood pressure ≥140 mm Hg, or diastolic blood pressure ≥90 mm Hg (19).
Statistical analysis
Quintiles of HOMA-IR and HOMA-B were defined by sex-specific cut points due to different HOMA-IR and HOMA-B levels between men and women. HOMA-IR and HOMA-B levels were censored at the 1.0 and 99.0 percentiles to minimize the influence of outliers. Demographic and metabolic characteristics were described in means [95% confidence intervals (CIs)] for continuous variables and percentages (95% CIs) for categorical variables according to quintiles of HOMA-IR and HOMA-B. The number of cardiometabolic disorders was calculated by summing the presence number of obesity or central obesity, diabetes, dyslipidemia, and hypertension as follows: each cardiometabolic disorder was scored 1 if this factor presented, and 0 otherwise. Prevalence (95% CIs) of cardiometabolic disorders, including obesity, central obesity, diabetes, dyslipidemia, and hypertension, as well as overall number of cardiometabolic disorders were examined according to quintiles of HOMA-IR and HOMA-B and subtypes of various criteria. Because it is well known that the log-binomial model is less numerically stable than the logistic model, prevalence ratios (95% CIs) of cardiometabolic disorders were estimated with the use of PROC GENMOD’s Poisson regression capability with the robust variance (20).
All analyses (except for the number of participants) were weighted to represent the overall Chinese adult population aged ≥18 years (2). Each study site was categorized as an underdeveloped, intermediately developed, or developed region according to the tertiles of their gross domestic product per capita in 2009. All reported P values are nominal and two-sided. Statistical analyses were performed with the use of SAS software, version 9.4 (SAS Institute).
Results
Mean HOMA-IR values [women, 1.63 (95% CI, 1.61 to 1.64) vs men, 1.55 (95% CI, 1.54 to 1.57)] and HOMA-B values [women, 81.84 (95% CI, 81.03 to 82.65) vs men, 72.91 (95% CI, 72.07 to 73.74]) were higher in women than in men (both P < 0.0001). Participants with higher HOMA-IR values had higher levels of BMI, waist circumference, fasting and OGTT 2-hour plasma glucose, HbA1c, fasting serum insulin, total cholesterol, LDL cholesterol, triglycerides, systolic and diastolic blood pressures, as well as lower level of HDL cholesterol compared with those with lower HOMA-IR values (Table 1). Participants with lower HOMA-B had higher levels of glycemic traits and blood pressures but lower levels of obesity traits and lipid profile (except for HDL cholesterol) than those with higher HOMA-B (Table 2).
Demographic and Cardiometabolic Characteristics According to HOMA-IR Quintiles
| Variable . | HOMA-IR Quintilesa . | ||||
|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | |
| No. of participants | 18,737 | 18,738 | 18,740 | 18,739 | 18,736 |
| Age, y | 46.8 (46.4–47.1) | 43.8 (43.4–44.1) | 41.7 (41.4–42.1) | 41.1 (40.8–41.4) | 41.6 (41.3–42.0) |
| Men, % | 49.0 (48.0–49.9) | 50.1 (49.1–51.1) | 51.1 (50.2–52.1) | 50.9 (49.9–51.8) | 52.0 (51.0–52.9) |
| Urbanization, % | |||||
| Urban | 23.5 (22.7–24.2) | 27.4 (26.6–28.1) | 30.2 (29.4–31.0) | 34.3 (33.4–35.1) | 36.7 (35.8–37.5) |
| Rural | 76.5 (75.8–77.3) | 72.6 (71.9–73.4) | 69.8 (69.0–70.6) | 65.7 (64.9–66.6) | 63.3 (62.5–64.2) |
| Economic development, % | |||||
| Underdevelopment | 38.4 (37.4–39.4) | 36.1 (35.2–37.1) | 32.9 (32.0–33.9) | 31.2 (30.2–32.1) | 29.6 (28.7–30.5) |
| Intermediately development | 37.1 (36.1–38.0) | 33.7 (32.8–34.6) | 33.4 (32.5–34.3) | 31.6 (30.7–32.5) | 29.2 (28.4–30.1) |
| Developed | 24.5 (23.7–25.3) | 30.2 (29.4–31.1) | 33.7 (32.8–34.6) | 37.2 (36.3–38.1) | 41.2 (40.2–42.1) |
| Education attainment >6 y, % | 48.8 (47.8–49.8) | 58.1 (57.2–59.1) | 64.6 (63.8–65.5) | 68.6 (67.7–69.4) | 69.2 (68.3–70.0) |
| Parental history of diabetes, % | 3.3 (2.9–3.6) | 3.8 (3.5–4.2) | 4.9 (4.5–5.3) | 5.7 (5.3–6.1) | 7.4 (7.0–7.9) |
| Parental history of hypertension, % | 18.7 (17.9–19.4) | 22.1 (21.3–22.8) | 24.4 (23.6–25.2) | 25.7 (24.9–26.5) | 28.8 (28.0–29.7) |
| Current smoker, % | 32.7 (31.8–33.6) | 30.3 (29.4–31.2) | 28.5 (27.6–29.4) | 25.7 (24.8–26.5) | 26.0 (25.1–26.8) |
| Current drinker, % | 31.2 (30.3–32.1) | 29.2 (28.3–30.0) | 30.0 (29.1–30.8) | 29.2 (28.3–30.0) | 29.6 (28.7–30.5) |
| Physical activity, MET-h/wk | 106.0 (103.7–108.2) | 96.3 (94.2–98.4) | 88.4 (86.3–90.5) | 79.4 (77.5–81.4) | 75.2 (73.4–77.1) |
| BMI, kg/m2 | 21.7 (21.7–21.8) | 22.6 (22.5–22.6) | 23.3 (23.2–23.4) | 24.3 (24.2–24.4) | 26.0 (25.9–26.1) |
| Waist circumference, cm | 74.8 (74.6–74.9) | 77.1 (76.9–77.3) | 79.0 (78.9–79.2) | 81.7 (81.5–81.9) | 86.3 (86.1–86.6) |
| Fasting plasma glucose, mg/dL | 89.1 (88.9–89.3) | 93.7 (93.4–93.9) | 96.5 (96.2–96.7) | 99.9 (99.6–100.2) | 112.0 (111.4–112.7) |
| OGTT 2-h plasma glucose, mg/dL | 103.6 (102.9–104.3) | 104.5 (103.9–105.1) | 107.0 (106.4–107.7) | 112.2 (111.5–112.9) | 131.1 (129.9–132.4) |
| HbA1c, % | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) | 5.7 (5.7–5.7) | 6.0 (6.0–6.0) |
| Fasting serum insulin, mIU/L | 2.5 (2.5–2.5) | 3.9 (3.9–3.9) | 5.2 (5.2–5.2) | 7.0 (7.0–7.1) | 12.8 (12.7–12.9) |
| Total cholesterol, mg/dL | 143.5 (142.7–144.3) | 151.4 (150.7–152.1) | 155.4 (154.7–156.2) | 161.4 (160.6–162.1) | 170.6 (169.7–171.4) |
| LDL cholesterol, mg/dL | 77.2 (76.6–77.7) | 84.0 (83.5–84.5) | 87.6 (87.1–88.2) | 92.1 (91.5–92.7) | 97.8 (97.2–98.4) |
| HDL cholesterol, mg/dL | 44.3 (44.1–44.6) | 44.0 (43.8–44.3) | 43.2 (42.9–43.4) | 42.3 (42.1–42.5) | 40.5 (40.3–40.8) |
| Triglycerides, mg/dL | 83.3 (81.9–84.6) | 96.0 (94.4–97.6) | 108.7 (107.0–110.4) | 129.1 (127.2–131.1) | 176.7 (173.4–179.9) |
| Systolic blood pressure, mm Hg | 129.5 (129.1–129.9) | 129.7 (129.3–130.1) | 129.9 (129.5–130.2) | 131.4 (131.0–131.8) | 135.4 (135.1–135.8) |
| Diastolic blood pressure, mm Hg | 78.3 (78.0–78.5) | 79.2 (79.0–79.4) | 79.8 (79.6–80.0) | 81.4 (81.2–81.6) | 84.0 (83.8–84.2) |
| Variable . | HOMA-IR Quintilesa . | ||||
|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | |
| No. of participants | 18,737 | 18,738 | 18,740 | 18,739 | 18,736 |
| Age, y | 46.8 (46.4–47.1) | 43.8 (43.4–44.1) | 41.7 (41.4–42.1) | 41.1 (40.8–41.4) | 41.6 (41.3–42.0) |
| Men, % | 49.0 (48.0–49.9) | 50.1 (49.1–51.1) | 51.1 (50.2–52.1) | 50.9 (49.9–51.8) | 52.0 (51.0–52.9) |
| Urbanization, % | |||||
| Urban | 23.5 (22.7–24.2) | 27.4 (26.6–28.1) | 30.2 (29.4–31.0) | 34.3 (33.4–35.1) | 36.7 (35.8–37.5) |
| Rural | 76.5 (75.8–77.3) | 72.6 (71.9–73.4) | 69.8 (69.0–70.6) | 65.7 (64.9–66.6) | 63.3 (62.5–64.2) |
| Economic development, % | |||||
| Underdevelopment | 38.4 (37.4–39.4) | 36.1 (35.2–37.1) | 32.9 (32.0–33.9) | 31.2 (30.2–32.1) | 29.6 (28.7–30.5) |
| Intermediately development | 37.1 (36.1–38.0) | 33.7 (32.8–34.6) | 33.4 (32.5–34.3) | 31.6 (30.7–32.5) | 29.2 (28.4–30.1) |
| Developed | 24.5 (23.7–25.3) | 30.2 (29.4–31.1) | 33.7 (32.8–34.6) | 37.2 (36.3–38.1) | 41.2 (40.2–42.1) |
| Education attainment >6 y, % | 48.8 (47.8–49.8) | 58.1 (57.2–59.1) | 64.6 (63.8–65.5) | 68.6 (67.7–69.4) | 69.2 (68.3–70.0) |
| Parental history of diabetes, % | 3.3 (2.9–3.6) | 3.8 (3.5–4.2) | 4.9 (4.5–5.3) | 5.7 (5.3–6.1) | 7.4 (7.0–7.9) |
| Parental history of hypertension, % | 18.7 (17.9–19.4) | 22.1 (21.3–22.8) | 24.4 (23.6–25.2) | 25.7 (24.9–26.5) | 28.8 (28.0–29.7) |
| Current smoker, % | 32.7 (31.8–33.6) | 30.3 (29.4–31.2) | 28.5 (27.6–29.4) | 25.7 (24.8–26.5) | 26.0 (25.1–26.8) |
| Current drinker, % | 31.2 (30.3–32.1) | 29.2 (28.3–30.0) | 30.0 (29.1–30.8) | 29.2 (28.3–30.0) | 29.6 (28.7–30.5) |
| Physical activity, MET-h/wk | 106.0 (103.7–108.2) | 96.3 (94.2–98.4) | 88.4 (86.3–90.5) | 79.4 (77.5–81.4) | 75.2 (73.4–77.1) |
| BMI, kg/m2 | 21.7 (21.7–21.8) | 22.6 (22.5–22.6) | 23.3 (23.2–23.4) | 24.3 (24.2–24.4) | 26.0 (25.9–26.1) |
| Waist circumference, cm | 74.8 (74.6–74.9) | 77.1 (76.9–77.3) | 79.0 (78.9–79.2) | 81.7 (81.5–81.9) | 86.3 (86.1–86.6) |
| Fasting plasma glucose, mg/dL | 89.1 (88.9–89.3) | 93.7 (93.4–93.9) | 96.5 (96.2–96.7) | 99.9 (99.6–100.2) | 112.0 (111.4–112.7) |
| OGTT 2-h plasma glucose, mg/dL | 103.6 (102.9–104.3) | 104.5 (103.9–105.1) | 107.0 (106.4–107.7) | 112.2 (111.5–112.9) | 131.1 (129.9–132.4) |
| HbA1c, % | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) | 5.7 (5.7–5.7) | 6.0 (6.0–6.0) |
| Fasting serum insulin, mIU/L | 2.5 (2.5–2.5) | 3.9 (3.9–3.9) | 5.2 (5.2–5.2) | 7.0 (7.0–7.1) | 12.8 (12.7–12.9) |
| Total cholesterol, mg/dL | 143.5 (142.7–144.3) | 151.4 (150.7–152.1) | 155.4 (154.7–156.2) | 161.4 (160.6–162.1) | 170.6 (169.7–171.4) |
| LDL cholesterol, mg/dL | 77.2 (76.6–77.7) | 84.0 (83.5–84.5) | 87.6 (87.1–88.2) | 92.1 (91.5–92.7) | 97.8 (97.2–98.4) |
| HDL cholesterol, mg/dL | 44.3 (44.1–44.6) | 44.0 (43.8–44.3) | 43.2 (42.9–43.4) | 42.3 (42.1–42.5) | 40.5 (40.3–40.8) |
| Triglycerides, mg/dL | 83.3 (81.9–84.6) | 96.0 (94.4–97.6) | 108.7 (107.0–110.4) | 129.1 (127.2–131.1) | 176.7 (173.4–179.9) |
| Systolic blood pressure, mm Hg | 129.5 (129.1–129.9) | 129.7 (129.3–130.1) | 129.9 (129.5–130.2) | 131.4 (131.0–131.8) | 135.4 (135.1–135.8) |
| Diastolic blood pressure, mm Hg | 78.3 (78.0–78.5) | 79.2 (79.0–79.4) | 79.8 (79.6–80.0) | 81.4 (81.2–81.6) | 84.0 (83.8–84.2) |
Data are weighted means (95% CI) for continuous variables and weighted percentages (95% CI) for categorical variables.
Ranges of HOMA-IR values in men were 0.31 to 0.63 for quintile 1, 0.64 to 0.95 for quintile 2, 0.96 to 1.34 for quintile 3, 1.35 to 2.04 for quintile 4, and 2.05 to 7.15 for quintile 5; in women, the ranges were 0.31 to 0.81 for quintile 1, 0.82 to 1.12 for quintile 2, 1.13 to 1.49 for quintile 3, 1.50 to 2.12 for quintile 4, and 2.13 to 7.15 for quintile 5.
Demographic and Cardiometabolic Characteristics According to HOMA-IR Quintiles
| Variable . | HOMA-IR Quintilesa . | ||||
|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | |
| No. of participants | 18,737 | 18,738 | 18,740 | 18,739 | 18,736 |
| Age, y | 46.8 (46.4–47.1) | 43.8 (43.4–44.1) | 41.7 (41.4–42.1) | 41.1 (40.8–41.4) | 41.6 (41.3–42.0) |
| Men, % | 49.0 (48.0–49.9) | 50.1 (49.1–51.1) | 51.1 (50.2–52.1) | 50.9 (49.9–51.8) | 52.0 (51.0–52.9) |
| Urbanization, % | |||||
| Urban | 23.5 (22.7–24.2) | 27.4 (26.6–28.1) | 30.2 (29.4–31.0) | 34.3 (33.4–35.1) | 36.7 (35.8–37.5) |
| Rural | 76.5 (75.8–77.3) | 72.6 (71.9–73.4) | 69.8 (69.0–70.6) | 65.7 (64.9–66.6) | 63.3 (62.5–64.2) |
| Economic development, % | |||||
| Underdevelopment | 38.4 (37.4–39.4) | 36.1 (35.2–37.1) | 32.9 (32.0–33.9) | 31.2 (30.2–32.1) | 29.6 (28.7–30.5) |
| Intermediately development | 37.1 (36.1–38.0) | 33.7 (32.8–34.6) | 33.4 (32.5–34.3) | 31.6 (30.7–32.5) | 29.2 (28.4–30.1) |
| Developed | 24.5 (23.7–25.3) | 30.2 (29.4–31.1) | 33.7 (32.8–34.6) | 37.2 (36.3–38.1) | 41.2 (40.2–42.1) |
| Education attainment >6 y, % | 48.8 (47.8–49.8) | 58.1 (57.2–59.1) | 64.6 (63.8–65.5) | 68.6 (67.7–69.4) | 69.2 (68.3–70.0) |
| Parental history of diabetes, % | 3.3 (2.9–3.6) | 3.8 (3.5–4.2) | 4.9 (4.5–5.3) | 5.7 (5.3–6.1) | 7.4 (7.0–7.9) |
| Parental history of hypertension, % | 18.7 (17.9–19.4) | 22.1 (21.3–22.8) | 24.4 (23.6–25.2) | 25.7 (24.9–26.5) | 28.8 (28.0–29.7) |
| Current smoker, % | 32.7 (31.8–33.6) | 30.3 (29.4–31.2) | 28.5 (27.6–29.4) | 25.7 (24.8–26.5) | 26.0 (25.1–26.8) |
| Current drinker, % | 31.2 (30.3–32.1) | 29.2 (28.3–30.0) | 30.0 (29.1–30.8) | 29.2 (28.3–30.0) | 29.6 (28.7–30.5) |
| Physical activity, MET-h/wk | 106.0 (103.7–108.2) | 96.3 (94.2–98.4) | 88.4 (86.3–90.5) | 79.4 (77.5–81.4) | 75.2 (73.4–77.1) |
| BMI, kg/m2 | 21.7 (21.7–21.8) | 22.6 (22.5–22.6) | 23.3 (23.2–23.4) | 24.3 (24.2–24.4) | 26.0 (25.9–26.1) |
| Waist circumference, cm | 74.8 (74.6–74.9) | 77.1 (76.9–77.3) | 79.0 (78.9–79.2) | 81.7 (81.5–81.9) | 86.3 (86.1–86.6) |
| Fasting plasma glucose, mg/dL | 89.1 (88.9–89.3) | 93.7 (93.4–93.9) | 96.5 (96.2–96.7) | 99.9 (99.6–100.2) | 112.0 (111.4–112.7) |
| OGTT 2-h plasma glucose, mg/dL | 103.6 (102.9–104.3) | 104.5 (103.9–105.1) | 107.0 (106.4–107.7) | 112.2 (111.5–112.9) | 131.1 (129.9–132.4) |
| HbA1c, % | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) | 5.7 (5.7–5.7) | 6.0 (6.0–6.0) |
| Fasting serum insulin, mIU/L | 2.5 (2.5–2.5) | 3.9 (3.9–3.9) | 5.2 (5.2–5.2) | 7.0 (7.0–7.1) | 12.8 (12.7–12.9) |
| Total cholesterol, mg/dL | 143.5 (142.7–144.3) | 151.4 (150.7–152.1) | 155.4 (154.7–156.2) | 161.4 (160.6–162.1) | 170.6 (169.7–171.4) |
| LDL cholesterol, mg/dL | 77.2 (76.6–77.7) | 84.0 (83.5–84.5) | 87.6 (87.1–88.2) | 92.1 (91.5–92.7) | 97.8 (97.2–98.4) |
| HDL cholesterol, mg/dL | 44.3 (44.1–44.6) | 44.0 (43.8–44.3) | 43.2 (42.9–43.4) | 42.3 (42.1–42.5) | 40.5 (40.3–40.8) |
| Triglycerides, mg/dL | 83.3 (81.9–84.6) | 96.0 (94.4–97.6) | 108.7 (107.0–110.4) | 129.1 (127.2–131.1) | 176.7 (173.4–179.9) |
| Systolic blood pressure, mm Hg | 129.5 (129.1–129.9) | 129.7 (129.3–130.1) | 129.9 (129.5–130.2) | 131.4 (131.0–131.8) | 135.4 (135.1–135.8) |
| Diastolic blood pressure, mm Hg | 78.3 (78.0–78.5) | 79.2 (79.0–79.4) | 79.8 (79.6–80.0) | 81.4 (81.2–81.6) | 84.0 (83.8–84.2) |
| Variable . | HOMA-IR Quintilesa . | ||||
|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | |
| No. of participants | 18,737 | 18,738 | 18,740 | 18,739 | 18,736 |
| Age, y | 46.8 (46.4–47.1) | 43.8 (43.4–44.1) | 41.7 (41.4–42.1) | 41.1 (40.8–41.4) | 41.6 (41.3–42.0) |
| Men, % | 49.0 (48.0–49.9) | 50.1 (49.1–51.1) | 51.1 (50.2–52.1) | 50.9 (49.9–51.8) | 52.0 (51.0–52.9) |
| Urbanization, % | |||||
| Urban | 23.5 (22.7–24.2) | 27.4 (26.6–28.1) | 30.2 (29.4–31.0) | 34.3 (33.4–35.1) | 36.7 (35.8–37.5) |
| Rural | 76.5 (75.8–77.3) | 72.6 (71.9–73.4) | 69.8 (69.0–70.6) | 65.7 (64.9–66.6) | 63.3 (62.5–64.2) |
| Economic development, % | |||||
| Underdevelopment | 38.4 (37.4–39.4) | 36.1 (35.2–37.1) | 32.9 (32.0–33.9) | 31.2 (30.2–32.1) | 29.6 (28.7–30.5) |
| Intermediately development | 37.1 (36.1–38.0) | 33.7 (32.8–34.6) | 33.4 (32.5–34.3) | 31.6 (30.7–32.5) | 29.2 (28.4–30.1) |
| Developed | 24.5 (23.7–25.3) | 30.2 (29.4–31.1) | 33.7 (32.8–34.6) | 37.2 (36.3–38.1) | 41.2 (40.2–42.1) |
| Education attainment >6 y, % | 48.8 (47.8–49.8) | 58.1 (57.2–59.1) | 64.6 (63.8–65.5) | 68.6 (67.7–69.4) | 69.2 (68.3–70.0) |
| Parental history of diabetes, % | 3.3 (2.9–3.6) | 3.8 (3.5–4.2) | 4.9 (4.5–5.3) | 5.7 (5.3–6.1) | 7.4 (7.0–7.9) |
| Parental history of hypertension, % | 18.7 (17.9–19.4) | 22.1 (21.3–22.8) | 24.4 (23.6–25.2) | 25.7 (24.9–26.5) | 28.8 (28.0–29.7) |
| Current smoker, % | 32.7 (31.8–33.6) | 30.3 (29.4–31.2) | 28.5 (27.6–29.4) | 25.7 (24.8–26.5) | 26.0 (25.1–26.8) |
| Current drinker, % | 31.2 (30.3–32.1) | 29.2 (28.3–30.0) | 30.0 (29.1–30.8) | 29.2 (28.3–30.0) | 29.6 (28.7–30.5) |
| Physical activity, MET-h/wk | 106.0 (103.7–108.2) | 96.3 (94.2–98.4) | 88.4 (86.3–90.5) | 79.4 (77.5–81.4) | 75.2 (73.4–77.1) |
| BMI, kg/m2 | 21.7 (21.7–21.8) | 22.6 (22.5–22.6) | 23.3 (23.2–23.4) | 24.3 (24.2–24.4) | 26.0 (25.9–26.1) |
| Waist circumference, cm | 74.8 (74.6–74.9) | 77.1 (76.9–77.3) | 79.0 (78.9–79.2) | 81.7 (81.5–81.9) | 86.3 (86.1–86.6) |
| Fasting plasma glucose, mg/dL | 89.1 (88.9–89.3) | 93.7 (93.4–93.9) | 96.5 (96.2–96.7) | 99.9 (99.6–100.2) | 112.0 (111.4–112.7) |
| OGTT 2-h plasma glucose, mg/dL | 103.6 (102.9–104.3) | 104.5 (103.9–105.1) | 107.0 (106.4–107.7) | 112.2 (111.5–112.9) | 131.1 (129.9–132.4) |
| HbA1c, % | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) | 5.7 (5.7–5.7) | 6.0 (6.0–6.0) |
| Fasting serum insulin, mIU/L | 2.5 (2.5–2.5) | 3.9 (3.9–3.9) | 5.2 (5.2–5.2) | 7.0 (7.0–7.1) | 12.8 (12.7–12.9) |
| Total cholesterol, mg/dL | 143.5 (142.7–144.3) | 151.4 (150.7–152.1) | 155.4 (154.7–156.2) | 161.4 (160.6–162.1) | 170.6 (169.7–171.4) |
| LDL cholesterol, mg/dL | 77.2 (76.6–77.7) | 84.0 (83.5–84.5) | 87.6 (87.1–88.2) | 92.1 (91.5–92.7) | 97.8 (97.2–98.4) |
| HDL cholesterol, mg/dL | 44.3 (44.1–44.6) | 44.0 (43.8–44.3) | 43.2 (42.9–43.4) | 42.3 (42.1–42.5) | 40.5 (40.3–40.8) |
| Triglycerides, mg/dL | 83.3 (81.9–84.6) | 96.0 (94.4–97.6) | 108.7 (107.0–110.4) | 129.1 (127.2–131.1) | 176.7 (173.4–179.9) |
| Systolic blood pressure, mm Hg | 129.5 (129.1–129.9) | 129.7 (129.3–130.1) | 129.9 (129.5–130.2) | 131.4 (131.0–131.8) | 135.4 (135.1–135.8) |
| Diastolic blood pressure, mm Hg | 78.3 (78.0–78.5) | 79.2 (79.0–79.4) | 79.8 (79.6–80.0) | 81.4 (81.2–81.6) | 84.0 (83.8–84.2) |
Data are weighted means (95% CI) for continuous variables and weighted percentages (95% CI) for categorical variables.
Ranges of HOMA-IR values in men were 0.31 to 0.63 for quintile 1, 0.64 to 0.95 for quintile 2, 0.96 to 1.34 for quintile 3, 1.35 to 2.04 for quintile 4, and 2.05 to 7.15 for quintile 5; in women, the ranges were 0.31 to 0.81 for quintile 1, 0.82 to 1.12 for quintile 2, 1.13 to 1.49 for quintile 3, 1.50 to 2.12 for quintile 4, and 2.13 to 7.15 for quintile 5.
Demographic and Cardiometabolic Characteristics According to HOMA-B Quintiles
| Variable . | HOMA-B Quintilesa . | ||||
|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | |
| No. of participants | 18,737 | 18,739 | 18,739 | 18,737 | 18,738 |
| Age, y | 49.8 (49.4–50.1) | 45.4 (45.1–45.7) | 42.7 (42.4–43.0) | 40.1 (39.8–40.4) | 37.3 (37.0–37.6) |
| Men, % | 49.4 (48.4–50.3) | 49.9 (48.9–50.8) | 51.0 (50.1–52.0) | 51.1 (50.2–52.1) | 51.8 (50.8–52.8) |
| Urbanization, % | |||||
| Urban | 25.4 (24.7–26.2) | 29.1 (28.3–29.9) | 32.2 (31.3–33.0) | 33.7 (32.8–34.5) | 32.5 (31.7–33.3) |
| Rural | 74.6 (73.8–75.3) | 70.9 (70.1–71.7) | 67.8 (67.0–68.7) | 66.3 (65.5–67.2) | 67.5 (66.7–68.3) |
| Economic development, % | |||||
| Underdevelopment | 35.5 (34.6–36.4) | 34.6 (33.6–35.5) | 33.2 (32.2–34.1) | 30.6 (29.6–31.5) | 33.6 (32.7–34.6) |
| Intermediately development | 35.1 (34.2–36.0) | 33.2 (32.3–34.0) | 32.1 (31.2–33.0) | 32.6 (31.7–33.5) | 31.4 (30.5–32.3) |
| Developed | 29.4 (28.5–30.2) | 32.3 (31.4–33.1) | 34.7 (33.8–35.6) | 36.8 (35.9–37.7) | 34.9 (34.0–35.8) |
| Education attainment >6 y, % | 46.2 (45.2–47.1) | 57.5 (56.6–58.4) | 63.9 (63.0–64.8) | 69.7 (68.9–70.6) | 72.4 (71.6–73.2) |
| Parental history of diabetes, % | 3.9 (3.6–4.3) | 4.4 (4.0–4.8) | 5.3 (4.9–5.7) | 5.6 (5.2–6.0) | 6.1 (5.7–6.5) |
| Parental history of hypertension, % | 19.1 (18.4–19.8) | 22.8 (22.1–23.7) | 24.6 (23.9–25.4) | 26.5 (25.7–27.3) | 27.0 (26.1–27.8) |
| Current smoker, % | 31.8 (30.9–32.6) | 28.5 (27.7–29.4) | 28.2 (27.3–29.1) | 26.7 (25.8–27.6) | 27.4 (26.6–28.3) |
| Current drinker, % | 31.6 (30.8–32.5) | 29.7 (28.8–30.6) | 30.0 (29.1–30.9) | 28.5 (27.6–29.4) | 29.2 (28.3–30.1) |
| Physical activity, MET-h/wk | 104.6 (102.3–106.8) | 95.5 (93.5–97.6) | 87.5 (85.4–89.5) | 78.5 (76.6–80.4) | 78.0 (76.1–79.9) |
| BMI, kg/m2 | 22.4 (22.4–22.5) | 23.1 (23.0–23.1) | 23.6 (23.5–23.7) | 24.2 (24.1–24.2) | 24.8 (24.8–24.9) |
| Waist circumference, cm | 77.1 (77.0–77.3) | 78.5 (78.3–78.7) | 79.8 (79.6–80.0) | 81.3 (81.1–81.5) | 82.9 (82.6–83.1) |
| Fasting plasma glucose, mg/dL | 111.3 (110.6–112.0) | 101.2 (100.9–101.5) | 98.3 (98.0–98.5) | 95.4 (95.1–95.6) | 89.0 (88.7–89.3) |
| OGTT 2-h plasma glucose, mg/dL | 130.6 (129.2–132.0) | 113.2 (112.4–113.9) | 109.4 (108.8–110.1) | 106.6 (106.0–107.2) | 103.2 (102.6–103.8) |
| HbA1c, % | 6.0 (6.0–6.0) | 5.7 (5.7–5.7) | 5.7 (5.7–5.7) | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) |
| Fasting serum insulin, mIU/L | 3.2 (3.2–3.3) | 4.4 (4.3–4.4) | 5.6 (5.6–5.6) | 7.3 (7.2–7.3) | 11.2 (11.1–11.4) |
| Total cholesterol, mg/dL | 153.2 (152.4–154.0) | 155.2 (154.4–155.9) | 157.5 (156.7–158.3) | 159.0 (158.1–159.8) | 159.7 (158.9–160.5) |
| LDL cholesterol, mg/dL | 84.3 (83.7–84.9) | 86.8 (86.2–87.3) | 88.8 (88.2–89.3) | 90.1 (89.5–90.7) | 90.5 (89.9–91.1) |
| HDL cholesterol, mg/dL | 44.2 (43.9–44.4) | 43.5 (43.3–43.8) | 42.7 (42.5–42.9) | 42.2 (42.0–42.4) | 41.6 (41.4–41.8) |
| Triglycerides, mg/dL | 102.4 (100.1–104.6) | 105.7 (103.9–107.5) | 117.6 (115.6–119.6) | 129.2 (126.8–131.7) | 144.3 (141.8–146.7) |
| Systolic blood pressure, mm Hg | 135.3 (134.9–135.7) | 131.9 (131.5–132.3) | 130.7 (130.3–131.1) | 129.8 (129.5–130.2) | 129.2 (128.9–129.6) |
| Diastolic blood pressure, mm Hg | 81.0 (80.7–81.2) | 80.3 (80.1–80.5) | 80.6 (80.4–80.8) | 80.7 (80.5–80.9) | 80.7 (80.5–80.9) |
| Variable . | HOMA-B Quintilesa . | ||||
|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | |
| No. of participants | 18,737 | 18,739 | 18,739 | 18,737 | 18,738 |
| Age, y | 49.8 (49.4–50.1) | 45.4 (45.1–45.7) | 42.7 (42.4–43.0) | 40.1 (39.8–40.4) | 37.3 (37.0–37.6) |
| Men, % | 49.4 (48.4–50.3) | 49.9 (48.9–50.8) | 51.0 (50.1–52.0) | 51.1 (50.2–52.1) | 51.8 (50.8–52.8) |
| Urbanization, % | |||||
| Urban | 25.4 (24.7–26.2) | 29.1 (28.3–29.9) | 32.2 (31.3–33.0) | 33.7 (32.8–34.5) | 32.5 (31.7–33.3) |
| Rural | 74.6 (73.8–75.3) | 70.9 (70.1–71.7) | 67.8 (67.0–68.7) | 66.3 (65.5–67.2) | 67.5 (66.7–68.3) |
| Economic development, % | |||||
| Underdevelopment | 35.5 (34.6–36.4) | 34.6 (33.6–35.5) | 33.2 (32.2–34.1) | 30.6 (29.6–31.5) | 33.6 (32.7–34.6) |
| Intermediately development | 35.1 (34.2–36.0) | 33.2 (32.3–34.0) | 32.1 (31.2–33.0) | 32.6 (31.7–33.5) | 31.4 (30.5–32.3) |
| Developed | 29.4 (28.5–30.2) | 32.3 (31.4–33.1) | 34.7 (33.8–35.6) | 36.8 (35.9–37.7) | 34.9 (34.0–35.8) |
| Education attainment >6 y, % | 46.2 (45.2–47.1) | 57.5 (56.6–58.4) | 63.9 (63.0–64.8) | 69.7 (68.9–70.6) | 72.4 (71.6–73.2) |
| Parental history of diabetes, % | 3.9 (3.6–4.3) | 4.4 (4.0–4.8) | 5.3 (4.9–5.7) | 5.6 (5.2–6.0) | 6.1 (5.7–6.5) |
| Parental history of hypertension, % | 19.1 (18.4–19.8) | 22.8 (22.1–23.7) | 24.6 (23.9–25.4) | 26.5 (25.7–27.3) | 27.0 (26.1–27.8) |
| Current smoker, % | 31.8 (30.9–32.6) | 28.5 (27.7–29.4) | 28.2 (27.3–29.1) | 26.7 (25.8–27.6) | 27.4 (26.6–28.3) |
| Current drinker, % | 31.6 (30.8–32.5) | 29.7 (28.8–30.6) | 30.0 (29.1–30.9) | 28.5 (27.6–29.4) | 29.2 (28.3–30.1) |
| Physical activity, MET-h/wk | 104.6 (102.3–106.8) | 95.5 (93.5–97.6) | 87.5 (85.4–89.5) | 78.5 (76.6–80.4) | 78.0 (76.1–79.9) |
| BMI, kg/m2 | 22.4 (22.4–22.5) | 23.1 (23.0–23.1) | 23.6 (23.5–23.7) | 24.2 (24.1–24.2) | 24.8 (24.8–24.9) |
| Waist circumference, cm | 77.1 (77.0–77.3) | 78.5 (78.3–78.7) | 79.8 (79.6–80.0) | 81.3 (81.1–81.5) | 82.9 (82.6–83.1) |
| Fasting plasma glucose, mg/dL | 111.3 (110.6–112.0) | 101.2 (100.9–101.5) | 98.3 (98.0–98.5) | 95.4 (95.1–95.6) | 89.0 (88.7–89.3) |
| OGTT 2-h plasma glucose, mg/dL | 130.6 (129.2–132.0) | 113.2 (112.4–113.9) | 109.4 (108.8–110.1) | 106.6 (106.0–107.2) | 103.2 (102.6–103.8) |
| HbA1c, % | 6.0 (6.0–6.0) | 5.7 (5.7–5.7) | 5.7 (5.7–5.7) | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) |
| Fasting serum insulin, mIU/L | 3.2 (3.2–3.3) | 4.4 (4.3–4.4) | 5.6 (5.6–5.6) | 7.3 (7.2–7.3) | 11.2 (11.1–11.4) |
| Total cholesterol, mg/dL | 153.2 (152.4–154.0) | 155.2 (154.4–155.9) | 157.5 (156.7–158.3) | 159.0 (158.1–159.8) | 159.7 (158.9–160.5) |
| LDL cholesterol, mg/dL | 84.3 (83.7–84.9) | 86.8 (86.2–87.3) | 88.8 (88.2–89.3) | 90.1 (89.5–90.7) | 90.5 (89.9–91.1) |
| HDL cholesterol, mg/dL | 44.2 (43.9–44.4) | 43.5 (43.3–43.8) | 42.7 (42.5–42.9) | 42.2 (42.0–42.4) | 41.6 (41.4–41.8) |
| Triglycerides, mg/dL | 102.4 (100.1–104.6) | 105.7 (103.9–107.5) | 117.6 (115.6–119.6) | 129.2 (126.8–131.7) | 144.3 (141.8–146.7) |
| Systolic blood pressure, mm Hg | 135.3 (134.9–135.7) | 131.9 (131.5–132.3) | 130.7 (130.3–131.1) | 129.8 (129.5–130.2) | 129.2 (128.9–129.6) |
| Diastolic blood pressure, mm Hg | 81.0 (80.7–81.2) | 80.3 (80.1–80.5) | 80.6 (80.4–80.8) | 80.7 (80.5–80.9) | 80.7 (80.5–80.9) |
Data are weighted means (95% CIs) for continuous variables and weighted percentages (95% CI) for categorical variables.
Ranges of HOMA-B in men were 5.57 to 29.03 for quintile 1, 29.04 to 43.64 for quintile 2, 43.65 to 61.82 for quintile 3, 61.83 to 94.81 for quintile 4, and 94.82 to 428.57 for quintile 5; in women, ranges were 5.57 to 38.52 for quintile 1, 38.53 to 54.44 for quintile 2, 54.45 to 73.20 for quintile 3, 73.21 to 105.63 for quintile 4, and 105.64 to 428.57 for quintile 5.
Demographic and Cardiometabolic Characteristics According to HOMA-B Quintiles
| Variable . | HOMA-B Quintilesa . | ||||
|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | |
| No. of participants | 18,737 | 18,739 | 18,739 | 18,737 | 18,738 |
| Age, y | 49.8 (49.4–50.1) | 45.4 (45.1–45.7) | 42.7 (42.4–43.0) | 40.1 (39.8–40.4) | 37.3 (37.0–37.6) |
| Men, % | 49.4 (48.4–50.3) | 49.9 (48.9–50.8) | 51.0 (50.1–52.0) | 51.1 (50.2–52.1) | 51.8 (50.8–52.8) |
| Urbanization, % | |||||
| Urban | 25.4 (24.7–26.2) | 29.1 (28.3–29.9) | 32.2 (31.3–33.0) | 33.7 (32.8–34.5) | 32.5 (31.7–33.3) |
| Rural | 74.6 (73.8–75.3) | 70.9 (70.1–71.7) | 67.8 (67.0–68.7) | 66.3 (65.5–67.2) | 67.5 (66.7–68.3) |
| Economic development, % | |||||
| Underdevelopment | 35.5 (34.6–36.4) | 34.6 (33.6–35.5) | 33.2 (32.2–34.1) | 30.6 (29.6–31.5) | 33.6 (32.7–34.6) |
| Intermediately development | 35.1 (34.2–36.0) | 33.2 (32.3–34.0) | 32.1 (31.2–33.0) | 32.6 (31.7–33.5) | 31.4 (30.5–32.3) |
| Developed | 29.4 (28.5–30.2) | 32.3 (31.4–33.1) | 34.7 (33.8–35.6) | 36.8 (35.9–37.7) | 34.9 (34.0–35.8) |
| Education attainment >6 y, % | 46.2 (45.2–47.1) | 57.5 (56.6–58.4) | 63.9 (63.0–64.8) | 69.7 (68.9–70.6) | 72.4 (71.6–73.2) |
| Parental history of diabetes, % | 3.9 (3.6–4.3) | 4.4 (4.0–4.8) | 5.3 (4.9–5.7) | 5.6 (5.2–6.0) | 6.1 (5.7–6.5) |
| Parental history of hypertension, % | 19.1 (18.4–19.8) | 22.8 (22.1–23.7) | 24.6 (23.9–25.4) | 26.5 (25.7–27.3) | 27.0 (26.1–27.8) |
| Current smoker, % | 31.8 (30.9–32.6) | 28.5 (27.7–29.4) | 28.2 (27.3–29.1) | 26.7 (25.8–27.6) | 27.4 (26.6–28.3) |
| Current drinker, % | 31.6 (30.8–32.5) | 29.7 (28.8–30.6) | 30.0 (29.1–30.9) | 28.5 (27.6–29.4) | 29.2 (28.3–30.1) |
| Physical activity, MET-h/wk | 104.6 (102.3–106.8) | 95.5 (93.5–97.6) | 87.5 (85.4–89.5) | 78.5 (76.6–80.4) | 78.0 (76.1–79.9) |
| BMI, kg/m2 | 22.4 (22.4–22.5) | 23.1 (23.0–23.1) | 23.6 (23.5–23.7) | 24.2 (24.1–24.2) | 24.8 (24.8–24.9) |
| Waist circumference, cm | 77.1 (77.0–77.3) | 78.5 (78.3–78.7) | 79.8 (79.6–80.0) | 81.3 (81.1–81.5) | 82.9 (82.6–83.1) |
| Fasting plasma glucose, mg/dL | 111.3 (110.6–112.0) | 101.2 (100.9–101.5) | 98.3 (98.0–98.5) | 95.4 (95.1–95.6) | 89.0 (88.7–89.3) |
| OGTT 2-h plasma glucose, mg/dL | 130.6 (129.2–132.0) | 113.2 (112.4–113.9) | 109.4 (108.8–110.1) | 106.6 (106.0–107.2) | 103.2 (102.6–103.8) |
| HbA1c, % | 6.0 (6.0–6.0) | 5.7 (5.7–5.7) | 5.7 (5.7–5.7) | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) |
| Fasting serum insulin, mIU/L | 3.2 (3.2–3.3) | 4.4 (4.3–4.4) | 5.6 (5.6–5.6) | 7.3 (7.2–7.3) | 11.2 (11.1–11.4) |
| Total cholesterol, mg/dL | 153.2 (152.4–154.0) | 155.2 (154.4–155.9) | 157.5 (156.7–158.3) | 159.0 (158.1–159.8) | 159.7 (158.9–160.5) |
| LDL cholesterol, mg/dL | 84.3 (83.7–84.9) | 86.8 (86.2–87.3) | 88.8 (88.2–89.3) | 90.1 (89.5–90.7) | 90.5 (89.9–91.1) |
| HDL cholesterol, mg/dL | 44.2 (43.9–44.4) | 43.5 (43.3–43.8) | 42.7 (42.5–42.9) | 42.2 (42.0–42.4) | 41.6 (41.4–41.8) |
| Triglycerides, mg/dL | 102.4 (100.1–104.6) | 105.7 (103.9–107.5) | 117.6 (115.6–119.6) | 129.2 (126.8–131.7) | 144.3 (141.8–146.7) |
| Systolic blood pressure, mm Hg | 135.3 (134.9–135.7) | 131.9 (131.5–132.3) | 130.7 (130.3–131.1) | 129.8 (129.5–130.2) | 129.2 (128.9–129.6) |
| Diastolic blood pressure, mm Hg | 81.0 (80.7–81.2) | 80.3 (80.1–80.5) | 80.6 (80.4–80.8) | 80.7 (80.5–80.9) | 80.7 (80.5–80.9) |
| Variable . | HOMA-B Quintilesa . | ||||
|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | |
| No. of participants | 18,737 | 18,739 | 18,739 | 18,737 | 18,738 |
| Age, y | 49.8 (49.4–50.1) | 45.4 (45.1–45.7) | 42.7 (42.4–43.0) | 40.1 (39.8–40.4) | 37.3 (37.0–37.6) |
| Men, % | 49.4 (48.4–50.3) | 49.9 (48.9–50.8) | 51.0 (50.1–52.0) | 51.1 (50.2–52.1) | 51.8 (50.8–52.8) |
| Urbanization, % | |||||
| Urban | 25.4 (24.7–26.2) | 29.1 (28.3–29.9) | 32.2 (31.3–33.0) | 33.7 (32.8–34.5) | 32.5 (31.7–33.3) |
| Rural | 74.6 (73.8–75.3) | 70.9 (70.1–71.7) | 67.8 (67.0–68.7) | 66.3 (65.5–67.2) | 67.5 (66.7–68.3) |
| Economic development, % | |||||
| Underdevelopment | 35.5 (34.6–36.4) | 34.6 (33.6–35.5) | 33.2 (32.2–34.1) | 30.6 (29.6–31.5) | 33.6 (32.7–34.6) |
| Intermediately development | 35.1 (34.2–36.0) | 33.2 (32.3–34.0) | 32.1 (31.2–33.0) | 32.6 (31.7–33.5) | 31.4 (30.5–32.3) |
| Developed | 29.4 (28.5–30.2) | 32.3 (31.4–33.1) | 34.7 (33.8–35.6) | 36.8 (35.9–37.7) | 34.9 (34.0–35.8) |
| Education attainment >6 y, % | 46.2 (45.2–47.1) | 57.5 (56.6–58.4) | 63.9 (63.0–64.8) | 69.7 (68.9–70.6) | 72.4 (71.6–73.2) |
| Parental history of diabetes, % | 3.9 (3.6–4.3) | 4.4 (4.0–4.8) | 5.3 (4.9–5.7) | 5.6 (5.2–6.0) | 6.1 (5.7–6.5) |
| Parental history of hypertension, % | 19.1 (18.4–19.8) | 22.8 (22.1–23.7) | 24.6 (23.9–25.4) | 26.5 (25.7–27.3) | 27.0 (26.1–27.8) |
| Current smoker, % | 31.8 (30.9–32.6) | 28.5 (27.7–29.4) | 28.2 (27.3–29.1) | 26.7 (25.8–27.6) | 27.4 (26.6–28.3) |
| Current drinker, % | 31.6 (30.8–32.5) | 29.7 (28.8–30.6) | 30.0 (29.1–30.9) | 28.5 (27.6–29.4) | 29.2 (28.3–30.1) |
| Physical activity, MET-h/wk | 104.6 (102.3–106.8) | 95.5 (93.5–97.6) | 87.5 (85.4–89.5) | 78.5 (76.6–80.4) | 78.0 (76.1–79.9) |
| BMI, kg/m2 | 22.4 (22.4–22.5) | 23.1 (23.0–23.1) | 23.6 (23.5–23.7) | 24.2 (24.1–24.2) | 24.8 (24.8–24.9) |
| Waist circumference, cm | 77.1 (77.0–77.3) | 78.5 (78.3–78.7) | 79.8 (79.6–80.0) | 81.3 (81.1–81.5) | 82.9 (82.6–83.1) |
| Fasting plasma glucose, mg/dL | 111.3 (110.6–112.0) | 101.2 (100.9–101.5) | 98.3 (98.0–98.5) | 95.4 (95.1–95.6) | 89.0 (88.7–89.3) |
| OGTT 2-h plasma glucose, mg/dL | 130.6 (129.2–132.0) | 113.2 (112.4–113.9) | 109.4 (108.8–110.1) | 106.6 (106.0–107.2) | 103.2 (102.6–103.8) |
| HbA1c, % | 6.0 (6.0–6.0) | 5.7 (5.7–5.7) | 5.7 (5.7–5.7) | 5.6 (5.6–5.6) | 5.6 (5.6–5.6) |
| Fasting serum insulin, mIU/L | 3.2 (3.2–3.3) | 4.4 (4.3–4.4) | 5.6 (5.6–5.6) | 7.3 (7.2–7.3) | 11.2 (11.1–11.4) |
| Total cholesterol, mg/dL | 153.2 (152.4–154.0) | 155.2 (154.4–155.9) | 157.5 (156.7–158.3) | 159.0 (158.1–159.8) | 159.7 (158.9–160.5) |
| LDL cholesterol, mg/dL | 84.3 (83.7–84.9) | 86.8 (86.2–87.3) | 88.8 (88.2–89.3) | 90.1 (89.5–90.7) | 90.5 (89.9–91.1) |
| HDL cholesterol, mg/dL | 44.2 (43.9–44.4) | 43.5 (43.3–43.8) | 42.7 (42.5–42.9) | 42.2 (42.0–42.4) | 41.6 (41.4–41.8) |
| Triglycerides, mg/dL | 102.4 (100.1–104.6) | 105.7 (103.9–107.5) | 117.6 (115.6–119.6) | 129.2 (126.8–131.7) | 144.3 (141.8–146.7) |
| Systolic blood pressure, mm Hg | 135.3 (134.9–135.7) | 131.9 (131.5–132.3) | 130.7 (130.3–131.1) | 129.8 (129.5–130.2) | 129.2 (128.9–129.6) |
| Diastolic blood pressure, mm Hg | 81.0 (80.7–81.2) | 80.3 (80.1–80.5) | 80.6 (80.4–80.8) | 80.7 (80.5–80.9) | 80.7 (80.5–80.9) |
Data are weighted means (95% CIs) for continuous variables and weighted percentages (95% CI) for categorical variables.
Ranges of HOMA-B in men were 5.57 to 29.03 for quintile 1, 29.04 to 43.64 for quintile 2, 43.65 to 61.82 for quintile 3, 61.83 to 94.81 for quintile 4, and 94.82 to 428.57 for quintile 5; in women, ranges were 5.57 to 38.52 for quintile 1, 38.53 to 54.44 for quintile 2, 54.45 to 73.20 for quintile 3, 73.21 to 105.63 for quintile 4, and 105.64 to 428.57 for quintile 5.
Table 3 and Table 4 list the prevalence ratios for cardiometabolic disorders according to sex-specific quintiles of HOMA-IR and HOMA-B, respectively. The prevalence of cardiometabolic disorders gradually increased across increasing quintiles of HOMA-IR, with the strongest association with diabetes, followed by obesity, central obesity, hypertension, and dyslipidemia. In addition, lower HOMA-B quintiles were associated with a higher prevalence of diabetes, hypertension, and dyslipidemia, but with lower prevalence of obesity and central obesity.
Weighted Prevalence Ratios for Cardiometabolic Disorders According to HOMA-IR Quintiles
| Cardiometabolic Disorder . | HOMA-IR Quintiles . | P for Trend . | ||||
|---|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | ||
| Obesitya | ||||||
| Prevalence (95% CI) | 0.8 (0.6–1.0) | 1.5 (1.2–1.7) | 2.4 (2.1–2.7) | 5.3 (4.9–5.7) | 14.1 (13.5–14.7) | |
| Prevalence ratio (95% CI)b | 1.00 | 1.73 (1.34–2.22) | 2.66 (2.11–3.34) | 5.44 (4.39–6.75) | 13.14 (10.63–16.23) | < 0.0001 |
| Central obesitya | ||||||
| Prevalence (95% CI) | 13.4 (12.8–14.0) | 20.4 (19.7–21.1) | 27.6 (26.8–28.5) | 37.9 (37.0–38.8) | 56.3 (55.3–57.2) | |
| Prevalence ratio (95% CI)b | 1.00 | 1.55 (1.47–1.64) | 2.11 (2.00–2.23) | 2.83 (2.69–2.99) | 4.07 (3.86–4.29) | < 0.0001 |
| Diabetesa | ||||||
| Prevalence (95% CI) | 3.9 (3.5–4.2) | 4.2 (3.8–4.6) | 5.3 (4.9–5.7) | 7.8 (7.3–8.3) | 21.5 (20.8–22.3) | |
| Prevalence ratio (95% CI)c | 1.00 | 1.57 (1.38–1.78) | 2.73 (2.43–3.08) | 5.47 (4.89–6.12) | 18.73 (16.89–20.78) | < 0.0001 |
| Dyslipidemiaa | ||||||
| Prevalence (95% CI) | 44.1 (43.1–45.0) | 45.2 (44.2–46.1) | 49.5 (48.5–50.5) | 54.3 (53.4–55.3) | 65.1 (64.1–66.0) | |
| Prevalence ratio (95% CI)c | 1.00 | 0.98 (0.95–1.01) | 1.02 (0.99–1.05) | 1.06 (1.03–1.09) | 1.16 (1.13–1.20) | < 0.0001 |
| Hypertensiona | ||||||
| Prevalence (95% CI) | 29.2 (28.4–30.1) | 29.4 (28.5–30.2) | 30.2 (29.4–31.1) | 34.2 (33.3–35.0) | 43.2 (42.3–44.1) | |
| Prevalence ratio (95% CI)c | 1.00 | 1.05 (1.01–1.09) | 1.08 (1.04–1.13) | 1.18 (1.13–1.22) | 1.33 (1.28–1.39) | < 0.0001 |
| Cardiometabolic Disorder . | HOMA-IR Quintiles . | P for Trend . | ||||
|---|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | ||
| Obesitya | ||||||
| Prevalence (95% CI) | 0.8 (0.6–1.0) | 1.5 (1.2–1.7) | 2.4 (2.1–2.7) | 5.3 (4.9–5.7) | 14.1 (13.5–14.7) | |
| Prevalence ratio (95% CI)b | 1.00 | 1.73 (1.34–2.22) | 2.66 (2.11–3.34) | 5.44 (4.39–6.75) | 13.14 (10.63–16.23) | < 0.0001 |
| Central obesitya | ||||||
| Prevalence (95% CI) | 13.4 (12.8–14.0) | 20.4 (19.7–21.1) | 27.6 (26.8–28.5) | 37.9 (37.0–38.8) | 56.3 (55.3–57.2) | |
| Prevalence ratio (95% CI)b | 1.00 | 1.55 (1.47–1.64) | 2.11 (2.00–2.23) | 2.83 (2.69–2.99) | 4.07 (3.86–4.29) | < 0.0001 |
| Diabetesa | ||||||
| Prevalence (95% CI) | 3.9 (3.5–4.2) | 4.2 (3.8–4.6) | 5.3 (4.9–5.7) | 7.8 (7.3–8.3) | 21.5 (20.8–22.3) | |
| Prevalence ratio (95% CI)c | 1.00 | 1.57 (1.38–1.78) | 2.73 (2.43–3.08) | 5.47 (4.89–6.12) | 18.73 (16.89–20.78) | < 0.0001 |
| Dyslipidemiaa | ||||||
| Prevalence (95% CI) | 44.1 (43.1–45.0) | 45.2 (44.2–46.1) | 49.5 (48.5–50.5) | 54.3 (53.4–55.3) | 65.1 (64.1–66.0) | |
| Prevalence ratio (95% CI)c | 1.00 | 0.98 (0.95–1.01) | 1.02 (0.99–1.05) | 1.06 (1.03–1.09) | 1.16 (1.13–1.20) | < 0.0001 |
| Hypertensiona | ||||||
| Prevalence (95% CI) | 29.2 (28.4–30.1) | 29.4 (28.5–30.2) | 30.2 (29.4–31.1) | 34.2 (33.3–35.0) | 43.2 (42.3–44.1) | |
| Prevalence ratio (95% CI)c | 1.00 | 1.05 (1.01–1.09) | 1.08 (1.04–1.13) | 1.18 (1.13–1.22) | 1.33 (1.28–1.39) | < 0.0001 |
Numbers of missing values were 57 for obesity, 49 for central obesity, 505 for diabetes, 49 for dyslipidemia, and 35 for hypertension.
Data were adjusted for age (18-44, 45-64, ≥65 years), sex, urbanization (urban, rural), economic development (underdevelopment, intermediately development, development), education attainment (≤6 or >6 years), current smoking (yes, no), current drinking (yes, no), physical activity (in quintiles), and HOMA-B values (in quintiles).
Data were further adjusted for parental history of diabetes, parental history of hypertension, and the joint categories of BMI and waist circumference (BMI <23 kg/m2 and normal waist circumference; BMI <23 kg/m2 and central obesity; BMI 23-24.9 kg/m2 and normal waist circumference; BMI 23-24.9 kg/m2 and central obesity; BMI 25-29.9 kg/m2 and normal waist circumference; BMI 25-29.9 kg/m2 and central obesity; BMI ≥30 kg/m2 and normal waist circumference; and BMI ≥30 kg/m2 and central obesity).
Weighted Prevalence Ratios for Cardiometabolic Disorders According to HOMA-IR Quintiles
| Cardiometabolic Disorder . | HOMA-IR Quintiles . | P for Trend . | ||||
|---|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | ||
| Obesitya | ||||||
| Prevalence (95% CI) | 0.8 (0.6–1.0) | 1.5 (1.2–1.7) | 2.4 (2.1–2.7) | 5.3 (4.9–5.7) | 14.1 (13.5–14.7) | |
| Prevalence ratio (95% CI)b | 1.00 | 1.73 (1.34–2.22) | 2.66 (2.11–3.34) | 5.44 (4.39–6.75) | 13.14 (10.63–16.23) | < 0.0001 |
| Central obesitya | ||||||
| Prevalence (95% CI) | 13.4 (12.8–14.0) | 20.4 (19.7–21.1) | 27.6 (26.8–28.5) | 37.9 (37.0–38.8) | 56.3 (55.3–57.2) | |
| Prevalence ratio (95% CI)b | 1.00 | 1.55 (1.47–1.64) | 2.11 (2.00–2.23) | 2.83 (2.69–2.99) | 4.07 (3.86–4.29) | < 0.0001 |
| Diabetesa | ||||||
| Prevalence (95% CI) | 3.9 (3.5–4.2) | 4.2 (3.8–4.6) | 5.3 (4.9–5.7) | 7.8 (7.3–8.3) | 21.5 (20.8–22.3) | |
| Prevalence ratio (95% CI)c | 1.00 | 1.57 (1.38–1.78) | 2.73 (2.43–3.08) | 5.47 (4.89–6.12) | 18.73 (16.89–20.78) | < 0.0001 |
| Dyslipidemiaa | ||||||
| Prevalence (95% CI) | 44.1 (43.1–45.0) | 45.2 (44.2–46.1) | 49.5 (48.5–50.5) | 54.3 (53.4–55.3) | 65.1 (64.1–66.0) | |
| Prevalence ratio (95% CI)c | 1.00 | 0.98 (0.95–1.01) | 1.02 (0.99–1.05) | 1.06 (1.03–1.09) | 1.16 (1.13–1.20) | < 0.0001 |
| Hypertensiona | ||||||
| Prevalence (95% CI) | 29.2 (28.4–30.1) | 29.4 (28.5–30.2) | 30.2 (29.4–31.1) | 34.2 (33.3–35.0) | 43.2 (42.3–44.1) | |
| Prevalence ratio (95% CI)c | 1.00 | 1.05 (1.01–1.09) | 1.08 (1.04–1.13) | 1.18 (1.13–1.22) | 1.33 (1.28–1.39) | < 0.0001 |
| Cardiometabolic Disorder . | HOMA-IR Quintiles . | P for Trend . | ||||
|---|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | ||
| Obesitya | ||||||
| Prevalence (95% CI) | 0.8 (0.6–1.0) | 1.5 (1.2–1.7) | 2.4 (2.1–2.7) | 5.3 (4.9–5.7) | 14.1 (13.5–14.7) | |
| Prevalence ratio (95% CI)b | 1.00 | 1.73 (1.34–2.22) | 2.66 (2.11–3.34) | 5.44 (4.39–6.75) | 13.14 (10.63–16.23) | < 0.0001 |
| Central obesitya | ||||||
| Prevalence (95% CI) | 13.4 (12.8–14.0) | 20.4 (19.7–21.1) | 27.6 (26.8–28.5) | 37.9 (37.0–38.8) | 56.3 (55.3–57.2) | |
| Prevalence ratio (95% CI)b | 1.00 | 1.55 (1.47–1.64) | 2.11 (2.00–2.23) | 2.83 (2.69–2.99) | 4.07 (3.86–4.29) | < 0.0001 |
| Diabetesa | ||||||
| Prevalence (95% CI) | 3.9 (3.5–4.2) | 4.2 (3.8–4.6) | 5.3 (4.9–5.7) | 7.8 (7.3–8.3) | 21.5 (20.8–22.3) | |
| Prevalence ratio (95% CI)c | 1.00 | 1.57 (1.38–1.78) | 2.73 (2.43–3.08) | 5.47 (4.89–6.12) | 18.73 (16.89–20.78) | < 0.0001 |
| Dyslipidemiaa | ||||||
| Prevalence (95% CI) | 44.1 (43.1–45.0) | 45.2 (44.2–46.1) | 49.5 (48.5–50.5) | 54.3 (53.4–55.3) | 65.1 (64.1–66.0) | |
| Prevalence ratio (95% CI)c | 1.00 | 0.98 (0.95–1.01) | 1.02 (0.99–1.05) | 1.06 (1.03–1.09) | 1.16 (1.13–1.20) | < 0.0001 |
| Hypertensiona | ||||||
| Prevalence (95% CI) | 29.2 (28.4–30.1) | 29.4 (28.5–30.2) | 30.2 (29.4–31.1) | 34.2 (33.3–35.0) | 43.2 (42.3–44.1) | |
| Prevalence ratio (95% CI)c | 1.00 | 1.05 (1.01–1.09) | 1.08 (1.04–1.13) | 1.18 (1.13–1.22) | 1.33 (1.28–1.39) | < 0.0001 |
Numbers of missing values were 57 for obesity, 49 for central obesity, 505 for diabetes, 49 for dyslipidemia, and 35 for hypertension.
Data were adjusted for age (18-44, 45-64, ≥65 years), sex, urbanization (urban, rural), economic development (underdevelopment, intermediately development, development), education attainment (≤6 or >6 years), current smoking (yes, no), current drinking (yes, no), physical activity (in quintiles), and HOMA-B values (in quintiles).
Data were further adjusted for parental history of diabetes, parental history of hypertension, and the joint categories of BMI and waist circumference (BMI <23 kg/m2 and normal waist circumference; BMI <23 kg/m2 and central obesity; BMI 23-24.9 kg/m2 and normal waist circumference; BMI 23-24.9 kg/m2 and central obesity; BMI 25-29.9 kg/m2 and normal waist circumference; BMI 25-29.9 kg/m2 and central obesity; BMI ≥30 kg/m2 and normal waist circumference; and BMI ≥30 kg/m2 and central obesity).
Weighted Prevalence Ratios for Cardiometabolic Disorders According to HOMA-B Quintiles
| Cardiometabolic Disorder . | HOMA-B Quintiles . | P for Trend . | ||||
|---|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | ||
| Obesitya | ||||||
| Prevalence (95% CI) | 1.9 (1.7–2.1) | 2.6 (2.3–2.9) | 3.9 (3.5–4.2) | 5.9 (5.5–6.3) | 10.3 (9.7–10.9) | |
| Prevalence ratio (95% CI)b | 0.60 (0.52–0.70) | 0.64 (0.56–0.73) | 0.66 (0.59–0.73) | 0.73 (0.67–0.79) | 1.00 | < 0.0001 |
| Central obesitya | ||||||
| Prevalence (95% CI) | 21.7 (21.0–22.4) | 25.9 (25.1–26.7) | 30.7 (29.9–31.5) | 37.1 (36.2–38.0) | 42.8 (41.8–43.7) | |
| Prevalence ratio (95% CI)b | 0.84 (0.81–0.88) | 0.90 (0.86–0.93) | 0.91 (0.88–0.94) | 0.95 (0.92–0.98) | 1.00 | < 0.0001 |
| Diabetesa | ||||||
| Prevalence (95% CI) | 19.9 (19.1–20.6) | 8.5 (8.0–9.0) | 6.4 (5.9–6.8) | 5.5 (5.1–6.0) | 5.0 (4.6–5.4) | |
| Prevalence ratio (95% CI)c | 14.27 (13.08–15.57) | 4.79 (4.35–5.28) | 2.37 (2.14–2.64) | 1.44 (1.29–1.60) | 1.00 | < 0.0001 |
| Dyslipidemiaa | ||||||
| Prevalence (95% CI) | 47.0 (46.1–48.0) | 48.2 (47.2–49.1) | 52.1 (51.2–53.1) | 54.0 (53.0–55.0) | 57.9 (56.9–58.9) | |
| Prevalence ratio (95% CI)c | 1.06 (1.03–1.09) | 1.01 (0.98–1.04) | 1.02 (0.99–1.05) | 0.99 (0.97–1.01) | 1.00 | 0.001 |
| Hypertensiona | ||||||
| Prevalence (95% CI) | 39.4 (38.5–40.3) | 33.9 (33.0–34.8) | 33.1 (32.2–34.0) | 31.2 (30.3–32.0) | 30.5 (29.7–31.4) | |
| Prevalence ratio (95% CI)c | 1.39 (1.34–1.44) | 1.21 (1.16–1.25) | 1.13 (1.09–1.17) | 1.02 (0.99–1.06) | 1.00 | < 0.0001 |
| Cardiometabolic Disorder . | HOMA-B Quintiles . | P for Trend . | ||||
|---|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | ||
| Obesitya | ||||||
| Prevalence (95% CI) | 1.9 (1.7–2.1) | 2.6 (2.3–2.9) | 3.9 (3.5–4.2) | 5.9 (5.5–6.3) | 10.3 (9.7–10.9) | |
| Prevalence ratio (95% CI)b | 0.60 (0.52–0.70) | 0.64 (0.56–0.73) | 0.66 (0.59–0.73) | 0.73 (0.67–0.79) | 1.00 | < 0.0001 |
| Central obesitya | ||||||
| Prevalence (95% CI) | 21.7 (21.0–22.4) | 25.9 (25.1–26.7) | 30.7 (29.9–31.5) | 37.1 (36.2–38.0) | 42.8 (41.8–43.7) | |
| Prevalence ratio (95% CI)b | 0.84 (0.81–0.88) | 0.90 (0.86–0.93) | 0.91 (0.88–0.94) | 0.95 (0.92–0.98) | 1.00 | < 0.0001 |
| Diabetesa | ||||||
| Prevalence (95% CI) | 19.9 (19.1–20.6) | 8.5 (8.0–9.0) | 6.4 (5.9–6.8) | 5.5 (5.1–6.0) | 5.0 (4.6–5.4) | |
| Prevalence ratio (95% CI)c | 14.27 (13.08–15.57) | 4.79 (4.35–5.28) | 2.37 (2.14–2.64) | 1.44 (1.29–1.60) | 1.00 | < 0.0001 |
| Dyslipidemiaa | ||||||
| Prevalence (95% CI) | 47.0 (46.1–48.0) | 48.2 (47.2–49.1) | 52.1 (51.2–53.1) | 54.0 (53.0–55.0) | 57.9 (56.9–58.9) | |
| Prevalence ratio (95% CI)c | 1.06 (1.03–1.09) | 1.01 (0.98–1.04) | 1.02 (0.99–1.05) | 0.99 (0.97–1.01) | 1.00 | 0.001 |
| Hypertensiona | ||||||
| Prevalence (95% CI) | 39.4 (38.5–40.3) | 33.9 (33.0–34.8) | 33.1 (32.2–34.0) | 31.2 (30.3–32.0) | 30.5 (29.7–31.4) | |
| Prevalence ratio (95% CI)c | 1.39 (1.34–1.44) | 1.21 (1.16–1.25) | 1.13 (1.09–1.17) | 1.02 (0.99–1.06) | 1.00 | < 0.0001 |
Numbers of missing values were 57 for obesity, 49 for central obesity, 505 for diabetes, 49 for dyslipidemia, and 35 for hypertension.
Data were adjusted for age (18-44, 45-64, ≥65 years), sex, urbanization (urban, rural), economic development (underdevelopment, intermediately development, development), education attainment (≤6 or >6 years), current smoking (yes, no), current drinking (yes, no), physical activity (in quintiles), and HOMA-IR values (in quintiles).
Data were further adjusted for parental history of diabetes, parental history of hypertension, and the joint categories of BMI and waist circumference (BMI <23 kg/m2 and normal waist circumference; BMI <23 kg/m2 and central obesity; BMI 23-24.9 kg/m2 and normal waist circumference; BMI 23-24.9 kg/m2 and central obesity; BMI 25-29.9 kg/m2 and normal waist circumference; BMI 25-29.9 kg/m2 and central obesity; BMI ≥30 kg/m2 and normal waist circumference; and BMI ≥30 kg/m2 and central obesity).
Weighted Prevalence Ratios for Cardiometabolic Disorders According to HOMA-B Quintiles
| Cardiometabolic Disorder . | HOMA-B Quintiles . | P for Trend . | ||||
|---|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | ||
| Obesitya | ||||||
| Prevalence (95% CI) | 1.9 (1.7–2.1) | 2.6 (2.3–2.9) | 3.9 (3.5–4.2) | 5.9 (5.5–6.3) | 10.3 (9.7–10.9) | |
| Prevalence ratio (95% CI)b | 0.60 (0.52–0.70) | 0.64 (0.56–0.73) | 0.66 (0.59–0.73) | 0.73 (0.67–0.79) | 1.00 | < 0.0001 |
| Central obesitya | ||||||
| Prevalence (95% CI) | 21.7 (21.0–22.4) | 25.9 (25.1–26.7) | 30.7 (29.9–31.5) | 37.1 (36.2–38.0) | 42.8 (41.8–43.7) | |
| Prevalence ratio (95% CI)b | 0.84 (0.81–0.88) | 0.90 (0.86–0.93) | 0.91 (0.88–0.94) | 0.95 (0.92–0.98) | 1.00 | < 0.0001 |
| Diabetesa | ||||||
| Prevalence (95% CI) | 19.9 (19.1–20.6) | 8.5 (8.0–9.0) | 6.4 (5.9–6.8) | 5.5 (5.1–6.0) | 5.0 (4.6–5.4) | |
| Prevalence ratio (95% CI)c | 14.27 (13.08–15.57) | 4.79 (4.35–5.28) | 2.37 (2.14–2.64) | 1.44 (1.29–1.60) | 1.00 | < 0.0001 |
| Dyslipidemiaa | ||||||
| Prevalence (95% CI) | 47.0 (46.1–48.0) | 48.2 (47.2–49.1) | 52.1 (51.2–53.1) | 54.0 (53.0–55.0) | 57.9 (56.9–58.9) | |
| Prevalence ratio (95% CI)c | 1.06 (1.03–1.09) | 1.01 (0.98–1.04) | 1.02 (0.99–1.05) | 0.99 (0.97–1.01) | 1.00 | 0.001 |
| Hypertensiona | ||||||
| Prevalence (95% CI) | 39.4 (38.5–40.3) | 33.9 (33.0–34.8) | 33.1 (32.2–34.0) | 31.2 (30.3–32.0) | 30.5 (29.7–31.4) | |
| Prevalence ratio (95% CI)c | 1.39 (1.34–1.44) | 1.21 (1.16–1.25) | 1.13 (1.09–1.17) | 1.02 (0.99–1.06) | 1.00 | < 0.0001 |
| Cardiometabolic Disorder . | HOMA-B Quintiles . | P for Trend . | ||||
|---|---|---|---|---|---|---|
| 1 . | 2 . | 3 . | 4 . | 5 . | ||
| Obesitya | ||||||
| Prevalence (95% CI) | 1.9 (1.7–2.1) | 2.6 (2.3–2.9) | 3.9 (3.5–4.2) | 5.9 (5.5–6.3) | 10.3 (9.7–10.9) | |
| Prevalence ratio (95% CI)b | 0.60 (0.52–0.70) | 0.64 (0.56–0.73) | 0.66 (0.59–0.73) | 0.73 (0.67–0.79) | 1.00 | < 0.0001 |
| Central obesitya | ||||||
| Prevalence (95% CI) | 21.7 (21.0–22.4) | 25.9 (25.1–26.7) | 30.7 (29.9–31.5) | 37.1 (36.2–38.0) | 42.8 (41.8–43.7) | |
| Prevalence ratio (95% CI)b | 0.84 (0.81–0.88) | 0.90 (0.86–0.93) | 0.91 (0.88–0.94) | 0.95 (0.92–0.98) | 1.00 | < 0.0001 |
| Diabetesa | ||||||
| Prevalence (95% CI) | 19.9 (19.1–20.6) | 8.5 (8.0–9.0) | 6.4 (5.9–6.8) | 5.5 (5.1–6.0) | 5.0 (4.6–5.4) | |
| Prevalence ratio (95% CI)c | 14.27 (13.08–15.57) | 4.79 (4.35–5.28) | 2.37 (2.14–2.64) | 1.44 (1.29–1.60) | 1.00 | < 0.0001 |
| Dyslipidemiaa | ||||||
| Prevalence (95% CI) | 47.0 (46.1–48.0) | 48.2 (47.2–49.1) | 52.1 (51.2–53.1) | 54.0 (53.0–55.0) | 57.9 (56.9–58.9) | |
| Prevalence ratio (95% CI)c | 1.06 (1.03–1.09) | 1.01 (0.98–1.04) | 1.02 (0.99–1.05) | 0.99 (0.97–1.01) | 1.00 | 0.001 |
| Hypertensiona | ||||||
| Prevalence (95% CI) | 39.4 (38.5–40.3) | 33.9 (33.0–34.8) | 33.1 (32.2–34.0) | 31.2 (30.3–32.0) | 30.5 (29.7–31.4) | |
| Prevalence ratio (95% CI)c | 1.39 (1.34–1.44) | 1.21 (1.16–1.25) | 1.13 (1.09–1.17) | 1.02 (0.99–1.06) | 1.00 | < 0.0001 |
Numbers of missing values were 57 for obesity, 49 for central obesity, 505 for diabetes, 49 for dyslipidemia, and 35 for hypertension.
Data were adjusted for age (18-44, 45-64, ≥65 years), sex, urbanization (urban, rural), economic development (underdevelopment, intermediately development, development), education attainment (≤6 or >6 years), current smoking (yes, no), current drinking (yes, no), physical activity (in quintiles), and HOMA-IR values (in quintiles).
Data were further adjusted for parental history of diabetes, parental history of hypertension, and the joint categories of BMI and waist circumference (BMI <23 kg/m2 and normal waist circumference; BMI <23 kg/m2 and central obesity; BMI 23-24.9 kg/m2 and normal waist circumference; BMI 23-24.9 kg/m2 and central obesity; BMI 25-29.9 kg/m2 and normal waist circumference; BMI 25-29.9 kg/m2 and central obesity; BMI ≥30 kg/m2 and normal waist circumference; and BMI ≥30 kg/m2 and central obesity).
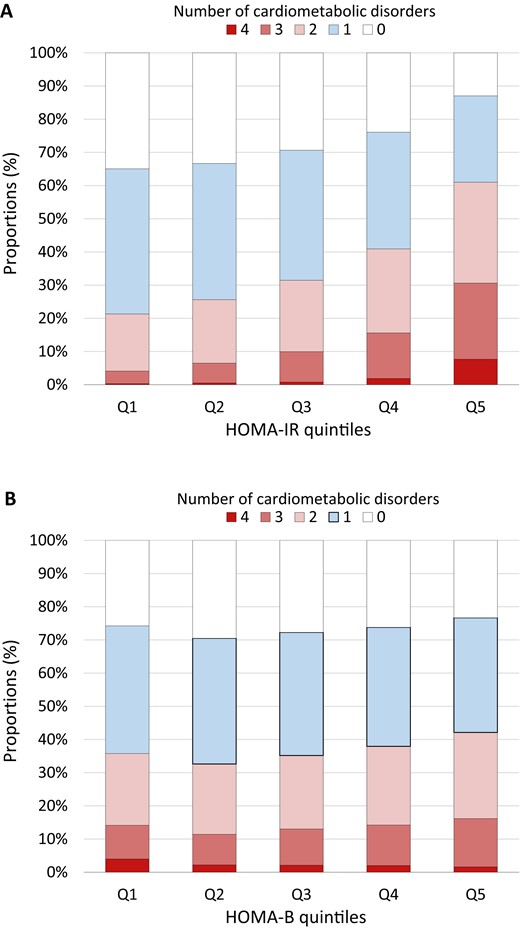
The number of overall cardiometabolic disorders, including obesity or central obesity, diabetes, dyslipidemia, and hypertension, increased across HOMA-IR quintiles but decreased across HOMA-B quintiles (Fig. 1). Proportions of participants with multiple cardiometabolic disorders according to HOMA-IR and HOMA-B quintiles are presented in Supplemental Tables 1 and 2.
Proportions of participants with multiple cardiometabolic disorders according to (A) HOMA-IR and (B) HOMA-B quintiles. Histograms are weighted percentages. The number of cardiometabolic disorders for each participant was the overall presence number of obesity or central obesity, diabetes, dyslipidemia, and hypertension; that is, for each disorder, the participants received a 1 if this disorder was present, and 0 otherwise.
Figure 2 shows the multivariable-adjusted prevalence ratios of cardiometabolic disorders, comparing nine groups of participants with various combinations of HOMA-IR and HOMA-B values. Obesity or central obesity was more prevalent in participants with higher HOMA-IR (corresponding to groups 7, 8, and 9 in Fig. 2). Compared with the other groups, participants with high HOMA-IR and low HOMA-B values (group 9) exhibited the highest prevalence ratios for diabetes, dyslipidemia, and hypertension. Lower HOMA-B value (groups 3, 6, and 9 in Fig. 2) was associated with higher prevalence of diabetes, dyslipidemia, and hypertension, regardless of HOMA-IR value. Likewise, higher HOMA-IR value (groups 7, 8, and 9) was associated with higher prevalence of these cardiometabolic disorders among participants with either low or high HOMA-B values, with exceptions that the combinations of higher HOMA-IR and high HOMA-B values were associated with lower prevalence of diabetes and hypertension than the combinations of lower HOMA-IR and low HOMA-B values (e.g., group 4 vs group 3, and group 7 vs group 6). Supplemental Table 3 lists the cardiometabolic disorders prevalence according to joint categories of HOMA-IR and HOMA-B.
(A, B) Prevalence ratios for cardiometabolic disorders according to joint categories of HOMA-IR and HOMA-B. Data are weighted prevalence ratios (95% CIs). Analyses were adjusted for age (18-44, 45-64, ≥65 years), urbanization (urban, rural), economic development (underdevelopment, intermediately development, development), education attainment (≤6 or >6 years), current smoking (yes, no), current drinking (yes, no), and physical activity (in quintiles) for obesity or central obesity as outcome; and were further adjusted for parental history of diabetes, parental history of hypertension, and the joint categories of BMI and waist circumference (BMI <23 kg/m2 and normal waist circumference; BMI <23 kg/m2 and central obesity; BMI 23-24.9 kg/m2 and normal waist circumference; BMI 23-24.9 kg/m2 and central obesity; BMI 25-29.9 kg/m2 and normal waist circumference; BMI 25-29.9 kg/m2 and central obesity; BMI ≥30 kg/m2 and normal waist circumference; and BMI ≥30 kg/m2 and central obesity) for other outcomes. HOMA-IR and HOMA-B values were divided by the respective quintiles: For HOMA-IR values, low refers to quintiles 1 and 2, median refers to quintiles 3 and 4, and high refers to quintile 5; for HOMA-B levels, low refers to quintile 1; median refers to quintiles 2 and 3; and high refers to quintiles 4 and 5.
Discussion
In a nationally representative sample of Chinese adults aged ≥18 years, the current study comprehensively investigated the independent and joint associations of IR and β-cell dysfunction with multiple cardiometabolic disorders. We found that high HOMA-IR value was consistently and independently associated with high prevalence of all established cardiometabolic disorders, whereas low HOMA-B value was independently associated with high prevalence of diabetes, dyslipidemia, and hypertension but low prevalence of obesity and central obesity. The prevalence of cardiometabolic disorders showed different patterns with varying magnitudes according to combinations of HOMA-IR and HOMA-B: Generally, diabetes, dyslipidemia, and hypertension were more prevalent among participants with high HOMA-IR and low HOMA-B values, whereas obesity or central obesity was more prevalent among those with high HOMA-IR and high HOMA-B values.
In the current study, as expected, both IR and β-cell dysfunction showed the strongest independent associations with diabetes among all cardiometabolic disorders, which was in line with the fundamental roles of IR and β-cell dysfunction in the development of diabetes (3, 4). In addition, according to various combinations of IR and β-cell dysfunction, the association of low HOMA-B value with high prevalence of diabetes was strengthened by high HOMA-IR value, and vice versa. Interestingly, low HOMA-B value was associated with an overwhelmingly high prevalence of diabetes, regardless of HOMA-IR value, whereas the relation between high HOMA-IR value and diabetes seemed to be partly counteracted by high HOMA-B value. In previous studies of East Asian people, individuals who had decreased β-cell function that could not compensate for the progressive decline in insulin sensitivity were at high risk of developing diabetes, and β-cell dysfunction has been suggested to be a better predictor for diabetes than IR in Japanese and Korean populations (21–23). For persons at high risk of diabetes, such as women with prior gestational diabetes, β-cell dysfunction had more pronounced contribution to postpartum diabetes among nonobese individuals, whereas IR contributed more to postpartum hyperglycemia among obese individuals (24). Our findings are in line with those of the previous studies and have added evidence from a representative sample of general Chinese adults that although both IR and β-cell dysfunction were strongly associated with high prevalence of diabetes, low HOMA-B values had a more prominent association with diabetes than high HOMA-IR values.
On the other hand, although β-cell dysfunction plays a critical role in affecting the pathogenesis of diabetes (10, 25), IR precedes the development of β-cell dysfunction and has been associated with obesity, dyslipidemia, and hypertension through mechanisms including inducing low-grade inflammation, modifying lipoprotein particles, impairing endothelial function, and an overactivating sympathetic nervous system (7, 26). However, the associations between β-cell dysfunction and these diabetes-related cardiometabolic disorders in general populations seemed to be less thoroughly documented (27). Studies have reported that β-cell function could remain stable or exhibit high activity in overweight or obese individuals, mainly due to the compensatory insulin secretion of β-cells in response to IR in obese individuals (28–30). But the compensation in insulin secretion may hit the limit with continued deterioration of IR (31). This evidence supports our findings that high HOMA-IR value was associated with more prevalent cardiometabolic disorders than was low HOMA-B value, whereas low HOMA-B value was not associated with a higher prevalence of obesity or central obesity unless combined with high HOMA-IR value.
The current study investigated the joint association of IR and β-cell dysfunction with cardiometabolic disorders in a nationally representative sample of Chinese adults. Our findings have important public health and clinical implications. Given that people with varying combinations of IR and β-cell dysfunction may have distinct cardiometabolic risk patterns, preventive and therapeutic strategies would be tailored toward individuals with specific risk patterns. The strengths of the current study included the nationally representative sample of Chinese adults, the strict quality assurance in data collection, the validated and reliable data, and the availability of biochemical markers of insulin metabolism and cardiometabolic risk. This study has several limitations. First, based on cross-sectional observations and potential reverse causation bias, we could not provide insight into the time dependency of changes in insulin sensitivity and β-cell function in relation to the development of cardiometabolic disorders. Second, we used the HOMA model to estimate IR and β-cell dysfunction. Demonstrated disposition index, a more useful marker of integrated β-cell function adjusted for insulin sensitivity, has been demonstrated as a better index to predict diabetes (23). Although the HOMA model is the most widely used surrogate measure for assessing IR and β-cell dysfunction in clinical and epidemiological studies, and validation studies have revealed good correlations between the HOMA model and the gold standard methods (32), the data should be interpreted carefully and dynamic testing is necessary to validate these findings. Third, although we have carefully adjusted for a set of confounders in the analysis, unmeasured confounders, such as dietary factors, may affect the observations.
In conclusion, in a nationally representative sample of Chinese adults, our data indicate that IR and β-cell dysfunction may synergistically influence cardiometabolic risk patterns. Our findings suggest that tailored treatment and intervention efforts may be required to prevent the progression of IR and β-cell dysfunction to diabetes and related cardiometabolic disorders in the Chinese population.
Abbreviations:
- BMI
body mass index
- CI
confidence interval
- HbA1c
glycated hemoglobin A1c
- HDL
high-density lipoprotein
- HOMA-B
homeostasis model assessment of β-cell function
- HOMA-IR
homeostasis model assessment of insulin resistance
- IR
insulin resistance
- LDL
low-density lipoprotein
- MET
metabolic equivalent
- OGTT
oral glucose tolerance test
Acknowledgments
Financial Support: This work was funded by the Chinese Ministry of Finance. It is also supported by the 973 Foundation (Grant 2015CB553601), National Key R&D Program of China (Grants 2016YFC1305600, 2017YFC1310700, 2016YFC0901200, and 2016YFC1304904), Nonprofit Industry Research Subject (Grant 201502007), National Natural Science Foundation of China [Grants 81500610 (to T.W.), 81622011, 81471062, 81500660, 81390352, and 81621061], and the “Shanghai Municipal Education Commission–Gaofeng Clinical Medicine Grant Support” from Shanghai Jiao Tong University School of Medicine (Grants 20171901, 20152508, 20161301, and 20161307).
Author Contributions: T.W., L.Q., G.N., W.W., and Y.B. contributed to the study conception and design. T.W., Z.Z., Y.X., M.X., J.L., M.L., Y.C., M.D., W.Z., and G.N. contributed to data acquisition. T.W., Z.Z., Y.X., and L.Q. contributed to data analysis and interpretation. T.W. and L.Q. drafted the manuscript. T.W., Z.Z., Y.X., L.Q., G.N., W.W., and Y.B. contributed to the critical revision of the report. G.N., W.W., and Y.B. directed the study.
Disclosure Summary: The authors have nothing to disclose.
References
World Health Organization. Obesity: preventing and managing the global epidemic. Available at: http://www.who.int/nutrition/publications/obesity_executive_summary.pdf. Accessed 1 January 2018.
The World Health Organization Western Pacific Region. The Asia-Pacific perspective: redefining obesity and its treatment. Available at: http://www.wpro.who.int/nutrition/documents/docs/Redefiningobesity.pdf. Accessed 1 January 2018.
Author notes
These authors contributed equally to this work.