-
PDF
- Split View
-
Views
-
Cite
Cite
Reinhold Ganz, Guido Grappiolo, Jeffrey W Mast, Joel Matta, Luigino Turchetto, Technical particularities of joint preserving hip surgery in osteopetrosis, Journal of Hip Preservation Surgery, Volume 4, Issue 4, December 2017, Pages 269–275, https://doi.org/10.1093/jhps/hnx032
Close - Share Icon Share
Abstract
Proximal femoral fracture and coxarthrosis are the most common orthopaedic problems of osteopetrosis. Fracture fixation is difficult and one-third fail, with total hip replacement as the final solution. There is little reported experience about how to deal with this particular type of bone and what has been published to date is surprisingly non-specific. Corrective osteotomies are mainly undertaken in children for non-union of a fractured femoral neck and/or for coxa vara. However, any information about technical problems and solutions is scarce and barely instructive. Osteotomy experience for osteopetrosis in youngsters and young adults has not been reported. Osteopetrosis bone is characterized by a small tolerance for displacement and by the high friction experienced when penetrating instruments and implants are used. This article describes the risks of hip surgery in the presence of osteopetrosis and also discusses osteotomies around the hip and how to limit any related complications. Four patients, who underwent different types of hip preservation procedure, have been used to illustrate the difficulties that can be encountered. The article also suggests ways to make osteotomies feasible in osteopetrosis bone, even in adults.
INTRODUCTION
Osteopetrosis was first published in 1904 by Albers-Schoenberg [1] and later by Karschner [2]. It is based on osteoclast dysfunction leading to failure of bone resorption and to increase of bone mass. Persistance of chondroid and primitive bone formation makes bone brittle [3]. In human osteopetrosis the main variants are (i) the malignant autosomal recessive infantile form, (ii) the intermediate autosomal recessive form and (iii) the autosomal dominant form [4, 5]. Patients with the malignant infantile form present pathological fractures at birth or early in infancy combined with severe bone marrow dysfunction. Life expectance is severely reduced due to haemorrage and/or sepsis [6]. The intermediate autosomal recessive form is rare and usually diagnosed from pathological fractures in childhood; patients survive into adulthood [6]. Prevalent and of primary orthopaedic interest is the autosomal dominant osteopetrosis, which can be further subdivided into Types I and II according to the radiological sclerosis pattern of the axial skeleton; type I is supposed to be slightly more benign [4]. Most manifestations of the condition are seen in the area of the hip [5]. Approximately, one-third of hip prostheses implanted in osteopetrosis are for failed fracture fixation and yet information about the handling of osteopetrosis bone, or any special technical precautions required, are rare and non-specific [7]. Osteotomies in the presence of osteopetrosis are generally confined to subtrochanteric valgization for non-union, or for coxa vara in children. Other osteotomies around the hip are not mentioned, nor are difficulties addressed which may appear during metal removal. In this article, we provide this information and illustrate it with four different examples.
GENERAL REMARKS
The dense structure of osteopetrosis bone is associated with a low modulus of elasticity, allowing little bony deformation. This facilitates fractures when grasping instruments and implants are used. Drills and saw blades may not grasp but nevertheless fill surprisingly fast with bone dust and heat the instrument and surrounding bone. During repetitive irrigation and cleaning it is difficult to maintain instruments in the desired direction. Blunt instruments substantially increase such difficulties. Meanwhile, repeated overheating may lead to breakage while drilling. Tapping a female screw thread can lead to the instrument displacing from its desired track, as well as a tendency to jam with deeper penetration; in the femoral head this may even lead to splitting of the bone, especially when a motorized tap is used.
The high friction between implants and osteopetrosis bone may lead to jamming and destruction of hexagonal screwheads, especially for long screws or those with a small diameter. Powered screwdrivers may predispose to fracture. Implants made from titanium clearly cause higher friction.
Bone healing in osteopetrosis can take longer than normal, especially in cortical bone where osteoclasts are insufficient to create channels in the existing bone and thereby allow osteoblasts to bridge and fill any gaps with new bone.
In addition, the removal of implants can be very laborious and breakage of screw heads is common, so the indications and techniques for surgery must carefully be considered. (Table I)
Specific recommendations
| Pay attention! Bone in osteopetrosis is brittle |
| If possible, do not use grasping instruments and implants like blade plates or bolt plates. |
| Always keep drills and saw blades cool and clean |
| Do not insert screws with powered assistance |
| Avoid long screws with a small diameter |
| Avoid titanium screws |
| Try to avoid removing metalwork |
| When removal is necessary, have special tools available |
| Pay attention! Bone in osteopetrosis is brittle |
| If possible, do not use grasping instruments and implants like blade plates or bolt plates. |
| Always keep drills and saw blades cool and clean |
| Do not insert screws with powered assistance |
| Avoid long screws with a small diameter |
| Avoid titanium screws |
| Try to avoid removing metalwork |
| When removal is necessary, have special tools available |
Specific recommendations
| Pay attention! Bone in osteopetrosis is brittle |
| If possible, do not use grasping instruments and implants like blade plates or bolt plates. |
| Always keep drills and saw blades cool and clean |
| Do not insert screws with powered assistance |
| Avoid long screws with a small diameter |
| Avoid titanium screws |
| Try to avoid removing metalwork |
| When removal is necessary, have special tools available |
| Pay attention! Bone in osteopetrosis is brittle |
| If possible, do not use grasping instruments and implants like blade plates or bolt plates. |
| Always keep drills and saw blades cool and clean |
| Do not insert screws with powered assistance |
| Avoid long screws with a small diameter |
| Avoid titanium screws |
| Try to avoid removing metalwork |
| When removal is necessary, have special tools available |
INTERTROCHANTERIC OSTEOTOMY
A search of the literature yielded three publications, each about paediatric hips. Two reported coxa vara treated by a subtrochanteric valgus osteotomy [8, 9]. No further details were given. The third, by Armstrong, Newfield and Gillespie [10], was a survey and review paper [8]: they reported that of seven fractures, the four that had undergone internal fixation had healed; the three treated non-operatively had failed to heal and developed a varus non-union. In 20 coxa vara hips, valgus osteotomy was consistently reliable, while pinning failed in two out of three cases.
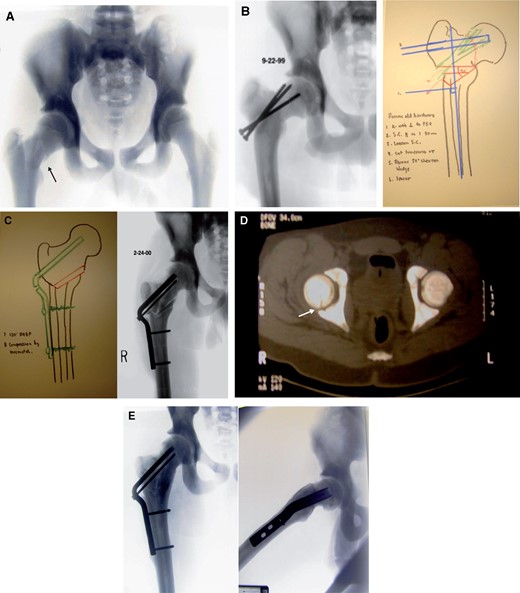
Figure 1A–F demonstrates the course of an intertrochanteric osteotomy in which technical problems led to serious complications. This 15-year-old male patient acquired a right femoral neck fracture (Fig. 1A). The operating note describes a difficult insertion and orientation of K-wires for the preliminary fixation. Similar problems occurred while attempting to maintain accurate drill direction, leading to a suboptimal placement of two short-threaded 6.5 mm screws and one bolt. Tightening of the screws led to rotation of the head and redisplacement of the fracture rather than to the desired interfragmentary compession. Ten months later there was non-union, varus and retrotilting of the head as well as breakout of one screw; a revision procedure was required (Fig. 1B). In an era when screw plates for osteotomies were not yet popularized, preoperative paper planning determined that a double angle blade plate with an 80 mm blade would bridge the non-union and allow normal leg length to be regained (Fig. 1C) [11]. Neutralization of any displacing effect of the seating chisel was obtained with careful pushing and pulling manoeuvres. However, as the instrument was advanced into the femoral head a sound change was followed by easier propagation. A fracture gap leading from the non-union area towards the head was then identified; closure of the gap was observed if the seating chisel was pulled back to the 70 mm mark. Consequently, a blade length 10 mm shorter than had been planned preoperatively was used. With a new saw blade, the intertrochanteric osteotomy was uneventful. The postoperative radiographs were identical with the planning and showed leg length had been restored (Fig. 1C). Postoperative CT imaging revealed a residual gap caused by a split in the femoral head but without a step (Fig. 1D). The patient’s records note that a lengthy period was needed until the osteotomy line disappeared but by 2 years after surgery the radiographs showed full consolidation with a good joint space. However, small ring osteophytes of the femoral head indicated that the joint was compromised (Fig. 1E).
Intertrochanteric valgus osteotomy for neck non-union. (A) A 15-year-old male with a mildly displaced medio-cervical fracture of the right femoral neck after low velocity trauma (arrow). (B) Varus tilt and non-union 10 months after screw fixation. The screws are migrating out of the proximal fragment but their direction is indicative of suboptimal insertion. First phase of planning with a seating chissel in place for 30° valgus correction using a 120° double angle blade plate. An 80-mm blade length should cross the non-union. A 30° wedge resection is mentioned. An additional 15° flexion to compensate for the retrotilt is not visible.in this plane. (C) Second planning paper shows the end result which incorporates full angular correction and leg length. The double line represents the osseous wedge placed into the posterior gap resulting from the flexion of the proximal fragment. The achieved correction has led to identical contours. The blade length is 10mm shorter, which allowed closure of the head split produced by the fully introduced seating chisel. (D) Postoperative computer tomography confirms the almost complete closure of the head split fracture (arrow). (E) Anteroposterior and lateral radiographies 2 years after osteotomy reveal complete healing of the non-union and osteotomy with a round head and large joint space without signs of necrosis. Small circumferential osteophytes may be a complication of the head split.
SUBCAPITAL REALIGNEMENT IN SEVERE CHRONIC SLIPPED CAPITAL FEMORAL EPIPHYSIS
Again, the literature reveals three case reports that deal with slipped capital femoral epiphysis (SCFE) in the context of osteopetrosis [12–14]. In only one, pinning in situ is mentioned but without further comment [13].
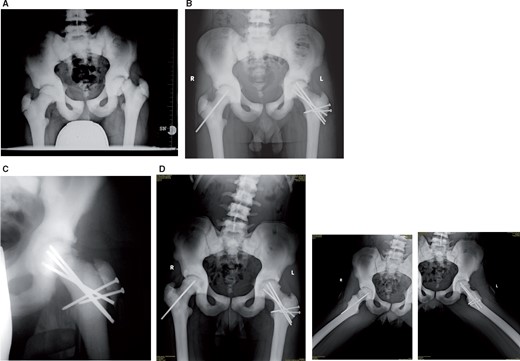
Figure 2A–D shows the subcapital realignment of a severe left-sided SCFE in a 12-year-old boy. As the slip was thought to be unstable (Fig. 2A), the surgical dislocation approach [15] was extended and the epiphysis pinned before dislocation. Drilling of the epiphysis was followed by brisk bleeding. Inspection after full joint dislocation did not show substantial damage to the acetabular labrum and adjacent articular cartilage but did reveal rupture of the femoral neck periosteum, albeit limited to the anterior surface. Even after extension of the retinacular flaps [16], the epiphysis was not detached, although separation was easy. After removal of callus formation at the proximal part of the posterior neck, and debridement of growth plate material, the epiphysis was manually reduced and fixed with a retrograde K-wire through the fovea capitis [16]. Advancing the wire until it perforated at the lateral subtrochanteric cortex was only possible after laborious antegrade predrilling. Similar difficulties were experienced during the antegrade insertion of a second K-wire. For definitive fixation, antegrade insertion of predrilled, fully threaded 3 mm wires was performed. Nevertheless penetration of the wire tip into the epiphysis led to distraction and rotation of the epiphysis, even with the previous K-wires in place. Consequently, retrograde insertion helped avoid interfragmentary distraction (Fig. 2B). Healing time was longer than with normal bone (Fig. 2C). By 3 years after this procedure there were no signs of femoral head necrosis (Fig. 2D).
Subcapital realignment of a severe chronic slipped capital femoral epiphysis (SCFE) in a 12-year-old male. (A) Severe deformity, radiologically and clinically classified as unstable. (B) Result 2 months after subcapital realignement and prophylactic pinning of the contralateral epiphysis. The radiograph does not demonstrate the difficulties in avoiding distraction and fragment rotation during antegrade pinning. The solution was retrograde pinning, only revealed by the blunt pin ends in the epiphysis. (C) Trochanteric osteotomy line still visible at 5 months postoperatively. (D) At 3 years there are comparable hip contours of both hips, which are clinically normal. The projecting pin on the right may possibly be shortened if it troubles the patient when lying on his side.
PERIACETABULAR OSTEOTOMY
It was not possible to find any literature about the use of pelvic osteotomy in osteopetrosis. However, Figure 3A–D shows a periacetabular osteotomy for acetabular dysplasia [17] in a 21-year-old female, with Grade 1–2 cartilage degeneration and osteopetrosis. Execution of the surgical procedure was less laborious than expected, although the resistance of the bone was higher than normal. This may have been because the osteotomy surfaces were smaller and cortices thinner compared with the proximal femur. It proved helpful to use double cuts for the first cortex of the pubis osteotomy and for the osteotomy at the turning point of the supraacetabular to retroacetabular cut. As with the standard procedure, the supraacetabular cut was undertaken with an oscillating saw, the remainder with especially thin and sharp osteotomes. In addition, it was anticipated that osteopetrosis bone might not follow a predetermined breaking line, as seen with normal bone. Consequently, all osteotomies were completed by using hand instruments. After the procedure, although the healing time seemed somewhat prolonged, by 5 years the joint space showed only minor additional narrowing.
Periacetabular osteotomy for acetabular dysplasia. (A) Bilateral residual acetabular dysplasia. While the left hip is asymptomatic the right hip shows Grade 1–2 osteoarthritic changes with slight subluxation; on examination it demonstrated a painful limitation of range of movement. (B) Pelvic radiograph shortly after periacetabular osteotomy showing normalized coverage and reduction of the femoral head. (C) Radiography 18 months after surgery. The main osteotomies are consolidated and the pubis gap is narrowed. (D) Radiograph six-and-a-half years after surgery with slightly decreased superior joint space. The patient reported some discomfort, although only after longer lasting physical activities.
METAL REMOVAL
It was not possible to identify any literature that discussed the special difficulties which can occur during the removal of metalwork from osteopetrosis hips.
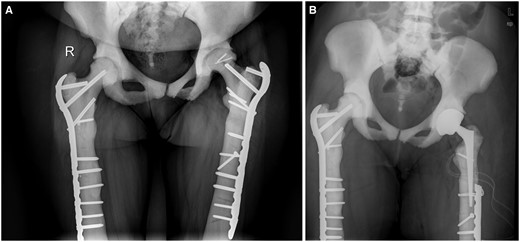
Figure 4A and B demonstrates the laborious and time-consuming efforts which may be needed, including the use of special instrumentation. This 37-year-old female patient suffered first from femoral shaft fractures which were fixed with steel plates. Shortly after consolidation she then sustained a subtrochanteric fracture, first on the right then on the left. The level of the fractures made removal of the existing plates necessary. Surgery to remove the plates was described as time consuming and complicated by breakage of some screwheads. For optimal bridging of the new fracture a special plate was chosen, allowing screw placement into the femoral neck and head while the long shaft covered and protected the screw holes of the former plate. For best positioning of the new plate, two portions of residual screw had to be overdrilled in order to be removed. While fixation and healing on the right side was uneventful, surgery on the left was complicated by a split in the femoral head during final insertion of the screw. The screw was thus replaced by a shorter one and the split femoral head fixed with two small screws. One year later the patient complained of substantial hip pain, possibly related to necrosis and collapse of the femoral head fragment although the subtrochanteric fracture had consolidated (Fig. 4A). A total hip replacement (THR) was thus recommended but to do this metal removal was necessary and special instruments were required, e.g. high speed diamond saw to cut metal and hollow drills to remove broken portions of screw were held available. Although the screws had to be removed for a distance corresponding to the length of the prosthetic stem, it was considered that if the plate and screws were left in place more distally they would provide better protection against a new fracture. Reaming of the femoral shaft to allow insertion of a prosthetic stem was anticipated to be difficult. In the event, this required laborious predrilling to allow the insertion of a small stem size (Fig. 4B).
Total hip replacement (THR) in a 37-year-old female after two bilateral femoral shaft fractures and a head split on the left. (A) On both sides there is one remaining threaded screw part left in place from steel plate fixation of the first fracture. For the second, more proximal fractures on both sides longer plates were used in order to bridge the screw holes. On the left, the implantation of the long screw in the femoral neck was complicated by a split fracture of the head during final seating of the screw against high resistance. The screw was shortened and the head split fixed with small screws. One year later the lateral part of the head collapsed and the joint space narrowed. (B) For THR, removal of the implant was necessary. Cutting of the proximal part of the plate using a high speed diamond saw was preferred to the more laborious attempts to remove the full length of plate and screws. Reaming of a new medullary canal was possible but very time consuming. A thin, conical prosthesis shaft was securely inserted without fracturing the surrounding bone.
DISCUSSION
The purpose of this paper is to demonstrate that even complex osteotomies to preserve the natural hip joint are feasible in osteopetrosis, when a number of technical matters are taken into consideration. Osteopetrosis bone is not very tolerant towards grasping instruments and implants. This is well demonstrated by the split femoral head in two of the cases we present here. The risks of fracture can be reduced if the surgeon prepares the area properly, for example, with a drill or saw. Techniques have also changed. For example, today, for a situation such as Case 2 (above) a screw plate implant would likely be better instead of the displacing blade plate that was used at the time. Conversely, non-displacing tools create high friction and heat, so constant irrigation is imperative as is repetitive irrigation of bone dust. High friction is also an issue during screw implantation, especially when small-diameter and/or long screws have to be inserted. It is possible that the high rate of failure after screw fixation of femoral neck fractures is in part related to the difficulty in applying interfragmentary compression with lag screws. For this same reason titanium implants should not be used in osteopetrosis bone.
One constant observation is that bone healing in osteopetrosis takes longer; therefore, limited weight-bearing should be recommended for a lengthier period than for normal bone. Experience with implant removal comes mainly from the failure of fixation of proximal femoral fractures when the hip is to be replaced by an artificial joint. Implant removal may require special instruments to overdrill any portions of broken screw. While any holes in the lateral femoral cortex may be splinted by a prosthesis stem, distal to this stem such holes may become a stress riser and can lead to a new fracture. Surgeons should remain aware of this and consider cutting the plate, removing its proximal portion, and leaving the distal part, beyond the tip of the prosthesis, still attached to the bone. Metal should not be removed routinely. If removal is unnecessary for inserting a prosthesis, metalwork can be left where it is. Implants left in situ in the femoral head and/or neck might also shield against femoral neck fracture, a rather frequent complication in osteopetrosis.
ACKNOWLEDGEMENT
The authors thank Selina Nauer, research assistant for technical support during preparation of this work.
FUNDING
No funding was used for the purposes of this study.
CONFLICT OF INTEREST STATEMENT
None declared.