-
PDF
- Split View
-
Views
-
Cite
Cite
Majd El Hajj Moussa, Charbel Tawk, Fadi Hoyek, Jean-Claude Lahoud, Traumatic inferior hip dislocation: a rare adult case with ipsilateral bifocal hip fracture, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw056, https://doi.org/10.1093/jscr/rjw056
Close - Share Icon Share
Abstract
Inferior dislocation is a rare type of hip dislocation, especially in adults. Few cases have been reported; most of them were isolated. This is the case of a traumatic adult hip dislocation after a road traffic accident. Reduction was made under general anaesthesia; a CT-Scan after the reduction showed a bifocal non-displaced hip fracture. In this article, we present a small review of the literature and we discuss the possible mechanism of hip dislocation. We found through our case study that this condition is not exclusive to children and CT-Scan is mandatory after the reduction of hip dislocation to eliminate any associated injury. To our knowledge, a bifocal hip fracture has not previously been documented, in the English language literature.
INTRODUCTION
Traumatic hip dislocation has increased due to the higher incidence of accidents involving high energy trauma [1]. Inferior hip dislocation (IHD) is the rarest among all types of hip dislocations and few adult cases have been reported in the literature [2]. We present an adult case of traumatic IHD following motor vehicle accident (MVA) with a bifocal hip fracture detected after reduction.
CASE REPORT
A 24-year-old male sustained a road traffic accident after a suicide attempt. He crashed his car into the wall at 70 mph. At the emergency room, the patient presented with severe right hip pain and a fixed deformity in flexion and abduction. Neurovascular examination was normal. He was slightly dyspnoeic due to a right mild pneumothorax with an oxygen saturation of 98% on room air. No other injuries were associated.
An antero-posterior pelvis radiograph was obtained and showed inferior dislocation of the right femoral head with no associated fracture (Fig. 1). Closed reduction was successfully achieved under general anaesthesia. Reduction consisted of:
Counter-traction using a sheet passed under his hip
Adduction
Internal rotation
Traction
Abduction
External rotation
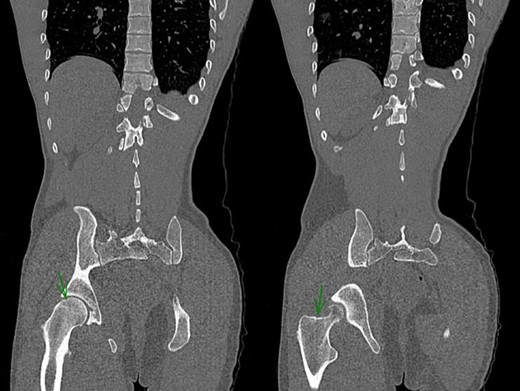
After reduction, the neurovascular examination remained normal. Pelvis CT-scan was performed and showed a bifocal fracture of the hip associating a non-displaced inter-trochanteric fracture and a non-displaced capital fracture (Fig. 2). Patient was discharged on day 5 with strict bed rest for 6 weeks.
Post-reduction CT-Scan of the pelvis showing a non-displaced fracture of the head of the femur and a non-displaced inter-trochanteric fracture of the right hip.
DISCUSSION
A search of the literature revealed 16 studies reporting 34 cases related to luxatio erecta, inferior dislocation or infra-cotyloid dislocation of the hip, the majority of which being in non-English literature. Until 2006, only five cases were reported among adults [2]. A study was published in 2012 [3] reporting a bilateral IHD in a 30-year-old patient. Bartley and Dimon [4] and Ferguson and Harris [5] reported the condition in an adult and a young man, respectively. In our case, the patient was 24-year-old. Hence, it is clear that IHD is not restricted to children as previous literature showed a preponderant incidence in paediatric group, proposed to be due to the lax ligaments in children.
Only three articles reported three cases of IHD associated with an injury to the ipsilateral femur: one recording a case of an inter-trochanteric fracture with IHD [1]; another reporting a great trochanter fracture [6]; and one reporting an associated open sub-trochanteric fracture [2]. In the present case, a non-displaced bifocal hip fracture was present.
When the hip dislocates inferiorly, it is flexed and the distal end of the femur rises above the horizontal plane of the pelvis at the acetabular fossae level. The exact mechanism leading to the deformity is not always remembered and has not been described in detail because the reported cases were children or teenagers. Two mechanisms of injury have been identified producing two different subtypes of IHD [7]. The first mechanism is when force is applied to an abducted, flexed thigh that is externally rotated, the femoral head levers out of the acetabulum. This represents the more common mechanism and probably it is the case of our patient. The femoral head is seen anteriorly in the region of obturator foramen, although in some cases, it may be displaced further laterally to an ischial location.
In the second mechanism, the femur is inverted and the head lies below the acetabulum and lateral to the ischial tuberosity. Hip is acutely flexed and rests against the lower abdomen. The knee is flexed with little abduction or external rotation of the thigh.
CT is advised to rule out any associated injury, but it should never delay reduction. Such delay has been associated with worse prognosis and increased incidence of avascular necrosis. Joint reduction can be achieved under general anesthesia (GA) by maintaining traction towards the head while gradually extending the thigh, sometimes with additional internal rotation. In our case, CT-Scan was performed after hip reduction to rule out any associated injury. It showed a bifocal non-displaced fracture of the hip associating an inter-trochanteric fracture and a capital fracture. The exact timing of the fracture remained unknown. We could not identify whether the initial trauma was the cause of the fracture or the reduction manoeuver.
Since recommendations include 6-week immobilization followed by partial weight bearing, orthopaedic treatment was the choice for the non-displaced hip fracture. Three months later, the patient was in a very good condition. He had full weight bearing with no associated complications.
IHD is a rare injury and very few cases have been reported in the literature, especially in adults. To our knowledge, a bifocal hip fracture has not previously been documented. Prompt diagnosis and treatment are crucial in the management of these cases to avoid neurovascular complications, particularly avascular necrosis of the head of femur. The present study reveals that this condition is not exclusive to children and CT is a must to rule out associated injuries. Closed reduction is usually possible under general anaesthesia and prognosis after reduction is excellent the sooner the reduction.
CONFLICT OF INTEREST STATEMENT
None declared.