-
PDF
- Split View
-
Views
-
Cite
Cite
Nimisha Vallabh, Venkat Srinivasan, David Hughes, David Agbamu, Ancient schwannoma in the sublingual space masquerading as a plunging ranula, Journal of Surgical Case Reports, Volume 2017, Issue 4, April 2017, rjx068, https://doi.org/10.1093/jscr/rjx068
Close - Share Icon Share
Abstract
Ancient schwannomas are benign, slow-growing tumours derived from the neural sheath. They are characterized by degenerative changes which are not seen in the common schwannoma. An unusual case of ancient schwannoma of the sublingual space is reported to highlight the diagnostic challenge that this tumour presents. A 49-year-old male patient presented with an 8-month history of a right-sided neck swelling, palpable in the anterior part of the submandibular triangle. Pre-operative imaging showed a non-enhancing mass in the sublingual space spilling into the submandibular triangle, consistent with a plunging ranula. Fine needle aspiration cytology was inconclusive. However, histopathology of the lesion confirmed the diagnosis of an ancient schwannoma, which is seldom found in the sublingual space.
INTRODUCTION
Ancient schwannomas are benign, slow-growing tumours derived from the neural sheath. They were first described by Ackerman and Taylor in 1951 [1] and can occur in a variety of regions of the head and neck but rarely in the sublingual space [2]. Swellings of the anterior triangle of the neck are common; imaging and fine needle aspiration cytology (FNAC) are often used to aid diagnosis. However, schwannomas remain difficult to diagnose and can be mistaken for other more common conditions. As these tumours often arise from major nerves, surgical management can lead to significant lifelong morbidity. Therefore, pre-operative diagnosis is important to allow the patient to make a fully informed decision regarding management of the tumour.
CASE REPORT
A 49-year-old male patient presented with an 8-month history of a right-sided neck swelling. The patient reported an intermittent dull ache associated with the mass but denied any association with eating. The patients medical history was unremarkable and he was a non-smoker. Clinical examination demonstrated a soft, 2 cm swelling palpable in the anterior part of the right submandibular triangle. There was no swelling seen or palpable in the floor of the mouth. The submandibular duct was clinically normal with no obvious calculi and examination of the neck was unremarkable.
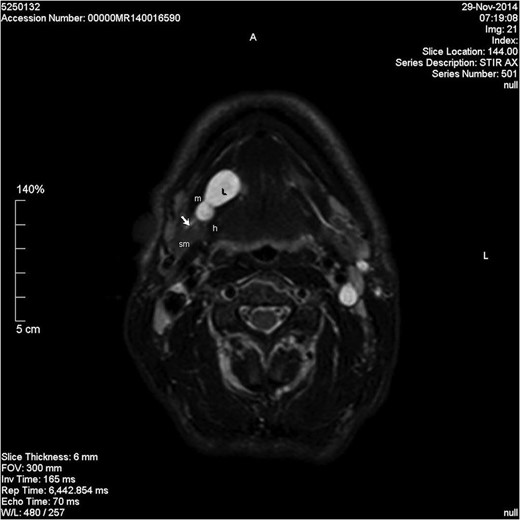
Axial STIR image showing a lobulated homogenous hyperintense lesion in the right floor of mouth. L, lesion; m, mylohyoid muscle; sm, submandibular gland; h, hyoglossus; short arrow, Wharton's duct.
Coronal T2-weighted image. L, lesion; m, mylohyoid muscle; sm, submandibular gland; ad, anterior belly of digastric muscle.
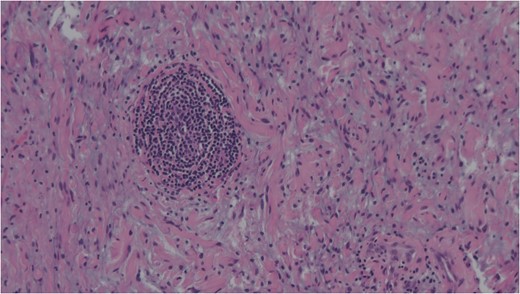
Spindle cells set in a myxoid stroma characteristic of schwannoma. Haemotoxylin and eosin (H&E).
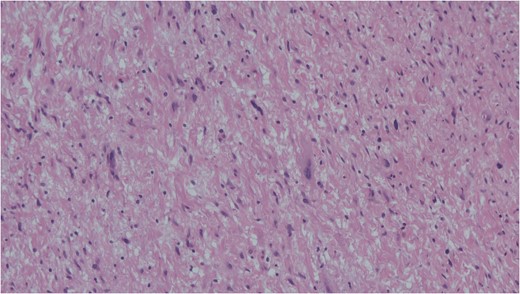
Cells with enlarged hyperchromatic nuclei seen in ancient schwannoma. Haemotoxylin and eosin (H&E).
DISCUSSION
Schwannomas are benign, slow-growing tumours of the neural sheath. They arise from Schwann cells which produce the myelin sheath covering of cranial, peripheral and autonomic nerves. It is reported that 25–45% of extracranial schwannomas are located in the head and neck regions [3], the most common site being the parapharyngeal space [2]. They are relatively rare and are often mistaken for metastatic disease or other non-neurogenic tumours. Once a diagnosis has been made, management may consist of observation, complete surgical excision or intracapsular enucleation.
Schwannoma is difficult to diagnose clinically but, a long-standing history and a firm mass are suggestive [4]. Radiological diagnosis can also be challenging with sensitivity estimated at 20% for computed tomography (CT) and up to 80% for MRI [5]. Ultrasonography is often used in the investigation of neck lumps. However, the appearance of a schwannoma can mimic a pleomorphic adenoma. The literature does not support the use of CT for the diagnosis of schwannoma and MRI is often preferred for better soft tissue delineation. This may aid in diagnosis and identification of the nerve of origin. Schwannomas appear hypointense on T1-weighted images and heterogeneously hyperintense on T2-weighted images [4, 6]. They demonstrate intense enhancement with gadolinium-based contrast. As demonstrated in our case, MRI can still fail to be diagnostic.
FNAC remains a valuable tool to characterize neck masses but its accuracy in schwannoma is only reported to be 20–25% [4, 6]. Macroscopically, schwannomas are smooth and uniform and often attached to their nerve of origin which may help intra-operative diagnosis. Histologically, schwannomas are encapsulated and consist of alternating Antoni-A and Antoni-B regions [7]. Ancient schwannomas can be recognized by their additional degenerative features such as fibrosis, cystic necrosis and degenerative nuclei [7]. They can often be mistaken for malignant tumours due to nuclear atypia and hyperchromasia [7].
The differential diagnosis of a right-sided neck swelling is varied and includes: submandibular gland neoplasm, lymphadenopathy, plunging ranula, haemangioma and lipoma. A ranula is a retention cyst of the sublingual gland which usually occurs secondary to trauma or duct obstruction. It often presents as a bluish swelling in the floor of the mouth. The swelling can extend behind or through the mylohyoid muscle and into the submandibular space forming a plunging ranula [5]. A plunging ranula is usually associated with an intra-oral component but rarely it can present as an isolated neck swelling [5]. The pre-operative imaging of our patient demonstrated a homogenous, non-enhancing lesion involving the sublingual gland and extending into the submandibular space. The lesion did not show enhancement with contrast which is unusual for a schwannoma [8], and may be interpreted as being consistent with a cystic lesion. Both schwannomas and ranulas appear hypointense on T1-weighted images and hyperintense on T2-weighted images. As FNAC was inconclusive, a differential diagnosis of several pathologies was considered based on clinical assessment and radiological investigations. Given the characteristic MRI appearances and the failure to enhance with contrast, a pre-operative diagnosis of plunging ranula was made.
ACKNOWLEDGEMENT
None.
CONFLICT OF INTEREST STATEMENT
None declared.