-
PDF
- Split View
-
Views
-
Cite
Cite
Colleen L. Lau, Mark Sweet, Philip Weinstein, A stitch in time: unrecognized retained foreign bodies after a needlefish injury, Journal of Travel Medicine, Volume 24, Issue 2, March/April 2017, taw092, https://doi.org/10.1093/jtm/taw092
Close - Share Icon Share
We present a case report of a traveller injured by a needlefish in the Caribbean. The needlefish leapt from the ocean and struck the traveller’s face at high speed, causing a seemingly superficial puncture wound on his nose. Later, it became apparent that multiple fish bones had broken off and lodged in his nasal cavity, very narrowly missing his cribriform plate. Some bones were discharged spontaneously through his nose over the next 3 months, and one required surgical removal. Our report highlights the importance of urgent radiological examination in patients injured by needlefish, even if the external wound appears insignificant.
Introduction
Injuries from marine animals are rare in travellers, and generally involve envenomation.1 With the exception of shark bites, non-envenomating physical injuries from fish are very rarely reported in travellers, but include several case reports of needlefish (Belonidae) injury. We add to this literature by presenting a case report from the Caribbean that illustrates the importance of precautionary radiological examination.
Case report
(a) An 8-mm wound over the left side of the nose after being struck in the face by a needlefish, (b) bones spontaneously discharged from the nose and (c) high-resolution photograph of needlefish mandible and teeth (Photo: Gary Taylor, University of Adelaide)
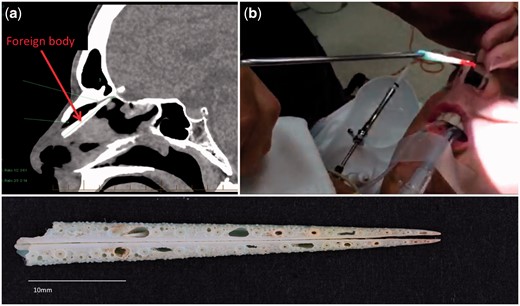
(a) CT scan of the paranasal sinuses, showing a 39-mm long linear foreign body in the upper left nasal cavity, (b) foreign body removed from nasal cavity by an ear, nose and throat surgeon 3 months after needlefish injury and (c) high-resolution photograph of needlefish beak (Photo: Gary Taylor, University of Adelaide)
Because the patient had retained the fish bones, we attempted to extract needlefish DNA to enable identification of the species of needlefish involved, but only human DNA could be recovered (S Donnellan, personal communication). Given the diversity of needlefish in the Caribbean, and the unknown age (size) of the fish responsible, it was not possible to identify the fish to species level based on the bones alone.
Discussion
Needlefish (family Belonidae), also known as Long Tom, are commonly found in tropical and subtropical oceans around the world, with 11 species in 4 genera in the Caribbean.2 They have long narrow jaws that extend into long beaks with sharp jagged teeth, and can be up to 1.5 m in length. Needlefish are carnivorous and generally school in surface waters. When disturbed, excited or attracted by light, needlefish can leap out of the water at high speeds of up to 60 km/h and inadvertently impale objects or persons in their ‘flight’ path, including outrigger canoes.3 The beak is capable of causing deep penetrating injuries, and parts of the beak or teeth may break off inside the victim’s body.
The majority of reported needlefish injuries have occurred in Oceania3,4 including Hawaii,5 but cases have also been reported in the medical literature from Japan,6 Sri Lanka,7 Middle East,8,9 Mediterranean10 and the Atlantic USA.11 Most victims of needlefish injuries have been fishermen, swimmers, divers, canoeists and windsurfers.4,11 Those involved in night-time activities in the ocean (e.g. night fishing, spear fishing with spotlights) are at particularly high risk because needlefish are attracted by and leap towards bright lights.3
Needlefish injuries are nevertheless rare, and even more rarely life threatening. The majority of reported penetrating injuries are to the extremities, chest, and abdomen, but do including life-threatening reports of haemoperitoneum from a punctured liver and a perforated bowel.5 There have been two reported fatalities related to head injuries; a 10-year-old Hawaiian boy who was struck in the head by a needlefish while fishing with his father and died from a carotid cavernous fistula,12 and a 41-year-old diver in Sri Lanka who developed a massive and fatal middle cerebral artery infarction from his injury.7 Other reports of serious and unusual head and neck injuries include penetrating orbital injury,6,13 ruptured orbital globe,14 tympanic membrane rupture,8 penetrating injury to the maxilla10 and penetrating injury to the neck.9
Our case report highlights that penetrating needlefish injuries with retained foreign bodies might not always be apparent on external physical examination, and corroborates previous reports where the extent of internal injuries have not been reliably predicted from the seemingly insignificant external wounds.6,9,10 Despite a small external wound, the long narrow beak can cause significant internal damage far from the point of entry, and our patient was very fortunate that he escaped any serious or life-threatening injuries, given that the needlefish beak lodged within a few millimetres of his brain.
Our patient was also fortunate not to suffer any serious infection with a foreign body of marine origin lodged in his nasal cavity for over 3 months. As with all penetrating marine wounds, needlefish injuries are prone to infection,9,11 particularly with Vibrio species and other Gram-negative bacteria. Any wounds sustained in a marine environment should therefore be thoroughly irrigated and cleaned, and prophylactic antibiotics considered. A tetanus vaccine booster should also be given if required, and, as in our case, surgical removal of the foreign bodies may be required.4,6,9,10,13 The failure to make an accurate diagnosis following needlefish injuries can result in chronic and frustrating symptoms for the patient. We therefore recommend radiological examination in all suspected cases to identify any retained foreign bodies, and avoid preventable chronic sequelae including infection.
Funding
CLL is supported by an Australian National Health and Medical Research Council (NHMRC) Fellowship (1109035). No specific funding was received for preparing this article.
Conflict of interest: None declared.
References
Author notes
These authors contributed equally to this work.
Conference presentation: The article was presented as a poster at the 2015 Travel Medicine Alliance Annual Meeting, held in Brisbane, Australia.