-
PDF
- Split View
-
Views
-
Cite
Cite
Heidi A. Ojha, Rachel S. Snyder, Todd E. Davenport, Direct Access Compared With Referred Physical Therapy Episodes of Care: A Systematic Review, Physical Therapy, Volume 94, Issue 1, 1 January 2014, Pages 14–30, https://doi.org/10.2522/ptj.20130096
Close - Share Icon Share
Evidence suggests that physical therapy through direct access may help decrease costs and improve patient outcomes compared with physical therapy by physician referral.
The purpose of this study was to conduct a systematic review of the literature on patients with musculoskeletal injuries and compare health care costs and patient outcomes in episodes of physical therapy by direct access compared with referred physical therapy.
Ovid MEDLINE, CINAHL (EBSCO), Web of Science, and PEDro were searched using terms related to physical therapy and direct access. Included articles were hand searched for additional references.
Included studies compared data from physical therapy by direct access with physical therapy by physician referral, studying cost, outcomes, or harm. The studies were appraised using the Centre for Evidence-Based Medicine (CEBM) levels of evidence criteria and assigned a methodological score.
Of the 1,501 articles that were screened, 8 articles at levels 3 to 4 on the CEBM scale were included. There were statistically significant and clinically meaningful findings across studies that satisfaction and outcomes were superior, and numbers of physical therapy visits, imaging ordered, medications prescribed, and additional non–physical therapy appointments were less in cohorts receiving physical therapy by direct access compared with referred episodes of care. There was no evidence for harm.
There is evidence across level 3 and 4 studies (grade B to C CEBM level of recommendation) that physical therapy by direct access compared with referred episodes of care is associated with improved patient outcomes and decreased costs.
Primary limitations were lack of group randomization, potential for selection bias, and limited generalizability.
Physical therapy by way of direct access may contain health care costs and promote high-quality health care. Third-party payers should consider paying for physical therapy by direct access to decrease health care costs and incentivize optimal patient outcomes.
An estimated 53.9 million people in the United States report having 1 or more musculoskeletal disorders, with per capita medical expenditures averaging more than $3,578.1 As musculoskeletal conditions represent some of the leading causes of restricted activity days,2 many of these individuals seek care from or are referred to a physical therapist. In 2007, Americans of all ages had more than 164 million ambulatory visits for physical therapy.3
Individuals typically seek physical therapy services through either direct access or physician referral. The term direct access, in this report, will be defined as patients seeking physical therapy care directly without first seeing a physician or physician assistant to receive a script or referral for physical therapy services. Some studies have suggested that early or direct access to physical therapy can reduce waiting time, improve convenience, reduce costs for the patient and health care system, and improve recovery time.4–6 The results of these studies directly support recent health care reform efforts in which legislators and health care providers have sought to provide efficient care through cost reduction and optimizing patient outcomes.
In response to the growing literature supporting physical therapy's role in primary care, 47 out of 50 states (United States) currently have legislation that provides for some form of direct access to physical therapy. However, various barriers prevent physical therapists from practicing in a direct access capacity. Many of these 47 states limit direct access to certain physical therapists' qualifications, specialty areas, or condition/diagnostic codes. Furthermore, physical therapists may require referrals from medical providers due to legal constraints, third-party payer requirements for reimbursement, and hospital bylaws. Finally, there is a lack of public awareness and autonomous health-seeking behavior among consumers.7 Consequently, even though most physical therapists have direct access privileges through their state practice acts, the large majority of patients are still managed through episodes of care that are initiated by physician referral.
Despite the growing body of scientific literature in support of consumer direct access to physical therapy, the only systematic review that, in part, evaluated the impact of physician referral versus direct access on outcomes and costs was published in 1997 by Robert and Stevens.4 The review4 found that the main advantages for direct referral to physical therapy were significant reductions in waiting times, convenience, and reduced costs for the patient. However, there was little evidence in the published literature at that time to make conclusions about recovery time, outcomes, or cost to the health system. There have been a number of articles published since the mid-1990's on this topic,8–15 and we are unaware of any recent reviews published on this topic.
The purpose of this study was to establish the effects of direct access and physician-referred episodes of care in individuals receiving physical therapy based on a systematic review of peer-reviewed literature. Published data regarding clinical outcomes, practice patterns, utilization, and economic data were used to characterize the effects of direct access versus physician-referred episodes of care. We hypothesized that policies permitting patients to seek physical therapy directly would result in decreased health care costs and similar patient outcomes. We also hypothesized that there would be no evidence of increased harm related to direct access compared with physician-referred episodes of physical therapy. The relevance of a systematic review at this time is that additional scientific weight can be provided to guide the physical therapist's role in health care reform and serve as a concise report to improve the ability of consumers, legislators, hospital administrators, and third-party payers to synthesize the existing literature and make conclusions regarding the quality and cost-effectiveness of primary access physical therapy.
Method
Data Sources and Searches
Databases of CINAHL (EBSCO) (restricted to humans, January 1990–July 2013), Web of Science (restricted to articles, 1990 and later), and PEDro (1990 and later) were searched last on July 5, 2013. Limits were not placed on language when conducting all searches because we did not want to exclude articles written in the Spanish language, one author's second language. All searches were restricted to 1990 to present because we wanted to specifically focus on more recently published literature to improve generalizability of results, reflecting changes in modern practice patterns and updated interpretations of the search terms “direct access” and “open access.” We searched the databases using combinations of the key words “direct access,” “primary care,” “physical therapy,” “physiotherapy,” and “open access.” In addition to these key words, we searched Ovid MEDLINE (1990 and later) using a comprehensive list of Medical Subject Headings (MeSH) terms related to our topic. The full electronic search strategy and results for the Ovid MEDLINE database are listed in Table 1 as an example of the searches performed in this review.
Examples of Search Words and Medical Subject Headings (MeSH) Terms Used in Ovid MEDLINE
| Search Word/MeSH Term (1990 to Present) . | No. of Articles Located . |
|---|---|
| Physical Therapy Modalities AND Family Practice | 120 |
| Physical Therapy Modalities AND Referral and Consultation | 200 |
| Physical Therapy Modalities AND Musculoskeletal Diseases | 315 |
| Professional Competence AND Physical Therapy Specialty | 66 |
| Community Health Centers (Organization and Administration) AND Referral and Consultation | 103 |
| Family Practice AND Physical Therapy Department, Hospital | 2 |
| Outpatient Clinics, Hospital (Utilization) AND Referral and Consultation | 190 |
| Physical Therapy Modalities AND Delivery of Health Care | 77 |
| Physical Therapy Modalities AND Primary Health Care | 150 |
| Total no. of articles located in database | 1,223 |
| Search Word/MeSH Term (1990 to Present) . | No. of Articles Located . |
|---|---|
| Physical Therapy Modalities AND Family Practice | 120 |
| Physical Therapy Modalities AND Referral and Consultation | 200 |
| Physical Therapy Modalities AND Musculoskeletal Diseases | 315 |
| Professional Competence AND Physical Therapy Specialty | 66 |
| Community Health Centers (Organization and Administration) AND Referral and Consultation | 103 |
| Family Practice AND Physical Therapy Department, Hospital | 2 |
| Outpatient Clinics, Hospital (Utilization) AND Referral and Consultation | 190 |
| Physical Therapy Modalities AND Delivery of Health Care | 77 |
| Physical Therapy Modalities AND Primary Health Care | 150 |
| Total no. of articles located in database | 1,223 |
Examples of Search Words and Medical Subject Headings (MeSH) Terms Used in Ovid MEDLINE
| Search Word/MeSH Term (1990 to Present) . | No. of Articles Located . |
|---|---|
| Physical Therapy Modalities AND Family Practice | 120 |
| Physical Therapy Modalities AND Referral and Consultation | 200 |
| Physical Therapy Modalities AND Musculoskeletal Diseases | 315 |
| Professional Competence AND Physical Therapy Specialty | 66 |
| Community Health Centers (Organization and Administration) AND Referral and Consultation | 103 |
| Family Practice AND Physical Therapy Department, Hospital | 2 |
| Outpatient Clinics, Hospital (Utilization) AND Referral and Consultation | 190 |
| Physical Therapy Modalities AND Delivery of Health Care | 77 |
| Physical Therapy Modalities AND Primary Health Care | 150 |
| Total no. of articles located in database | 1,223 |
| Search Word/MeSH Term (1990 to Present) . | No. of Articles Located . |
|---|---|
| Physical Therapy Modalities AND Family Practice | 120 |
| Physical Therapy Modalities AND Referral and Consultation | 200 |
| Physical Therapy Modalities AND Musculoskeletal Diseases | 315 |
| Professional Competence AND Physical Therapy Specialty | 66 |
| Community Health Centers (Organization and Administration) AND Referral and Consultation | 103 |
| Family Practice AND Physical Therapy Department, Hospital | 2 |
| Outpatient Clinics, Hospital (Utilization) AND Referral and Consultation | 190 |
| Physical Therapy Modalities AND Delivery of Health Care | 77 |
| Physical Therapy Modalities AND Primary Health Care | 150 |
| Total no. of articles located in database | 1,223 |
Study Selection
Studies had to satisfy all of the following criteria to be included in this review: (1) included patients with greater than 85% musculoskeletal injuries treated by a physical therapist in an outpatient setting, (2) included original quantitative data of at least one group that received physical therapy through direct access or direct allocation to a physical therapist without seeing a physician, (3) included original quantitative data for at least one group that received physical therapy through physician referral, (4) greater than 50% of the patients in both groups had to have received physical therapy, and (5) included assessment of at least one of the following: outcomes of physical therapy (improvement or harm), cost, or outcome measures that would affect cost or outcomes (use of imaging, pharmacological interventions, consultant appointments, and patient satisfaction). Among all articles read in full text, studies were excluded if they were written in a language that the authors did not speak (all languages except English and Spanish).
Data Extraction
Titles and abstracts were screened by the authors (H.A.O. and T.E.D.). Full texts were obtained for any article that could not be ruled out based on the specified inclusion criteria. The Figure lists our search strategy, also referenced in the “Results” section of the article. The primary characteristics were extracted from each study. Results of the direct access and physician referral groups from each study were extracted for outcomes of interest at all time frames (most studies collected outcomes during the course of physical therapy, at discharge, or both). These outcomes of interest were: cost-effectiveness, number of physical therapy visits, discharge outcomes, imaging use, medication use, patient or physician satisfaction, number of additional referrals, additional care sought, or evidence of harm to the patient, physical therapist, or facility. Because of the conceptual heterogeneity in dependent variable measurements and lack of reports of variability around point estimates, we were unable to pool data and calculate effect sizes. Therefore, means or differences between means were listed for each outcome measure extracted, and standard deviations and ranges were reported as available (if not reported, the study did not report the information).
The flowchart outlines the search strategy. Because of the conceptual heterogeneity in dependent variable measurements and lack of reports of variability around point estimates, we were unable to pool data and calculate effect sizes.
Quality Assessment
The validity of studies using a between-group comparison was evaluated by 2 authors not blinded to authors or journals. We used the Oxford 2011 Centre of Evidence-Based Medicine (CEBM) recommendations to rate each article's level of evidence16 and the Downs and Black checklist17 to assign a methodological quality score to each article because all of our included studies were nonrandomized. See Table 2 and Appendix 1 for descriptions of the CEBM levels of evidence and Downs and Black checklist criteria. The level of evidence was determined across studies for the purpose of assigning a grade of recommendation to synthesize results; however, level of evidence was not utilized as an exclusion criterion due to the limited number of articles that met our defined criteria.
Study Characteristics and Results of Included Studiesa
| Study and Country . | Quality . | Sample Size . | Group Statisticsb . | Cost . | Physical Therapy Visitsc. . | Imaging Ordered . | Pharmacological Treatment . | Appointments . | Patient Satisfaction . | DC Outcomes or Harm . |
|---|---|---|---|---|---|---|---|---|---|---|
| Hackett et al,15 1993 United Kingdom | CEBMd 3 D&B 13/26 | Two rural practices, ~42% spinal injuries, the rest extremity injuries(> 95% msk) Insurance: NHS I: n=85 C: n=133 | I: open access | Mean cost to pts=£9.55($14.83) | |$\bar{X}$|=7.2 | 5.1% referred for imaging | 48% received prescription medications | 2.3% had GP consultations, 2.5% referred to specialists | 93.2% satisfiedf | Days of work missed due to dx=10.4 |
| C: referred by orthopedic consultants | Mean cost to pts=£47.94($74.48) | |$\bar{X}$|=7.0 | 13.6% referred for imaging | 84% received prescription prescription | 1.5% had GP consultations, 8.2% referred to specialists | 84.1% satisfiedf | Days of work missed due to dx=27.9 | |||
| Statistics | P<.01 (95% CI= £12.41, £63.65) | NS | P NR | P<.001e | P NR | P<.01e | P NR | |||
| Holdsworth and Webster,12 2004 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices, Insurance: NHS I: n=76 C: n=264 | I: self-referrals | Fewer physical therapy visits | Fewer GP contacts 3 mo after physical therapy | VAS score decreased from 5.7 (SD=2.3) to 2.7 (SD=1.7) 78% achieved goals 79% completed thee course of physical therapy | ||||
| C: GP referral groupg | More Physical therapy visits | More GP contacts 3 mo after physical therapy | VAS score decreased from 5.7 (SD=2.2) to 3.2 (SD=1.6) 63% achieved goals 60% completed their course of physical therapy | |||||||
| Statistics | P=.038 | P=.0113 | VAS P=.011, Goals achieved NS, P=.079 Course completed P=.004 | |||||||
| Holdsworth et al,13 2007 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices throughout Scotland Insurance: NHS I: n=648 C: n=1,795 | I: self-referrals n=648 | Average cost per episode of care £66.31 (£136.02) | |$\bar{X}$|=4.6 (range= 1–22) | Radiographs=4.00 | 32.2% received medicationsh | 18% visited GP on more than one occasion | 67% achieved goals | |
| C:GP referral group g n=1,795 | Average cost per episode of care £88.99 (£138.26) | |$\bar{X}$|=4.6 (range= 1–22) | Radiographs=7.43 | 44.1% received medicationsh | 39% visited GP on more than one occasion | 65% achieved goals | ||||
| Statistics | NR | NS | P<.01 | P<.0001 | P<.001 | NS, P=.82 | ||||
| Webster et al,14 2008 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices Insurance: NHS I: n=648 C: n=1,795 | I: self-referrals | 17% contacting GP 1 mo after DC | Satisfied i=79% | |||||
| C: GP referral group | 19% contacting GP 1 mo after DC | Satisfied i=74% | ||||||||
| Statistics | NS, P=.219 | P<.001 | ||||||||
| Mitchell and de Lissovoy,91997 United States | CEBM 3 D&B 18/26 | Acute/sporadic msk- related disorders, adults aged <65 y and their children, BCBS I: n=252 C: n=353 | l: direct access | $1,004 paid claims per episode of carei | X̅=20.2 | Radiology claims 0.32 | Drug claims 1.47 | Mean hospital admits 0.25 | ||
| C: physician referral | $2,236 paid claims per episode of carej | X̅=33.6 | Radiology claims 1.02 | Drug claims 3.13 | Mean hospital admits 0.64 | |||||
| Statistics | P<.001 | P<.0001 | P<.01 | P<.01 | P<.01 | |||||
| Leemrijse et al,8 2008 The Netherlands | CEBM 4 D&B 22/26 | PTs at private practices listed in a database: specialist PTs (ei Peds) excluded I: n=2977 C: n=7,533 | I: direct access | X̅=8.1 (SD=6.6) | Goals fully achieved at DC, 850 (72.6%) | |||||
| C: physician referral | X̅=10.5 (SD=8.9) | 2,102 (63.3%) | ||||||||
| Statistics | P<.001 | P<.001 | ||||||||
| Moore et al,10 2005 United States | CEBM 4 D&B 13/26 | Military patents seen by PTs;dx msk dx I:n=50,799 C: n=421,219 | I: direct access | No harmk | ||||||
| C: PTs via referral | No harmk | |||||||||
| Statistics | PNR | |||||||||
| Pendergast et a1,11 2012 United States | CEBM 4 D&B 22/26 | Adults (18–64 y) treated in outpatient clinics (private or hospital based) on private (BCBS) at least 87% msk l: n=17,497 C: n=45,210 | I: self-referred | Mean allowable amounts: PT=$503.12 (SD=$478.18), non-PT=$526.26 (SD=$1,448.95) | X̅=5.90 (SD=5.55) | |||||
| C: physician referral | Mean allowable amounts: PT=$605.49 (SD=$549.61), non-PT=$678.64 (SD=$1,744.11) | X̅=7.00 (SD=6.09) | ||||||||
| Statistics | Both P<.001 | P<.001 |
| Study and Country . | Quality . | Sample Size . | Group Statisticsb . | Cost . | Physical Therapy Visitsc. . | Imaging Ordered . | Pharmacological Treatment . | Appointments . | Patient Satisfaction . | DC Outcomes or Harm . |
|---|---|---|---|---|---|---|---|---|---|---|
| Hackett et al,15 1993 United Kingdom | CEBMd 3 D&B 13/26 | Two rural practices, ~42% spinal injuries, the rest extremity injuries(> 95% msk) Insurance: NHS I: n=85 C: n=133 | I: open access | Mean cost to pts=£9.55($14.83) | |$\bar{X}$|=7.2 | 5.1% referred for imaging | 48% received prescription medications | 2.3% had GP consultations, 2.5% referred to specialists | 93.2% satisfiedf | Days of work missed due to dx=10.4 |
| C: referred by orthopedic consultants | Mean cost to pts=£47.94($74.48) | |$\bar{X}$|=7.0 | 13.6% referred for imaging | 84% received prescription prescription | 1.5% had GP consultations, 8.2% referred to specialists | 84.1% satisfiedf | Days of work missed due to dx=27.9 | |||
| Statistics | P<.01 (95% CI= £12.41, £63.65) | NS | P NR | P<.001e | P NR | P<.01e | P NR | |||
| Holdsworth and Webster,12 2004 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices, Insurance: NHS I: n=76 C: n=264 | I: self-referrals | Fewer physical therapy visits | Fewer GP contacts 3 mo after physical therapy | VAS score decreased from 5.7 (SD=2.3) to 2.7 (SD=1.7) 78% achieved goals 79% completed thee course of physical therapy | ||||
| C: GP referral groupg | More Physical therapy visits | More GP contacts 3 mo after physical therapy | VAS score decreased from 5.7 (SD=2.2) to 3.2 (SD=1.6) 63% achieved goals 60% completed their course of physical therapy | |||||||
| Statistics | P=.038 | P=.0113 | VAS P=.011, Goals achieved NS, P=.079 Course completed P=.004 | |||||||
| Holdsworth et al,13 2007 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices throughout Scotland Insurance: NHS I: n=648 C: n=1,795 | I: self-referrals n=648 | Average cost per episode of care £66.31 (£136.02) | |$\bar{X}$|=4.6 (range= 1–22) | Radiographs=4.00 | 32.2% received medicationsh | 18% visited GP on more than one occasion | 67% achieved goals | |
| C:GP referral group g n=1,795 | Average cost per episode of care £88.99 (£138.26) | |$\bar{X}$|=4.6 (range= 1–22) | Radiographs=7.43 | 44.1% received medicationsh | 39% visited GP on more than one occasion | 65% achieved goals | ||||
| Statistics | NR | NS | P<.01 | P<.0001 | P<.001 | NS, P=.82 | ||||
| Webster et al,14 2008 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices Insurance: NHS I: n=648 C: n=1,795 | I: self-referrals | 17% contacting GP 1 mo after DC | Satisfied i=79% | |||||
| C: GP referral group | 19% contacting GP 1 mo after DC | Satisfied i=74% | ||||||||
| Statistics | NS, P=.219 | P<.001 | ||||||||
| Mitchell and de Lissovoy,91997 United States | CEBM 3 D&B 18/26 | Acute/sporadic msk- related disorders, adults aged <65 y and their children, BCBS I: n=252 C: n=353 | l: direct access | $1,004 paid claims per episode of carei | X̅=20.2 | Radiology claims 0.32 | Drug claims 1.47 | Mean hospital admits 0.25 | ||
| C: physician referral | $2,236 paid claims per episode of carej | X̅=33.6 | Radiology claims 1.02 | Drug claims 3.13 | Mean hospital admits 0.64 | |||||
| Statistics | P<.001 | P<.0001 | P<.01 | P<.01 | P<.01 | |||||
| Leemrijse et al,8 2008 The Netherlands | CEBM 4 D&B 22/26 | PTs at private practices listed in a database: specialist PTs (ei Peds) excluded I: n=2977 C: n=7,533 | I: direct access | X̅=8.1 (SD=6.6) | Goals fully achieved at DC, 850 (72.6%) | |||||
| C: physician referral | X̅=10.5 (SD=8.9) | 2,102 (63.3%) | ||||||||
| Statistics | P<.001 | P<.001 | ||||||||
| Moore et al,10 2005 United States | CEBM 4 D&B 13/26 | Military patents seen by PTs;dx msk dx I:n=50,799 C: n=421,219 | I: direct access | No harmk | ||||||
| C: PTs via referral | No harmk | |||||||||
| Statistics | PNR | |||||||||
| Pendergast et a1,11 2012 United States | CEBM 4 D&B 22/26 | Adults (18–64 y) treated in outpatient clinics (private or hospital based) on private (BCBS) at least 87% msk l: n=17,497 C: n=45,210 | I: self-referred | Mean allowable amounts: PT=$503.12 (SD=$478.18), non-PT=$526.26 (SD=$1,448.95) | X̅=5.90 (SD=5.55) | |||||
| C: physician referral | Mean allowable amounts: PT=$605.49 (SD=$549.61), non-PT=$678.64 (SD=$1,744.11) | X̅=7.00 (SD=6.09) | ||||||||
| Statistics | Both P<.001 | P<.001 |
I=intervention group, C=comparison group, D&B=Downs and Black checlist (see Appendix 1 for criteria), NH =National Health Service, BCBS=Blue Cross Blue Shield, pts=patients, CEBM=Centre for Evidence- Based Medicine, dx=diagnosis, DC=discharge, PT=physical therapist, msk=musculoskeletal, peds=pediatrics, 95% CI=95% confidence interval, GP-general practitioner, NR=not reported, NS=not significant.
Statistical difference between I and C groups.
Physical therapy visits per episode of care (mean across all patients).
Levels of evidence are based on the Oxford 2011 CEBM levels of evidence: level 1=systematic review of randomized trials or n=1 trial; level 2=randomized trial or observational study with dramatic effect; level 3=nonrandomized controlled cohort/follow-up study; level 4=case-series, case-control, or historically controlled studies; level 5=mechanism-based reasoning.
P value includes practice A (physician owned) + practice B (direct access) vs practice C (referral); 95% C1=26.1% to 44.0%.
Evaluated management of their condition as average or above.
GP-suggested referral group results excluded.
Medications=nonsteroidal anti-inflammatory drugs and analgesics.
Percent satisfied=percent satisfied or very satisfied.
Paid claims for all services/drugs per episode of care.
No adverse events resulting from PT dx or management, no state licenses modified or revoked for disciplinary action, no litigation cases filed against US government
Study Characteristics and Results of Included Studiesa
| Study and Country . | Quality . | Sample Size . | Group Statisticsb . | Cost . | Physical Therapy Visitsc. . | Imaging Ordered . | Pharmacological Treatment . | Appointments . | Patient Satisfaction . | DC Outcomes or Harm . |
|---|---|---|---|---|---|---|---|---|---|---|
| Hackett et al,15 1993 United Kingdom | CEBMd 3 D&B 13/26 | Two rural practices, ~42% spinal injuries, the rest extremity injuries(> 95% msk) Insurance: NHS I: n=85 C: n=133 | I: open access | Mean cost to pts=£9.55($14.83) | |$\bar{X}$|=7.2 | 5.1% referred for imaging | 48% received prescription medications | 2.3% had GP consultations, 2.5% referred to specialists | 93.2% satisfiedf | Days of work missed due to dx=10.4 |
| C: referred by orthopedic consultants | Mean cost to pts=£47.94($74.48) | |$\bar{X}$|=7.0 | 13.6% referred for imaging | 84% received prescription prescription | 1.5% had GP consultations, 8.2% referred to specialists | 84.1% satisfiedf | Days of work missed due to dx=27.9 | |||
| Statistics | P<.01 (95% CI= £12.41, £63.65) | NS | P NR | P<.001e | P NR | P<.01e | P NR | |||
| Holdsworth and Webster,12 2004 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices, Insurance: NHS I: n=76 C: n=264 | I: self-referrals | Fewer physical therapy visits | Fewer GP contacts 3 mo after physical therapy | VAS score decreased from 5.7 (SD=2.3) to 2.7 (SD=1.7) 78% achieved goals 79% completed thee course of physical therapy | ||||
| C: GP referral groupg | More Physical therapy visits | More GP contacts 3 mo after physical therapy | VAS score decreased from 5.7 (SD=2.2) to 3.2 (SD=1.6) 63% achieved goals 60% completed their course of physical therapy | |||||||
| Statistics | P=.038 | P=.0113 | VAS P=.011, Goals achieved NS, P=.079 Course completed P=.004 | |||||||
| Holdsworth et al,13 2007 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices throughout Scotland Insurance: NHS I: n=648 C: n=1,795 | I: self-referrals n=648 | Average cost per episode of care £66.31 (£136.02) | |$\bar{X}$|=4.6 (range= 1–22) | Radiographs=4.00 | 32.2% received medicationsh | 18% visited GP on more than one occasion | 67% achieved goals | |
| C:GP referral group g n=1,795 | Average cost per episode of care £88.99 (£138.26) | |$\bar{X}$|=4.6 (range= 1–22) | Radiographs=7.43 | 44.1% received medicationsh | 39% visited GP on more than one occasion | 65% achieved goals | ||||
| Statistics | NR | NS | P<.01 | P<.0001 | P<.001 | NS, P=.82 | ||||
| Webster et al,14 2008 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices Insurance: NHS I: n=648 C: n=1,795 | I: self-referrals | 17% contacting GP 1 mo after DC | Satisfied i=79% | |||||
| C: GP referral group | 19% contacting GP 1 mo after DC | Satisfied i=74% | ||||||||
| Statistics | NS, P=.219 | P<.001 | ||||||||
| Mitchell and de Lissovoy,91997 United States | CEBM 3 D&B 18/26 | Acute/sporadic msk- related disorders, adults aged <65 y and their children, BCBS I: n=252 C: n=353 | l: direct access | $1,004 paid claims per episode of carei | X̅=20.2 | Radiology claims 0.32 | Drug claims 1.47 | Mean hospital admits 0.25 | ||
| C: physician referral | $2,236 paid claims per episode of carej | X̅=33.6 | Radiology claims 1.02 | Drug claims 3.13 | Mean hospital admits 0.64 | |||||
| Statistics | P<.001 | P<.0001 | P<.01 | P<.01 | P<.01 | |||||
| Leemrijse et al,8 2008 The Netherlands | CEBM 4 D&B 22/26 | PTs at private practices listed in a database: specialist PTs (ei Peds) excluded I: n=2977 C: n=7,533 | I: direct access | X̅=8.1 (SD=6.6) | Goals fully achieved at DC, 850 (72.6%) | |||||
| C: physician referral | X̅=10.5 (SD=8.9) | 2,102 (63.3%) | ||||||||
| Statistics | P<.001 | P<.001 | ||||||||
| Moore et al,10 2005 United States | CEBM 4 D&B 13/26 | Military patents seen by PTs;dx msk dx I:n=50,799 C: n=421,219 | I: direct access | No harmk | ||||||
| C: PTs via referral | No harmk | |||||||||
| Statistics | PNR | |||||||||
| Pendergast et a1,11 2012 United States | CEBM 4 D&B 22/26 | Adults (18–64 y) treated in outpatient clinics (private or hospital based) on private (BCBS) at least 87% msk l: n=17,497 C: n=45,210 | I: self-referred | Mean allowable amounts: PT=$503.12 (SD=$478.18), non-PT=$526.26 (SD=$1,448.95) | X̅=5.90 (SD=5.55) | |||||
| C: physician referral | Mean allowable amounts: PT=$605.49 (SD=$549.61), non-PT=$678.64 (SD=$1,744.11) | X̅=7.00 (SD=6.09) | ||||||||
| Statistics | Both P<.001 | P<.001 |
| Study and Country . | Quality . | Sample Size . | Group Statisticsb . | Cost . | Physical Therapy Visitsc. . | Imaging Ordered . | Pharmacological Treatment . | Appointments . | Patient Satisfaction . | DC Outcomes or Harm . |
|---|---|---|---|---|---|---|---|---|---|---|
| Hackett et al,15 1993 United Kingdom | CEBMd 3 D&B 13/26 | Two rural practices, ~42% spinal injuries, the rest extremity injuries(> 95% msk) Insurance: NHS I: n=85 C: n=133 | I: open access | Mean cost to pts=£9.55($14.83) | |$\bar{X}$|=7.2 | 5.1% referred for imaging | 48% received prescription medications | 2.3% had GP consultations, 2.5% referred to specialists | 93.2% satisfiedf | Days of work missed due to dx=10.4 |
| C: referred by orthopedic consultants | Mean cost to pts=£47.94($74.48) | |$\bar{X}$|=7.0 | 13.6% referred for imaging | 84% received prescription prescription | 1.5% had GP consultations, 8.2% referred to specialists | 84.1% satisfiedf | Days of work missed due to dx=27.9 | |||
| Statistics | P<.01 (95% CI= £12.41, £63.65) | NS | P NR | P<.001e | P NR | P<.01e | P NR | |||
| Holdsworth and Webster,12 2004 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices, Insurance: NHS I: n=76 C: n=264 | I: self-referrals | Fewer physical therapy visits | Fewer GP contacts 3 mo after physical therapy | VAS score decreased from 5.7 (SD=2.3) to 2.7 (SD=1.7) 78% achieved goals 79% completed thee course of physical therapy | ||||
| C: GP referral groupg | More Physical therapy visits | More GP contacts 3 mo after physical therapy | VAS score decreased from 5.7 (SD=2.2) to 3.2 (SD=1.6) 63% achieved goals 60% completed their course of physical therapy | |||||||
| Statistics | P=.038 | P=.0113 | VAS P=.011, Goals achieved NS, P=.079 Course completed P=.004 | |||||||
| Holdsworth et al,13 2007 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices throughout Scotland Insurance: NHS I: n=648 C: n=1,795 | I: self-referrals n=648 | Average cost per episode of care £66.31 (£136.02) | |$\bar{X}$|=4.6 (range= 1–22) | Radiographs=4.00 | 32.2% received medicationsh | 18% visited GP on more than one occasion | 67% achieved goals | |
| C:GP referral group g n=1,795 | Average cost per episode of care £88.99 (£138.26) | |$\bar{X}$|=4.6 (range= 1–22) | Radiographs=7.43 | 44.1% received medicationsh | 39% visited GP on more than one occasion | 65% achieved goals | ||||
| Statistics | NR | NS | P<.01 | P<.0001 | P<.001 | NS, P=.82 | ||||
| Webster et al,14 2008 Scotland | CEBM 3 D&B 16/26 | Pts with msk injuries from 26 general practices Insurance: NHS I: n=648 C: n=1,795 | I: self-referrals | 17% contacting GP 1 mo after DC | Satisfied i=79% | |||||
| C: GP referral group | 19% contacting GP 1 mo after DC | Satisfied i=74% | ||||||||
| Statistics | NS, P=.219 | P<.001 | ||||||||
| Mitchell and de Lissovoy,91997 United States | CEBM 3 D&B 18/26 | Acute/sporadic msk- related disorders, adults aged <65 y and their children, BCBS I: n=252 C: n=353 | l: direct access | $1,004 paid claims per episode of carei | X̅=20.2 | Radiology claims 0.32 | Drug claims 1.47 | Mean hospital admits 0.25 | ||
| C: physician referral | $2,236 paid claims per episode of carej | X̅=33.6 | Radiology claims 1.02 | Drug claims 3.13 | Mean hospital admits 0.64 | |||||
| Statistics | P<.001 | P<.0001 | P<.01 | P<.01 | P<.01 | |||||
| Leemrijse et al,8 2008 The Netherlands | CEBM 4 D&B 22/26 | PTs at private practices listed in a database: specialist PTs (ei Peds) excluded I: n=2977 C: n=7,533 | I: direct access | X̅=8.1 (SD=6.6) | Goals fully achieved at DC, 850 (72.6%) | |||||
| C: physician referral | X̅=10.5 (SD=8.9) | 2,102 (63.3%) | ||||||||
| Statistics | P<.001 | P<.001 | ||||||||
| Moore et al,10 2005 United States | CEBM 4 D&B 13/26 | Military patents seen by PTs;dx msk dx I:n=50,799 C: n=421,219 | I: direct access | No harmk | ||||||
| C: PTs via referral | No harmk | |||||||||
| Statistics | PNR | |||||||||
| Pendergast et a1,11 2012 United States | CEBM 4 D&B 22/26 | Adults (18–64 y) treated in outpatient clinics (private or hospital based) on private (BCBS) at least 87% msk l: n=17,497 C: n=45,210 | I: self-referred | Mean allowable amounts: PT=$503.12 (SD=$478.18), non-PT=$526.26 (SD=$1,448.95) | X̅=5.90 (SD=5.55) | |||||
| C: physician referral | Mean allowable amounts: PT=$605.49 (SD=$549.61), non-PT=$678.64 (SD=$1,744.11) | X̅=7.00 (SD=6.09) | ||||||||
| Statistics | Both P<.001 | P<.001 |
I=intervention group, C=comparison group, D&B=Downs and Black checlist (see Appendix 1 for criteria), NH =National Health Service, BCBS=Blue Cross Blue Shield, pts=patients, CEBM=Centre for Evidence- Based Medicine, dx=diagnosis, DC=discharge, PT=physical therapist, msk=musculoskeletal, peds=pediatrics, 95% CI=95% confidence interval, GP-general practitioner, NR=not reported, NS=not significant.
Statistical difference between I and C groups.
Physical therapy visits per episode of care (mean across all patients).
Levels of evidence are based on the Oxford 2011 CEBM levels of evidence: level 1=systematic review of randomized trials or n=1 trial; level 2=randomized trial or observational study with dramatic effect; level 3=nonrandomized controlled cohort/follow-up study; level 4=case-series, case-control, or historically controlled studies; level 5=mechanism-based reasoning.
P value includes practice A (physician owned) + practice B (direct access) vs practice C (referral); 95% C1=26.1% to 44.0%.
Evaluated management of their condition as average or above.
GP-suggested referral group results excluded.
Medications=nonsteroidal anti-inflammatory drugs and analgesics.
Percent satisfied=percent satisfied or very satisfied.
Paid claims for all services/drugs per episode of care.
No adverse events resulting from PT dx or management, no state licenses modified or revoked for disciplinary action, no litigation cases filed against US government
All studies were independently scored using a modification of the Downs and Black tool17 by 2 reviewers (H.A.O. and R.S.S.) who were blinded to each other's results. After scoring, any disagreements were resolved by discussion (T.E.D.). The Downs and Black checklist is a tool that can be used to assess the methodological quality of nonrandomized studies. We developed guidelines, specific to our study type, to improve agreement between raters ( Appendix 1). Reliability between reviewers' initial Downs and Black checklist scores was calculated using the kappa coefficient. Similar to other previously published reviews,18–20 the tool was slightly modified for use in our study by dropping 2 checklist items from our analysis. We decided that criterion 17 (“In trials and cohort studies, do the analyses adjust for different lengths of follow-up of patients, or, in case-control studies, is the time period between the intervention and outcome the same for cases and controls?”) was not a good evaluation of quality because the follow-up period in many studies was initial evaluation to discharge, which was influenced by one of our primary outcome measures (number of physical therapy visits). Criterion 27 (“Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is less than 5%?”) also was not scored because we consulted a statistician who believed that significance found should not be influenced by post hoc power analyses and a difference between groups is either significant or not at study end, regardless of how much power was assumed a priori.21 The maximum score on the scale was 26, as one item had a potential of 2 points and we omitted 2 criteria (Tab. 2).
Data Synthesis and Analysis
After assigning a level of evidence to each article according to the CEBM criteria, the data were synthesized by the primary author (H.A.O.), stratified by outcome measure utilizing grades of recommendation A to D according to the CEBM criteria (see Tab. 3 for a description of each grade of recommendation). If the majority of articles showed a statistically significant difference between groups, the results were considered consistent across studies for that outcome measure. Likewise, if half of the articles that reported on an outcome measure showed a significant difference and the other half did not reach significance, the results were considered inconsistent.
Data Synthesis
| Outcome Measure . | Summary . | CEBM Grade of Recommendationa . |
|---|---|---|
| Cost | One level 3 study and 2 level 4 studies showed significantly decreased cost in the direct access group vs the physician referral group; 1 study (level 3) did not report significance, but reported means show a large effect size | B |
| No. of physical therapy visits | 3 level 4 studies and 1 level 3 study showed significantly decreased visits in the direct access group vs the physician referral group; 2 studies (levels 2 and 3) showed no significant differences between groups | C |
| Pharmacological interventions | 3 studies (2 level 3 studies, 1 level 4 study) showed significantly more use of pharmacological interventions in the physician referral group vs the direct access group | B |
| Imaging ordered | All 3 studies (2 level 3 studies, 1 level 4 study) showed significantly increased imaging ordered in the physician referral group vs the direct access group | B |
| General practitioner, consultation services, or hospital admits | 2 studies (1 level 3 study, 1 level 4 study) showed significantly fewer GP visits after physical therapy discharge and significantly fewer hospital admissions during physical therapy care; 2 studies (both level 3) showed no difference between groups | D |
| Patient satisfaction | 2 studies (level 3) reported significantly greater satisfaction in the direct access group vs the physician referral group | B |
| Discharge outcomes (function/ goals) and harm | 3 studies (2 level 3 studies, 1 level 4 study) show improved discharge outcomes for direct access vs physician referral; 1 study (level 3) showed no difference 1 study showed no reports of harm in either group | C |
| Outcome Measure . | Summary . | CEBM Grade of Recommendationa . |
|---|---|---|
| Cost | One level 3 study and 2 level 4 studies showed significantly decreased cost in the direct access group vs the physician referral group; 1 study (level 3) did not report significance, but reported means show a large effect size | B |
| No. of physical therapy visits | 3 level 4 studies and 1 level 3 study showed significantly decreased visits in the direct access group vs the physician referral group; 2 studies (levels 2 and 3) showed no significant differences between groups | C |
| Pharmacological interventions | 3 studies (2 level 3 studies, 1 level 4 study) showed significantly more use of pharmacological interventions in the physician referral group vs the direct access group | B |
| Imaging ordered | All 3 studies (2 level 3 studies, 1 level 4 study) showed significantly increased imaging ordered in the physician referral group vs the direct access group | B |
| General practitioner, consultation services, or hospital admits | 2 studies (1 level 3 study, 1 level 4 study) showed significantly fewer GP visits after physical therapy discharge and significantly fewer hospital admissions during physical therapy care; 2 studies (both level 3) showed no difference between groups | D |
| Patient satisfaction | 2 studies (level 3) reported significantly greater satisfaction in the direct access group vs the physician referral group | B |
| Discharge outcomes (function/ goals) and harm | 3 studies (2 level 3 studies, 1 level 4 study) show improved discharge outcomes for direct access vs physician referral; 1 study (level 3) showed no difference 1 study showed no reports of harm in either group | C |
Description of grades of recommendation are according to the Centre for Evidence-Based Medicine criteria: A, consistent level 1 studies; B, consistent level 2 or 3 studies or extrapolations from level 1 studies; C, level 4 studies or extrapolations from level 2 or 3 studies; D, level 5 evidence or troublingly inconsistent or inconclusive studies of any level.
Data Synthesis
| Outcome Measure . | Summary . | CEBM Grade of Recommendationa . |
|---|---|---|
| Cost | One level 3 study and 2 level 4 studies showed significantly decreased cost in the direct access group vs the physician referral group; 1 study (level 3) did not report significance, but reported means show a large effect size | B |
| No. of physical therapy visits | 3 level 4 studies and 1 level 3 study showed significantly decreased visits in the direct access group vs the physician referral group; 2 studies (levels 2 and 3) showed no significant differences between groups | C |
| Pharmacological interventions | 3 studies (2 level 3 studies, 1 level 4 study) showed significantly more use of pharmacological interventions in the physician referral group vs the direct access group | B |
| Imaging ordered | All 3 studies (2 level 3 studies, 1 level 4 study) showed significantly increased imaging ordered in the physician referral group vs the direct access group | B |
| General practitioner, consultation services, or hospital admits | 2 studies (1 level 3 study, 1 level 4 study) showed significantly fewer GP visits after physical therapy discharge and significantly fewer hospital admissions during physical therapy care; 2 studies (both level 3) showed no difference between groups | D |
| Patient satisfaction | 2 studies (level 3) reported significantly greater satisfaction in the direct access group vs the physician referral group | B |
| Discharge outcomes (function/ goals) and harm | 3 studies (2 level 3 studies, 1 level 4 study) show improved discharge outcomes for direct access vs physician referral; 1 study (level 3) showed no difference 1 study showed no reports of harm in either group | C |
| Outcome Measure . | Summary . | CEBM Grade of Recommendationa . |
|---|---|---|
| Cost | One level 3 study and 2 level 4 studies showed significantly decreased cost in the direct access group vs the physician referral group; 1 study (level 3) did not report significance, but reported means show a large effect size | B |
| No. of physical therapy visits | 3 level 4 studies and 1 level 3 study showed significantly decreased visits in the direct access group vs the physician referral group; 2 studies (levels 2 and 3) showed no significant differences between groups | C |
| Pharmacological interventions | 3 studies (2 level 3 studies, 1 level 4 study) showed significantly more use of pharmacological interventions in the physician referral group vs the direct access group | B |
| Imaging ordered | All 3 studies (2 level 3 studies, 1 level 4 study) showed significantly increased imaging ordered in the physician referral group vs the direct access group | B |
| General practitioner, consultation services, or hospital admits | 2 studies (1 level 3 study, 1 level 4 study) showed significantly fewer GP visits after physical therapy discharge and significantly fewer hospital admissions during physical therapy care; 2 studies (both level 3) showed no difference between groups | D |
| Patient satisfaction | 2 studies (level 3) reported significantly greater satisfaction in the direct access group vs the physician referral group | B |
| Discharge outcomes (function/ goals) and harm | 3 studies (2 level 3 studies, 1 level 4 study) show improved discharge outcomes for direct access vs physician referral; 1 study (level 3) showed no difference 1 study showed no reports of harm in either group | C |
Description of grades of recommendation are according to the Centre for Evidence-Based Medicine criteria: A, consistent level 1 studies; B, consistent level 2 or 3 studies or extrapolations from level 1 studies; C, level 4 studies or extrapolations from level 2 or 3 studies; D, level 5 evidence or troublingly inconsistent or inconclusive studies of any level.
Results
Abstracts of initially identified articles (n=1,501) were screened for eligibility. The Figure displays our search strategy, and Table 1 lists the results of the Ovid/MEDLINE electronic search. There was one article22 that, from the title, seemed to meet our inclusion criteria; however, we were unable to obtain the abstract or full text to determine eligibility for inclusion, and no contact information was available for the authors. Accordingly, we were able to obtain 8 studies in full text that met our inclusion criteria. Two of the 8 included studies—Holdsworth et al13 and Webster et al14—investigated different outcomes from the same population and cohorts, so this review summarized the results from 7 datasets reported across the 8 included studies. The most common reasons for exclusion were lack of analysis on our outcomes of interest and no direct comparison of direct access and referral interventions, as specified in the “Method” section of the article.
Table 2 lists characteristics of each study included in this review and the level of evidence using the CEBM criteria (levels ranged from 3 to 4). None of the studies which met our criteria were randomized; 4 were nonrandomized prospective cohort studies, and 4 were nonrandomized retrospective cohort studies. The Downs and Black checklist scores are reported in Table 4 and ranged from 13 to 22 out of a total of 26 points. Interrater reliability for the Downs and Black checklist scoring (H.A.O. and R.S.S.) was kappa=.931 (P<.001; Cohen kappa±.025 standard error). Any differences in rating were resolved through consensus. Results were summarized qualitatively by outcome measures (included below) and are presented in further detail in Table 2. Data synthesis results are presented in Table 3.
Methodological Quality
| Study . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . | 11 . | 12 . | 13 . | 14 . | 15 . | 16 . | 17 . | 18 . | 19 . | 20 . | 21 . | 22 . | 23 . | 24 . | 25 . | 26 . | 27 . | D&B Scorea . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hackett et al,15 1993 | Y | N | Y | Y | P | Y | N | N | N | N | Y | Y | Y | U | U | Y | Y | N | Y | N | Y | N | N | Y | N | 13/26 | ||
| Holdsworth et a1,13 2007 | V | Y | Y | Y | N | Y | Y | N | N | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 18/26 | ||
| Holdsworth and Webster,12 2004 | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | N | Y | N | N | Y | Y | N | Y | Y | Y | N | N | N | N | 16/26 | ||
| Webster et a1,14 2008 | Y | Y | Y | Y | P | Y | Y | N | N | Y | N | N | Y | N | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 16/26 | ||
| Leemrijse et a1,8 2008 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 22/26 | ||
| Mitchell and de Lissovoy,9 1997 | Y | Y | Y | Y | N | Y | U | N | Y | N | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 18/26 | ||
| Pendergast et a1,112012 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 22/26 | ||
| Moore et al,10 2005 | Y | Y | N | Y | N | Y | Y | Y | N | N | U | U | Y | Y | N | Y | Y | U | Y | Y | Y | N | N | N | N | 13/26 |
| Study . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . | 11 . | 12 . | 13 . | 14 . | 15 . | 16 . | 17 . | 18 . | 19 . | 20 . | 21 . | 22 . | 23 . | 24 . | 25 . | 26 . | 27 . | D&B Scorea . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hackett et al,15 1993 | Y | N | Y | Y | P | Y | N | N | N | N | Y | Y | Y | U | U | Y | Y | N | Y | N | Y | N | N | Y | N | 13/26 | ||
| Holdsworth et a1,13 2007 | V | Y | Y | Y | N | Y | Y | N | N | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 18/26 | ||
| Holdsworth and Webster,12 2004 | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | N | Y | N | N | Y | Y | N | Y | Y | Y | N | N | N | N | 16/26 | ||
| Webster et a1,14 2008 | Y | Y | Y | Y | P | Y | Y | N | N | Y | N | N | Y | N | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 16/26 | ||
| Leemrijse et a1,8 2008 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 22/26 | ||
| Mitchell and de Lissovoy,9 1997 | Y | Y | Y | Y | N | Y | U | N | Y | N | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 18/26 | ||
| Pendergast et a1,112012 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 22/26 | ||
| Moore et al,10 2005 | Y | Y | N | Y | N | Y | Y | Y | N | N | U | U | Y | Y | N | Y | Y | U | Y | Y | Y | N | N | N | N | 13/26 |
Criteria are based on Downs and Black checklist (Appendix 1): Y (yes)=criterion met, N (no) =criterion not met P=criterion partially met, and U=criterion unable to determine from the study manuscript. Criterion 5 has a maximum of 2 points, and all other criteria have a maximum of 1 point. U ratings received zero points. Criteria 17 and 27 were omitted due to reasons explained in the “Quality Assessment” section.
Methodological Quality
| Study . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . | 11 . | 12 . | 13 . | 14 . | 15 . | 16 . | 17 . | 18 . | 19 . | 20 . | 21 . | 22 . | 23 . | 24 . | 25 . | 26 . | 27 . | D&B Scorea . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hackett et al,15 1993 | Y | N | Y | Y | P | Y | N | N | N | N | Y | Y | Y | U | U | Y | Y | N | Y | N | Y | N | N | Y | N | 13/26 | ||
| Holdsworth et a1,13 2007 | V | Y | Y | Y | N | Y | Y | N | N | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 18/26 | ||
| Holdsworth and Webster,12 2004 | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | N | Y | N | N | Y | Y | N | Y | Y | Y | N | N | N | N | 16/26 | ||
| Webster et a1,14 2008 | Y | Y | Y | Y | P | Y | Y | N | N | Y | N | N | Y | N | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 16/26 | ||
| Leemrijse et a1,8 2008 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 22/26 | ||
| Mitchell and de Lissovoy,9 1997 | Y | Y | Y | Y | N | Y | U | N | Y | N | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 18/26 | ||
| Pendergast et a1,112012 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 22/26 | ||
| Moore et al,10 2005 | Y | Y | N | Y | N | Y | Y | Y | N | N | U | U | Y | Y | N | Y | Y | U | Y | Y | Y | N | N | N | N | 13/26 |
| Study . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . | 11 . | 12 . | 13 . | 14 . | 15 . | 16 . | 17 . | 18 . | 19 . | 20 . | 21 . | 22 . | 23 . | 24 . | 25 . | 26 . | 27 . | D&B Scorea . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hackett et al,15 1993 | Y | N | Y | Y | P | Y | N | N | N | N | Y | Y | Y | U | U | Y | Y | N | Y | N | Y | N | N | Y | N | 13/26 | ||
| Holdsworth et a1,13 2007 | V | Y | Y | Y | N | Y | Y | N | N | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 18/26 | ||
| Holdsworth and Webster,12 2004 | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | N | Y | N | N | Y | Y | N | Y | Y | Y | N | N | N | N | 16/26 | ||
| Webster et a1,14 2008 | Y | Y | Y | Y | P | Y | Y | N | N | Y | N | N | Y | N | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 16/26 | ||
| Leemrijse et a1,8 2008 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 22/26 | ||
| Mitchell and de Lissovoy,9 1997 | Y | Y | Y | Y | N | Y | U | N | Y | N | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 18/26 | ||
| Pendergast et a1,112012 | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | N | N | Y | Y | 22/26 | ||
| Moore et al,10 2005 | Y | Y | N | Y | N | Y | Y | Y | N | N | U | U | Y | Y | N | Y | Y | U | Y | Y | Y | N | N | N | N | 13/26 |
Criteria are based on Downs and Black checklist (Appendix 1): Y (yes)=criterion met, N (no) =criterion not met P=criterion partially met, and U=criterion unable to determine from the study manuscript. Criterion 5 has a maximum of 2 points, and all other criteria have a maximum of 1 point. U ratings received zero points. Criteria 17 and 27 were omitted due to reasons explained in the “Quality Assessment” section.
Health Care Costs
Data from the included studies supported a grade B recommendation that costs to patient or insurance companies per physical therapy episode of care were less when patients saw a physical therapist directly versus through physician referral, likely due to less imaging ordered, injections performed, and medications prescribed. Four studies9,11,13,15 reported on cost differences between direct access and physician referral groups, and all reported lower costs (to the patient, insurance company, or health system) in the direct access group during the participants' episode of care. Pendergast et al11 found the mean allowable amounts during the episode of physical therapy care were approximately $152 less for physical therapy–related costs and $102 less for non–physical therapy–related costs, amounting to over $250 less for total costs per episode of care (P<.001). Mitchell and de Lissovoy9 found that paid claims per episode of care were $1,232 less in the direct access group for all services and drugs per episode of physical therapy care (P<.001). Hackett et al15 reported a mean difference of approximately £38 (∼$59) less cost* per patient among those who incurred costs from physical therapy (P<.01; 95% confidence interval=£12.41, £63.65); however, this finding was largely because the referral practice had a high percentage of patients who received private physical therapy treatments (description of private physical therapy not fully explained in the article). Finally, although Holdsworth et al13 did not run statistical analyses, patients in the direct access group had approximately £22 (∼$34) less cost (not including cost to patients), which we extrapolated would amount to an average cost benefit to the National Health Service of Scotland of approximately £2 million per year (∼$3,107,400).
Number of Physical Therapy Visits
Data were available to support a grade C recommendation that the number of physical therapy visits was significantly less in the direct access group compared with the physician-referred group. Six articles compared mean number of physical therapy visits per patient episode of care with 4 studies (levels 3 and 4)8,9,11,12 reporting that patients in the direct access group had significantly fewer visits and 2 studies (level 3)13,15 reporting no significant difference between groups. Of note, both studies conducted in the United States9,11 that collected data on number of visits showed a significant difference between groups. Pendergast et al,11 who included the largest number of participants (direct access group, N=17,362; physician referral group, N=44,755) of the 6 studies, reported a mean difference of 1.1 visits between groups (P<.001). Mitchell and de Lissovoy9 reported the largest mean difference, with the direct access group using 20.2 visits compared with the physician referral group using 33.6 (P<.0001); however, this study was conducted in 1997, so it might not reflect more recent practice patterns.
Adjunctive Testing and Interventions (Imaging and Pharmacological Interventions)
There was a grade B recommendation that less adjunctive testing and fewer interventions were prescribed when a patient received physical therapy through direct access compared with physician referral. All 3 studies9,13,15 looking at pharmacological interventions showed significant differences between groups. Mitchell and de Lissovoy9 reported there were significantly fewer drug claims in the direct access group (P<.01), Hackett et al15 reported fewer medications were prescribed in the direct access group (P<.001), and Holdsworth et al13 reported 12% less took nonsteroidal anti-inflammatory drugs or analgesics in the direct access group (P<.0001).
All 3 studies 9,13,15 investigating imaging showed significant differences between groups. Mitchell and de Lissovoy9 reported fewer radiology claims (P<.01), Hackett et al15 reported 8% less imaging ordered in the direct access group (no statistical tests run), and Holdsworth et al13 showed 6% less imaging ordered in the direct access group (P<.001).
Physician Appointments, Consultation Services, and Hospital Admits
Data from the included studies supported a grade D (inconsistent) recommendation that patients in the direct access group saw their general practitioner (GP) or other consultants less than in the physician referral group, suggesting that patients maintain contact with other medical providers despite seeking direct access to physical therapy. Out of 3 studies12,14,15 reporting on frequency of GP consultation services, only Holdsworth and Webster12 found a significant difference (P=.0113), with 29% of the direct access group having at least one contact with their GP for the same diagnosis 3 months after physical therapy versus 46% in the physician referral group (for other mean differences, see Tab. 2). Webster et al14 found that the number of GP consultations 1 month after physical therapy was approximately the same in both groups (not significant, P=.219). Hackett et al15 investigated the frequency of GP visits during the course of physical therapy care and found patients, on average, saw their GP for 2 visits in both groups. Regarding hospital admissions, only the study by Mitchell and de Lissovoy9 investigated this outcome measure and showed significantly fewer mean hospital admissions in the direct access group (P<.01).
Patient Satisfaction
The data of the included studies indicated a grade B recommendation that patients reported a higher level of satisfaction when they received physical therapy through direct access versus physician referral. The 2 studies14,15 that investigated satisfaction showed that patients in the direct access group reported greater satisfaction compared with patients in the physician referral group. Webster et al14 showed 5% more of the participants in the direct access group were satisfied or very satisfied (P<.001). Hackett et al15 showed 9% more of the participants in the direct access group evaluated management of their condition as average or above average, although it was difficult to conclude whether the level of significance (P<.01) would have been the same if only direct access and physician referral groups were compared because the study ran these tests among 3 groups (including one group for which data was not extracted).
Patient Outcomes and Harm
A grade C recommendation was suggested by data from the included studies that patients receiving physical therapy through direct access versus referral had better outcomes at discharge. Four studies8,12,13,15 reported on discharge outcomes, and although all of the studies showed improved outcomes in the direct access group, the differences reached significance in 2 studies8,12 (one level 3, one level 4). Leemrijse et al8 reported that the percentage of patients who fully achieved goals at discharge was 9% more in the direct access group compared with the physician referral group (P<.001). Holdsworth and Webster12 reported the percentage of patients who finished their course of care was 79% in the direct access group compared with 60% in the physician referral group (P=.004), and the percentage of those who achieved their goals was 15% more in the direct access group compared with a control group (P=.079). In this study, significantly less average pain was reported at discharge (the direct access group decreased 3 points on the visual analog scale and the physician referral group decreased 2.5 points on the visual analog scale) (P=.011), although we question whether this is a clinically meaningful finding. Hackett et al15 reported the mean number of days of work missed due to the condition was 17 days less in the direct access group compared with the physician referral group, although statistical analyses were not reported for this difference. Holdsworth and colleagues12,13 reported no significant difference between groups regarding percentage who achieved goals (the direct access group had, on average, 2% more achieved goals compared with the physician referral group, P=.82).
Data from the included studies indicated a grade C recommendation that individuals seen by a physical therapist in a direct access capacity did not result in harm because only one level 4 study reported on this outcome measure. Moore and colleagues10 retrospectively compared harm between direct access and physician referral groups. There were no reported adverse events in either group resulting from physical therapist diagnosis and management, no credentials or state licenses modified or revoked for disciplinary action, and no litigation cases filed against the US government in either group over a 40-month observation period. The sample sizes in that study were quite large, with 50,799 patients included in the direct access group and 61,854 patients included in the physician referral group. It is commonly thought that physical therapists seeing patients in a direct access capacity would result in overlooking serious diagnoses that could mimic musculoskeletal presentations, thereby putting the patient's health at risk. Contrary to this conception, Moore et al cited samples of diagnoses identified by physical therapists in the study, which included Ewing sarcoma, Charcot-Marie tooth disease, fractures, nerve injuries (long thoracic, suprascapular, and spinal nerve root injuries), posterior lateral corner sprain, osteochondritis dessicans, ankylosing spondylitis, tarsal coalition, compartment syndrome, and scapholunate instability. Of note, compared with the other studies in this review that involved civilian physical therapists, the large majority of physical therapists in this study were military physical therapists, with 8% civilian physical therapists, many with specialized training. Approximately 38% of the physical therapists had board-certified training in one or more specialties (eg, orthopedics, neurology, sports), and 88% had attended a specialty training course.
Results Summary
Due to limitations inherent in study design, differences in number of participants between groups, and other potentially confounding variables, we believe our most relevant findings are that patient and health care costs were not greater in the direct access group compared with the physician referral group. Furthermore, these results do not indicate that patients seen through direct access received more visits or achieved inferior outcomes compared with those who were referred by physicians. Harm was not reported in the majority of the studies; however, one large-scale study examining military physical therapists showed no harm when individuals received direct access physical therapy. Given that patients in the direct access group received fewer medications and less imaging while achieving similar or superior discharge outcomes, the results from this review suggest a relative decreased risk of harm in the direct access group, potentially due to fewer side effects of medication or less exposure to imaging radiation.
Discussion
The purpose of this review was to determine whether health care costs were less and outcomes were improved if individuals received physical therapy care through direct access compared with physician referral. All studies (level 3–4 evidence) reporting on cost showed decreased cost in the direct access group (grade B recommendation), likely due to decreased imaging, number of physical therapy visits, and medications prescribed. Similarly, all studies (level 3–4 evidence) showed the same or better discharge outcomes (grade C), achieved in fewer physical therapy visits (grade C), with increased satisfaction (grade B) in the direct access group and without any evidence of increased risk of harm to the patient (grade C). This preliminary support for improved outcomes in the direct access group potentially could be due to earlier initiation of physical therapy. These observations are consistent with prior individual studies that collectively support improved outcomes for patients and decreased costs associated with earlier initiation of physical therapy clinical management.23–26 Between-cohort differences in each study were generally small in magnitude; however, they could result in meaningful optimization of patient outcomes and decreases in costs when distributed over the large US health care environment. In summary, findings from this systematic review support the safety, efficacy, and cost-effectiveness of physical therapist services by way of direct access compared with physician-referred episodes of care.
Little previous work has been conducted to critically evaluate and synthesize the literature related to physical therapy clinical management obtained through direct access. The previous systematic review on this topic by Robert and Stevens published in 19974 examined a related question, reporting results from studies largely conducted within the National Health Service of the United Kingdom. Similar to the results of this review, Robert and Stevens found improved waiting time, recovery time, convenience, and costs among patients receiving physical therapy through direct or open access. However, in this report, the terms “direct access” and “open access” seem to have been defined as expeditious physical therapy referrals from generalist physicians, such as “on-demand” physical therapy clinics, which reflects a gatekeeping model, with the GP initiating the physical therapy referral. We believe our review was able to more directly focus on results of direct access physical therapy defined by the consumer self-referring for physical therapy. Another review recently published by Desmeules and colleagues27 focused on physical therapists in advanced practice or extended scope roles compared with usual care by physicians and other medical providers for patients with musculoskeletal disorders. Similar to our findings, the review found advanced practice care may be as (or more) beneficial than usual care by physicians in terms of treatment effectiveness, use of health care resources, economic costs and patient satisfaction.
In contrast, in our review, we investigated a group of physical therapists, the majority of whom were not practicing in advanced practice roles (7 out of 8 studies exclusively focused on physical therapists without any special training reported who largely held master's or bachelor's degrees), and still found advantages in terms of treatment effectiveness, use of resources, economic costs, and patient satisfaction over initial physician care. As the annual percentage of civilians who are board-certified physical therapy specialists has been steadily increasing, perhaps the profession is progressing in skill level to more frequently serve in these advance practice roles. However, in the interim, our review suggests the current basic training and competency requirements are sufficient for physical therapists without this specialized training to function in a direct access capacity.
Various methodological limitations were identified in the literature, which should be addressed in future studies. Dependent variable measurements and data reporting were so heterogeneous that data could not be pooled through meta-analytic procedures. Fewer than half of the included studies (3 out of 8) were conducted in the United States, which is relevant because of the unique payer arrangements and practice regulations involving physical therapists in the US health care market. Furthermore, health care costs vary substantially across countries, thus cost savings and expenditure cannot be generalized. All included studies involved an outpatient orthopedic practice environment, so other practice areas were under-represented. There was no randomization of study participants to groups, and blinding of participants was not conducted. This approach is relevant because, in addition to potentially limiting inferences that can be made regarding cause and effect based on the evidence, there is a possibility for the influence of uncontrolled selection bias among individuals who self-refer for physical therapy through direct access.
From the results of the logistic regression conducted by Holdsworth and Webster,12 individuals in a single health district (n=679) in Scotland who engaged in direct access utilization of physical therapist services were significantly more likely to report male sex, younger age, shorter symptom duration, and engagement in paid employment than individuals who received physical therapy in physician-referred episodes of care. Subsequently, Leemrijse and colleagues8 reported as the results of a logistic regression analysis that individuals in the Netherlands (n=10,519) who are younger, with higher educational attainment, nonspecific spine symptoms, recurrent symptoms, and prior treatment by a physical therapist were significantly more likely to have direct access to physical therapist services than individuals who were referred by a physician. Although this information reflects characteristics that may be over-represented in the direct access group, these findings also provide valuable information that can be used to guide preparation for physical therapists to function in a direct access environment. Finally, publication bias and selective reporting within each study could have introduced risk of bias to our summary of evidence.
The consistent results identified across the several moderate-quality studies included in this systematic review may form a solid basis for policy and payment decisions that would facilitate delivery of physical therapist services through direct access.8,9,11–15,28 Some form of direct access to physical therapist services is currently available by statute in 47 out of 50 states (United States),29 as well as internationally.8,15 However, self-referral accounts have been estimated to account for as little as 6% to 10% of referral volume30 in some direct access states. One reason for this limitation is that most third-party payers do not compensate physical therapists for evaluation and management of patients who self-refer for physical therapy.† In addition, direct access is unrecognized as a covered route of access to physical therapy in the United States at the federal level. These legislators and payers should consider the potential for improved patient outcomes and significant health care cost savings by facilitating more widespread direct access to physical therapist services. A common argument made by proponents of physician referral against more widespread direct access to physical therapist services has been potential adverse effects on patient safety. However, no scientific literature is currently available to support this claim. In the United States, the Commission on Accreditation in Physical Therapy Education (CAPTE) criteria support the ability of all physical therapists to engage in the delivery of physical therapy through direct access. Furthermore, direct access to physical therapy is commonplace in many other countries even though the large majority of physical therapists practice with a bachelor's or master's level education. In the United States, the large majority of physical therapist programs are doctor of physical therapy programs; however, a comparatively low percentage of physical therapists practice in a direct access capacity due to these various barriers.
In conclusion, this review suggests that physical therapists practicing in a direct access capacity have the potential to decrease costs and improve outcomes in patients with musculoskeletal complaints without prescribing medications and ordering adjunctive testing that could introduce harm to the patient. At a minimum, the results presented in this report show no evidence of greater costs or increased number of visits or harm when patients self-refer directly to a physical therapist. Finally, despite self-referring for physical therapy, it appears that patients continue to be engaged with physicians throughout their course of care; thus, it is unlikely that widespread implementation of direct access to physical therapy will reduce demand for seeking care from other practitioners. The potential benefit of direct access to physical therapy in other practice settings should be further explored, as well as alternate pathways for providing health services that take advantage of the safety, efficacy, and cost-effectiveness of direct access physical therapy.
A platform presentation of this research was given at the Combined Sections Meeting of the American Physical Therapy Association; February 21–24, 2013; San Diego, California.
This study was funded by the Health Services Research Pipeline established through the American Physical Therapy Association to cover basic supplies and conference fees related to the research.
For all conversions, we used Great Britain sterling pound to US dollar, Bank of England daily rate as of August 15, 2013 (http://www.bankofengland.co.uk/boeapps/iadb/Rates.asp).
A recommended process for third-party health insurance organizations to calculate the economic benefit of consumer direct access to physical therapy is presented in Appendix 2.
References
Appendix 1
Modified Downs and Black Criteria and Scoring Guidelinesa
| Number . | Criteria . | Scoring Criteria . |
|---|---|---|
| Reporting | ||
| 1 | Is the hypothesis/aim/objective of the study clearly described? | A point was awarded if the hypothesis aim or objective of the study was implicitly or explicitly indicated anywhere in the article. |
| 2 | Are the main outcomes to be measured clearly described in the introduction or "Method" section? | A point was not awarded it the main outcome to be measured was first mentioned in the "Results" section. |
| 3 | Are the characteristics of the patients included in the study clearly described? | A point was awarded if inclusion or exclusion criteria, or both, were indicated. |
| 4 | Are the interventions of interest clearly described? | A point was awarded only when the intervention was clear and specific. For the purpose of this review, we interpreted "clear and specific" to mean direct mention of groups being direct access compared with referral with or without further descriptors of what this constituted. |
| 5 | Are the distributions of principal confounders for each group of participants to be compared clearly described? | Two points were awarded if a study reported any possible confounders (eg, sex ratios, age, comorbidities, severity of injury) that might account for differences between groups clearly in table format. One point was awarded if the study indicated that groups were matched for any such demographical variables or if potential confounders were mentioned in the text of the article but not clearly listed in table format. No points were awarded if the study did not report any confounders. |
| 6 | Are the main findings of the study clearly described? | A point was awarded if quantitative data were reported for all of the main outcome measures indicated in the introduction or "Method" section. |
| 7 | Does the study provide estimates of the random variability in the data for the main outcomes? | A point was awarded if the interquartile range (for non-normally distributed data), standard error, standard deviation, or confidence intervals (for normally distributed data) were reported. If the distribution of the data was not described, we assumed that the estimates used were appropriate, and we answered "yes" (1 point). |
| 8 | Have all of the important adverse events that may be a consequence of the intervention been reported? | A point was awarded if any adverse events, unwanted side effects, or lack thereof were explicitly indicated from either referral or direct access interventions. Although adverse events were outcome measures extracted from the studies in this review, we believed that they also were indicative of comprehensive reporting. A point. was not awarded if a study made no mention of the presence or absence of adverse events (eg, loss of license of a therapist, minor or serious side effects of intervention) in the direct access or physician referral groups. |
| 9 | Have the characteristics of patients lost to follow-up been described? | The authors of this tool indicated that this question should be answered "yes" where there were no losses to follow-up or where losses to follow-up were small that findings would have been unaffected by their inclusion. For the purposes of this review, a point was awarded if a study explicitly reported that there were no losses to follow-up or if the losses to follow-up accounted for a maximum of 10% of the sample of participants originally enrolled in the study (or up to 5% of the original number of participants assigned to each direct access and physician referral group). No point was awarded if the study did not report the number of patients lost to follow-up or this information could not be obtained from the tables, figures, or text of the study. |
| 10 | Have actual probability values been reported (eg, .035 rather than <.05) for the main outcomes, except where the probability value is less than .001? | A point was awarded if the exact P value was provided for both statistically significant and nonsignificant results for at least the main outcome measures. A point was not awarded if a study simply indicated that the results for the main outcome measures were not significant without providing the exact P value. |
| External Validity | ||
| 11 | Were the individuals asked to participate in the study representative of the entire population from which they were recruited? | A point was awarded if the study identified the source population for patients and described how the patients were selected. Patients were determined to be representative if they comprised the entire source population, an unselected sample of consecutive patients, or a random sample (only feasible where a list of all members of the relevant population exists). Where a study red not report the proportion of the source population horn which the patients are derived, the question was answered as unable to determine. |
| 12 | Were those individuals who were prepared to participate representative of the entire population from which they were recruited? | The proportion of those asked who agreed to participate or responded should be stated. Validation that the sample was representative would include demonstrating that the distribution of the main confounding factors was the same in the study sample and the source population (eg, if the demographics and diagnoses of the patients were considered representative of a typical outpatient moo practice, the study was awarded a point). No point was awarded if the proportion of those asked who agreed to participate or responded was not stated. |
| 13 | Were the staff, places, and faculties where the patients were treated representative of the treatment the majority of patients receive? | A point was awarded unless the study specifically stated that patients were treated by a therapist who received specialized training or the direct access or physician referral group received treatment in a specialized facility defined by advanced training or focus of intervention in “niche” areas of physical therapy (eg, pediatrics). |
| Internal Validity—Bias | ||
| 14 | Was an attempt made to blind study participants to the intervention they received? | A point was awarded if the patients were not aware of, or would have no way of knowing (as in the case of retrospective studies), which intervention they received. The study was not awarded a point if it was prospective and failed to mention whether the patients had knowledge of whether they were assigned to the direct access or physician referral group. |
| 15 | Was an attempt made to blind those measuring the main outcomes of the intervention? | A point was awarded if the study specifically stated that those assessing the outcome measures were unaware of (or would have no way of knowing) whether the patients were in the direct access or physician referral group. |
| 16 | If any of the results of the study were based on "data dredging," was this made clear? | A point was awarded if no retrospective unplanned (at the outset of the study) subgroup analyses were reported. |
| 17 | In trials and cohort studies, do the analyses adjust for different lengths of follow-up of patients, or, in case-control studies, is the time period between the intervention and outcome the same for cases and controls, | For the purposes of this review, this question was omitted due to reasons previously stated. |
| 18 | Were the statistical tests used to assess the main outcomes appropriate, | If the distribution of the data (normal or not) was not described, it was assumed that the estimates used were appropriate, and a point was awarded. No point was awarded for studies that reported qualitative or quantitative data without any form of statistical comparisons or if the statistical tests reported were not appropriate. |
| 19 | Was adherence to the intervention reliable? | If the authors in prospective studies reported nonadherence to physical therapy intervention or adherence could not be determined, the study was not awarded a point. In retrospective studies, data were collected only for those patients who completed their episode of care (adherence to physical therapy assumed), and a point was awarded. For studies where the effect of any nonadherence was likely to bias any association to the null, the study received a point. |
| 20 | Were the main outcome measures used accurate (valid and reliable)? | A point was awarded if the primary outcome measures were thought to be valid and reliable (eg, number of physical therapy visits per chart report), regardless of whether reliability or validity was reported. A point was not awarded if at least one of the primary outcome measures in the study was not valid or reliable or if this information was not reported or could not be determined (ie, a questionnaire without reported validity or reliability). |
| Internal Validity-Confounding (Selection Bias) | ||
| 21 | Were the patients in different intervention groups (trials and cohort studies), or were the cases and controls (case-control studies) recruited from the same population? | A point was awarded when participants from both direct access and physician referral groups were recruited from the same population. Otherwise, a point was not awarded (eg, a point was not awarded when all participants from the physician referral group received care at clinic A and all participants in the direct access group received care at clinic B, because they could have represented 2 distinct populations). |
| 22 | Were study participants in different intervention groups (trials and cohort studies), or were the cases and controls (case-control studies) recruited over the same period of time? | A point was awarded when the study provided a specific time line for patient recruitment (prospective studies) or when data were collected between reported dates of patient care (retrospective studies). |
| 23 | Were study participants randomized to intervention groups? | A point for random allocation was awarded if random allocation of patients was stated in the "Method" section of the article. The precise method of randomization need not be specified. Quasi-randomization allocation procedures, such as allocation by bed availability, did not satisfy this criterion. For crossover study designs, a point was awarded when participants were randomly allocated in the order in which treatments were received. |
| 24 | Was the randomized intervention assignment concealed from both patients and health care team until recruitment was complete and irrevocable? | The study did not receive a point unless the participants were randomly allocated and the methods for ensuring random allocation were specified. |
| 25 | Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? | A point was awarded unless the effect of the main confounders was not investigated or confounding was demonstrated, but no adjustment was made in the final analyses. |
| 26 | Were losses of patients to follow-up taken into account? | A point was awarded as long as the number of dropouts lost to follow-up accounted for less than 10% of the initial number of total participants or a maximum of 5% from each group. The question was answered with "unable to determine" if the number of patients lost to follow-up were not reported or could not be deduced from the outcome data (le, initial and final sample sizes not indicated). |
| Power | ||
| 27 | Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is less than .05? | For the purposes of this evidence-based review, this question was omitted. |
| Number . | Criteria . | Scoring Criteria . |
|---|---|---|
| Reporting | ||
| 1 | Is the hypothesis/aim/objective of the study clearly described? | A point was awarded if the hypothesis aim or objective of the study was implicitly or explicitly indicated anywhere in the article. |
| 2 | Are the main outcomes to be measured clearly described in the introduction or "Method" section? | A point was not awarded it the main outcome to be measured was first mentioned in the "Results" section. |
| 3 | Are the characteristics of the patients included in the study clearly described? | A point was awarded if inclusion or exclusion criteria, or both, were indicated. |
| 4 | Are the interventions of interest clearly described? | A point was awarded only when the intervention was clear and specific. For the purpose of this review, we interpreted "clear and specific" to mean direct mention of groups being direct access compared with referral with or without further descriptors of what this constituted. |
| 5 | Are the distributions of principal confounders for each group of participants to be compared clearly described? | Two points were awarded if a study reported any possible confounders (eg, sex ratios, age, comorbidities, severity of injury) that might account for differences between groups clearly in table format. One point was awarded if the study indicated that groups were matched for any such demographical variables or if potential confounders were mentioned in the text of the article but not clearly listed in table format. No points were awarded if the study did not report any confounders. |
| 6 | Are the main findings of the study clearly described? | A point was awarded if quantitative data were reported for all of the main outcome measures indicated in the introduction or "Method" section. |
| 7 | Does the study provide estimates of the random variability in the data for the main outcomes? | A point was awarded if the interquartile range (for non-normally distributed data), standard error, standard deviation, or confidence intervals (for normally distributed data) were reported. If the distribution of the data was not described, we assumed that the estimates used were appropriate, and we answered "yes" (1 point). |
| 8 | Have all of the important adverse events that may be a consequence of the intervention been reported? | A point was awarded if any adverse events, unwanted side effects, or lack thereof were explicitly indicated from either referral or direct access interventions. Although adverse events were outcome measures extracted from the studies in this review, we believed that they also were indicative of comprehensive reporting. A point. was not awarded if a study made no mention of the presence or absence of adverse events (eg, loss of license of a therapist, minor or serious side effects of intervention) in the direct access or physician referral groups. |
| 9 | Have the characteristics of patients lost to follow-up been described? | The authors of this tool indicated that this question should be answered "yes" where there were no losses to follow-up or where losses to follow-up were small that findings would have been unaffected by their inclusion. For the purposes of this review, a point was awarded if a study explicitly reported that there were no losses to follow-up or if the losses to follow-up accounted for a maximum of 10% of the sample of participants originally enrolled in the study (or up to 5% of the original number of participants assigned to each direct access and physician referral group). No point was awarded if the study did not report the number of patients lost to follow-up or this information could not be obtained from the tables, figures, or text of the study. |
| 10 | Have actual probability values been reported (eg, .035 rather than <.05) for the main outcomes, except where the probability value is less than .001? | A point was awarded if the exact P value was provided for both statistically significant and nonsignificant results for at least the main outcome measures. A point was not awarded if a study simply indicated that the results for the main outcome measures were not significant without providing the exact P value. |
| External Validity | ||
| 11 | Were the individuals asked to participate in the study representative of the entire population from which they were recruited? | A point was awarded if the study identified the source population for patients and described how the patients were selected. Patients were determined to be representative if they comprised the entire source population, an unselected sample of consecutive patients, or a random sample (only feasible where a list of all members of the relevant population exists). Where a study red not report the proportion of the source population horn which the patients are derived, the question was answered as unable to determine. |
| 12 | Were those individuals who were prepared to participate representative of the entire population from which they were recruited? | The proportion of those asked who agreed to participate or responded should be stated. Validation that the sample was representative would include demonstrating that the distribution of the main confounding factors was the same in the study sample and the source population (eg, if the demographics and diagnoses of the patients were considered representative of a typical outpatient moo practice, the study was awarded a point). No point was awarded if the proportion of those asked who agreed to participate or responded was not stated. |
| 13 | Were the staff, places, and faculties where the patients were treated representative of the treatment the majority of patients receive? | A point was awarded unless the study specifically stated that patients were treated by a therapist who received specialized training or the direct access or physician referral group received treatment in a specialized facility defined by advanced training or focus of intervention in “niche” areas of physical therapy (eg, pediatrics). |
| Internal Validity—Bias | ||
| 14 | Was an attempt made to blind study participants to the intervention they received? | A point was awarded if the patients were not aware of, or would have no way of knowing (as in the case of retrospective studies), which intervention they received. The study was not awarded a point if it was prospective and failed to mention whether the patients had knowledge of whether they were assigned to the direct access or physician referral group. |
| 15 | Was an attempt made to blind those measuring the main outcomes of the intervention? | A point was awarded if the study specifically stated that those assessing the outcome measures were unaware of (or would have no way of knowing) whether the patients were in the direct access or physician referral group. |
| 16 | If any of the results of the study were based on "data dredging," was this made clear? | A point was awarded if no retrospective unplanned (at the outset of the study) subgroup analyses were reported. |
| 17 | In trials and cohort studies, do the analyses adjust for different lengths of follow-up of patients, or, in case-control studies, is the time period between the intervention and outcome the same for cases and controls, | For the purposes of this review, this question was omitted due to reasons previously stated. |
| 18 | Were the statistical tests used to assess the main outcomes appropriate, | If the distribution of the data (normal or not) was not described, it was assumed that the estimates used were appropriate, and a point was awarded. No point was awarded for studies that reported qualitative or quantitative data without any form of statistical comparisons or if the statistical tests reported were not appropriate. |
| 19 | Was adherence to the intervention reliable? | If the authors in prospective studies reported nonadherence to physical therapy intervention or adherence could not be determined, the study was not awarded a point. In retrospective studies, data were collected only for those patients who completed their episode of care (adherence to physical therapy assumed), and a point was awarded. For studies where the effect of any nonadherence was likely to bias any association to the null, the study received a point. |
| 20 | Were the main outcome measures used accurate (valid and reliable)? | A point was awarded if the primary outcome measures were thought to be valid and reliable (eg, number of physical therapy visits per chart report), regardless of whether reliability or validity was reported. A point was not awarded if at least one of the primary outcome measures in the study was not valid or reliable or if this information was not reported or could not be determined (ie, a questionnaire without reported validity or reliability). |
| Internal Validity-Confounding (Selection Bias) | ||
| 21 | Were the patients in different intervention groups (trials and cohort studies), or were the cases and controls (case-control studies) recruited from the same population? | A point was awarded when participants from both direct access and physician referral groups were recruited from the same population. Otherwise, a point was not awarded (eg, a point was not awarded when all participants from the physician referral group received care at clinic A and all participants in the direct access group received care at clinic B, because they could have represented 2 distinct populations). |
| 22 | Were study participants in different intervention groups (trials and cohort studies), or were the cases and controls (case-control studies) recruited over the same period of time? | A point was awarded when the study provided a specific time line for patient recruitment (prospective studies) or when data were collected between reported dates of patient care (retrospective studies). |
| 23 | Were study participants randomized to intervention groups? | A point for random allocation was awarded if random allocation of patients was stated in the "Method" section of the article. The precise method of randomization need not be specified. Quasi-randomization allocation procedures, such as allocation by bed availability, did not satisfy this criterion. For crossover study designs, a point was awarded when participants were randomly allocated in the order in which treatments were received. |
| 24 | Was the randomized intervention assignment concealed from both patients and health care team until recruitment was complete and irrevocable? | The study did not receive a point unless the participants were randomly allocated and the methods for ensuring random allocation were specified. |
| 25 | Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? | A point was awarded unless the effect of the main confounders was not investigated or confounding was demonstrated, but no adjustment was made in the final analyses. |
| 26 | Were losses of patients to follow-up taken into account? | A point was awarded as long as the number of dropouts lost to follow-up accounted for less than 10% of the initial number of total participants or a maximum of 5% from each group. The question was answered with "unable to determine" if the number of patients lost to follow-up were not reported or could not be deduced from the outcome data (le, initial and final sample sizes not indicated). |
| Power | ||
| 27 | Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is less than .05? | For the purposes of this evidence-based review, this question was omitted. |
For original criteria, refer to Downs and Black.17
Modified Downs and Black Criteria and Scoring Guidelinesa
| Number . | Criteria . | Scoring Criteria . |
|---|---|---|
| Reporting | ||
| 1 | Is the hypothesis/aim/objective of the study clearly described? | A point was awarded if the hypothesis aim or objective of the study was implicitly or explicitly indicated anywhere in the article. |
| 2 | Are the main outcomes to be measured clearly described in the introduction or "Method" section? | A point was not awarded it the main outcome to be measured was first mentioned in the "Results" section. |
| 3 | Are the characteristics of the patients included in the study clearly described? | A point was awarded if inclusion or exclusion criteria, or both, were indicated. |
| 4 | Are the interventions of interest clearly described? | A point was awarded only when the intervention was clear and specific. For the purpose of this review, we interpreted "clear and specific" to mean direct mention of groups being direct access compared with referral with or without further descriptors of what this constituted. |
| 5 | Are the distributions of principal confounders for each group of participants to be compared clearly described? | Two points were awarded if a study reported any possible confounders (eg, sex ratios, age, comorbidities, severity of injury) that might account for differences between groups clearly in table format. One point was awarded if the study indicated that groups were matched for any such demographical variables or if potential confounders were mentioned in the text of the article but not clearly listed in table format. No points were awarded if the study did not report any confounders. |
| 6 | Are the main findings of the study clearly described? | A point was awarded if quantitative data were reported for all of the main outcome measures indicated in the introduction or "Method" section. |
| 7 | Does the study provide estimates of the random variability in the data for the main outcomes? | A point was awarded if the interquartile range (for non-normally distributed data), standard error, standard deviation, or confidence intervals (for normally distributed data) were reported. If the distribution of the data was not described, we assumed that the estimates used were appropriate, and we answered "yes" (1 point). |
| 8 | Have all of the important adverse events that may be a consequence of the intervention been reported? | A point was awarded if any adverse events, unwanted side effects, or lack thereof were explicitly indicated from either referral or direct access interventions. Although adverse events were outcome measures extracted from the studies in this review, we believed that they also were indicative of comprehensive reporting. A point. was not awarded if a study made no mention of the presence or absence of adverse events (eg, loss of license of a therapist, minor or serious side effects of intervention) in the direct access or physician referral groups. |
| 9 | Have the characteristics of patients lost to follow-up been described? | The authors of this tool indicated that this question should be answered "yes" where there were no losses to follow-up or where losses to follow-up were small that findings would have been unaffected by their inclusion. For the purposes of this review, a point was awarded if a study explicitly reported that there were no losses to follow-up or if the losses to follow-up accounted for a maximum of 10% of the sample of participants originally enrolled in the study (or up to 5% of the original number of participants assigned to each direct access and physician referral group). No point was awarded if the study did not report the number of patients lost to follow-up or this information could not be obtained from the tables, figures, or text of the study. |
| 10 | Have actual probability values been reported (eg, .035 rather than <.05) for the main outcomes, except where the probability value is less than .001? | A point was awarded if the exact P value was provided for both statistically significant and nonsignificant results for at least the main outcome measures. A point was not awarded if a study simply indicated that the results for the main outcome measures were not significant without providing the exact P value. |
| External Validity | ||
| 11 | Were the individuals asked to participate in the study representative of the entire population from which they were recruited? | A point was awarded if the study identified the source population for patients and described how the patients were selected. Patients were determined to be representative if they comprised the entire source population, an unselected sample of consecutive patients, or a random sample (only feasible where a list of all members of the relevant population exists). Where a study red not report the proportion of the source population horn which the patients are derived, the question was answered as unable to determine. |
| 12 | Were those individuals who were prepared to participate representative of the entire population from which they were recruited? | The proportion of those asked who agreed to participate or responded should be stated. Validation that the sample was representative would include demonstrating that the distribution of the main confounding factors was the same in the study sample and the source population (eg, if the demographics and diagnoses of the patients were considered representative of a typical outpatient moo practice, the study was awarded a point). No point was awarded if the proportion of those asked who agreed to participate or responded was not stated. |
| 13 | Were the staff, places, and faculties where the patients were treated representative of the treatment the majority of patients receive? | A point was awarded unless the study specifically stated that patients were treated by a therapist who received specialized training or the direct access or physician referral group received treatment in a specialized facility defined by advanced training or focus of intervention in “niche” areas of physical therapy (eg, pediatrics). |
| Internal Validity—Bias | ||
| 14 | Was an attempt made to blind study participants to the intervention they received? | A point was awarded if the patients were not aware of, or would have no way of knowing (as in the case of retrospective studies), which intervention they received. The study was not awarded a point if it was prospective and failed to mention whether the patients had knowledge of whether they were assigned to the direct access or physician referral group. |
| 15 | Was an attempt made to blind those measuring the main outcomes of the intervention? | A point was awarded if the study specifically stated that those assessing the outcome measures were unaware of (or would have no way of knowing) whether the patients were in the direct access or physician referral group. |
| 16 | If any of the results of the study were based on "data dredging," was this made clear? | A point was awarded if no retrospective unplanned (at the outset of the study) subgroup analyses were reported. |
| 17 | In trials and cohort studies, do the analyses adjust for different lengths of follow-up of patients, or, in case-control studies, is the time period between the intervention and outcome the same for cases and controls, | For the purposes of this review, this question was omitted due to reasons previously stated. |
| 18 | Were the statistical tests used to assess the main outcomes appropriate, | If the distribution of the data (normal or not) was not described, it was assumed that the estimates used were appropriate, and a point was awarded. No point was awarded for studies that reported qualitative or quantitative data without any form of statistical comparisons or if the statistical tests reported were not appropriate. |
| 19 | Was adherence to the intervention reliable? | If the authors in prospective studies reported nonadherence to physical therapy intervention or adherence could not be determined, the study was not awarded a point. In retrospective studies, data were collected only for those patients who completed their episode of care (adherence to physical therapy assumed), and a point was awarded. For studies where the effect of any nonadherence was likely to bias any association to the null, the study received a point. |
| 20 | Were the main outcome measures used accurate (valid and reliable)? | A point was awarded if the primary outcome measures were thought to be valid and reliable (eg, number of physical therapy visits per chart report), regardless of whether reliability or validity was reported. A point was not awarded if at least one of the primary outcome measures in the study was not valid or reliable or if this information was not reported or could not be determined (ie, a questionnaire without reported validity or reliability). |
| Internal Validity-Confounding (Selection Bias) | ||
| 21 | Were the patients in different intervention groups (trials and cohort studies), or were the cases and controls (case-control studies) recruited from the same population? | A point was awarded when participants from both direct access and physician referral groups were recruited from the same population. Otherwise, a point was not awarded (eg, a point was not awarded when all participants from the physician referral group received care at clinic A and all participants in the direct access group received care at clinic B, because they could have represented 2 distinct populations). |
| 22 | Were study participants in different intervention groups (trials and cohort studies), or were the cases and controls (case-control studies) recruited over the same period of time? | A point was awarded when the study provided a specific time line for patient recruitment (prospective studies) or when data were collected between reported dates of patient care (retrospective studies). |
| 23 | Were study participants randomized to intervention groups? | A point for random allocation was awarded if random allocation of patients was stated in the "Method" section of the article. The precise method of randomization need not be specified. Quasi-randomization allocation procedures, such as allocation by bed availability, did not satisfy this criterion. For crossover study designs, a point was awarded when participants were randomly allocated in the order in which treatments were received. |
| 24 | Was the randomized intervention assignment concealed from both patients and health care team until recruitment was complete and irrevocable? | The study did not receive a point unless the participants were randomly allocated and the methods for ensuring random allocation were specified. |
| 25 | Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? | A point was awarded unless the effect of the main confounders was not investigated or confounding was demonstrated, but no adjustment was made in the final analyses. |
| 26 | Were losses of patients to follow-up taken into account? | A point was awarded as long as the number of dropouts lost to follow-up accounted for less than 10% of the initial number of total participants or a maximum of 5% from each group. The question was answered with "unable to determine" if the number of patients lost to follow-up were not reported or could not be deduced from the outcome data (le, initial and final sample sizes not indicated). |
| Power | ||
| 27 | Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is less than .05? | For the purposes of this evidence-based review, this question was omitted. |
| Number . | Criteria . | Scoring Criteria . |
|---|---|---|
| Reporting | ||
| 1 | Is the hypothesis/aim/objective of the study clearly described? | A point was awarded if the hypothesis aim or objective of the study was implicitly or explicitly indicated anywhere in the article. |
| 2 | Are the main outcomes to be measured clearly described in the introduction or "Method" section? | A point was not awarded it the main outcome to be measured was first mentioned in the "Results" section. |
| 3 | Are the characteristics of the patients included in the study clearly described? | A point was awarded if inclusion or exclusion criteria, or both, were indicated. |
| 4 | Are the interventions of interest clearly described? | A point was awarded only when the intervention was clear and specific. For the purpose of this review, we interpreted "clear and specific" to mean direct mention of groups being direct access compared with referral with or without further descriptors of what this constituted. |
| 5 | Are the distributions of principal confounders for each group of participants to be compared clearly described? | Two points were awarded if a study reported any possible confounders (eg, sex ratios, age, comorbidities, severity of injury) that might account for differences between groups clearly in table format. One point was awarded if the study indicated that groups were matched for any such demographical variables or if potential confounders were mentioned in the text of the article but not clearly listed in table format. No points were awarded if the study did not report any confounders. |
| 6 | Are the main findings of the study clearly described? | A point was awarded if quantitative data were reported for all of the main outcome measures indicated in the introduction or "Method" section. |
| 7 | Does the study provide estimates of the random variability in the data for the main outcomes? | A point was awarded if the interquartile range (for non-normally distributed data), standard error, standard deviation, or confidence intervals (for normally distributed data) were reported. If the distribution of the data was not described, we assumed that the estimates used were appropriate, and we answered "yes" (1 point). |
| 8 | Have all of the important adverse events that may be a consequence of the intervention been reported? | A point was awarded if any adverse events, unwanted side effects, or lack thereof were explicitly indicated from either referral or direct access interventions. Although adverse events were outcome measures extracted from the studies in this review, we believed that they also were indicative of comprehensive reporting. A point. was not awarded if a study made no mention of the presence or absence of adverse events (eg, loss of license of a therapist, minor or serious side effects of intervention) in the direct access or physician referral groups. |
| 9 | Have the characteristics of patients lost to follow-up been described? | The authors of this tool indicated that this question should be answered "yes" where there were no losses to follow-up or where losses to follow-up were small that findings would have been unaffected by their inclusion. For the purposes of this review, a point was awarded if a study explicitly reported that there were no losses to follow-up or if the losses to follow-up accounted for a maximum of 10% of the sample of participants originally enrolled in the study (or up to 5% of the original number of participants assigned to each direct access and physician referral group). No point was awarded if the study did not report the number of patients lost to follow-up or this information could not be obtained from the tables, figures, or text of the study. |
| 10 | Have actual probability values been reported (eg, .035 rather than <.05) for the main outcomes, except where the probability value is less than .001? | A point was awarded if the exact P value was provided for both statistically significant and nonsignificant results for at least the main outcome measures. A point was not awarded if a study simply indicated that the results for the main outcome measures were not significant without providing the exact P value. |
| External Validity | ||
| 11 | Were the individuals asked to participate in the study representative of the entire population from which they were recruited? | A point was awarded if the study identified the source population for patients and described how the patients were selected. Patients were determined to be representative if they comprised the entire source population, an unselected sample of consecutive patients, or a random sample (only feasible where a list of all members of the relevant population exists). Where a study red not report the proportion of the source population horn which the patients are derived, the question was answered as unable to determine. |
| 12 | Were those individuals who were prepared to participate representative of the entire population from which they were recruited? | The proportion of those asked who agreed to participate or responded should be stated. Validation that the sample was representative would include demonstrating that the distribution of the main confounding factors was the same in the study sample and the source population (eg, if the demographics and diagnoses of the patients were considered representative of a typical outpatient moo practice, the study was awarded a point). No point was awarded if the proportion of those asked who agreed to participate or responded was not stated. |
| 13 | Were the staff, places, and faculties where the patients were treated representative of the treatment the majority of patients receive? | A point was awarded unless the study specifically stated that patients were treated by a therapist who received specialized training or the direct access or physician referral group received treatment in a specialized facility defined by advanced training or focus of intervention in “niche” areas of physical therapy (eg, pediatrics). |
| Internal Validity—Bias | ||
| 14 | Was an attempt made to blind study participants to the intervention they received? | A point was awarded if the patients were not aware of, or would have no way of knowing (as in the case of retrospective studies), which intervention they received. The study was not awarded a point if it was prospective and failed to mention whether the patients had knowledge of whether they were assigned to the direct access or physician referral group. |
| 15 | Was an attempt made to blind those measuring the main outcomes of the intervention? | A point was awarded if the study specifically stated that those assessing the outcome measures were unaware of (or would have no way of knowing) whether the patients were in the direct access or physician referral group. |
| 16 | If any of the results of the study were based on "data dredging," was this made clear? | A point was awarded if no retrospective unplanned (at the outset of the study) subgroup analyses were reported. |
| 17 | In trials and cohort studies, do the analyses adjust for different lengths of follow-up of patients, or, in case-control studies, is the time period between the intervention and outcome the same for cases and controls, | For the purposes of this review, this question was omitted due to reasons previously stated. |
| 18 | Were the statistical tests used to assess the main outcomes appropriate, | If the distribution of the data (normal or not) was not described, it was assumed that the estimates used were appropriate, and a point was awarded. No point was awarded for studies that reported qualitative or quantitative data without any form of statistical comparisons or if the statistical tests reported were not appropriate. |
| 19 | Was adherence to the intervention reliable? | If the authors in prospective studies reported nonadherence to physical therapy intervention or adherence could not be determined, the study was not awarded a point. In retrospective studies, data were collected only for those patients who completed their episode of care (adherence to physical therapy assumed), and a point was awarded. For studies where the effect of any nonadherence was likely to bias any association to the null, the study received a point. |
| 20 | Were the main outcome measures used accurate (valid and reliable)? | A point was awarded if the primary outcome measures were thought to be valid and reliable (eg, number of physical therapy visits per chart report), regardless of whether reliability or validity was reported. A point was not awarded if at least one of the primary outcome measures in the study was not valid or reliable or if this information was not reported or could not be determined (ie, a questionnaire without reported validity or reliability). |
| Internal Validity-Confounding (Selection Bias) | ||
| 21 | Were the patients in different intervention groups (trials and cohort studies), or were the cases and controls (case-control studies) recruited from the same population? | A point was awarded when participants from both direct access and physician referral groups were recruited from the same population. Otherwise, a point was not awarded (eg, a point was not awarded when all participants from the physician referral group received care at clinic A and all participants in the direct access group received care at clinic B, because they could have represented 2 distinct populations). |
| 22 | Were study participants in different intervention groups (trials and cohort studies), or were the cases and controls (case-control studies) recruited over the same period of time? | A point was awarded when the study provided a specific time line for patient recruitment (prospective studies) or when data were collected between reported dates of patient care (retrospective studies). |
| 23 | Were study participants randomized to intervention groups? | A point for random allocation was awarded if random allocation of patients was stated in the "Method" section of the article. The precise method of randomization need not be specified. Quasi-randomization allocation procedures, such as allocation by bed availability, did not satisfy this criterion. For crossover study designs, a point was awarded when participants were randomly allocated in the order in which treatments were received. |
| 24 | Was the randomized intervention assignment concealed from both patients and health care team until recruitment was complete and irrevocable? | The study did not receive a point unless the participants were randomly allocated and the methods for ensuring random allocation were specified. |
| 25 | Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? | A point was awarded unless the effect of the main confounders was not investigated or confounding was demonstrated, but no adjustment was made in the final analyses. |
| 26 | Were losses of patients to follow-up taken into account? | A point was awarded as long as the number of dropouts lost to follow-up accounted for less than 10% of the initial number of total participants or a maximum of 5% from each group. The question was answered with "unable to determine" if the number of patients lost to follow-up were not reported or could not be deduced from the outcome data (le, initial and final sample sizes not indicated). |
| Power | ||
| 27 | Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is less than .05? | For the purposes of this evidence-based review, this question was omitted. |
For original criteria, refer to Downs and Black.17
Appendix 2
One Method of Calculating Differences in Cost Between Direct Access and Physician-Referred Episodes of Care
In the event that third-party payers want to calculate differences in cost between direct access and referred episodes of care in their own records, one potential way cited previously.11 is listed below:
|
In the event that third-party payers want to calculate differences in cost between direct access and referred episodes of care in their own records, one potential way cited previously.11 is listed below:
|
One Method of Calculating Differences in Cost Between Direct Access and Physician-Referred Episodes of Care
In the event that third-party payers want to calculate differences in cost between direct access and referred episodes of care in their own records, one potential way cited previously.11 is listed below:
|
In the event that third-party payers want to calculate differences in cost between direct access and referred episodes of care in their own records, one potential way cited previously.11 is listed below:
|
Author notes
Dr Ojha and Dr Davenport provided concept/idea/research design, writing, data collection, project management, and fund procurement. All authors provided data analysis and consultation (including review of manuscript before submission). The authors thank Eugene Komaroff and Elizabeth Frank for reviewing the manuscript.


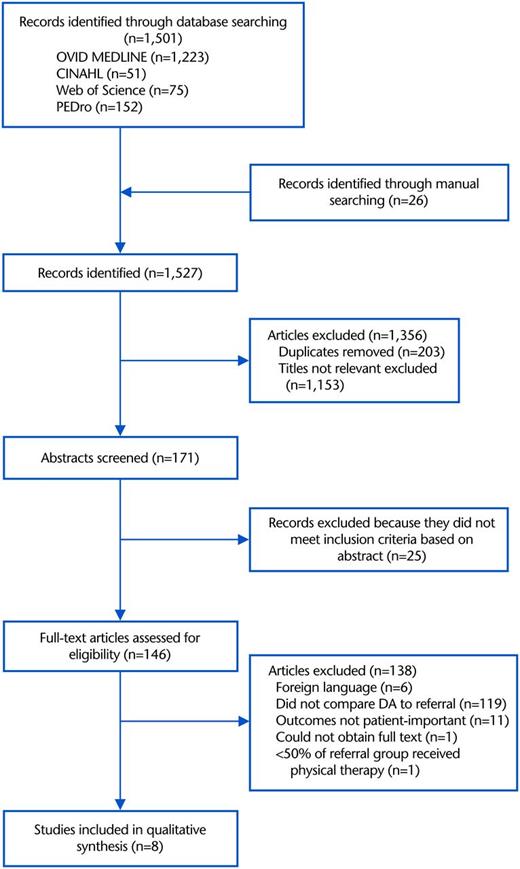

Comments