-
PDF
- Split View
-
Views
-
Cite
Cite
Ilona J.M. de Rooij, Ingrid G.L. van de Port, Jan-Willem G. Meijer, Effect of Virtual Reality Training on Balance and Gait Ability in Patients With Stroke: Systematic Review and Meta-Analysis, Physical Therapy, Volume 96, Issue 12, 1 December 2016, Pages 1905–1918, https://doi.org/10.2522/ptj.20160054
Close - Share Icon Share
Abstract
Virtual reality (VR) training is considered to be a promising novel therapy for balance and gait recovery in patients with stroke.
The aim of this study was to conduct a systematic literature review with meta-analysis to investigate whether balance or gait training using VR is more effective than conventional balance or gait training in patients with stroke.
A literature search was carried out in the databases PubMed, Embase, MEDLINE, and Cochrane Library up to December 1, 2015.
Randomized controlled trials that compared the effect of balance or gait training with and without VR on balance and gait ability in patients with stroke were included.
Twenty-one studies with a median PEDro score of 6.0 were included. The included studies demonstrated a significant greater effect of VR training on balance and gait recovery after stroke compared with conventional therapy as indicated with the most frequently used measures: gait speed, Berg Balance Scale, and Timed “Up & Go” Test. Virtual reality was more effective to train gait and balance than conventional training when VR interventions were added to conventional therapy and when time dose was matched.
The presence of publication bias and diversity in included studies were limitations of the study.
The results suggest that VR training is more effective than balance or gait training without VR for improving balance or gait ability in patients with stroke. Future studies are recommended to investigate the effect of VR on participation level with an adequate follow-up period. Overall, a positive and promising effect of VR training on balance and gait ability is expected.
Many patients with stroke experience sensory, motor, cognitive, and visual impairments, which all have an impact on their ability to perform daily life activities.1,2 Approximately 80% of patients with stroke are affected by motor impairment, which represents loss and limitation in muscle strength and coordination. Motor impairment in the legs greatly affects balance and walking ability.3 In a study by Pollock et al,4 approximately 88% of all patients with stroke who were discharged from hospital reported insufficient walking ability. In addition, 26% to 33% of the home-dwelling patients with stroke were still unable to walk unsupervised in the community,5–7 presumably mainly because of difficulties with negotiating stairs, inclines, or unlevel surfaces.6,7 Therefore, gait recovery has been recognized as an important goal in stroke rehabilitation.8–10
Impaired gait is highly associated with balance dysfunction.4,11 In addition, improvement in balance has been shown to be the most important determinant for regaining gait as measured with the Functional Ambulation Categories.12 During balance and gait recovery, patients with stroke have to relearn voluntary control over the affected muscles. In conventional therapy, this relearning is done through physical therapy and occupational therapy, which focus on high-intensity, repetitive, and task-specific practice.3,13 High-intensity, repetitive, task-oriented, and task-specific practice has proven to be important for effective therapy in all stages after stroke.14 However, the conventional rehabilitation techniques are often labor- and resource-intensive, tedious, and result most of the time in modest and delayed effects in patients with stroke.13 In addition, the frequency and intensity of the conventional therapies as performed in clinical practice have been found to be insufficient to achieve maximum recovery.14,15
In recent years, the use of virtual reality (VR) has been introduced in the field of stroke rehabilitation.16 Virtual reality is an advanced computer-human interface with a variety of safe 3-dimensional environments in which patients with stroke can perform real-time tasks and anticipate and react to objects or events.13,17,18 It has been shown that VR can improve upper extremity motor function in adults with chronic hemiparesis as a result from a stroke.18 It also is thought that VR contributes to positive changes in neural organization and walking ability.19
Multiple recent systematic reviews about the effect of VR training supported the use of VR in lower extremity stroke rehabilitation to improve balance and gait ability.9,20–23 Two of these reviews9,21 lacked a meta-analysis, and the majority of the studies did not perform subanalyses of the results (eg, by making a division between studies in which VR was time dose matched to conventional therapy and studies in which VR training was additional to conventional therapy). The most recent review about the effect of VR training on balance and gait ability showed significant benefits of VR training on gait speed, Berg Balance Scale (BBS) scores, and Timed “Up & Go” Test (TUG) scores when VR was time dose matched to conventional therapy.22 In contrast to the studies supporting VR training, 2 recently published reviews using a commercial VR system concluded that there was insufficient evidence to ensure the effectiveness of VR training on balance ability.24,25 However, in the past year, new randomized controlled trials (RCTs) comparing the effect of VR training with conventional therapy have been published. Because of the inconclusive results in the previous reviews about the effect of VR training, the important question remains whether VR interventions are more effective than balance or gait training without VR in patients with stroke.9 Therefore, the questions that are addressed in the present review are: (1) Are VR interventions to train gait or balance more effective than conventional gait or balance training on balance and gait ability in patients with stroke when time dose is matched? and (2) Are VR interventions in addition to conventional therapy more effective than conventional therapy alone in improving balance and gait ability in patients with stroke?
Method
Data Sources and Searches
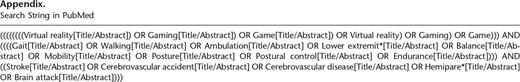
A literature search was carried out using the databases PubMed (since 1950), Embase (since 1974), MEDLINE (since 1946), and Cochrane Library (since 1993) from inception until December 1, 2015. Search terms included key words related to VR (eg, “game,” “gaming”), stroke (“cerebrovascular accident/disease,” “brain attack”), balance (“posture,” “postural control,” “mobility”), or gait (“ambulation,” “walking,” “lower extremity,” “endurance”). These terms were used as key words in the title and abstract in all databases. In PubMed, terms related to virtual reality also were searched in the full text. The search strategy used in PubMed is provided in the Appendix. The titles and abstracts were displayed and screened by 2 reviewers to identify relevant studies.
Study Selection
Only RCTs that compared the effect of gait or balance training without VR with the effect of gait or balance training with VR in patients with stroke were included. The VR intervention replaced the conventional therapy or was in addition to the conventional therapy. For inclusion, RCTs had to be peer-reviewed articles and written in the Dutch, German, or English language. Studies that compared VR interventions with no intervention or form of therapy were excluded. Gait ability could be measured using parameters of spatiotemporal gait ability, functional gait ability, or both, and balance ability could be measured using static and dynamic balance parameters. Furthermore, VR had to consist of a screen or a head-mounted device. The patients with stroke had to perform gait or balance exercises on the ground, a balance board, or a treadmill while looking at the VR scenes. This approach means that studies using robots or standing frames were excluded.
Data Extraction and Quality Assessment
The following data were extracted from the included articles: sex, age, time since stroke, content of intervention, time dose of training, and significant main findings in measures of balance and gait ability between groups. Data extraction was performed by 2 independent researchers (I.R., I.P.). They assessed the methodological quality of the RCTs using the PEDro scale.26 This scale consists of 11 items that can contribute 1 point to the total score if they are satisfied, except for item 1 (eligibility criteria), which is scored “yes” or “no.” The PEDro scale is proven to have sufficient reliability to determine the quality of RCTs. Articles with a score of 6 or higher are considered as high quality, and those with scores of less than 6 are defined as lower quality.27 In case of disagreement in the quality assessment of the 2 reviewers, consensus was reached by discussion or consulting a third person. Publication bias was analyzed using forest plots for the measures gait speed and TUG.
Data Synthesis and Analysis
The included studies were analyzed based on participant characteristics, outcome parameters, content of VR interventions, and main findings. A meta-analysis of studies with a PEDro score of 6 or higher was performed using Review Manager software, version 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).28 The pooled effect estimates were computed from the change scores between baseline and end of the intervention, their standard deviations, and the number of participants. Authors were contacted via email for unreported data. Missing standard deviations of the change values in the studies of Barcala et al29 and Rajaratnam et al30 were imputed from other published literature. Other standard deviations of change values that were still not available after mail contact were estimated using the difference in means and P value, t value, or F value as described in the Cochrane Handbook.31
In case of low heterogeneity, the fixed-effect model was used to pool study results for the outcomes BBS, TUG, and gait speed. When significant heterogeneity was observed (I2 >50%), the random-effects model was applied. In addition, a sensitivity analysis was conducted when heterogeneity was present. Forest plots were generated to present the pooled effect, and the mean difference (MD) with 95% confidence interval (CI) was calculated for the BBS and TUG outcomes. For the outcome gait speed, the standardized mean difference (SMD) was expressed because this outcome was obtained through multiple measurement scales. A distinction was made between studies in which the VR intervention replaced the conventional therapy (time dose matched) and studies in which the VR intervention was added to the conventional therapy.
Results
Identification of Studies
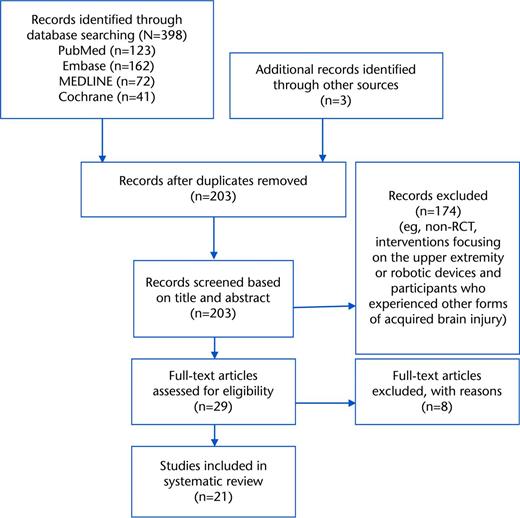
In total, 398 relevant articles were found in PubMed, Embase, MEDLINE, and Cochrane Library. In addition, 3 articles29,32,33 were identified through hand searching reference lists. When duplicates were removed, 203 articles remained. Based on title and abstract of these 203 articles, 174 articles were excluded (Fig. 1). The main reasons for excluding these articles were study designs other than RCTs, interventions focusing on the upper extremity or robotic devices, and participants who experienced other forms of acquired brain injury. Furthermore, 8 articles were excluded based on the full-text article. Two of these studies did not involve randomization,34,35 1 study lacked a control group,36 and 4 studies contained a control group that did not receive conventional therapy37 or a control group that also watched at a VR screen38,39 or played VR at home.40 Another reason for exclusion was VR training that did not involve balance or gait training.41 Eventually, 21 articles were included in the review.
Flowchart of the study selection. RCT=randomized controlled trial.
Description of Included Studies
In the 21 included studies, the mean age of the participants varied between 45.9 and 65.9 years in the VR group and 46.3 and 65.7 years in the control group. Time since stroke ranged between 12.7 days and 11.3 years in the VR group and between 13.2 days and 11.6 years in the control group. Eight studies8,32,42–47 were treadmill based and provided a VR intervention in combination with walking. The other 13 studies focused on balance interventions by performing exercises on the ground16,48–53 or a balance board.29,30,33,54–56 The focus of the balance interventions was on the lower extremities. In the study by Song et al,50 however, the upper extremity was involved more directly because the participants had to accomplish tasks with their arms in order to direct their center of pressure outside the feet. In 17 studies8,30,32,33,42–49,51–53,55,56 the time dose of therapy in the VR and control groups was equal. In 4 studies,16,29,50,54 the participants in the VR group performed the VR intervention in addition to a conventional therapy program, which means that the time dose of therapy was higher in the VR group compared with the control group (Tab. 1). The additional training of the VR group in these studies varied between 6029 and 12016 minutes a week.
Characteristics of the Selected Studies and Analysis of Outcome Measures and of Gait Ability and Balance and Main Findingsa
| Study . | N (Male) . | Mean Age (SD) (y) . | Time Since Stroke (SD) . | VR Intervention . | Control Intervention . |
|---|---|---|---|---|---|
| Givon et al,52 2016 | 47 (28) | VR group: 56.7 (9.3) Control group: 62.0 (9.3) | VR group: 3.0 (1.8) y Control group: 2.6 (1.8) y | VR group training | Conventional group therapy |
| Kim et al,47 2015 | 17 (9) | VR group: 56.2 (7.56) Control group: 48.7 (9.3) | VR group: 7.5 (4.4) mo Control group: 16.6 (8.8) mo | Conventional therapy plus VR-based treadmill training | Conventional therapy |
| Lee et al,55 2015 | 24 (16) | VR group: 45.9 (12.3) Control group: 49.2 (12.9) | nr | Conventional therapy plus VR training | Conventional therapy plus task-oriented training |
| Lee et al,55 2015 | 20 (11) | VR group: 57.2 (9.2) Control group: 52.7 (11.7) | nr | VR training with cognitive tasks | PNF exercise program |
| Llorens et al,49 2015 | 20 (9) | VR group: 58.3 (11.6) Control group: 55.0 (11.6) | VR group: 407.5 (232.4) d Control group: 587 (222.1) d | Conventional therapy plus VR therapy | Conventional therapy |
| Song et al,53 2015 | 40 (22) | VR group: 51.4 (40.6) Control group: 50.1 (7.8) | VR group: 14.8 (6.1) mo Control group: 14.3 (3.4) mo | VR training | Ergometer bicycle training |
| Cho et al,43 2014 | 30 (15) | VR group: 65.9 (5.7) Control group: 63.5 (5.5) | VR group: 414.5 (150.4) d Control group: 460.3 (186.8) d | Conventional therapy plus VR-based treadmill training | Conventional therapy plus traditional non-VR treadmill training |
| Hung et al,33 2014 | 28 (18) | VR group: 55.4 (10.0) Control group: 53.4 (10.0) | VR group: 21.0 (11.3) mo Control group: 15.9 (8.0) mo | Conventional therapy plus VR training | Conventional therapy plus weight-shift training |
| Morone et al,51 2014 | 50 (nr) | VR group: 58.4 (9.6) Control group: 62.0 (10.3) | VR group: 61.0 (36.5) d Control group: 41.7 (36.9) d | Conventional therapy plus VR therapy | Conventional therapy plus extra balance therapy |
| Song et al,59 2014 | 20 (11) | VR group: 65.6 (13.5) Control group: 61.2 (13.8) | VR group: 12.7 (3.2) d Control group: 13.2 (3.4) d | Conventional therapy plus VR training | Conventional therapy |
| Barcala et al,29 2013 | 20 (9) | VR group: 65.2 02.5) Control group: 63.5 (14.5) | VR group: 12.3 (7.1) mo Control group: 15.2 (6.6) mo | Conventional therapy plus VR training | Conventional therapy |
| Cho et al,42 2013 | 14 (7) | VR group: 64.6 (4.4) Control group: 65.1 (4.7) | VR group: 288.3 (69.2) d Control group: 312.4 (83.7) d | Conventional therapy plus VR-based treadmill training | Conventional therapy plus traditional non-VR treadmill training |
| Park et al,” 2013 | 16 (11) | VR group: 48.8 (8.8) Control group: 46.3 (6.8) | VR group: 11.3 (4.5) y Control group: 11.6 (4.4) y | Conventional therapy plus reality-based training | Conventional therapy |
| Givon et al,52 2016 | Equal | Functional: 10MWT | ns | ||
| Kim et al,47 2015 | Equal | Static balance: PSPL (AP, ML, and total), APSS | PSPL (AP, ML, and total), APSS (P<.05) | ||
| Lee et al,55 2015 | Equal | Static balance: COP path length, COP velocity Dynamic balance: FRT | FRT (P<.0001) | ||
| Lee et al,55 2015 | Equal | Dynamic balance: BBS, TUG | BBS, TUG (P<.05) | ||
| Lloréns et al,49 2015 | Equal | Functional: 10MWT | 1OMWT (P<.05) | Dynamic balance: BBS, Tinetti POMA, Brunel Balance Assessment | BBS (P<.05) |
| Song et al,53 2015 | Equal | Functional: 10MWT | 10MWT (P<.05) | Static balance: weight- bearing ratio affected side, forward and backward LOS Dynamic balance: TUG | Weight-bearing ratio affected side, forward and backward LOS, TUG (P<.05) |
| Cho et al,43 2014 | Equal | Spatiotemporal: gait speed, cadence, step length, stride length, double-limb support period, single-limb support period | Gait speed, cadence, single- and double-limb support period, step and stride length (P<.029) | Static balance: AP-PSV, ML-PSV, PSVM Dynamic balance: BBS, TUG | BBS, TUG (P=.001) |
| Hung et al,33 2014 | Equal | Static balance: SI, weight-bearing asymmetry on affected leg Dynamic balance: TUG, FRT | SI (P‹.05) | ||
| Morone et al,51 2014 | Equal | Functional: 10MWT, FAC | 10MWT (P=.021) | Dynamic balance: BBS | BBS (P=.004) |
| Song et al,50 2014 | Higher | Static balance: Fl scores, SI, WDI Dynamic balance: BBS | SI and WDI while standing with eyes open and when standing on a pillow with eyes open (P‹.017) | ||
| Barcala et al,29 2013 | Higher | Dynamic balance: BBS, TUG Static balance: COP oscillations | ns | ||
| Cho et al,42 2013 | Equal | Spatiotemporal: gait speed, cadence, paretic side step length, stride length, and single-limb support period | Gait speed, cadence (P=.01) | Dynamic balance: BBS, TUG | BBS, TUG (P=.01) |
| Park et al,48 2013 | Equal | Spatiotemporal: gait speed, cadence, step length, stride length Functional: 10MWT | Stride length (P<.03) | ||
| Rajaratnam et al,30 2013 | Equal | Static balance: CoP sway Dynamic balance: BBS, TUG, FRT | FRT (P=.01) | ||
| Cho et al,54 2012 | Higher | Static balance: AP-PSV and ML-PSV (with eyes open or closed) Dynamic balance: BBS, TUG | BBS, TUG (P<.05) | ||
| Jung et al,44 2012 | Equal | Dynamic balance: TUG, ABC scale | TUG, ABC (P<.05) | ||
| Kang et al,32 2012 | Equal | Functional: 6MWT, 10MWT | 6MWT, 10MWT (P<.05) | Dynamic balance: TUG, FRT | VR group vs control group 1: TUG (P<.05) VR group vs control group 2: TUG, FRT (P<.05) |
| Yang et al,46 2011 | Equal | Static balance: COPML, COPAP, COPE, COPA, symmetry index (quiet stance and sit-to-stand transfer), COPE/P (sitto-stand transfer) stance time/P, step no./P, contact A/P (level walking) | COPML (P=.038) | ||
| Kim et al,16 2009 | Higher | Spatiotemporal: cadence, step time, stance time, swing time, single/double support time, step/stride length Functional: 10MWT, MMAS | Cadence, step length, step time (P<.014) | Static balance: mean balance, sway area, sway path, maximal velocity Dynamic balance: BBS, AP angle, ML angle | BBS, AP angle, and ML angle (P<.01) |
| Yang et al,8 2008 | Equal | Functional: 10MWT, community walking time, WAQ | Pretest-posttest: 10MWT, community walking time (P<.05) Follow-up: WAQ (P=.03) | Dynamic balance: ABC scale | ns |
| Jaffe et al,45 2004 | Equal | Spatiotemporal: gait speed, cadence, step and stride length Functional: obstacle test, distance on 6MWT | Gait speed, stride length (ss), obstacle clearance, step length of nonparetic leg (ss) and paretic leg (fs) (P<.05) | ||
| Rajaratnam et al,30 2013 | 19 (7) | VR group: 58.7 (8.6) Control group: 65.3 (9.6) | VR group: 14.7 (7.5) d Control group: 15.2 (6.3) d | Conventional therapy plus VR balance training | Conventional therapy |
| Cho et al,54 2012 | 22 (14) | VR group: 65.3 (8.4) Control group: 63.1 (6.9) | VR group: 12.5 (2.6) mo Control group: 12.6 (2.5) mo | Conventional therapy plus VR balance training | Conventional therapy |
| Jung et al,44 2012 | 21 (13) | VR group: 60.5 (8.6) Control group: 63.6 (5.1) | VR group: 12.6 (3.3) mo Control group: 15.4 (4.7) mo | VR treadmill training | Non-VR treadmill training |
| Kang et al,32 2012 | 30 (15) | VR group: 55.9 (6.4) Control group 1: 56.3 (7.6) Control group 2: 56.1 (7.8) | VR group: 14.1 (4.4) mo Control group 1: 13.5 (4.0) mo Control group 2: 15.1 (7.4) mo | Conventional therapy plus VR treadmill training | Conventional therapy plus non-VR treadmill training (control group 1) or stretching exercises (control group 2) |
| Yang et al,46 2011 | 14 (nr) | VR group: 56.3 (10.2) Control group: 65.7 (5.9) | VR group: 17.0 (8.6) mo Control group: 16.3 (10.4) mo | VR treadmill training | Non-VR treadmill training |
| Kim et al,16 2009 | 24 (14) | VR group: 52.4 (10.1) Control group: 51.75 (7.1) | VR group: 25.9 (10.0) mo Control group: 24.3 (8.9) mo | Conventional therapy plus VR therapy | Conventional therapy |
| Yang et al,8 2008 | 20 (10) | VR group: 55.5 (12.2) Control group: 60.9 (9.3) | VR group: 5.9 (4.2) y Control group: 6.1 (10.3) y | VR treadmill training | Non-VR treadmill training |
| Jaffe et al,45 2004 | 20 (12) | VR group: 58.2 (11.2) Control group: 63.2 (8.3) | VR group: 3.9 (2.3) y Control group: 3.6 (2.6) y | Virtual object training | Stepping over real foam objects on a 10-m walkway |
| Study . | N (Male) . | Mean Age (SD) (y) . | Time Since Stroke (SD) . | VR Intervention . | Control Intervention . |
|---|---|---|---|---|---|
| Givon et al,52 2016 | 47 (28) | VR group: 56.7 (9.3) Control group: 62.0 (9.3) | VR group: 3.0 (1.8) y Control group: 2.6 (1.8) y | VR group training | Conventional group therapy |
| Kim et al,47 2015 | 17 (9) | VR group: 56.2 (7.56) Control group: 48.7 (9.3) | VR group: 7.5 (4.4) mo Control group: 16.6 (8.8) mo | Conventional therapy plus VR-based treadmill training | Conventional therapy |
| Lee et al,55 2015 | 24 (16) | VR group: 45.9 (12.3) Control group: 49.2 (12.9) | nr | Conventional therapy plus VR training | Conventional therapy plus task-oriented training |
| Lee et al,55 2015 | 20 (11) | VR group: 57.2 (9.2) Control group: 52.7 (11.7) | nr | VR training with cognitive tasks | PNF exercise program |
| Llorens et al,49 2015 | 20 (9) | VR group: 58.3 (11.6) Control group: 55.0 (11.6) | VR group: 407.5 (232.4) d Control group: 587 (222.1) d | Conventional therapy plus VR therapy | Conventional therapy |
| Song et al,53 2015 | 40 (22) | VR group: 51.4 (40.6) Control group: 50.1 (7.8) | VR group: 14.8 (6.1) mo Control group: 14.3 (3.4) mo | VR training | Ergometer bicycle training |
| Cho et al,43 2014 | 30 (15) | VR group: 65.9 (5.7) Control group: 63.5 (5.5) | VR group: 414.5 (150.4) d Control group: 460.3 (186.8) d | Conventional therapy plus VR-based treadmill training | Conventional therapy plus traditional non-VR treadmill training |
| Hung et al,33 2014 | 28 (18) | VR group: 55.4 (10.0) Control group: 53.4 (10.0) | VR group: 21.0 (11.3) mo Control group: 15.9 (8.0) mo | Conventional therapy plus VR training | Conventional therapy plus weight-shift training |
| Morone et al,51 2014 | 50 (nr) | VR group: 58.4 (9.6) Control group: 62.0 (10.3) | VR group: 61.0 (36.5) d Control group: 41.7 (36.9) d | Conventional therapy plus VR therapy | Conventional therapy plus extra balance therapy |
| Song et al,59 2014 | 20 (11) | VR group: 65.6 (13.5) Control group: 61.2 (13.8) | VR group: 12.7 (3.2) d Control group: 13.2 (3.4) d | Conventional therapy plus VR training | Conventional therapy |
| Barcala et al,29 2013 | 20 (9) | VR group: 65.2 02.5) Control group: 63.5 (14.5) | VR group: 12.3 (7.1) mo Control group: 15.2 (6.6) mo | Conventional therapy plus VR training | Conventional therapy |
| Cho et al,42 2013 | 14 (7) | VR group: 64.6 (4.4) Control group: 65.1 (4.7) | VR group: 288.3 (69.2) d Control group: 312.4 (83.7) d | Conventional therapy plus VR-based treadmill training | Conventional therapy plus traditional non-VR treadmill training |
| Park et al,” 2013 | 16 (11) | VR group: 48.8 (8.8) Control group: 46.3 (6.8) | VR group: 11.3 (4.5) y Control group: 11.6 (4.4) y | Conventional therapy plus reality-based training | Conventional therapy |
| Givon et al,52 2016 | Equal | Functional: 10MWT | ns | ||
| Kim et al,47 2015 | Equal | Static balance: PSPL (AP, ML, and total), APSS | PSPL (AP, ML, and total), APSS (P<.05) | ||
| Lee et al,55 2015 | Equal | Static balance: COP path length, COP velocity Dynamic balance: FRT | FRT (P<.0001) | ||
| Lee et al,55 2015 | Equal | Dynamic balance: BBS, TUG | BBS, TUG (P<.05) | ||
| Lloréns et al,49 2015 | Equal | Functional: 10MWT | 1OMWT (P<.05) | Dynamic balance: BBS, Tinetti POMA, Brunel Balance Assessment | BBS (P<.05) |
| Song et al,53 2015 | Equal | Functional: 10MWT | 10MWT (P<.05) | Static balance: weight- bearing ratio affected side, forward and backward LOS Dynamic balance: TUG | Weight-bearing ratio affected side, forward and backward LOS, TUG (P<.05) |
| Cho et al,43 2014 | Equal | Spatiotemporal: gait speed, cadence, step length, stride length, double-limb support period, single-limb support period | Gait speed, cadence, single- and double-limb support period, step and stride length (P<.029) | Static balance: AP-PSV, ML-PSV, PSVM Dynamic balance: BBS, TUG | BBS, TUG (P=.001) |
| Hung et al,33 2014 | Equal | Static balance: SI, weight-bearing asymmetry on affected leg Dynamic balance: TUG, FRT | SI (P‹.05) | ||
| Morone et al,51 2014 | Equal | Functional: 10MWT, FAC | 10MWT (P=.021) | Dynamic balance: BBS | BBS (P=.004) |
| Song et al,50 2014 | Higher | Static balance: Fl scores, SI, WDI Dynamic balance: BBS | SI and WDI while standing with eyes open and when standing on a pillow with eyes open (P‹.017) | ||
| Barcala et al,29 2013 | Higher | Dynamic balance: BBS, TUG Static balance: COP oscillations | ns | ||
| Cho et al,42 2013 | Equal | Spatiotemporal: gait speed, cadence, paretic side step length, stride length, and single-limb support period | Gait speed, cadence (P=.01) | Dynamic balance: BBS, TUG | BBS, TUG (P=.01) |
| Park et al,48 2013 | Equal | Spatiotemporal: gait speed, cadence, step length, stride length Functional: 10MWT | Stride length (P<.03) | ||
| Rajaratnam et al,30 2013 | Equal | Static balance: CoP sway Dynamic balance: BBS, TUG, FRT | FRT (P=.01) | ||
| Cho et al,54 2012 | Higher | Static balance: AP-PSV and ML-PSV (with eyes open or closed) Dynamic balance: BBS, TUG | BBS, TUG (P<.05) | ||
| Jung et al,44 2012 | Equal | Dynamic balance: TUG, ABC scale | TUG, ABC (P<.05) | ||
| Kang et al,32 2012 | Equal | Functional: 6MWT, 10MWT | 6MWT, 10MWT (P<.05) | Dynamic balance: TUG, FRT | VR group vs control group 1: TUG (P<.05) VR group vs control group 2: TUG, FRT (P<.05) |
| Yang et al,46 2011 | Equal | Static balance: COPML, COPAP, COPE, COPA, symmetry index (quiet stance and sit-to-stand transfer), COPE/P (sitto-stand transfer) stance time/P, step no./P, contact A/P (level walking) | COPML (P=.038) | ||
| Kim et al,16 2009 | Higher | Spatiotemporal: cadence, step time, stance time, swing time, single/double support time, step/stride length Functional: 10MWT, MMAS | Cadence, step length, step time (P<.014) | Static balance: mean balance, sway area, sway path, maximal velocity Dynamic balance: BBS, AP angle, ML angle | BBS, AP angle, and ML angle (P<.01) |
| Yang et al,8 2008 | Equal | Functional: 10MWT, community walking time, WAQ | Pretest-posttest: 10MWT, community walking time (P<.05) Follow-up: WAQ (P=.03) | Dynamic balance: ABC scale | ns |
| Jaffe et al,45 2004 | Equal | Spatiotemporal: gait speed, cadence, step and stride length Functional: obstacle test, distance on 6MWT | Gait speed, stride length (ss), obstacle clearance, step length of nonparetic leg (ss) and paretic leg (fs) (P<.05) | ||
| Rajaratnam et al,30 2013 | 19 (7) | VR group: 58.7 (8.6) Control group: 65.3 (9.6) | VR group: 14.7 (7.5) d Control group: 15.2 (6.3) d | Conventional therapy plus VR balance training | Conventional therapy |
| Cho et al,54 2012 | 22 (14) | VR group: 65.3 (8.4) Control group: 63.1 (6.9) | VR group: 12.5 (2.6) mo Control group: 12.6 (2.5) mo | Conventional therapy plus VR balance training | Conventional therapy |
| Jung et al,44 2012 | 21 (13) | VR group: 60.5 (8.6) Control group: 63.6 (5.1) | VR group: 12.6 (3.3) mo Control group: 15.4 (4.7) mo | VR treadmill training | Non-VR treadmill training |
| Kang et al,32 2012 | 30 (15) | VR group: 55.9 (6.4) Control group 1: 56.3 (7.6) Control group 2: 56.1 (7.8) | VR group: 14.1 (4.4) mo Control group 1: 13.5 (4.0) mo Control group 2: 15.1 (7.4) mo | Conventional therapy plus VR treadmill training | Conventional therapy plus non-VR treadmill training (control group 1) or stretching exercises (control group 2) |
| Yang et al,46 2011 | 14 (nr) | VR group: 56.3 (10.2) Control group: 65.7 (5.9) | VR group: 17.0 (8.6) mo Control group: 16.3 (10.4) mo | VR treadmill training | Non-VR treadmill training |
| Kim et al,16 2009 | 24 (14) | VR group: 52.4 (10.1) Control group: 51.75 (7.1) | VR group: 25.9 (10.0) mo Control group: 24.3 (8.9) mo | Conventional therapy plus VR therapy | Conventional therapy |
| Yang et al,8 2008 | 20 (10) | VR group: 55.5 (12.2) Control group: 60.9 (9.3) | VR group: 5.9 (4.2) y Control group: 6.1 (10.3) y | VR treadmill training | Non-VR treadmill training |
| Jaffe et al,45 2004 | 20 (12) | VR group: 58.2 (11.2) Control group: 63.2 (8.3) | VR group: 3.9 (2.3) y Control group: 3.6 (2.6) y | Virtual object training | Stepping over real foam objects on a 10-m walkway |
nr=not reported, ns= nonsignificant, 6MWT=Six-Minute Walk Test, 10MWT=10-Meter Walk Test, ABC=Activities-specific Balance Confidence, AP=anterior-posterior, AP-PSV=anterior-posterior postural sway velocity, AP and ML angle=angle between a vertical line from the spatial center of the supporting feet and a second line connecting from the same point to the individual’s center of gravity, APSS=average postural sway speed, BBS=Berg Balance Scale, contact A/P=contact area of the paretic limb, COP=center of pressure, COPA=center of pressure sway area, COPAP=center of pressure displacement in anterior-posterior direction, COPE=center-of-pressure total path excursion, COPE/P=center-of-pressure path excursion under the paretic limb, COPML=center-of-pressure displacement in medial-lateral direction, Fl=falling index, fast=as fast as possible pace, FAC=Functional Ambulation Categories, FRT=Functional Reach Test, ML=medial-lateral, ML-PSV=medial-lateral postural sway velocity, MMAS=Modified Motor Assessment Scale, POMA=Performance-Oriented Mobility Assessment, PSPL=postural sway path length, PSVM=postural sway velocity moment, Sl=stability index, ss=selfselected pace, stance time/P=stance time of the paretic limb, LOS=limit of stability, step no./=step number of the paretic limb, TUG=Timed “Up & Go” Test, WAQ=Walking Ability Questionnaire, WDI=weight distribution index.
Characteristics of the Selected Studies and Analysis of Outcome Measures and of Gait Ability and Balance and Main Findingsa
| Study . | N (Male) . | Mean Age (SD) (y) . | Time Since Stroke (SD) . | VR Intervention . | Control Intervention . |
|---|---|---|---|---|---|
| Givon et al,52 2016 | 47 (28) | VR group: 56.7 (9.3) Control group: 62.0 (9.3) | VR group: 3.0 (1.8) y Control group: 2.6 (1.8) y | VR group training | Conventional group therapy |
| Kim et al,47 2015 | 17 (9) | VR group: 56.2 (7.56) Control group: 48.7 (9.3) | VR group: 7.5 (4.4) mo Control group: 16.6 (8.8) mo | Conventional therapy plus VR-based treadmill training | Conventional therapy |
| Lee et al,55 2015 | 24 (16) | VR group: 45.9 (12.3) Control group: 49.2 (12.9) | nr | Conventional therapy plus VR training | Conventional therapy plus task-oriented training |
| Lee et al,55 2015 | 20 (11) | VR group: 57.2 (9.2) Control group: 52.7 (11.7) | nr | VR training with cognitive tasks | PNF exercise program |
| Llorens et al,49 2015 | 20 (9) | VR group: 58.3 (11.6) Control group: 55.0 (11.6) | VR group: 407.5 (232.4) d Control group: 587 (222.1) d | Conventional therapy plus VR therapy | Conventional therapy |
| Song et al,53 2015 | 40 (22) | VR group: 51.4 (40.6) Control group: 50.1 (7.8) | VR group: 14.8 (6.1) mo Control group: 14.3 (3.4) mo | VR training | Ergometer bicycle training |
| Cho et al,43 2014 | 30 (15) | VR group: 65.9 (5.7) Control group: 63.5 (5.5) | VR group: 414.5 (150.4) d Control group: 460.3 (186.8) d | Conventional therapy plus VR-based treadmill training | Conventional therapy plus traditional non-VR treadmill training |
| Hung et al,33 2014 | 28 (18) | VR group: 55.4 (10.0) Control group: 53.4 (10.0) | VR group: 21.0 (11.3) mo Control group: 15.9 (8.0) mo | Conventional therapy plus VR training | Conventional therapy plus weight-shift training |
| Morone et al,51 2014 | 50 (nr) | VR group: 58.4 (9.6) Control group: 62.0 (10.3) | VR group: 61.0 (36.5) d Control group: 41.7 (36.9) d | Conventional therapy plus VR therapy | Conventional therapy plus extra balance therapy |
| Song et al,59 2014 | 20 (11) | VR group: 65.6 (13.5) Control group: 61.2 (13.8) | VR group: 12.7 (3.2) d Control group: 13.2 (3.4) d | Conventional therapy plus VR training | Conventional therapy |
| Barcala et al,29 2013 | 20 (9) | VR group: 65.2 02.5) Control group: 63.5 (14.5) | VR group: 12.3 (7.1) mo Control group: 15.2 (6.6) mo | Conventional therapy plus VR training | Conventional therapy |
| Cho et al,42 2013 | 14 (7) | VR group: 64.6 (4.4) Control group: 65.1 (4.7) | VR group: 288.3 (69.2) d Control group: 312.4 (83.7) d | Conventional therapy plus VR-based treadmill training | Conventional therapy plus traditional non-VR treadmill training |
| Park et al,” 2013 | 16 (11) | VR group: 48.8 (8.8) Control group: 46.3 (6.8) | VR group: 11.3 (4.5) y Control group: 11.6 (4.4) y | Conventional therapy plus reality-based training | Conventional therapy |
| Givon et al,52 2016 | Equal | Functional: 10MWT | ns | ||
| Kim et al,47 2015 | Equal | Static balance: PSPL (AP, ML, and total), APSS | PSPL (AP, ML, and total), APSS (P<.05) | ||
| Lee et al,55 2015 | Equal | Static balance: COP path length, COP velocity Dynamic balance: FRT | FRT (P<.0001) | ||
| Lee et al,55 2015 | Equal | Dynamic balance: BBS, TUG | BBS, TUG (P<.05) | ||
| Lloréns et al,49 2015 | Equal | Functional: 10MWT | 1OMWT (P<.05) | Dynamic balance: BBS, Tinetti POMA, Brunel Balance Assessment | BBS (P<.05) |
| Song et al,53 2015 | Equal | Functional: 10MWT | 10MWT (P<.05) | Static balance: weight- bearing ratio affected side, forward and backward LOS Dynamic balance: TUG | Weight-bearing ratio affected side, forward and backward LOS, TUG (P<.05) |
| Cho et al,43 2014 | Equal | Spatiotemporal: gait speed, cadence, step length, stride length, double-limb support period, single-limb support period | Gait speed, cadence, single- and double-limb support period, step and stride length (P<.029) | Static balance: AP-PSV, ML-PSV, PSVM Dynamic balance: BBS, TUG | BBS, TUG (P=.001) |
| Hung et al,33 2014 | Equal | Static balance: SI, weight-bearing asymmetry on affected leg Dynamic balance: TUG, FRT | SI (P‹.05) | ||
| Morone et al,51 2014 | Equal | Functional: 10MWT, FAC | 10MWT (P=.021) | Dynamic balance: BBS | BBS (P=.004) |
| Song et al,50 2014 | Higher | Static balance: Fl scores, SI, WDI Dynamic balance: BBS | SI and WDI while standing with eyes open and when standing on a pillow with eyes open (P‹.017) | ||
| Barcala et al,29 2013 | Higher | Dynamic balance: BBS, TUG Static balance: COP oscillations | ns | ||
| Cho et al,42 2013 | Equal | Spatiotemporal: gait speed, cadence, paretic side step length, stride length, and single-limb support period | Gait speed, cadence (P=.01) | Dynamic balance: BBS, TUG | BBS, TUG (P=.01) |
| Park et al,48 2013 | Equal | Spatiotemporal: gait speed, cadence, step length, stride length Functional: 10MWT | Stride length (P<.03) | ||
| Rajaratnam et al,30 2013 | Equal | Static balance: CoP sway Dynamic balance: BBS, TUG, FRT | FRT (P=.01) | ||
| Cho et al,54 2012 | Higher | Static balance: AP-PSV and ML-PSV (with eyes open or closed) Dynamic balance: BBS, TUG | BBS, TUG (P<.05) | ||
| Jung et al,44 2012 | Equal | Dynamic balance: TUG, ABC scale | TUG, ABC (P<.05) | ||
| Kang et al,32 2012 | Equal | Functional: 6MWT, 10MWT | 6MWT, 10MWT (P<.05) | Dynamic balance: TUG, FRT | VR group vs control group 1: TUG (P<.05) VR group vs control group 2: TUG, FRT (P<.05) |
| Yang et al,46 2011 | Equal | Static balance: COPML, COPAP, COPE, COPA, symmetry index (quiet stance and sit-to-stand transfer), COPE/P (sitto-stand transfer) stance time/P, step no./P, contact A/P (level walking) | COPML (P=.038) | ||
| Kim et al,16 2009 | Higher | Spatiotemporal: cadence, step time, stance time, swing time, single/double support time, step/stride length Functional: 10MWT, MMAS | Cadence, step length, step time (P<.014) | Static balance: mean balance, sway area, sway path, maximal velocity Dynamic balance: BBS, AP angle, ML angle | BBS, AP angle, and ML angle (P<.01) |
| Yang et al,8 2008 | Equal | Functional: 10MWT, community walking time, WAQ | Pretest-posttest: 10MWT, community walking time (P<.05) Follow-up: WAQ (P=.03) | Dynamic balance: ABC scale | ns |
| Jaffe et al,45 2004 | Equal | Spatiotemporal: gait speed, cadence, step and stride length Functional: obstacle test, distance on 6MWT | Gait speed, stride length (ss), obstacle clearance, step length of nonparetic leg (ss) and paretic leg (fs) (P<.05) | ||
| Rajaratnam et al,30 2013 | 19 (7) | VR group: 58.7 (8.6) Control group: 65.3 (9.6) | VR group: 14.7 (7.5) d Control group: 15.2 (6.3) d | Conventional therapy plus VR balance training | Conventional therapy |
| Cho et al,54 2012 | 22 (14) | VR group: 65.3 (8.4) Control group: 63.1 (6.9) | VR group: 12.5 (2.6) mo Control group: 12.6 (2.5) mo | Conventional therapy plus VR balance training | Conventional therapy |
| Jung et al,44 2012 | 21 (13) | VR group: 60.5 (8.6) Control group: 63.6 (5.1) | VR group: 12.6 (3.3) mo Control group: 15.4 (4.7) mo | VR treadmill training | Non-VR treadmill training |
| Kang et al,32 2012 | 30 (15) | VR group: 55.9 (6.4) Control group 1: 56.3 (7.6) Control group 2: 56.1 (7.8) | VR group: 14.1 (4.4) mo Control group 1: 13.5 (4.0) mo Control group 2: 15.1 (7.4) mo | Conventional therapy plus VR treadmill training | Conventional therapy plus non-VR treadmill training (control group 1) or stretching exercises (control group 2) |
| Yang et al,46 2011 | 14 (nr) | VR group: 56.3 (10.2) Control group: 65.7 (5.9) | VR group: 17.0 (8.6) mo Control group: 16.3 (10.4) mo | VR treadmill training | Non-VR treadmill training |
| Kim et al,16 2009 | 24 (14) | VR group: 52.4 (10.1) Control group: 51.75 (7.1) | VR group: 25.9 (10.0) mo Control group: 24.3 (8.9) mo | Conventional therapy plus VR therapy | Conventional therapy |
| Yang et al,8 2008 | 20 (10) | VR group: 55.5 (12.2) Control group: 60.9 (9.3) | VR group: 5.9 (4.2) y Control group: 6.1 (10.3) y | VR treadmill training | Non-VR treadmill training |
| Jaffe et al,45 2004 | 20 (12) | VR group: 58.2 (11.2) Control group: 63.2 (8.3) | VR group: 3.9 (2.3) y Control group: 3.6 (2.6) y | Virtual object training | Stepping over real foam objects on a 10-m walkway |
| Study . | N (Male) . | Mean Age (SD) (y) . | Time Since Stroke (SD) . | VR Intervention . | Control Intervention . |
|---|---|---|---|---|---|
| Givon et al,52 2016 | 47 (28) | VR group: 56.7 (9.3) Control group: 62.0 (9.3) | VR group: 3.0 (1.8) y Control group: 2.6 (1.8) y | VR group training | Conventional group therapy |
| Kim et al,47 2015 | 17 (9) | VR group: 56.2 (7.56) Control group: 48.7 (9.3) | VR group: 7.5 (4.4) mo Control group: 16.6 (8.8) mo | Conventional therapy plus VR-based treadmill training | Conventional therapy |
| Lee et al,55 2015 | 24 (16) | VR group: 45.9 (12.3) Control group: 49.2 (12.9) | nr | Conventional therapy plus VR training | Conventional therapy plus task-oriented training |
| Lee et al,55 2015 | 20 (11) | VR group: 57.2 (9.2) Control group: 52.7 (11.7) | nr | VR training with cognitive tasks | PNF exercise program |
| Llorens et al,49 2015 | 20 (9) | VR group: 58.3 (11.6) Control group: 55.0 (11.6) | VR group: 407.5 (232.4) d Control group: 587 (222.1) d | Conventional therapy plus VR therapy | Conventional therapy |
| Song et al,53 2015 | 40 (22) | VR group: 51.4 (40.6) Control group: 50.1 (7.8) | VR group: 14.8 (6.1) mo Control group: 14.3 (3.4) mo | VR training | Ergometer bicycle training |
| Cho et al,43 2014 | 30 (15) | VR group: 65.9 (5.7) Control group: 63.5 (5.5) | VR group: 414.5 (150.4) d Control group: 460.3 (186.8) d | Conventional therapy plus VR-based treadmill training | Conventional therapy plus traditional non-VR treadmill training |
| Hung et al,33 2014 | 28 (18) | VR group: 55.4 (10.0) Control group: 53.4 (10.0) | VR group: 21.0 (11.3) mo Control group: 15.9 (8.0) mo | Conventional therapy plus VR training | Conventional therapy plus weight-shift training |
| Morone et al,51 2014 | 50 (nr) | VR group: 58.4 (9.6) Control group: 62.0 (10.3) | VR group: 61.0 (36.5) d Control group: 41.7 (36.9) d | Conventional therapy plus VR therapy | Conventional therapy plus extra balance therapy |
| Song et al,59 2014 | 20 (11) | VR group: 65.6 (13.5) Control group: 61.2 (13.8) | VR group: 12.7 (3.2) d Control group: 13.2 (3.4) d | Conventional therapy plus VR training | Conventional therapy |
| Barcala et al,29 2013 | 20 (9) | VR group: 65.2 02.5) Control group: 63.5 (14.5) | VR group: 12.3 (7.1) mo Control group: 15.2 (6.6) mo | Conventional therapy plus VR training | Conventional therapy |
| Cho et al,42 2013 | 14 (7) | VR group: 64.6 (4.4) Control group: 65.1 (4.7) | VR group: 288.3 (69.2) d Control group: 312.4 (83.7) d | Conventional therapy plus VR-based treadmill training | Conventional therapy plus traditional non-VR treadmill training |
| Park et al,” 2013 | 16 (11) | VR group: 48.8 (8.8) Control group: 46.3 (6.8) | VR group: 11.3 (4.5) y Control group: 11.6 (4.4) y | Conventional therapy plus reality-based training | Conventional therapy |
| Givon et al,52 2016 | Equal | Functional: 10MWT | ns | ||
| Kim et al,47 2015 | Equal | Static balance: PSPL (AP, ML, and total), APSS | PSPL (AP, ML, and total), APSS (P<.05) | ||
| Lee et al,55 2015 | Equal | Static balance: COP path length, COP velocity Dynamic balance: FRT | FRT (P<.0001) | ||
| Lee et al,55 2015 | Equal | Dynamic balance: BBS, TUG | BBS, TUG (P<.05) | ||
| Lloréns et al,49 2015 | Equal | Functional: 10MWT | 1OMWT (P<.05) | Dynamic balance: BBS, Tinetti POMA, Brunel Balance Assessment | BBS (P<.05) |
| Song et al,53 2015 | Equal | Functional: 10MWT | 10MWT (P<.05) | Static balance: weight- bearing ratio affected side, forward and backward LOS Dynamic balance: TUG | Weight-bearing ratio affected side, forward and backward LOS, TUG (P<.05) |
| Cho et al,43 2014 | Equal | Spatiotemporal: gait speed, cadence, step length, stride length, double-limb support period, single-limb support period | Gait speed, cadence, single- and double-limb support period, step and stride length (P<.029) | Static balance: AP-PSV, ML-PSV, PSVM Dynamic balance: BBS, TUG | BBS, TUG (P=.001) |
| Hung et al,33 2014 | Equal | Static balance: SI, weight-bearing asymmetry on affected leg Dynamic balance: TUG, FRT | SI (P‹.05) | ||
| Morone et al,51 2014 | Equal | Functional: 10MWT, FAC | 10MWT (P=.021) | Dynamic balance: BBS | BBS (P=.004) |
| Song et al,50 2014 | Higher | Static balance: Fl scores, SI, WDI Dynamic balance: BBS | SI and WDI while standing with eyes open and when standing on a pillow with eyes open (P‹.017) | ||
| Barcala et al,29 2013 | Higher | Dynamic balance: BBS, TUG Static balance: COP oscillations | ns | ||
| Cho et al,42 2013 | Equal | Spatiotemporal: gait speed, cadence, paretic side step length, stride length, and single-limb support period | Gait speed, cadence (P=.01) | Dynamic balance: BBS, TUG | BBS, TUG (P=.01) |
| Park et al,48 2013 | Equal | Spatiotemporal: gait speed, cadence, step length, stride length Functional: 10MWT | Stride length (P<.03) | ||
| Rajaratnam et al,30 2013 | Equal | Static balance: CoP sway Dynamic balance: BBS, TUG, FRT | FRT (P=.01) | ||
| Cho et al,54 2012 | Higher | Static balance: AP-PSV and ML-PSV (with eyes open or closed) Dynamic balance: BBS, TUG | BBS, TUG (P<.05) | ||
| Jung et al,44 2012 | Equal | Dynamic balance: TUG, ABC scale | TUG, ABC (P<.05) | ||
| Kang et al,32 2012 | Equal | Functional: 6MWT, 10MWT | 6MWT, 10MWT (P<.05) | Dynamic balance: TUG, FRT | VR group vs control group 1: TUG (P<.05) VR group vs control group 2: TUG, FRT (P<.05) |
| Yang et al,46 2011 | Equal | Static balance: COPML, COPAP, COPE, COPA, symmetry index (quiet stance and sit-to-stand transfer), COPE/P (sitto-stand transfer) stance time/P, step no./P, contact A/P (level walking) | COPML (P=.038) | ||
| Kim et al,16 2009 | Higher | Spatiotemporal: cadence, step time, stance time, swing time, single/double support time, step/stride length Functional: 10MWT, MMAS | Cadence, step length, step time (P<.014) | Static balance: mean balance, sway area, sway path, maximal velocity Dynamic balance: BBS, AP angle, ML angle | BBS, AP angle, and ML angle (P<.01) |
| Yang et al,8 2008 | Equal | Functional: 10MWT, community walking time, WAQ | Pretest-posttest: 10MWT, community walking time (P<.05) Follow-up: WAQ (P=.03) | Dynamic balance: ABC scale | ns |
| Jaffe et al,45 2004 | Equal | Spatiotemporal: gait speed, cadence, step and stride length Functional: obstacle test, distance on 6MWT | Gait speed, stride length (ss), obstacle clearance, step length of nonparetic leg (ss) and paretic leg (fs) (P<.05) | ||
| Rajaratnam et al,30 2013 | 19 (7) | VR group: 58.7 (8.6) Control group: 65.3 (9.6) | VR group: 14.7 (7.5) d Control group: 15.2 (6.3) d | Conventional therapy plus VR balance training | Conventional therapy |
| Cho et al,54 2012 | 22 (14) | VR group: 65.3 (8.4) Control group: 63.1 (6.9) | VR group: 12.5 (2.6) mo Control group: 12.6 (2.5) mo | Conventional therapy plus VR balance training | Conventional therapy |
| Jung et al,44 2012 | 21 (13) | VR group: 60.5 (8.6) Control group: 63.6 (5.1) | VR group: 12.6 (3.3) mo Control group: 15.4 (4.7) mo | VR treadmill training | Non-VR treadmill training |
| Kang et al,32 2012 | 30 (15) | VR group: 55.9 (6.4) Control group 1: 56.3 (7.6) Control group 2: 56.1 (7.8) | VR group: 14.1 (4.4) mo Control group 1: 13.5 (4.0) mo Control group 2: 15.1 (7.4) mo | Conventional therapy plus VR treadmill training | Conventional therapy plus non-VR treadmill training (control group 1) or stretching exercises (control group 2) |
| Yang et al,46 2011 | 14 (nr) | VR group: 56.3 (10.2) Control group: 65.7 (5.9) | VR group: 17.0 (8.6) mo Control group: 16.3 (10.4) mo | VR treadmill training | Non-VR treadmill training |
| Kim et al,16 2009 | 24 (14) | VR group: 52.4 (10.1) Control group: 51.75 (7.1) | VR group: 25.9 (10.0) mo Control group: 24.3 (8.9) mo | Conventional therapy plus VR therapy | Conventional therapy |
| Yang et al,8 2008 | 20 (10) | VR group: 55.5 (12.2) Control group: 60.9 (9.3) | VR group: 5.9 (4.2) y Control group: 6.1 (10.3) y | VR treadmill training | Non-VR treadmill training |
| Jaffe et al,45 2004 | 20 (12) | VR group: 58.2 (11.2) Control group: 63.2 (8.3) | VR group: 3.9 (2.3) y Control group: 3.6 (2.6) y | Virtual object training | Stepping over real foam objects on a 10-m walkway |
nr=not reported, ns= nonsignificant, 6MWT=Six-Minute Walk Test, 10MWT=10-Meter Walk Test, ABC=Activities-specific Balance Confidence, AP=anterior-posterior, AP-PSV=anterior-posterior postural sway velocity, AP and ML angle=angle between a vertical line from the spatial center of the supporting feet and a second line connecting from the same point to the individual’s center of gravity, APSS=average postural sway speed, BBS=Berg Balance Scale, contact A/P=contact area of the paretic limb, COP=center of pressure, COPA=center of pressure sway area, COPAP=center of pressure displacement in anterior-posterior direction, COPE=center-of-pressure total path excursion, COPE/P=center-of-pressure path excursion under the paretic limb, COPML=center-of-pressure displacement in medial-lateral direction, Fl=falling index, fast=as fast as possible pace, FAC=Functional Ambulation Categories, FRT=Functional Reach Test, ML=medial-lateral, ML-PSV=medial-lateral postural sway velocity, MMAS=Modified Motor Assessment Scale, POMA=Performance-Oriented Mobility Assessment, PSPL=postural sway path length, PSVM=postural sway velocity moment, Sl=stability index, ss=selfselected pace, stance time/P=stance time of the paretic limb, LOS=limit of stability, step no./=step number of the paretic limb, TUG=Timed “Up & Go” Test, WAQ=Walking Ability Questionnaire, WDI=weight distribution index.
PEDro Scores
The PEDro scores of the included studies varied between 3 and 8, with a median of 6.0 and an interquartile range of 2.0 (Tab. 2). Thirteen studies had a score of 6 or higher and were considered of high quality. All trials randomly allocated the participants. Furthermore, the majority of trials reported eligibility criteria (95.4%), had similar groups at baseline (85.7%), performed between-group analyses (95.4%) and assessor blinding (61.9%), collected data of more than 85.0% of the participants (76.2%), and used both point measures and measures of variability (90.5%). In total, 23 (10.0%) of the 231 items from the PEDro scale were initially scored different by the 2 reviewers. After discussion, there was agreement for all items.
PEDro Scores of the Included Studiesa
| Study . | Eligibility Criteria . | Random Allocation . | Concealed Allocation . | Baseline Comparability . | Participant Blinded . | Clinician Blinded . | Assessor Blinded . | Data for at Least 1 Outcome From >85% of Participants . | No Missing Data or If Missing, Intention-to-Treat Analysis . | Between-Groups Analysis . | Point Estimates and Variability . | Total Score (/10) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Givon et al,52 2016 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 6 |
| Kim et al,47 2015 | No | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Lee et al,55 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Lee et al,56 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Llorens et al,49 2015 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Song et al,53 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Cho et al,43 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Hung et al,33 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Morone et al,51 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Song et al,50 2014 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Barcala et al,29 2013 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Cho et al,42 2013 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Park et al,48 2013 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Rajaratnam et al,30 2013 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 6 |
| Cho et al,54 2012 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Jung et al,44 2012 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Kang et al,32 2012 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Yang et al, 201146 | Yes | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 5 |
| Kim et al,16 2009 | Yes | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Yang et al,8 2008 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 7 |
| Jaffe et al,45 2004 | Yes | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 3 |
| Study . | Eligibility Criteria . | Random Allocation . | Concealed Allocation . | Baseline Comparability . | Participant Blinded . | Clinician Blinded . | Assessor Blinded . | Data for at Least 1 Outcome From >85% of Participants . | No Missing Data or If Missing, Intention-to-Treat Analysis . | Between-Groups Analysis . | Point Estimates and Variability . | Total Score (/10) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Givon et al,52 2016 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 6 |
| Kim et al,47 2015 | No | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Lee et al,55 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Lee et al,56 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Llorens et al,49 2015 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Song et al,53 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Cho et al,43 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Hung et al,33 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Morone et al,51 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Song et al,50 2014 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Barcala et al,29 2013 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Cho et al,42 2013 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Park et al,48 2013 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Rajaratnam et al,30 2013 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 6 |
| Cho et al,54 2012 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Jung et al,44 2012 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Kang et al,32 2012 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Yang et al, 201146 | Yes | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 5 |
| Kim et al,16 2009 | Yes | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Yang et al,8 2008 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 7 |
| Jaffe et al,45 2004 | Yes | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 3 |
1=yes, 0=no.
PEDro Scores of the Included Studiesa
| Study . | Eligibility Criteria . | Random Allocation . | Concealed Allocation . | Baseline Comparability . | Participant Blinded . | Clinician Blinded . | Assessor Blinded . | Data for at Least 1 Outcome From >85% of Participants . | No Missing Data or If Missing, Intention-to-Treat Analysis . | Between-Groups Analysis . | Point Estimates and Variability . | Total Score (/10) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Givon et al,52 2016 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 6 |
| Kim et al,47 2015 | No | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Lee et al,55 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Lee et al,56 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Llorens et al,49 2015 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Song et al,53 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Cho et al,43 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Hung et al,33 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Morone et al,51 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Song et al,50 2014 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Barcala et al,29 2013 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Cho et al,42 2013 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Park et al,48 2013 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Rajaratnam et al,30 2013 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 6 |
| Cho et al,54 2012 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Jung et al,44 2012 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Kang et al,32 2012 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Yang et al, 201146 | Yes | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 5 |
| Kim et al,16 2009 | Yes | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Yang et al,8 2008 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 7 |
| Jaffe et al,45 2004 | Yes | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 3 |
| Study . | Eligibility Criteria . | Random Allocation . | Concealed Allocation . | Baseline Comparability . | Participant Blinded . | Clinician Blinded . | Assessor Blinded . | Data for at Least 1 Outcome From >85% of Participants . | No Missing Data or If Missing, Intention-to-Treat Analysis . | Between-Groups Analysis . | Point Estimates and Variability . | Total Score (/10) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Givon et al,52 2016 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 6 |
| Kim et al,47 2015 | No | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Lee et al,55 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Lee et al,56 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Llorens et al,49 2015 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Song et al,53 2015 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Cho et al,43 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Hung et al,33 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Morone et al,51 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Song et al,50 2014 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Barcala et al,29 2013 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Cho et al,42 2013 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Park et al,48 2013 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Rajaratnam et al,30 2013 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 6 |
| Cho et al,54 2012 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Jung et al,44 2012 | Yes | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Kang et al,32 2012 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Yang et al, 201146 | Yes | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 5 |
| Kim et al,16 2009 | Yes | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Yang et al,8 2008 | Yes | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 7 |
| Jaffe et al,45 2004 | Yes | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 3 |
1=yes, 0=no.
Content of the VR Interventions of Included Studies
There was wide variety in frequency, intervention setup, and content of the VR intervention (eTabs. 1 and 2, available at ptjournal.apta.org). The frequency varied between 2 and 5 VR training sessions a week. Eight studies8,32,42–47 focused on a gait intervention, and 13 studies16,29,30,33,48–56 focused on balance interventions. To project the virtual environment, a head-mounted device was used in 4 studies,32,44,45,48 and the VR was projected on a screen in the other 17 studies.8,16,29,30,33,42,43,46,47,49–56
Outcome Measures and Main Findings of Included Studies
All studies showed a significant difference between the VR and control groups in favor of the VR intervention in different measures of balance or gait ability, except for the studies by Barcala et al29 and Givon et al52 (Tab. 1). Four studies were not included in the meta-analysis: 3 studies46,47,55 did not report gait speed, BBS scores, or TUG scores and reported only on static balance parameters, and data of one study50 were not available for a pooled analysis.
Gait ability
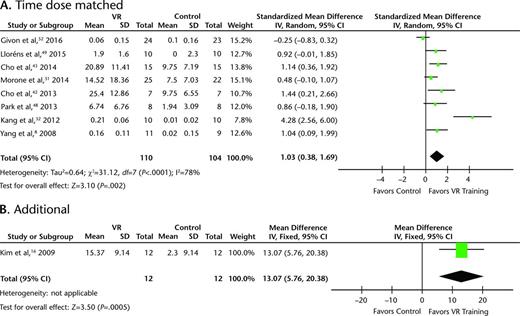
Of the studies measuring gait ability, 2 studies42,43 reported on spatiotemporal parameters, 3 studies16,45,48 used both spatiotemporal and functional outcome measures, and 6 studies8,32,49,51–53 focused only on functional gait ability. Gait speed was the most frequently used measure of gait ability, as all studies measuring gait ability included gait speed as an outcome measure. This outcome measure was obtained using pressure-sensitive equipment or the 10-Meter Walk Test. Eight of the 11 studies (n=211) showed significantly greater increases in gait speed in the VR group (n=108) compared with the control group (n=103).8,32,42,43,45,49,51,53 The effect of VR training on gait speed was further examined by pooling the data of 8 studies in which VR training was time dose matched to conventional therapy (Fig. 2A). The pooled SMD showed that time dose–matched VR training improved gait speed significantly more than conventional therapy (SMD=1.03; 95% CI=0.38, 1.69; P=.002). The I2 statistic of 78% represents substantial heterogeneity. A sensitivity analysis showed that this heterogeneity was mainly due to the magnitude of the effect of the studies by Kang et al32 and Givon et al52 (eFigs. 1 and 2, available at ptjournal.apta.org). When these studies were excluded, the I2 of the pooled effect became 0%, with an SMD of 0.86 (95% CI=0.52, 1.20; P<.001).
Forest plot of the pooled results of the effect of VR training on gait speed in (A) time dose–matched studies (n=214) and (B) studies in which VR was additional to conventional therapy (n=24). VR=virtual reality, IV=inverse variance, CI=confidence interval.
In one study,16 VR training was additional to conventional therapy. This study showed a significant improvement in gait speed in favor of the VR group (Fig. 2B).
Balance
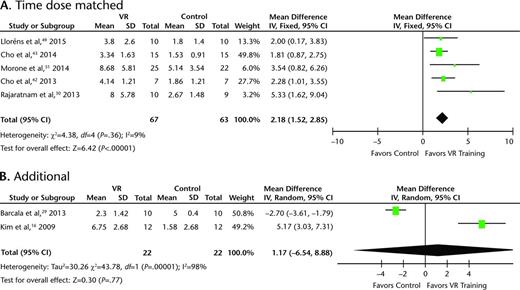
Regarding studies on balance, 7 studies8,32,42,44,49,51,56 reported on dynamic balance, 2 studies46,47 reported on static balance, and 9 studies16,29,30,33,43,50,53–55 reported on both dynamic and static balance outcome measures. Significant differences in the effect on static balance between the VR group (n=47) and control group (n=44) were found in 4 of the 11 studies reporting on static balance.46,47,50,53 The dynamic balance of patients with stroke seems to improve significantly more after a VR intervention compared with a conventional intervention. Significant differences were found for the BBS in favor of the VR group in 7 out of 10 studies reporting on this scale (n=180).16,42,43,49,51,54,56 The pooled MD for VR training time dose matched to conventional therapy showed that VR training significantly improved the BBS score with 2.18 (95% CI=1.52, 2.85; P<.001) (Fig. 3A). The I2 statistic of 9% represents low heterogeneity. The heterogeneity between the 2 studies in which VR was added to the conventional therapy was high (I2=98%). The pooled MD did not show a significant effect of VR training compared with conventional therapy (MD=1.17; 95% CI=−6.54, 8.88; P=.77) (Fig. 3B).
Forest plot of the pooled results for effect of VR training on Berg Balance Scale in (A) time dose–matched studies (n=130) and (B) studies in which VR was additional to conventional therapy (n=44). VR=virtual reality, IV=inverse variance, CI=confidence interval.
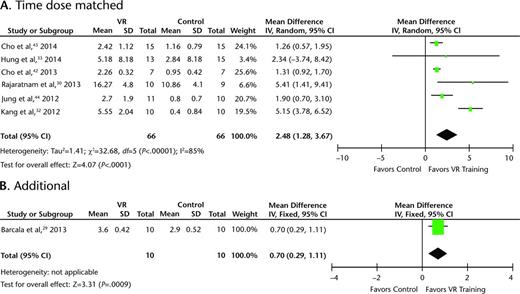
Time of the TUG improved significantly more in the VR group of 7 studies.32,42–44,53,54,56 Only Barcala et al,29 Rajaratnam et al,30 and Hung et al33 did not find significant results for the TUG in favor of the VR group. The pooled results for the TUG showed a significant MD of 2.48 (95% CI=1.28, 3.67; P<.001) in favor of the VR group. However, substantial heterogeneity was indicated with an I2 statistic of 85% (Fig. 4A). When excluding the studies by Rajaratnam et al30 and Kang et al,32 no heterogeneity (I2=0%) was observed. The MD was 1.35 and remained significant in favor of the VR group (95% CI=1.02, 1.67; P<.001) (eFigs. 1 and 2). The pooled MD for VR training in addition to conventional therapy was reported in just one study.29 This study showed a significant improvement in time of the TUG in favor of the VR group (Fig. 4B).
Forest plot of the pooled results for the effect of VR training on Timed “Up & Go” Test in (A) time dose–matched studies (n=132) and (B) studies in which VR was additional to conventional therapy (n=20). VR=virtual reality, IV=inverse variance, CI=confidence interval.
Discussion
This systematic review provided evidence for a stronger effect of VR training compared with conventional therapy, as suggested by the significantly greater improvements in balance and gait ability. Gait speed, BBS score, and time of TUG were the most frequently used measures to underpin the stronger effect of VR training. Pooled effect estimates showed significant improvements in these 3 outcome measures in favor of the VR group for both time dose–matched VR interventions and VR interventions in addition to conventional therapy. The positive findings of VR training are in line with previous reviews on the effect of VR on the lower extremity in patients with stroke.9,20–23,57 The systematic reviews by Dos Santos et al24 and Cheok et al25 did not support these positive findings. This conflicting finding may be due to the fact that these reviews included only RCTs that used a Nintendo Wii (Nintendo, Kyoto, Japan) intervention as VR and, therefore, included only 524 or 625 studies. In addition, 2 of the included RCTs in both reviews concentrated on upper extremity motor function58 or global motor function59 and did not include dynamic balance measures (BBS, TUG) or static balance measures. The pooled effect for the BBS when VR was added to conventional therapy was the only measure that did not significantly improve more after VR training. The high heterogeneity between the 2 studies included in the analysis of the BBS may explain why there was no significant pooled effect of VR training in addition to conventional therapy. The meta-analysis included only studies of high quality, as indicated by a PEDro score of 6 or higher. However, when performing the same meta-analyses using all studies for which data were available, the conclusions were the same.
The added value of VR on balance and gait ability compared with most of the currently provided conventional therapies may be explained by multiple aspects. Virtual reality creates patient-specific motor training with a high level of repetitive and variable training. Repetitive training has been hypothesized to form the physiological basis of motor learning.60 The majority of studies included in this review provided highly repetitive VR training. However, noticeable differences among the studies could be found in the intensity of training. In the studies by Jaffe et al45 and Park et al,48 the number of steps or corrections in balance that participants had to take were small, which is in contrast to the highly repetitive training in the other 19 studies. Because repetitive training has proven to be an important principle of motor learning,60 these 2 studies may not have fully optimized the benefits of VR. This possibility is confirmed by the results for gait speed, which showed a nonsignificant or minor effect of VR in the studies by Park et al48 and Jaffe et al,45 respectively.
Besides repetitive training, variability in practice is important for motor learning because it will lead to improvement in the ability to adapt to novel situations.13 Virtual reality also enables therapists to provide individualized training in which the intensity and difficulty of the training exercises can easily be adjusted to the characteristics and needs of the patient.61 Controlled constraints can be applied to patients with stroke who are performing exercises, which is necessary for optimal learning.9,17
Besides, more feedback about the performance of participants can be given in VR training than would be possible in real-world practice. Feedback can be divided into intrinsic and extrinsic. Intrinsic feedback refers to somatic information, including tactile, proprioceptive, and kinesthetic information, and may be damaged in patients with stroke. Extrinsic or augmented feedback is provided through an external source.62,63 This so-called augmented feedback can be provided in knowledge of results at the end of a training task or knowledge of performance concurrent with the performance of the training task.64 It is well known that feedback improves the learning rate64 and that patients with stroke benefit from practice with augmented feedback.65 Visual feedback, specifically, has been shown to play a role in improving balance in patients with stroke.66,67 All studies in this review included visual, auditory, or sensory augmented feedback, for instance, derived from real-world video recording or an avatar that copies the individual's movements. Therefore, this aspect of VR may play a crucial role in the positive effect of VR on improving balance and gait ability.
Lastly, VR is thought to improve motivation and enjoyment, to decrease the perception of exertion, and to increase the activity adherence in training.68 The degree to which participants feel motivated and engaged during VR training can depend on the individual and the intervention. None of the studies included in the present review measured motivation. However, Lloréns et al40 already assessed motivation and showed that people with stroke considered a VR-based balance intervention as highly motivating. To study the role of motivation as one of the underlying mechanisms for the effect of VR training, future studies need to include motivation as an outcome measure.
The majority of the included studies provided high methodological quality. However, most studies did not perform concealed allocation and lacked an intention-to-treat analysis, which could have led to bias in the included trials. In addition, the majority of studies did not provide participant and clinician blinding, which was expected in this kind of intervention. However, the assessor who performed the measurements was blinded in the majority of the studies. Besides methodological quality, the transparency of the included studies may have had an influence on the results of this review. Not all included studies described the intervention and stroke population in detail and reported their results completely. We tried to retrieve most of the unreported data by contacting the authors through email. Regarding the stroke population, disease status or severity may influence the effect of VR interventions. Because half of the included studies did not report Brunnstrom stages or other measures of disease status, this stroke characteristic could not be included in this review.
Study Limitations
The review identified some limitations that should be taken into account when interpreting the effect of VR training on balance and gait ability in patients recovering from stroke. First, the broad inclusion and diversity in the included studies bring some limitations with it. The included studies were diverse regarding the population of patients with stroke, especially regarding the wide variation in time since stroke. It was expected that the effect of VR training was higher in patients early after stroke because brain plasticity and structural reorganization is higher early after lesions69 and endogenous recovery after stroke has been reported to reach a plateau in 6 months.70 However, this expectation was not supported by our results because the 3 studies30,50,51 with a mean time since stroke that did not exceed 2 months did not report another trend in the results compared with the other 18 studies with a mean time since stroke of more than 7 months. Because of a lack of a clear definition of VR, there is diversity in the VR interventions included in the review. In addition, there is diversity in control interventions, leading to a variation in contrast between intervention and control groups among the included studies.
It is important to point out that the reported control group mostly represents conventional therapy, which may not actually and truly control for the VR intervention. An appropriate control group should match the VR intervention in dose, intensity, structure, goal-oriented focus, progressive increase of task demands, and inclusion of an explicit balance or walking component.71 For example, in the balance study by Morone et al,51 the control therapy consisted of both walking and balance exercises, whereas the VR training was specifically focused on balance. In the treadmill studies, the control therapy often consisted of treadmill training, but without VR. Using this design, the true additional value of VR could be studied. In this review, both VR in addition to conventional therapy and VR training time dose matched to conventional therapy showed a significantly greater effect on balance and gait ability compared with conventional therapy. The addition of VR appeared to have a smaller effect on improving balance and gait ability than time dose–matched VR training. However, the meta-analysis for additional VR training comprised only 3 studies.
Second, the generalizability of this review regarding age is questionable because only relatively young patients with stroke were included. It might be assumed that implementing VR in an older population is more challenging. In addition, the generalizability of the results of this review is limited to gait and balance outcomes and specifically gait speed, BBS scores, and TUG scores. We chose to include these uniform outcome measures to perform a valuable meta-analysis. However, in several of the included studies, other balance and gait outcomes were performed, and some of these performance-based outcome measures did not demonstrate significant differences between VR training and conventional therapy. In addition, there is a lack of outcome measures on participation level and follow-up analysis. The effectiveness of the VR intervention is measured using spatiotemporal or functional gait measures and dynamic or static balance measures. However, to our knowledge, how these outcome measures translate into daily life participation levels and quality of life has not been investigated. Other reviews18,72 also concluded that there is a lack of RCTs that measure the effect of VR on participation level. The inclusion of outcome measures focusing on improvement of participation levels and quality of life would have strengthened the results on the effect of VR on balance and gait and the translation to real life, especially as a previous study73 suggested that training in a virtual environment might improve quality of life and feeling of safety. Furthermore, most of the studies measured the effect of VR directly after the intervention; only 4 studies8,33,48,52 also measured the effect of VR after 1 or 3 months of follow-up. However, it would be interesting to investigate the long-term effects of VR training to ascertain whether VR-induced improvement can be sustained over time and how the improvements translate into home or community environments.16 To improve the strength of evidence on the effects of VR, future studies need to be large RCTs investigating the effect of VR from body function to participation level and have to be conducted with standardized training doses and adequate follow-up.
Lastly, we included 21 studies using broad inclusion criteria regarding the VR interventions, suggesting that we did not miss studies comparing VR training with gait or balance training without VR. However, visual inspection of funnel plots in which the SMDs for the TUG and gait speed were plotted against the standard error of the SMD shows asymmetry, which suggests the presence of publication bias. As most published studies showed a positive effect, it might be suggested that studies with a negative outcome were missed.
In conclusion, this review suggests that VR training is more effective than conventional therapy without VR in improving balance and gait ability in patients with stroke, both when VR interventions are added to conventional therapy and when time dose is matched. Keeping in mind that different interventions and outcome measures were used, no definite conclusions can be drawn about the most effective sort of VR training intervention. Future studies are recommended to investigate the effect of VR on participation level with large sample sizes and an adequate follow-up period. Overall, a positive and promising effect of VR training on balance and gait ability is expected.
All authors provided concept/idea/research design and writing. Ms de Rooij and Dr van de Port provided data collection and data analysis. Dr Meijer provided project management and fund procurement. Dr van de Port and Dr Meijer provided consultation (including review of manuscript before submission).
The authors thank Thamar Bovend'Eerdt, PhD, for his contribution as scientific adviser for the establishment of the research questions and specification of the study design.
References




Comments