-
PDF
- Split View
-
Views
-
Cite
Cite
Soomi Lee, Lauren Hale, Anne-Marie Chang, Nicole G Nahmod, Lindsay Master, Lawrence M Berger, Orfeu M Buxton, Longitudinal associations of childhood bedtime and sleep routines with adolescent body mass index, Sleep, Volume 42, Issue 1, January 2019, zsy202, https://doi.org/10.1093/sleep/zsy202
Close - Share Icon Share
Abstract
Having a regular, age-appropriate bedtime and sufficient sleep from early childhood may be important for healthy weight in adolescence. This study aimed to (1) identify heterogeneous groups of children by bedtime and sleep routines and (2) test longitudinal associations of childhood bedtime and sleep routine groups with adolescent body mass index (BMI).
We analyzed longitudinal data from the Fragile Families and Child Wellbeing Study, a national birth cohort from 20 US cities (N = 2196). Childhood bedtime and sleep routines were assessed by mothers’ reports of their children’s presence and timing of bedtimes, adherence to bedtimes, and habitual sleep duration at ages 5 and 9. At age 15, these adolescents reported their height and weight, which were used to calculate BMI z-score.
Latent Class Analysis revealed four groups of childhood bedtime and sleep routines: No Bedtime Routine Age 5 (Group 1), No Bedtime Routine Age 9 (Group 2), Borderline Bedtimes Ages 5 and 9 (Group 3), and Age-Appropriate Bedtime and Sleep Routines Ages 5 and 9 (Group 4, reference). Compared with adolescents in the reference group, those in the No Bedtime Routine Age 9 (Group 2) had +0.38 SD greater BMI (95% CI = [0.13 to 0.63]), above the level for overweight (1.02 SD BMI/85th percentile). Associations persisted after adjusting for age 3 BMI and sociodemographic characteristics.
Results demonstrate heterogeneity in childhood bedtime routine groups and their associations with adolescent BMI. Future studies should focus on whether childhood sleep behavior interventions promote healthier sleep and weight in later life course stages.
The current findings show that childhood bedtime and sleep routine groups predict adolescent sleep patterns and body mass index (BMI). In a national longitudinal study of urban households, one-third of children consistently adhered to age-appropriate bedtimes at ages 5 and 9. Compared with these children, those who had no bedtime routine at age 9 had shorter self-reported and actigraphic sleep duration and higher BMI at age 15, after adjusting for childhood BMI. The results support existing pediatric recommendations for having and adhering to age-appropriate bedtimes during childhood by demonstrating longitudinal associations with adolescent BMI.
Introduction
The prevalence of obesity and overweight among adolescents has increased over the past four decades internationally [1], including the United States [2]. Studies have noted parallel increases in obesity and sleep insufficiency and a positive association between them [3]. For example, young children who sleep 30 min less per night than is recommended have a higher risk of being overweight in middle childhood [4, 5]. Other studies of cross-sectional associations between adolescent sleep duration and body weight [6–8] suggest an 80% reduction in obesity risk for every additional hour of sleep in adolescence [6]. A meta-analysis spanning 11 longitudinal studies showed that short sleep duration in children/adolescents doubles the risk of overweight/obesity [7]. Most of these studies, however, focused on sleep duration alone as a risk factor of weight gain [9–12], without considering bedtimes and bedtime adherence. Experimental studies of sleep loss suggest multiple behavioral (e.g. overeating sweets) [13, 14], physiological, and metabolic mechanisms for this weight gain [3]. Early environmental context, such as parental routines with respect to bedtime, during childhood may also contribute to adolescent body weight [3, 15]. The goal of this study was to estimate longitudinal associations of childhood bedtime and sleep routines from ages 5 and 9 with adolescent body weight at age 15.
The presence of and adherence to bedtimes and bedtime routines may underlie the association of insufficient sleep and obesity. We hypothesized that adolescents who were engaged in age-appropriate, recommended bedtime and sleep routines at ages 5 and 9 would have lower body mass index (BMI) at age 15 than those lacking bedtime routines and those with late bedtimes. We analyzed both self-reported and actigraphy-measured sleep duration at age 15 to verify whether the identified childhood bedtime and sleep routine groups predict adolescent sleep duration similarly across measurement strategies.
Methods
Data
Our data were drawn from the Fragile Families and Child Wellbeing Study (FFCWS), a longitudinal study of children born between 1998 and 2000 in 20 US cities. The FFCWS is a stratified random sample of urban households and includes an oversampling of nonmarital births, children born to black and/or Hispanic mothers, and those whose families have lower levels of income and education [16].
Mothers (n = 4898) were initially interviewed in the hospital within 2 days of their child’s birth. Follow-up interviews were completed when the focal child was approximately ages 1, 3, 5, 9, and 15. Information about child sleep at ages 5 and 9 was collected during in-home interviews of mothers (n = 3023 and 3515, respectively). Only mothers who were the primary caregiver of the focal adolescent until age 15, and did not have missing data for the three indicators of child bedtime routines at ages 5 and 9, were included in this study (N = 2169), our analytic sample to identify childhood bedtime and sleep routine groups.
At age 15, the children, now adolescents, reported their habitual weeknight sleep duration (n = 2097). These adolescents reported height and weight for BMI (kg/m2; 1942 adolescents). A randomly selected subsample of these adolescents were invited and consented to participate in a 1 week actigraphy substudy, and 637 adolescents provided one or more valid weeknights’ sleep duration (M = 4.4 nights, SD = 1.7). The majority (85%) provided sleep data for at least 3 weekdays: 7% provided 1 day, 8% provided 2 days, 12% provided 3 days, 17% provided 4 days, 34% provided 5 days, 14% provided 6 days, and the rest (8%) provided at least 7 days of weeknight sleep duration data. We analyzed this subsample for actigraphic sleep duration. Procedures were approved by appropriate Institutional Review Boards.
Measures
Childhood bedtime and sleep routines
We assessed three domains of bedtimes: (1) whether the child had a bedtime and, if so, that time; (2) typical adherence to that bedtime, if present; and (3) habitual sleep duration. Mothers provided responses on each item during ages 5 and 9 in-home interviews. We defined age-appropriate sufficient sleep duration in accordance with the consensus recommended amount of sleep for pediatric populations by the American Academy of Sleep Medicine [17] endorsed by the American Academy of Pediatrics.
Presence and timing of bedtimes
At the age 5 and 9 interviews, FFCWS asked mothers “Does your child have a regular bedtime during the week? (no/yes)” and if yes, “When is (his/her) regular bedtime (hour, minute, AM/PM)?” To determine an appropriate (early) bedtime for each age group, we worked backwards from the time that a typical child wakes up. For example, a 5-year-old who needs to be at school by 8:30 am requires about an hour to get ready and eat breakfast. This means that the child needs to go to bed before 8:30 pm to get more than 11 hr of sufficient sleep (i.e. age-appropriate bedtimes); bedtimes between 8:30 and 9:30 pm may translate to 10–11 hr of sleep and are thus borderline bedtimes [17–19]. Similarly, a 9-year-old who needs to be at school by 8:00 am might awaken about 7:00 am, meaning the child needs to go to bed before 9:00 pm to have more than the minimum of 10 hr of sufficient sleep [19]. Considering these factors, we categorized the presence and timing of bedtimes as follows:
| Age 5 . | Age 9 . |
|---|---|
| No bedtime | No bedtime |
| Late: 9:30 pm < bedtimes | Late: 10:00 pm < bedtimes |
| Borderline: 8:30 pm ≤ bedtimes ≤ 9:30 pm | Borderline: 9:00 pm ≤ bedtimes ≤ 10:00 pm |
| Age-Appropriate: bedtimes < 8:30 pm | Age-Appropriate: bedtimes < 9:00 pm |
| Age 5 . | Age 9 . |
|---|---|
| No bedtime | No bedtime |
| Late: 9:30 pm < bedtimes | Late: 10:00 pm < bedtimes |
| Borderline: 8:30 pm ≤ bedtimes ≤ 9:30 pm | Borderline: 9:00 pm ≤ bedtimes ≤ 10:00 pm |
| Age-Appropriate: bedtimes < 8:30 pm | Age-Appropriate: bedtimes < 9:00 pm |
| Age 5 . | Age 9 . |
|---|---|
| No bedtime | No bedtime |
| Late: 9:30 pm < bedtimes | Late: 10:00 pm < bedtimes |
| Borderline: 8:30 pm ≤ bedtimes ≤ 9:30 pm | Borderline: 9:00 pm ≤ bedtimes ≤ 10:00 pm |
| Age-Appropriate: bedtimes < 8:30 pm | Age-Appropriate: bedtimes < 9:00 pm |
| Age 5 . | Age 9 . |
|---|---|
| No bedtime | No bedtime |
| Late: 9:30 pm < bedtimes | Late: 10:00 pm < bedtimes |
| Borderline: 8:30 pm ≤ bedtimes ≤ 9:30 pm | Borderline: 9:00 pm ≤ bedtimes ≤ 10:00 pm |
| Age-Appropriate: bedtimes < 8:30 pm | Age-Appropriate: bedtimes < 9:00 pm |
Bedtime adherence
Mothers were asked “How many times last week Monday-Friday, did your child adhere to that bedtime (frequency)?” We categorized bedtime adherence as “0” if the child had no regular bedtime or adhered to their regular bedtime 2 or fewer days in the week, “1” if the child adhered to their bedtime 3–4 days in the week, or “2” if the child adhered to the bedtime 5 days in the week.
Sleep duration
At the age 5 and 9 interviews, mothers were asked “How many hours of sleep a night does your child usually get during the week (integer hours)?” Age-appropriate sufficient sleep was defined as 11 hr or more sleep/night for 5-year-old and 10 hr or more sleep/night for 9-year-old [17–19]. Borderline sleep was when sleep duration was within 1 hr of the recommended amount for that age (10–11 hr/night at age 5 and 9–10 hr/night at age 9). Insufficient sleep was when sleep duration was less than the minimum borderline for that age (less than 10 hr/night at age 5 and less than 9 hr/night at age 9).
Childhood and adolescent BMI
Adolescent BMI was assessed through the questions, “How tall are you?” with adolescents asked to report number of feet and inches and “About how much do you weigh?” with youth asked to report number of pounds. Childhood height and weight were reported by mothers during age 3 in-home survey. BMI z-score was calculated based on 2000 CDC growth charts [20]. A z-score of 0 represents the 50th percentile (median) BMI for the adolescent’s age and sex, and a z-score > +1 SD corresponds to the 85th percentile and indicates that an individual is overweight. We adjusted for age 3 BMI z-score when predicting age 15 BMI z-score.
Adolescent weeknight sleep duration
Self-reported sleep duration at age 15 was calculated as the difference between adolescents’ self-reported typical weeknight bedtimes and wake times. Bedtimes and wake times were taken from responses to the following two questions: (1) “What time do you usually go to bed on week nights?” and (2) “What time do you usually wake up on weekday mornings?” For actigraphy-assessed sleep duration at age 15, we used wrist accelerometers (Actiwatch Spectrum, Philips-Respironics, Murrysville, PA) to measure typical weeknight sleep duration. Actigraphy data were scored using a standard algorithm validated previously [21–23]. Specifically, recordings were scored by at least two independent scorers, and reviewed and adjudicated by an independent third scorer if there was a discrepancy of >15 min in sleep duration between the initial two scorers. Typical weeknight sleep duration was calculated by averaging nightly sleep duration across multiple weeknights (in minutes/day).
Covariates
Our analyses adjusted for a range of sociodemographic factors that may be associated with adolescent sleep, including adolescent sex (male vs. female), age (in months), race (Black, Hispanic, Multiracial/Other race, vs. White), mother’s education (some college or more education vs. high school or less), and household income to poverty threshold (<49%, 50%–99%, 100%–199%, 200%–299%, vs. >300%) based on the US Census Bureau data, factoring in year and size of household [24]. Covariates were measured at age 15 except for sex determined at birth and age 3 BMI z-score. Continuous variables were centered at sample means (but not standardized).
Analytic strategy
First, we conducted latent class analysis (LCA) in MPlus 7.2 to identify underlying subgroups in our sample defined by different combinations of bedtime and sleep routines across child ages 5 and 9 [25]. The LCA provides model fit criteria, including the Akaike Information Criterion (AIC; with lower scores signifying better fit), Bayesian Information Criterion (BIC; lower scores signifying better fit), Entropy (ranges from 0 to 1, with 1 indicating greater precision in membership classification), and the Vuong–Lo–Mendell–Rubin Likelihood Ratio Test (VLMR-LRT; significant p values suggest that the estimated model fits the data better than a model with one less class). We used six indicators: (1) presence and timing of bedtimes, (2) bedtime adherence, and (3) habitual sleep duration, each measured at ages 5 and 9, in our LCA model. We then used chi-square tests to compare differences in bedtime routines and sleep behaviors between the identified groups. Second, using a series of General Linear Models in SAS 9.4, we tested associations of childhood bedtime routine class membership with age 15 BMI z-score. We also checked whether the childhood bedtime routine class membership predicted age 15 sleep duration (self-reports and actigraphy). In Model 1, only the childhood bedtime routine groups were included. In Model 2, covariates (except BMI z-score at age 3) were added. In Model 3, we additionally adjusted for age 3 BMI z-score. This residualized gain approach examines age 15 BMI as a function of bedtime routine after adjusting for initial (age 3) BMI [26].
Results
Descriptive statistics
Mean adolescent age was just over 15 years (SD = 0.61, Range = 14−18), and sex was evenly distributed (52% were male). About half (48%) were Black, non-Hispanic, 22% were Hispanic, 17% were White, non-Hispanic, and 13% were multiracial/other race. At age 15, 64% of their mothers had some college or greater education and 36% had high school or less education. Thirty-two percent of sample households lived in poverty (household income to poverty threshold < 100%); 27% were between thresholds of 100%−199%). On average, adolescents had about 8 hr self-reported sleep and 7.8 hr actigraphy sleep per weeknight. The unadjusted mean BMI z-score at age 15 was 0.7 and about 40% of the sample was overweight, with BMI z-scores higher than +1 and about 10% of the sample was obese, with BMI z-scores higher than +2.
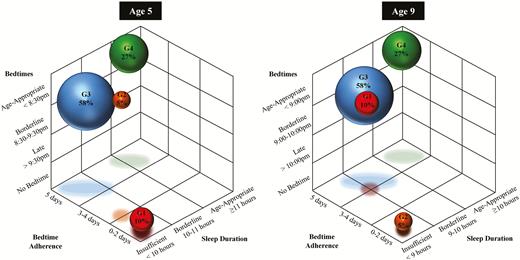
Identified groups of childhood bedtime and sleep routines
Figure 1 illustrates four identified groups based on presence and timing of a bedtime, bedtime adherence, and sleep duration at child ages 5 and 9, derived from the LCA. The model fit criteria best supported a 4-class solution; AIC and BIC were lower than ones with fewer classes, the Entropy was acceptable (0.751), and the VLMR-LRT p value was significant where that of a 5-class solution was not significant (Supplementary Table 1). The three dimensions in Figure 1 have valence: groups located in the top-center area have better childhood bedtime and sleep routines than those located in the bottom-center area. In the most optimal group, at age 5, 27% of children were characterized by having age-appropriate bedtimes, high adherence to those age-appropriate bedtimes, and age-appropriate sufficient sleep duration (Group 4; note the shadow of the green ball). More than half (58%) were characterized as having borderline bedtimes, high adherence to those borderline bedtimes, and insufficient sleep duration (Group 3; blue). The other two groups exhibited less desirable characteristics: 5% had borderline bedtimes with low adherence and insufficient sleep duration (Group 2; orange) and the rest 10% had no bedtime and insufficient sleep duration (Group 1; red). At age 9, these group characteristics mostly remained consistent, except Groups 1 and 2. Group 1 had no bedtime routine at age 5, but adopted borderline bedtimes at age 9. Group 2 had borderline bedtimes at age 5, but had no bedtime at age 9. Thus, Group 1 exhibited an improving bedtime routine trajectory, whereas Group 2’s bedtime routine trajectory worsened. Based on these distinctive characteristics, identified as clustered in the LCA, we labeled each group as Group 1 “No Bedtime Routine Age 5” (n = 210), Group 2 “No Bedtime Routine Age 9” (n = 119), Group 3 “Borderline Bedtimes Ages 5&9” (n = 1248), and Group 4 (reference) “Age-Appropriate Bedtime and Sleep Routines Ages 5&9” (n = 592). These four groups significantly differed from each other in terms of six variables of childhood bedtime and sleep routines (Table 1).
Four groups identified from latent class analysis based on the presence and timing of mother-reported bedtimes, bedtime adherence, and sleep duration at ages 5 and 9, N = 2169. G1 (Group 1) = “No Bedtime Routine Age 5” (n = 210); G2 (Group 2) = “No Bedtime Routine Age 9” (n = 119); G3 (Group 3) = “Borderline Bedtimes Ages 5&9” (n = 1248); G4 (Group 4) = “Age-Appropriate Bedtime and Sleep Routines Ages 5&9” (n = 592).
Characteristics of the identified latent groups of bedtime and sleep routines at ages 5 and 9
| . | Total Sample(N = 2169) . | Group 1 “No Bedtime Routine Age 5”(n = 210, 10%) . | Group 2 “No Bedtime Routine Age 9” (n = 119, 5%) . | Group 3 “Borderline Bedtimes Ages 5&9”(n = 1248, 58%) . | Group 4 “Age-Appropriate Bedtime and Sleep Routines Ages 5&9”(n = 592, 27%) . | χ2 test(df = 6) . | |
|---|---|---|---|---|---|---|---|
| Presence and timing of bedtimes | |||||||
| Age 5 | No bedtime | 7 | 58 | 29 | 0 | 0 | *** |
| Late: >9:30 pm | 12 | 7 | 21 | 18 | 0 | ||
| Borderline: 8:30–9:30 pm | 57 | 35 | 42 | 75 | 28 | ||
| Age-appropriate: <8:30 pm | 21 | 0 | 8 | 7 | 72 | ||
| Age 9 | No bedtime | 5 | 0 | 96 | 0 | 0 | *** |
| Late: >10:00 pm | 6 | 13 | 0 | 9 | 1 | ||
| Borderline: 9:00–10:00 pm | 53 | 63 | 4 | 71 | 23 | ||
| Age-appropriate: <9:00 pm | 35 | 23 | 0 | 21 | 76 | ||
| Bedtime adherence | |||||||
| Age 5 | 0–2 days | 13 | 100 | 43 | 0 | 4 | *** |
| 3–4 days | 26 | 0 | 20 | 32 | 24 | ||
| 5 days | 61 | 0 | 37 | 68 | 71 | ||
| Age 9 | 0–2 days | 21 | 28 | 100 | 17 | 13 | *** |
| 3–4 days | 30 | 33 | 0 | 32 | 31 | ||
| 5 days | 49 | 39 | 0 | 51 | 56 | ||
| Habitual sleep duration | |||||||
| Age 5 | Insufficient: <10 hr | 49 | 71 | 66 | 58 | 18 | *** |
| Borderline: 10–11 hr | 34 | 21 | 22 | 36 | 36 | ||
| Age-appropriate: ≥11 hr | 18 | 8 | 13 | 6 | 46 | ||
| Age 9 | Insufficient: <9 hr | 35 | 48 | 71 | 39 | 15 | *** |
| Borderline: 9–10 hr | 33 | 35 | 16 | 38 | 24 | ||
| Age-Appropriate: ≥10 hr | 32 | 17 | 13 | 23 | 61 | ||
| . | Total Sample(N = 2169) . | Group 1 “No Bedtime Routine Age 5”(n = 210, 10%) . | Group 2 “No Bedtime Routine Age 9” (n = 119, 5%) . | Group 3 “Borderline Bedtimes Ages 5&9”(n = 1248, 58%) . | Group 4 “Age-Appropriate Bedtime and Sleep Routines Ages 5&9”(n = 592, 27%) . | χ2 test(df = 6) . | |
|---|---|---|---|---|---|---|---|
| Presence and timing of bedtimes | |||||||
| Age 5 | No bedtime | 7 | 58 | 29 | 0 | 0 | *** |
| Late: >9:30 pm | 12 | 7 | 21 | 18 | 0 | ||
| Borderline: 8:30–9:30 pm | 57 | 35 | 42 | 75 | 28 | ||
| Age-appropriate: <8:30 pm | 21 | 0 | 8 | 7 | 72 | ||
| Age 9 | No bedtime | 5 | 0 | 96 | 0 | 0 | *** |
| Late: >10:00 pm | 6 | 13 | 0 | 9 | 1 | ||
| Borderline: 9:00–10:00 pm | 53 | 63 | 4 | 71 | 23 | ||
| Age-appropriate: <9:00 pm | 35 | 23 | 0 | 21 | 76 | ||
| Bedtime adherence | |||||||
| Age 5 | 0–2 days | 13 | 100 | 43 | 0 | 4 | *** |
| 3–4 days | 26 | 0 | 20 | 32 | 24 | ||
| 5 days | 61 | 0 | 37 | 68 | 71 | ||
| Age 9 | 0–2 days | 21 | 28 | 100 | 17 | 13 | *** |
| 3–4 days | 30 | 33 | 0 | 32 | 31 | ||
| 5 days | 49 | 39 | 0 | 51 | 56 | ||
| Habitual sleep duration | |||||||
| Age 5 | Insufficient: <10 hr | 49 | 71 | 66 | 58 | 18 | *** |
| Borderline: 10–11 hr | 34 | 21 | 22 | 36 | 36 | ||
| Age-appropriate: ≥11 hr | 18 | 8 | 13 | 6 | 46 | ||
| Age 9 | Insufficient: <9 hr | 35 | 48 | 71 | 39 | 15 | *** |
| Borderline: 9–10 hr | 33 | 35 | 16 | 38 | 24 | ||
| Age-Appropriate: ≥10 hr | 32 | 17 | 13 | 23 | 61 | ||
N = 2169. Percentages that characterize class characteristics are in bold to facilitate interpretation.
***p < .001.
Characteristics of the identified latent groups of bedtime and sleep routines at ages 5 and 9
| . | Total Sample(N = 2169) . | Group 1 “No Bedtime Routine Age 5”(n = 210, 10%) . | Group 2 “No Bedtime Routine Age 9” (n = 119, 5%) . | Group 3 “Borderline Bedtimes Ages 5&9”(n = 1248, 58%) . | Group 4 “Age-Appropriate Bedtime and Sleep Routines Ages 5&9”(n = 592, 27%) . | χ2 test(df = 6) . | |
|---|---|---|---|---|---|---|---|
| Presence and timing of bedtimes | |||||||
| Age 5 | No bedtime | 7 | 58 | 29 | 0 | 0 | *** |
| Late: >9:30 pm | 12 | 7 | 21 | 18 | 0 | ||
| Borderline: 8:30–9:30 pm | 57 | 35 | 42 | 75 | 28 | ||
| Age-appropriate: <8:30 pm | 21 | 0 | 8 | 7 | 72 | ||
| Age 9 | No bedtime | 5 | 0 | 96 | 0 | 0 | *** |
| Late: >10:00 pm | 6 | 13 | 0 | 9 | 1 | ||
| Borderline: 9:00–10:00 pm | 53 | 63 | 4 | 71 | 23 | ||
| Age-appropriate: <9:00 pm | 35 | 23 | 0 | 21 | 76 | ||
| Bedtime adherence | |||||||
| Age 5 | 0–2 days | 13 | 100 | 43 | 0 | 4 | *** |
| 3–4 days | 26 | 0 | 20 | 32 | 24 | ||
| 5 days | 61 | 0 | 37 | 68 | 71 | ||
| Age 9 | 0–2 days | 21 | 28 | 100 | 17 | 13 | *** |
| 3–4 days | 30 | 33 | 0 | 32 | 31 | ||
| 5 days | 49 | 39 | 0 | 51 | 56 | ||
| Habitual sleep duration | |||||||
| Age 5 | Insufficient: <10 hr | 49 | 71 | 66 | 58 | 18 | *** |
| Borderline: 10–11 hr | 34 | 21 | 22 | 36 | 36 | ||
| Age-appropriate: ≥11 hr | 18 | 8 | 13 | 6 | 46 | ||
| Age 9 | Insufficient: <9 hr | 35 | 48 | 71 | 39 | 15 | *** |
| Borderline: 9–10 hr | 33 | 35 | 16 | 38 | 24 | ||
| Age-Appropriate: ≥10 hr | 32 | 17 | 13 | 23 | 61 | ||
| . | Total Sample(N = 2169) . | Group 1 “No Bedtime Routine Age 5”(n = 210, 10%) . | Group 2 “No Bedtime Routine Age 9” (n = 119, 5%) . | Group 3 “Borderline Bedtimes Ages 5&9”(n = 1248, 58%) . | Group 4 “Age-Appropriate Bedtime and Sleep Routines Ages 5&9”(n = 592, 27%) . | χ2 test(df = 6) . | |
|---|---|---|---|---|---|---|---|
| Presence and timing of bedtimes | |||||||
| Age 5 | No bedtime | 7 | 58 | 29 | 0 | 0 | *** |
| Late: >9:30 pm | 12 | 7 | 21 | 18 | 0 | ||
| Borderline: 8:30–9:30 pm | 57 | 35 | 42 | 75 | 28 | ||
| Age-appropriate: <8:30 pm | 21 | 0 | 8 | 7 | 72 | ||
| Age 9 | No bedtime | 5 | 0 | 96 | 0 | 0 | *** |
| Late: >10:00 pm | 6 | 13 | 0 | 9 | 1 | ||
| Borderline: 9:00–10:00 pm | 53 | 63 | 4 | 71 | 23 | ||
| Age-appropriate: <9:00 pm | 35 | 23 | 0 | 21 | 76 | ||
| Bedtime adherence | |||||||
| Age 5 | 0–2 days | 13 | 100 | 43 | 0 | 4 | *** |
| 3–4 days | 26 | 0 | 20 | 32 | 24 | ||
| 5 days | 61 | 0 | 37 | 68 | 71 | ||
| Age 9 | 0–2 days | 21 | 28 | 100 | 17 | 13 | *** |
| 3–4 days | 30 | 33 | 0 | 32 | 31 | ||
| 5 days | 49 | 39 | 0 | 51 | 56 | ||
| Habitual sleep duration | |||||||
| Age 5 | Insufficient: <10 hr | 49 | 71 | 66 | 58 | 18 | *** |
| Borderline: 10–11 hr | 34 | 21 | 22 | 36 | 36 | ||
| Age-appropriate: ≥11 hr | 18 | 8 | 13 | 6 | 46 | ||
| Age 9 | Insufficient: <9 hr | 35 | 48 | 71 | 39 | 15 | *** |
| Borderline: 9–10 hr | 33 | 35 | 16 | 38 | 24 | ||
| Age-Appropriate: ≥10 hr | 32 | 17 | 13 | 23 | 61 | ||
N = 2169. Percentages that characterize class characteristics are in bold to facilitate interpretation.
***p < .001.
Associations of childhood bedtime and sleep routines with age 15 BMI z-score
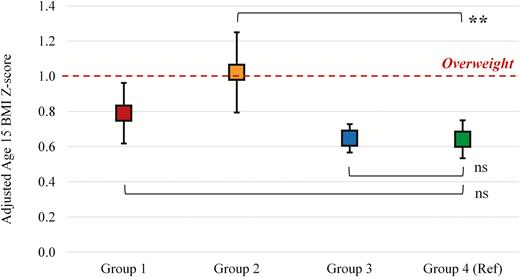
Table 2 shows how membership in these LCA-defined groups predict age 15 BMI z-scores. Model 1 revealed that adolescents in the three less optimal bedtime and sleep routine groups (Groups 1, 2, and 3) had significantly higher BMI at the p < .05 level than those in the most optimal, healthy bedtime and sleep routine reference group. However, after controlling for sociodemographic covariates (Model 2) and adjusting for age 3 BMI (Model 3), only the effect of Group 2 membership on age 15 BMI remained significant. Compared with adolescents in the “Age-Appropriate Bedtime and Sleep Routines Ages 5&9” (Group 4; reference), those included in the “No Bedtime Routine Age 9” had higher BMI, with a mean difference of +0.38 SD in BMI z units (p < .01, 95% CI = [0.13 to 0.63]). This difference was the same as a β coefficient from a supplementary model predicting changes in BMI (age 15 score − age 3 score) after adjusting for age 3 BMI, meaning that compared with those in the reference group, adolescents in the Group 2 exhibited 0.38 greater increase in BMI from ages 3 to 15. Figure 2 depicts least squares means of age 15 BMI z-score by groups after adjusting for all covariates. Adolescents in Group 4 had +0.64 SD of BMI from the population median (74th percentile), and those in Group 2 had +1.02 SD of BMI (85th percentile). Note that all the four groups had BMI higher than the US population mean (dashed horizontal line).
Results of general linear models examining the association between childhood bedtime and sleep routines and adolescent BMI, kg/m2z-score
| . | Age 15 BMI z-score . | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | ||||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 0.53 | <.0001 | [0.44, 0.62] | 0.35 | <.0001 | [0.18, 0.53] | 0.37 | 0.0004 | [0.17, 0.57] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | |||||||||
| Group 1 “No bedtime routine age 5” | 0.21 | 0.0198 | [0.03, 0.39] | 0.16 | 0.083 | [−0.02, 0.34] | 0.15 | 0.1395 | [−0.05, 0.35] |
| Group 2 “No bedtime routine age 9” | 0.39 | 0.0007 | [0.16, 0.61] | 0.34 | 0.0033 | [0.11, 0.56] | 0.38 | 0.0027 | [0.13, 0.63] |
| Group 3 “Borderline bedtimes ages 5&9” | 0.16 | 0.0045 | [0.05, 0.27] | 0.11 | 0.0611 | [−0.01, 0.22] | 0.01 | 0.929 | [−0.12, 0.13] |
| Child sex: Boy (ref: Girl) | −0.12 | 0.011 | [−0.22, −0.03] | −0.15 | 0.0059 | [−0.26, −0.04] | |||
| Child age | 0.02 | 0.6069 | [−0.06, 0.1] | 0.03 | 0.5624 | [−0.06, 0.11] | |||
| Child Race (ref: White, non-Hispanic) | |||||||||
| Black, non-Hispanic | 0.22 | 0.0026 | [0.08, 0.37] | 0.19 | 0.0258 | [0.02, 0.36] | |||
| Hispanic | 0.30 | 0.0003 | [0.14, 0.46] | 0.21 | 0.0266 | [0.02, 0.4] | |||
| Multiracial/Other | 0.15 | 0.102 | [−0.03, 0.34] | 0.22 | 0.0342 | [0.02, 0.43] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −0.04 | 0.4375 | [−0.15, 0.06] | −0.09 | 0.1449 | [−0.21, 0.03] | |||
| Income to Poverty Threshold (ref: ≥300%) | |||||||||
| <49% | 0.14 | 0.1179 | [−0.03, 0.31] | 0.12 | 0.2203 | [−0.07, 0.31] | |||
| 50%–99% | 0.18 | 0.0223 | [0.03, 0.33] | 0.09 | 0.2974 | [−0.08, 0.27] | |||
| 100%–199% | 0.20 | 0.0042 | [0.06, 0.34] | 0.16 | 0.0432 | [0, 0.32] | |||
| 200%–299% | 0.09 | 0.2946 | [−0.07, 0.25] | 0.08 | 0.4004 | [−0.1, 0.26] | |||
| Age 3 BMI z-score | 0.31 | <.0001 | [0.26, 0.35] | ||||||
| Fit Statistics | |||||||||
| F test | 5.28 | 0.0013 | 4.79 | <.0001 | 17.23 | <.0001 | |||
| . | Age 15 BMI z-score . | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | ||||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 0.53 | <.0001 | [0.44, 0.62] | 0.35 | <.0001 | [0.18, 0.53] | 0.37 | 0.0004 | [0.17, 0.57] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | |||||||||
| Group 1 “No bedtime routine age 5” | 0.21 | 0.0198 | [0.03, 0.39] | 0.16 | 0.083 | [−0.02, 0.34] | 0.15 | 0.1395 | [−0.05, 0.35] |
| Group 2 “No bedtime routine age 9” | 0.39 | 0.0007 | [0.16, 0.61] | 0.34 | 0.0033 | [0.11, 0.56] | 0.38 | 0.0027 | [0.13, 0.63] |
| Group 3 “Borderline bedtimes ages 5&9” | 0.16 | 0.0045 | [0.05, 0.27] | 0.11 | 0.0611 | [−0.01, 0.22] | 0.01 | 0.929 | [−0.12, 0.13] |
| Child sex: Boy (ref: Girl) | −0.12 | 0.011 | [−0.22, −0.03] | −0.15 | 0.0059 | [−0.26, −0.04] | |||
| Child age | 0.02 | 0.6069 | [−0.06, 0.1] | 0.03 | 0.5624 | [−0.06, 0.11] | |||
| Child Race (ref: White, non-Hispanic) | |||||||||
| Black, non-Hispanic | 0.22 | 0.0026 | [0.08, 0.37] | 0.19 | 0.0258 | [0.02, 0.36] | |||
| Hispanic | 0.30 | 0.0003 | [0.14, 0.46] | 0.21 | 0.0266 | [0.02, 0.4] | |||
| Multiracial/Other | 0.15 | 0.102 | [−0.03, 0.34] | 0.22 | 0.0342 | [0.02, 0.43] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −0.04 | 0.4375 | [−0.15, 0.06] | −0.09 | 0.1449 | [−0.21, 0.03] | |||
| Income to Poverty Threshold (ref: ≥300%) | |||||||||
| <49% | 0.14 | 0.1179 | [−0.03, 0.31] | 0.12 | 0.2203 | [−0.07, 0.31] | |||
| 50%–99% | 0.18 | 0.0223 | [0.03, 0.33] | 0.09 | 0.2974 | [−0.08, 0.27] | |||
| 100%–199% | 0.20 | 0.0042 | [0.06, 0.34] | 0.16 | 0.0432 | [0, 0.32] | |||
| 200%–299% | 0.09 | 0.2946 | [−0.07, 0.25] | 0.08 | 0.4004 | [−0.1, 0.26] | |||
| Age 3 BMI z-score | 0.31 | <.0001 | [0.26, 0.35] | ||||||
| Fit Statistics | |||||||||
| F test | 5.28 | 0.0013 | 4.79 | <.0001 | 17.23 | <.0001 | |||
n = 1942 adolescents who provided age 15 BMI z-score; 1938 and 1306 observations were used in Models 2 and 3, respectively, due to missing responses in covariates.
Results of general linear models examining the association between childhood bedtime and sleep routines and adolescent BMI, kg/m2z-score
| . | Age 15 BMI z-score . | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | ||||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 0.53 | <.0001 | [0.44, 0.62] | 0.35 | <.0001 | [0.18, 0.53] | 0.37 | 0.0004 | [0.17, 0.57] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | |||||||||
| Group 1 “No bedtime routine age 5” | 0.21 | 0.0198 | [0.03, 0.39] | 0.16 | 0.083 | [−0.02, 0.34] | 0.15 | 0.1395 | [−0.05, 0.35] |
| Group 2 “No bedtime routine age 9” | 0.39 | 0.0007 | [0.16, 0.61] | 0.34 | 0.0033 | [0.11, 0.56] | 0.38 | 0.0027 | [0.13, 0.63] |
| Group 3 “Borderline bedtimes ages 5&9” | 0.16 | 0.0045 | [0.05, 0.27] | 0.11 | 0.0611 | [−0.01, 0.22] | 0.01 | 0.929 | [−0.12, 0.13] |
| Child sex: Boy (ref: Girl) | −0.12 | 0.011 | [−0.22, −0.03] | −0.15 | 0.0059 | [−0.26, −0.04] | |||
| Child age | 0.02 | 0.6069 | [−0.06, 0.1] | 0.03 | 0.5624 | [−0.06, 0.11] | |||
| Child Race (ref: White, non-Hispanic) | |||||||||
| Black, non-Hispanic | 0.22 | 0.0026 | [0.08, 0.37] | 0.19 | 0.0258 | [0.02, 0.36] | |||
| Hispanic | 0.30 | 0.0003 | [0.14, 0.46] | 0.21 | 0.0266 | [0.02, 0.4] | |||
| Multiracial/Other | 0.15 | 0.102 | [−0.03, 0.34] | 0.22 | 0.0342 | [0.02, 0.43] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −0.04 | 0.4375 | [−0.15, 0.06] | −0.09 | 0.1449 | [−0.21, 0.03] | |||
| Income to Poverty Threshold (ref: ≥300%) | |||||||||
| <49% | 0.14 | 0.1179 | [−0.03, 0.31] | 0.12 | 0.2203 | [−0.07, 0.31] | |||
| 50%–99% | 0.18 | 0.0223 | [0.03, 0.33] | 0.09 | 0.2974 | [−0.08, 0.27] | |||
| 100%–199% | 0.20 | 0.0042 | [0.06, 0.34] | 0.16 | 0.0432 | [0, 0.32] | |||
| 200%–299% | 0.09 | 0.2946 | [−0.07, 0.25] | 0.08 | 0.4004 | [−0.1, 0.26] | |||
| Age 3 BMI z-score | 0.31 | <.0001 | [0.26, 0.35] | ||||||
| Fit Statistics | |||||||||
| F test | 5.28 | 0.0013 | 4.79 | <.0001 | 17.23 | <.0001 | |||
| . | Age 15 BMI z-score . | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | Model 3 . | ||||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 0.53 | <.0001 | [0.44, 0.62] | 0.35 | <.0001 | [0.18, 0.53] | 0.37 | 0.0004 | [0.17, 0.57] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | |||||||||
| Group 1 “No bedtime routine age 5” | 0.21 | 0.0198 | [0.03, 0.39] | 0.16 | 0.083 | [−0.02, 0.34] | 0.15 | 0.1395 | [−0.05, 0.35] |
| Group 2 “No bedtime routine age 9” | 0.39 | 0.0007 | [0.16, 0.61] | 0.34 | 0.0033 | [0.11, 0.56] | 0.38 | 0.0027 | [0.13, 0.63] |
| Group 3 “Borderline bedtimes ages 5&9” | 0.16 | 0.0045 | [0.05, 0.27] | 0.11 | 0.0611 | [−0.01, 0.22] | 0.01 | 0.929 | [−0.12, 0.13] |
| Child sex: Boy (ref: Girl) | −0.12 | 0.011 | [−0.22, −0.03] | −0.15 | 0.0059 | [−0.26, −0.04] | |||
| Child age | 0.02 | 0.6069 | [−0.06, 0.1] | 0.03 | 0.5624 | [−0.06, 0.11] | |||
| Child Race (ref: White, non-Hispanic) | |||||||||
| Black, non-Hispanic | 0.22 | 0.0026 | [0.08, 0.37] | 0.19 | 0.0258 | [0.02, 0.36] | |||
| Hispanic | 0.30 | 0.0003 | [0.14, 0.46] | 0.21 | 0.0266 | [0.02, 0.4] | |||
| Multiracial/Other | 0.15 | 0.102 | [−0.03, 0.34] | 0.22 | 0.0342 | [0.02, 0.43] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −0.04 | 0.4375 | [−0.15, 0.06] | −0.09 | 0.1449 | [−0.21, 0.03] | |||
| Income to Poverty Threshold (ref: ≥300%) | |||||||||
| <49% | 0.14 | 0.1179 | [−0.03, 0.31] | 0.12 | 0.2203 | [−0.07, 0.31] | |||
| 50%–99% | 0.18 | 0.0223 | [0.03, 0.33] | 0.09 | 0.2974 | [−0.08, 0.27] | |||
| 100%–199% | 0.20 | 0.0042 | [0.06, 0.34] | 0.16 | 0.0432 | [0, 0.32] | |||
| 200%–299% | 0.09 | 0.2946 | [−0.07, 0.25] | 0.08 | 0.4004 | [−0.1, 0.26] | |||
| Age 3 BMI z-score | 0.31 | <.0001 | [0.26, 0.35] | ||||||
| Fit Statistics | |||||||||
| F test | 5.28 | 0.0013 | 4.79 | <.0001 | 17.23 | <.0001 | |||
n = 1942 adolescents who provided age 15 BMI z-score; 1938 and 1306 observations were used in Models 2 and 3, respectively, due to missing responses in covariates.
Longitudinal associations of childhood bedtime and sleep routine groups with adolescent BMI z-score. Group 1 = “No Bedtime Routine Age 5”; Group 2 = “No Bedtime Routine Age 9”; Group 3 = “Borderline Bedtimes Ages 5&9”; Group 4 = “Age-Appropriate Bedtime and Sleep Routines Ages 5&9.” n = 1942 adolescents who provided age 15 height and weight to calculate BMI z-score. Symbols indicate least squares (LS) means of age 15 BMI z-score adjusted for age 3 BMI z-score as well as sociodemographic covariates. Compared with adolescents in Group 4 (reference), those in Group 2 had 0.38 SD higher BMI z-score. Adolescents in Group 4 had +0.64 SD from the population median (74th percentile), and those in Group 2 had +1.02 SD (85th percentile) that corresponds to the risk of overweight (≥+1 SD or 85th percentile). LS means for Group 1 and 3 did not differ from that of the reference group. **p < .01; ns = not significant.
Associations of childhood bedtime and sleep routines with age 15 sleep duration
Table 3 shows the results of our confirmatory analyses examining the associations of the identified childhood bedtime and sleep routine groups with adolescent self-reported weeknight sleep duration. Model 1 revealed that adolescents who were included in the three less optimal bedtime and sleep routine groups (Groups 1, 2, and 3) as children all reported significantly shorter age 15 sleep duration, compared with those in the healthy bedtime and sleep routine group (Group 4; reference). These effects remained significant after adjusting for covariates in Model 2. Adolescents in the “No Bedtime Routine Age 5” (Group 1), “No Bedtime Routine Age 9” (Group 2), and Borderline Bedtimes Ages 5 and 9 (Group 3) reported shorter sleep than the reference group, by 20, 19, and 11 min, respectively. Post hoc pairwise comparisons showed that there was no significant mean difference in self-reported sleep duration among groups 1, 2, and 3.
Results of general linear models examining the association between childhood bedtime and sleep routines and adolescent self-reported weeknight sleep duration (minutes)
| . | Age 15 self-reported weeknight Sleep duration (minutes) . | |||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2: . | ||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 491.38 | <.0001 | [485.14, 497.63] | 492.13 | <.0001 | [480.26, 504.01] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | ||||||
| Group 1 “No bedtime routine age 5” | −21.75 | 0.0004 | [−33.86, −9.65] | −20.42 | 0.001 | [−32.57, −8.28] |
| Group 2 “No bedtime routine age 9” | −21.23 | 0.006 | [−36.36, −6.09] | −19.40 | 0.0119 | [−34.52, −4.28] |
| Group 3 “Borderline bedtimes ages 5&9” | −12.62 | 0.0011 | [−20.18, −5.05] | −10.90 | 0.0052 | [−18.55, −3.26] |
| Child sex: Boy (ref: Girl) | 8.26 | 0.0122 | [1.8, 14.72] | |||
| Child age | −2.77 | 0.3082 | [−8.09, 2.56] | |||
| Child Race (ref: White, non-Hispanic) | ||||||
| Black, non-Hispanic | −15.68 | 0.0018 | [−25.52, −5.84] | |||
| Hispanic | 0.34 | 0.9509 | [−10.54, 11.22] | |||
| Multiracial/Other | 0.44 | 0.9442 | [−11.84, 12.72] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −6.94 | 0.0596 | [−14.16, 0.28] | |||
| Income to Poverty Threshold (ref: ≥300%) | ||||||
| <49% | 17.49 | 0.003 | [5.95, 29.03] | |||
| 50%–99% | 8.96 | 0.0938 | [−1.52, 19.45] | |||
| 100%–199% | 6.87 | 0.1522 | [−2.54, 16.28] | |||
| 200%–299% | −1.76 | 0.7522 | [−12.67, 9.15] | |||
| Fit Statistics | ||||||
| F test | 6.22 | 0.0003 | 5.01 | <.0001 | ||
| . | Age 15 self-reported weeknight Sleep duration (minutes) . | |||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2: . | ||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 491.38 | <.0001 | [485.14, 497.63] | 492.13 | <.0001 | [480.26, 504.01] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | ||||||
| Group 1 “No bedtime routine age 5” | −21.75 | 0.0004 | [−33.86, −9.65] | −20.42 | 0.001 | [−32.57, −8.28] |
| Group 2 “No bedtime routine age 9” | −21.23 | 0.006 | [−36.36, −6.09] | −19.40 | 0.0119 | [−34.52, −4.28] |
| Group 3 “Borderline bedtimes ages 5&9” | −12.62 | 0.0011 | [−20.18, −5.05] | −10.90 | 0.0052 | [−18.55, −3.26] |
| Child sex: Boy (ref: Girl) | 8.26 | 0.0122 | [1.8, 14.72] | |||
| Child age | −2.77 | 0.3082 | [−8.09, 2.56] | |||
| Child Race (ref: White, non-Hispanic) | ||||||
| Black, non-Hispanic | −15.68 | 0.0018 | [−25.52, −5.84] | |||
| Hispanic | 0.34 | 0.9509 | [−10.54, 11.22] | |||
| Multiracial/Other | 0.44 | 0.9442 | [−11.84, 12.72] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −6.94 | 0.0596 | [−14.16, 0.28] | |||
| Income to Poverty Threshold (ref: ≥300%) | ||||||
| <49% | 17.49 | 0.003 | [5.95, 29.03] | |||
| 50%–99% | 8.96 | 0.0938 | [−1.52, 19.45] | |||
| 100%–199% | 6.87 | 0.1522 | [−2.54, 16.28] | |||
| 200%–299% | −1.76 | 0.7522 | [−12.67, 9.15] | |||
| Fit Statistics | ||||||
| F test | 6.22 | 0.0003 | 5.01 | <.0001 | ||
N = 2097 adolescents who provided age 15 self-reported sleep duration; in Model 2, 2093 observations were used due to missing responses in covariates.
Results of general linear models examining the association between childhood bedtime and sleep routines and adolescent self-reported weeknight sleep duration (minutes)
| . | Age 15 self-reported weeknight Sleep duration (minutes) . | |||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2: . | ||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 491.38 | <.0001 | [485.14, 497.63] | 492.13 | <.0001 | [480.26, 504.01] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | ||||||
| Group 1 “No bedtime routine age 5” | −21.75 | 0.0004 | [−33.86, −9.65] | −20.42 | 0.001 | [−32.57, −8.28] |
| Group 2 “No bedtime routine age 9” | −21.23 | 0.006 | [−36.36, −6.09] | −19.40 | 0.0119 | [−34.52, −4.28] |
| Group 3 “Borderline bedtimes ages 5&9” | −12.62 | 0.0011 | [−20.18, −5.05] | −10.90 | 0.0052 | [−18.55, −3.26] |
| Child sex: Boy (ref: Girl) | 8.26 | 0.0122 | [1.8, 14.72] | |||
| Child age | −2.77 | 0.3082 | [−8.09, 2.56] | |||
| Child Race (ref: White, non-Hispanic) | ||||||
| Black, non-Hispanic | −15.68 | 0.0018 | [−25.52, −5.84] | |||
| Hispanic | 0.34 | 0.9509 | [−10.54, 11.22] | |||
| Multiracial/Other | 0.44 | 0.9442 | [−11.84, 12.72] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −6.94 | 0.0596 | [−14.16, 0.28] | |||
| Income to Poverty Threshold (ref: ≥300%) | ||||||
| <49% | 17.49 | 0.003 | [5.95, 29.03] | |||
| 50%–99% | 8.96 | 0.0938 | [−1.52, 19.45] | |||
| 100%–199% | 6.87 | 0.1522 | [−2.54, 16.28] | |||
| 200%–299% | −1.76 | 0.7522 | [−12.67, 9.15] | |||
| Fit Statistics | ||||||
| F test | 6.22 | 0.0003 | 5.01 | <.0001 | ||
| . | Age 15 self-reported weeknight Sleep duration (minutes) . | |||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2: . | ||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 491.38 | <.0001 | [485.14, 497.63] | 492.13 | <.0001 | [480.26, 504.01] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | ||||||
| Group 1 “No bedtime routine age 5” | −21.75 | 0.0004 | [−33.86, −9.65] | −20.42 | 0.001 | [−32.57, −8.28] |
| Group 2 “No bedtime routine age 9” | −21.23 | 0.006 | [−36.36, −6.09] | −19.40 | 0.0119 | [−34.52, −4.28] |
| Group 3 “Borderline bedtimes ages 5&9” | −12.62 | 0.0011 | [−20.18, −5.05] | −10.90 | 0.0052 | [−18.55, −3.26] |
| Child sex: Boy (ref: Girl) | 8.26 | 0.0122 | [1.8, 14.72] | |||
| Child age | −2.77 | 0.3082 | [−8.09, 2.56] | |||
| Child Race (ref: White, non-Hispanic) | ||||||
| Black, non-Hispanic | −15.68 | 0.0018 | [−25.52, −5.84] | |||
| Hispanic | 0.34 | 0.9509 | [−10.54, 11.22] | |||
| Multiracial/Other | 0.44 | 0.9442 | [−11.84, 12.72] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −6.94 | 0.0596 | [−14.16, 0.28] | |||
| Income to Poverty Threshold (ref: ≥300%) | ||||||
| <49% | 17.49 | 0.003 | [5.95, 29.03] | |||
| 50%–99% | 8.96 | 0.0938 | [−1.52, 19.45] | |||
| 100%–199% | 6.87 | 0.1522 | [−2.54, 16.28] | |||
| 200%–299% | −1.76 | 0.7522 | [−12.67, 9.15] | |||
| Fit Statistics | ||||||
| F test | 6.22 | 0.0003 | 5.01 | <.0001 | ||
N = 2097 adolescents who provided age 15 self-reported sleep duration; in Model 2, 2093 observations were used due to missing responses in covariates.
Table 4 shows results predicting age 15 actigraphy weeknight sleep duration. After adjusting for the covariates, the results of Model 2 showed that, compared with those in the reference group, adolescents in the “No Bedtime Routine Age 9” (Group 2) and in the “Borderline Bedtimes Ages 5&9” (Group 3) had 35 and 16 min shorter actigraphic sleep duration, respectively. There was no significant difference between groups 2 and 3. The least squares means of age 15 actigraphy sleep duration were 7.8 hr (95% CI = [7.5, 8.1]), 7.5 hr (95% CI = [7.1, 7.9]), 7.8 hr (95% CI = [7.7, 7.9]), and 8.1 hr (95% CI = [7.9, 8.3]) per night for Groups 1, 2, 3, and 4, respectively. Thus, our additional analyses indicated that the identified groups of bedtime and sleep routines at ages 5 and 9 were predictive of age 15 sleep duration. Results were consistent when the analyses were executed employing only the 592 adolescents who provided two or more valid weeknights of actigraphy-assessed sleep data at age 15.
Results of general linear models examining the association between childhood bedtime and sleep routines and adolescent actigraphy weeknight nighttime sleep duration (minutes)
| . | Age 15 actigraphy weeknight Sleep duration (minutes) . | |||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | ||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 483.98 | <.0001 | [473.19, 494.77] | 488.64 | <.0001 | [468.44, 508.84] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | ||||||
| Group 1 “No bedtime routine age 5” | −16.82 | 0.1016 | [−36.96, 3.33] | −16.50 | 0.1049 | [−36.46, 3.46] |
| Group 2 “No bedtime routine age 9” | −31.58 | 0.0238 | [−58.95, −4.2] | −34.70 | 0.013 | [−62.06, −7.34] |
| Group 3 “Borderline bedtimes ages 5&9” | −18.41 | 0.0061 | [−31.55, −5.28] | −16.31 | 0.0148 | [−29.42, −3.21] |
| Child sex: Boy (ref: Girl) | −16.08 | 0.0048 | [−27.24, −4.92] | |||
| Child age | −4.03 | 0.4869 | [−15.41, 7.35] | |||
| Child Race (ref: White, non-Hispanic) | ||||||
| Black, non-Hispanic | −17.28 | 0.0451 | [−34.17, −0.38] | |||
| Hispanic | 9.45 | 0.3037 | [−8.58, 27.47] | |||
| Multiracial/Other | −19.34 | 0.0718 | [−40.39, 1.72] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −2.12 | 0.7415 | [−14.72, 10.48] | |||
| Income to Poverty Threshold (ref: ≥300%) | ||||||
| <49% | 20.23 | 0.0437 | [0.58, 39.88] | |||
| 50%–99% | 10.67 | 0.2454 | [−7.35, 28.69] | |||
| 100%–199% | 17.44 | 0.0346 | [1.26, 33.62] | |||
| 200%–299% | 6.85 | 0.4745 | [−11.95, 25.65] | |||
| Fit Statistics | ||||||
| F test | 3.27 | 0.0208 | 3.19 | 0.0001 | ||
| . | Age 15 actigraphy weeknight Sleep duration (minutes) . | |||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | ||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 483.98 | <.0001 | [473.19, 494.77] | 488.64 | <.0001 | [468.44, 508.84] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | ||||||
| Group 1 “No bedtime routine age 5” | −16.82 | 0.1016 | [−36.96, 3.33] | −16.50 | 0.1049 | [−36.46, 3.46] |
| Group 2 “No bedtime routine age 9” | −31.58 | 0.0238 | [−58.95, −4.2] | −34.70 | 0.013 | [−62.06, −7.34] |
| Group 3 “Borderline bedtimes ages 5&9” | −18.41 | 0.0061 | [−31.55, −5.28] | −16.31 | 0.0148 | [−29.42, −3.21] |
| Child sex: Boy (ref: Girl) | −16.08 | 0.0048 | [−27.24, −4.92] | |||
| Child age | −4.03 | 0.4869 | [−15.41, 7.35] | |||
| Child Race (ref: White, non-Hispanic) | ||||||
| Black, non-Hispanic | −17.28 | 0.0451 | [−34.17, −0.38] | |||
| Hispanic | 9.45 | 0.3037 | [−8.58, 27.47] | |||
| Multiracial/Other | −19.34 | 0.0718 | [−40.39, 1.72] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −2.12 | 0.7415 | [−14.72, 10.48] | |||
| Income to Poverty Threshold (ref: ≥300%) | ||||||
| <49% | 20.23 | 0.0437 | [0.58, 39.88] | |||
| 50%–99% | 10.67 | 0.2454 | [−7.35, 28.69] | |||
| 100%–199% | 17.44 | 0.0346 | [1.26, 33.62] | |||
| 200%–299% | 6.85 | 0.4745 | [−11.95, 25.65] | |||
| Fit Statistics | ||||||
| F test | 3.27 | 0.0208 | 3.19 | 0.0001 | ||
n = 637 adolescents who provided 1 or more valid weeknights of actigraphy-assessed sleep data at age 15; in Model 2, 634 observations were used due to missing responses in covariates; consistent results were found with 592 adolescents who provided two or more valid weeknights of actigraphy-assessed sleep data at age 15.
Results of general linear models examining the association between childhood bedtime and sleep routines and adolescent actigraphy weeknight nighttime sleep duration (minutes)
| . | Age 15 actigraphy weeknight Sleep duration (minutes) . | |||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | ||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 483.98 | <.0001 | [473.19, 494.77] | 488.64 | <.0001 | [468.44, 508.84] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | ||||||
| Group 1 “No bedtime routine age 5” | −16.82 | 0.1016 | [−36.96, 3.33] | −16.50 | 0.1049 | [−36.46, 3.46] |
| Group 2 “No bedtime routine age 9” | −31.58 | 0.0238 | [−58.95, −4.2] | −34.70 | 0.013 | [−62.06, −7.34] |
| Group 3 “Borderline bedtimes ages 5&9” | −18.41 | 0.0061 | [−31.55, −5.28] | −16.31 | 0.0148 | [−29.42, −3.21] |
| Child sex: Boy (ref: Girl) | −16.08 | 0.0048 | [−27.24, −4.92] | |||
| Child age | −4.03 | 0.4869 | [−15.41, 7.35] | |||
| Child Race (ref: White, non-Hispanic) | ||||||
| Black, non-Hispanic | −17.28 | 0.0451 | [−34.17, −0.38] | |||
| Hispanic | 9.45 | 0.3037 | [−8.58, 27.47] | |||
| Multiracial/Other | −19.34 | 0.0718 | [−40.39, 1.72] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −2.12 | 0.7415 | [−14.72, 10.48] | |||
| Income to Poverty Threshold (ref: ≥300%) | ||||||
| <49% | 20.23 | 0.0437 | [0.58, 39.88] | |||
| 50%–99% | 10.67 | 0.2454 | [−7.35, 28.69] | |||
| 100%–199% | 17.44 | 0.0346 | [1.26, 33.62] | |||
| 200%–299% | 6.85 | 0.4745 | [−11.95, 25.65] | |||
| Fit Statistics | ||||||
| F test | 3.27 | 0.0208 | 3.19 | 0.0001 | ||
| . | Age 15 actigraphy weeknight Sleep duration (minutes) . | |||||
|---|---|---|---|---|---|---|
| . | Model 1 . | Model 2 . | ||||
| . | B . | P . | 95% CI . | B . | P . | 95% CI . |
| Intercept | 483.98 | <.0001 | [473.19, 494.77] | 488.64 | <.0001 | [468.44, 508.84] |
| Groups of Bedtime and Sleep Routines at Ages 5&9 (ref: Group 4) | ||||||
| Group 1 “No bedtime routine age 5” | −16.82 | 0.1016 | [−36.96, 3.33] | −16.50 | 0.1049 | [−36.46, 3.46] |
| Group 2 “No bedtime routine age 9” | −31.58 | 0.0238 | [−58.95, −4.2] | −34.70 | 0.013 | [−62.06, −7.34] |
| Group 3 “Borderline bedtimes ages 5&9” | −18.41 | 0.0061 | [−31.55, −5.28] | −16.31 | 0.0148 | [−29.42, −3.21] |
| Child sex: Boy (ref: Girl) | −16.08 | 0.0048 | [−27.24, −4.92] | |||
| Child age | −4.03 | 0.4869 | [−15.41, 7.35] | |||
| Child Race (ref: White, non-Hispanic) | ||||||
| Black, non-Hispanic | −17.28 | 0.0451 | [−34.17, −0.38] | |||
| Hispanic | 9.45 | 0.3037 | [−8.58, 27.47] | |||
| Multiracial/Other | −19.34 | 0.0718 | [−40.39, 1.72] | |||
| Mothers’ Education: Some college or above (ref: High school or less) | −2.12 | 0.7415 | [−14.72, 10.48] | |||
| Income to Poverty Threshold (ref: ≥300%) | ||||||
| <49% | 20.23 | 0.0437 | [0.58, 39.88] | |||
| 50%–99% | 10.67 | 0.2454 | [−7.35, 28.69] | |||
| 100%–199% | 17.44 | 0.0346 | [1.26, 33.62] | |||
| 200%–299% | 6.85 | 0.4745 | [−11.95, 25.65] | |||
| Fit Statistics | ||||||
| F test | 3.27 | 0.0208 | 3.19 | 0.0001 | ||
n = 637 adolescents who provided 1 or more valid weeknights of actigraphy-assessed sleep data at age 15; in Model 2, 634 observations were used due to missing responses in covariates; consistent results were found with 592 adolescents who provided two or more valid weeknights of actigraphy-assessed sleep data at age 15.
Discussion
This study empirically identified four groups characterizing childhood bedtime and sleep routines in the FFCWS, specifically, children having “No Bedtime Routine Age 5,” “No Bedtime Routine Age 9,” “Borderline Bedtimes Age 5&9,” and “Age-Appropriate Bedtime and Sleep Routines Ages 5&9.” Compared with adolescents with age-appropriate sleep health, who met current pediatric recommendations for both bedtimes and sleep duration, those in the other groups had shorter self-reported and actigraphy-assessed sleep duration at age 15. Thus, sleep health patterns during childhood are predictive of subsequent sleep duration during adolescence in expected ways. Furthermore, those with no bedtimes and no bedtime routine in childhood exhibited higher BMI as adolescents, demonstrating longitudinal associations of early childhood bedtime and sleep routines with adolescent body weight even after adjusting for age 3 body weight. These results add to the empirical evidence that early life sleep and contemporaneous sleep are important to weight status during adolescence [4, 5, 8, 27], reinforcing that multidimensional aspects of childhood sleep health (presence and timing of bedtimes, adherence to bedtimes, and habitual sleep duration) have consequences for adolescent BMI. This study highlights the clinical importance of guiding parents on parenting practices related to bedtimes and sleep.
Our findings demonstrate heterogeneity in bedtime and sleep routines experienced during childhood within a sample of adolescents in urban households. In our sample, only 27% had age-appropriate bedtimes, high adherence to those age-appropriate bedtimes, and age-appropriate sufficient sleep duration at ages 5 and 9 (Figure 1). Adolescents in the other three groups were distinguished by having no bedtime, a later than age-appropriate bedtime, lower bedtime adherence, and/or insufficient sleep during ages 5 and 9. In particular, 15% had no bedtime at either age 5 or 9. The different groups of childhood bedtime and sleep routines found in this study provide a broader view of how multiple aspects of bedtime and sleep variables combine to reveal modifiable threats to children’s sleep, important for subsequent adolescent sleep and health.
We found that adolescents in the “No Bedtime Routine Age 9” group exhibited a greater BMI at age 15 after adjusting for age 3 BMI than those in the “Age-Appropriate Bedtime and Sleep Routines Ages 5&9” group. A recent meta-analysis showed that short sleep duration was associated with a greater risk of developing overweight or obesity in childhood and adolescence [8]. Our study extends this previous work by demonstrating that childhood bedtime and sleep routine groups based on multiple indicators (rather than simply sleep duration) were associated with adolescent BMI. Specifically, adolescents in “No Bedtime Routine Age 9” group had +1.02 SD of BMI z-score, which corresponds to the risk of overweight (>+1 SD according to the WHO growth reference) [28]. Importantly, this group of children exhibited a worsening bedtime routine trajectory; they had borderline bedtimes with low adherence at age 5, but had mostly abandoned them at age 9. Adolescents who had no bedtime at age 5 but adopted borderline bedtimes at age 9 (Group 1) did not have significantly higher BMI at age 15 than those in the reference group. These findings advance our understanding about the longitudinal impact of childhood bedtime routines. Having a regular bedtime routine from early childhood is important for sleep and BMI, as suggested by previous research [29], yet maintaining a bedtime routine continuously and improving it over time may be more important, as found in this study. Future preventive efforts may need to focus on educating parents about the importance of establishing and maintaining consistent, age-appropriate bedtimes from early childhood.
Having later bedtimes, fewer bedtime routines, and less sleep in childhood was associated with shorter sleep duration in adolescence, evaluated via both self-reported and actigraphy measures. Importantly, only 27% of sample adolescents averaged 8 hr or more measured sleep per night, meeting the age-appropriate minimum amount of sleep recommended by the American Academy of Sleep Medicine [17, 30]. The rest obtained less than 8 hr of sleep per night, on average, raising concerns about their development and health [31–34].
There are limitations in this study that provide guidance for future research. First, we used self-reported height and weight to calculate BMI, which may reflect self-report bias or other measurement error. Future studies may benefit from using measured height and weight to increase the validity of BMI. Second, although we controlled for an extensive list of sociodemographic and family characteristics, there may still be omitted factors that affect bedtime and sleep routines. For example, commuting time to school may be a confounder, as school start times were previously found to be associated with wake time and time in bed [35]. Third, in our sample, the correlation between self-reported sleep duration and actigraphy-assessed sleep duration at age 15 was not high (r = 0.10, p < .05). This may reflect potential recall bias in reporting sleep duration, particularly in adolescent sample. Future studies focusing on adolescent sleep should pay attention to this issue.
Conclusion
This study adds to the empirical evidence by providing prospective data on a large national sample of urban youth with objective measurement of sleep and BMI at mid-adolescence. The findings support the pediatric recommendation that having, and adhering to, age-appropriate and regular bedtime routines during childhood is associated with sufficient sleep and healthy body weight in adolescence. Continued research should identify additional modifiable factors to improve adolescent sleep and weight status. Establishing favorable sleep health behaviors for children and helping them to consistently follow these patterns are things families with children can start practicing now to improve future health.
Funding
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health under award numbers R01HD36916, R01HD39135, R01HD40421; and R01HD073352 (to Hale), as well as a consortium of private foundations. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest statement. The authors have indicated no financial conflicts of interest relevant to the current study. Outside of the current work, Orfeu M. Buxton received two subcontract grants to Penn State from Mobile Sleep Technologies (NSF/STTR #1622766 and NIH/NIA SBIR R43AG056250). No off-label or investigational use is indicated.




Comments