-
PDF
- Split View
-
Views
-
Cite
Cite
Saana Myllyntausta, Paula Salo, Erkki Kronholm, Jaana Pentti, Mika Kivimäki, Jussi Vahtera, Sari Stenholm, Changes in Sleep Difficulties During the Transition to Statutory Retirement, Sleep, Volume 41, Issue 1, January 2018, zsx182, https://doi.org/10.1093/sleep/zsx182
Close - Share Icon Share
Abstract
This study examined changes in sleep during the transition from full-time work to statutory retirement. Both the prevalence of any sleep difficulty and the prevalence of specific sleep difficulties, such as difficulties falling asleep, difficulties maintaining sleep, waking up too early in the morning, and nonrestorative sleep, were examined.
Data from the Finnish Public Sector study were used. The study population consisted of 5,807 Finnish public sector employees who retired on statutory basis between 2000 and 2011. The participants responded on the Jenkins Sleep Problem Scale Questionnaire before and after retirement in surveys conducted every 4 years.
At the last study wave before retirement, 30% of the participants had sleep difficulties. Prevalence of any sleep difficulty decreased during the retirement transition: the risk ratio (RR) for having sleep difficulties in the first study wave following retirement compared with the last study wave preceding retirement was 0.89 (95% confidence interval [CI] 0.85–0.94). During the retirement transition, both waking up too early in the morning (RR = 0.76, 95% CI 0.69–0.82) and nonrestorative sleep (RR = 0.47, 95% CI 0.42–0.53) decreased, whereas there was no change in difficulties falling asleep or difficulties maintaining sleep. The decreases in sleep difficulties occurred primarily among those with psychological distress, suboptimal self-rated health, short sleep duration, and job strain before retirement.
These longitudinal data suggest that transition to statutory retirement is associated with a decrease in sleep difficulties, especially waking up too early in the morning and nonrestorative sleep.
This study provides evidence that sleep difficulties are common during the final working years and that sleep difficulties decrease during the transition from full-time work to statutory retirement. Divergent changes were observed in specific types of sleep difficulties around retirement; both waking up too early in the morning and nonrestorative sleep decreased substantially during the transition to retirement, whereas difficulties falling asleep and difficulties maintaining sleep did not change during this period. The changes in sleep difficulties were found to occur primarily among those with suboptimal self-rated health, psychological distress, and short sleep duration before retirement. Further studies with shorter measurement intervals are needed to determine whether the changes in sleep difficulties occur immediately following retirement.
INTRODUCTION
Across the Western countries, a growing proportion of the population is approaching the age of retirement or have already retired. Retirement is a major transition from both an individual and societal perspective, but its impacts on sleep have not been widely studied. Older age is associated with higher prevalence of sleep disturbance as older people tend to sleep less efficiently, awaken more frequently, and have more difficulty returning to sleep.1–3 Consequently, as populations are aging, sleeping problems can be expected to become more prevalent. However, various studies have found a strong positive correlation between occupational stress and sleep disturbances,4–7 and as retirement removes work-related stressors, it could also bring about decreases in sleep difficulties.
There are only a few studies on the association of retirement with sleep duration8–10 and sleep difficulties.11–14 We have previously shown that sleep duration increases following retirement.10 Retirement has also been associated with a reduction in the at-risk sleep patterns, defined as sleep durations under 7 hours and over 9 hours.9 By contrast, findings on the impact of retirement on sleep difficulties are inconsistent. In previous cross-sectional research, where retirees have been compared with those still working, retirement has been associated with both a higher prevalence of sleep difficulties12,15 and no major worsening in sleep quality.11 Some longitudinal studies have found sleep difficulties to decrease following retirement.13,14 For example, in the GAZEL study, the odds for general sleep disturbances were 26% lower during a 7-year post-retirement period than during a 7-year period before retirement.13 The authors of the study suggested that this decrease may have resulted at least partly from the removal of work-related stressors. The VISAT study examined different types of sleep difficulties and found that participants who retired after baseline measurement reported less premature awakenings at follow-up compared with those who continued working.14 In that study, retirement was not associated with changes in any other sleep difficulties, including difficulties falling or maintaining sleep or getting back to sleep. Longitudinal studies comparing retirees with nonretirees, however, are open to selection bias as they cannot distinguish whether the differences in sleep between the two groups are due to retirement, or because people who retire differ from those who continue to work. A within-individual follow-up with repeated data on different types of sleep difficulties around retirement from the same individuals would provide a stronger design to study the effects of retirement on sleep.
The aim of this study was to examine changes in self-rated sleep difficulties around retirement, by using repeated measurements of sleep difficulties around the transition from full-time work to statutory retirement. Risk for sleep difficulties was compared at two study waves measured 4 years apart in three different time periods: pre-retirement, during the transition to retirement, and post-retirement. Both the changes in any sleep difficulty and in four specific sleep difficulties, including difficulties falling asleep, difficulties maintaining sleep during the night, waking up too early in the morning, and nonrestorative sleep, were examined. We additionally examined several sociodemographic and work-related factors as well as health-related behaviors and factors as possible pre-retirement predictors for changes in sleep difficulties.
METHODS
Study Population
Data were drawn from the Finnish Public Sector (FPS) study, an ongoing prospective occupational cohort study. All employees from the participating organizations of the FPS study (ten towns and six hospital districts), who had been working for a minimum of 6 months between 1991 and 2005, comprised the FPS study population (n = 151901).16 The nested survey cohorts included all those employed at the time of the surveys or who had left the organizations after participating in an earlier survey. For this study, data from the repeated surveys performed in 2000–2002, 2004, and 2008 for current employees and in 2005, 2009, and 2013 for retirees and other leavers were used. The survey data were successfully linked to the Finnish Centre for Pension’s register (retirement date and type), to employers’ records (birth date, gender, and occupational title), and the National Health Registers (diseases and medications) by using personal identity codes assigned to all citizens in Finland. For the analyses, anonymized data without the identity codes were used. The FPS study was approved by the Ethics Committee of the Hospital District of Helsinki and Uusimaa.
The selection of the study sample is illustrated in a flow chart in Figure 1. Of the FPS cohort members, we included those persons who had retired at the statutory retirement age (i.e., old-age retirement) as their first awarded pension scheme (n = 5,898). Thus, participants that had retired on a part-time retirement (n = 3,718) or on health grounds (n = 5,623) or because of unemployment (n = 284) were excluded from this study, because these types of retirement are potentially related to the causes that may affect sleep (e.g., disease) and thus subject to reverse causation bias.
For the analysis, the data were centered around the actual retirement date. There were three possible study waves before retirement (wave–3, wave–2, wave–1), and three possible waves after retirement (wave+1, wave+2, wave+3). The interval between each successive wave was on average 4 years. For this study, the study population was further restricted to those participants who had provided information on sleep difficulties in at least two surveys, one immediately before and after the transition to statutory retirement (i.e., in wave–1 and wave+1) (n = 5,807). The final sample chosen for the analyses (n = 5,807) was similar to the eligible population (i.e., the 9,433 statutory retirees) in terms of the distributions of gender (22% men in the eligible population vs. 20% in the final sample), retirement age (73% retired between ages 60 and 64 in both the eligible population and the final sample), occupational status (38% manual workers in the eligible population vs. 35% in the final sample), and the prevalence of sleep difficulties before retirement (31% in the eligible population vs. 30% in the final sample). Each participant may have taken part in a maximum of four study waves and, on average, participants provided data on sleep difficulties at 3.7 (range 2–4) of the possible four study waves during a follow-up of 8–12 years. The relation of the survey years to the study waves around retirement is demonstrated in Supplementary Table S1.
Assessment of Retirement
All gainful employment in Finland is insured in a pension plan and accrues a pension. The Finnish Centre for Pensions coordinates all the earning-related pensions for permanent residents in Finland17 and was thus able to provide data on each participants’ retirement. The start dates for pension were obtained for all participants from 2000 through 2011, irrespective of the participants’ employment status or workplace at follow-up. The start dates for pension were used to calculate a retirement age for each participant. Retirement age was used as a continuous variable when adjusted for in the statistical analyses, and also as a pre-retirement factor for which three categories of retirement age were formed: <60 years, 60–64 years, and >64 years.
According to the public sector Employees’ Pension Act, the statutory retirement age was generally 63–65 years until the end of 2004, and 63–68 years from 2005 onwards in Finland. However, some employees had kept their earlier retirement age from the previous pension act in which pension ages were below 63 years in some occupations (e.g., 60 years for primary school teachers).
Assessment of Sleep Difficulties
In each survey wave, sleep difficulties were measured with the Jenkins Sleep Problem Scale.18 This scale comprises four questions that address the occurrence of difficulties falling asleep, difficulties maintaining sleep during the night (i.e., “waking up several times per night”), waking up too early in the morning (i.e., “having troubles staying sleep (including too early awakening)”), and nonrestorative sleep (i.e., “waking up after the usual amount of sleep feeling tired and worn out”). Participants were asked to report the frequency of each of these difficulties during the past 4 weeks (never, one–three nights per month, one night per week, two–four nights per week, five–six nights per week, and nearly every night). To examine changes of any sleep difficulty, referred now on as any sleep difficulty, a variable was created based on the most frequent symptom the participant reported. The four items of the scale were also analyzed individually, referred now on as specific sleep difficulties. Both any sleep difficulty and the specific sleep difficulties were all dichotomized, and the participant was considered to have a sleep difficulty if the frequency was higher than four nights per week.
Assessment of Pre-Retirement Factors
Sociodemographic and Work-Related Factors
The participants’ gender and occupational title were obtained from the employers’ registers. The occupational titles by the last-known occupation preceding retirement were used to categorize occupational status into three groups: upper-grade nonmanual workers (e.g., teachers, physicians), lower-grade nonmanual workers (e.g., registered nurses, technicians), and manual workers (e.g., cleaners, maintenance workers). From the last questionnaire preceding retirement (wave–1), we obtained information on participants’ marital status (married vs. not married), whether they did shift or night work (no vs. yes; the latter consisting of shift work with or without night shifts, regular night work, and other irregular work) and whether they had job strain (no vs. yes). Job strain was ascertained using scales of job control and job demands from the shorter version of the Job Content Questionnaire,19,20 using the median values from the year 2000 survey in the entire FPS cohort as the cutoff points to identify the participant with job strain (a high demands and a low control score).
Health-Related Behaviors and Factors
Information on health-related behaviors and factors was obtained from the last questionnaire preceding retirement (wave–1), apart from the chronic conditions for which information in all available pre-retirement waves (wave–3, wave–2, or wave–1) was taken into account. Physical activity was assessed with reports on average weekly hours of leisure-time physical activity (including commuting) within previous year in walking, brisk walking, jogging and running, and their equivalent activities.21,22 The time spent on activity at each intensity level in hours per week was multiplied by the average energy expenditure of each activity, expressed in metabolic equivalent (MET). Physical activity was used as a continuous variable when used as a covariate in the analyses. When used as a pre-retirement factor, it was categorized into four groups: inactive (<7 MET hours/week), low (7–14 MET hours/week), medium (14–30 MET hours/week), and high (≥30 MET hours/week). Alcohol use was used as a continuous variable when used as a covariate in the analyses and categorized according to habitual frequencies of beer, wine, and spirits consumption into none, moderate, and heavy, when used as a pre-retirement factor. The limit for heavy alcohol use was set as >16 drinks/week for women and >24 drinks/week for men, as these limits correspond to the lower limit for heavy use of alcohol set by the Finnish Ministry of Health and Social Affairs.23,24 Smoking status was categorized into never, former, or current.
Self-reports on body weight and height were used to calculate BMI (kg/m2), which was used as a continuous variable when used as a covariate in the analyses. When used as a pre-retirement factor, BMI was categorized into underweight (<18.5 kg/m2), normal weight (BMI 18.5–25 kg/m2), overweight (BMI 25–29.9 kg/m2), and obesity (BMI ≥30 kg/m2). Self-rated health was assessed with a 5-point scale (1 = good,…, 5 = poor) and was then dichotomized into good (response scores 1 and 2) and suboptimal (scores 3 to 5). Psychological distress was measured with the 12-item version of General Health Questionnaire25 and the total score of the questionnaire was used as a continuous variable when used as a covariate in the analyses. When used as a pre-retirement factor, a cutoff point of three or more symptoms was used to indicate psychological distress (no vs. yes). Sleep duration was assessed by asking participants how many hours they usually sleep per 24 hours and used as a continuous variable when used as a covariate in the analyses. When used as a pre-retirement factor, sleep duration was categorized into short (≤6.5 hours), mid-range (7–8.5 hours), and long (≥9 hours). We also examined four chronic conditions: arthritis, cardiometabolic diseases, asthma, and cancer. For arthritis, we combined information from the questionnaires (osteoarthritis) and the nation-wide registers (rheumatoid arthritis) based on the Social Insurance Institution of Finland’s (SII) Drug Reimbursement Register. From the SII Drug Reimbursement Register, we also obtained information on cardiometabolic diseases (diabetes and coronary heart disease combined) and asthma. Information of cancer was obtained from the Finnish Cancer Registry.
Statistical Analyses
Associations of sleep difficulties and the characteristics of the study population before retirement (wave–1) were examined by calculating risk ratios (RRs) and their 95% confidence intervals (CIs) in each group using log-binominal regression while adjusting for gender, retirement age, and occupational status. Prevalence estimates and their 95% CIs were calculated for any sleep difficulty and the four specific sleep difficulties in each study wave around retirement by using log-binominal regression analyses with generalized estimating equations (GEEs). The GEE model controls for the intra-individual correlation between the repeated measurements using an exchangeable correlation structure and is not sensitive to measurements missing completely at random.26,27 These analyses were similarly adjusted for gender, retirement age, and occupational status.
In order to study changes in sleep difficulties around the transition to retirement, we constructed three consecutive periods: the pre-retirement period (from wave−3 to wave−2), the retirement transition (from wave−1 to wave+1), and the post-retirement period (from wave+2 to wave+3). We then analyzed the changes in any sleep difficulty and the four specific sleep difficulties within each period by comparing the prevalence of sleep difficulties at the latter study wave to the previous study wave (e.g., wave+1 compared with wave-1) and the results are shown in RRs and their 95% CIs. Two models were created: Model 1, adjusted for gender, retirement age, and occupational status, and Model 2, which was additionally adjusted for marital status, shift or night work, job strain, physical activity, alcohol use, smoking, BMI, self-rated health, psychological distress, arthritis, cardiometabolic diseases, asthma, cancer, and sleep duration before retirement. To examine whether the RRs differed among the pre-retirement period, the retirement transition, and the post-retirement period, period × time interaction effects were tested, in which time variable was treated as a continuous variable.
To examine factors predicting changes in any sleep difficulty during retirement transition, we calculated RRs and their 95% CIs in the study wave immediately after retirement (wave+1) compared with the study wave immediately before retirement (wave–1) for each level of the characteristics of the study population before retirement. In addition, interactions between the changes in sleep difficulties and the characteristics before retirement (time × pre-retirement characteristic interaction) were analyzed. We additionally examined whether those pre-retirement factors that predicted changes in any sleep difficulty also predicted changes in the four specific sleep difficulties during the retirement transition. This was done by calculating RRs and their 95% CIs in the study wave immediately after retirement (wave+1) compared with the study wave immediately before retirement (wave–1) for each level of all the pre-retirement factors that predicted changes in any sleep difficulty. These models were adjusted for gender, retirement age, and occupational status.
Finally, we conducted an additional analysis to assess the robustness of the associations found in the main analyses by using a lower cut-off point for the occurrence of sleep difficulties. In this analysis, participant was considered to have a sleep difficulty if the frequency was higher than two nights per week. In addition, we examined the distribution of responses to the four questions of the Jenkins Sleep Problem Scale about the frequency of each sleep difficulty in the study waves immediately before retirement (wave–1) and after retirement (wave+1). This was done to clarify how the four specific sleep difficulties changed during the retirement transition. The SAS 9.4 Statistical Package was used for all of the analyses (SAS Institute Inc., Cary, North Carolina).
RESULTS
The pre-retirement characteristics of the study population (n= 5,807) are shown in Table 1. The majority of the study population were women (80%) and married (74%). The average age at retirement was 61.9 (SD = 2.0) years, and the majority of this population did not do shift or night work (70%) and did not experience job strain (75%) before retirement. As seen in Table 1, health-related factors and health-related behaviors were strongly associated with the sleep difficulties before retirement. From the sociodemographic and work-related factors, female gender, job strain, and manual occupational status were associated with sleep difficulties at pre-retirement. On the contrary, retirement age, marital status, or shift or night work were not associated with sleep difficulties before retirement.
Characteristics of the Study Population (n = 5,807) Before Retirement.
| Characteristics . | n (%) . | Sleep difficulties before retirementa . | ||
|---|---|---|---|---|
| RR . | 95% CI . | |||
| Gender | ||||
| Men | 1162 (20) | 1 | ||
| Women | 4645 (80) | 1.19 | 1.05 | 1.34 |
| Retirement age | ||||
| <60 | 691 (12) | 1 | 0.90 | 1.20 |
| 60–64 | 4266 (73) | 1.00 | ||
| >64 | 850 (15) | 1.19 | 0.99 | 1.43 |
| Occupational status | ||||
| Upper grade nonmanual | 2205 (38) | 1 | ||
| Lower grade nonmanual | 1551 (27) | 1.01 | 0.90 | 1.14 |
| Manual | 2023 (35) | 1.17 | 1.05 | 1.30 |
| Marital status | ||||
| Married | 4263 (74) | 1 | ||
| Not married | 1474 (26) | 0.92 | 0.83 | 1.03 |
| Shift/night work | ||||
| No | 4003 (70) | 1 | ||
| Yes | 1713 (30) | 0.93 | 0.83 | 1.04 |
| Job strain | ||||
| No | 4314 (75) | 1 | ||
| Yes | 1413 (25) | 1.26 | 1.13 | 1.40 |
| Physical activity | ||||
| Inactive | 1130 (20) | 1.20 | 1.05 | 1.37 |
| Low | 1304 (23) | 1.11 | 0.98 | 1.27 |
| Moderate | 1691 (29) | 1.04 | 0.92 | 1.18 |
| High | 1646 (29) | 1 | ||
| Alcohol use | ||||
| None | 918 (16) | 1 | ||
| Moderate | 4416 (77) | 1.02 | 0.90 | 1.17 |
| Heavy | 437 (8) | 1.35 | 1.11 | 1.64 |
| Smoking | ||||
| Never | 4234 (75) | 1 | ||
| Former | 943 (17) | 1.20 | 1.06 | 1.36 |
| Current | 498 (9) | 0.89 | 0.75 | 1.07 |
| Body mass index | ||||
| Underweight (<18.5 kg/m2) | 25 (0.5) | 1.24 | 0.64 | 2.39 |
| Normal weight (18.5–24.9 kg/m2) | 2382 (43) | 1 | ||
| Overweight (25–29.9 kg/m2) | 2279 (41) | 1.08 | 0.97 | 1.20 |
| Obese (≥30 kg/m2) | 898 (16) | 1.30 | 1.14 | 1.48 |
| Self-rated health | ||||
| Good | 3647 (63) | 1 | ||
| Suboptimal | 2126 (37) | 2.03 | 1.85 | 2.23 |
| Psychological distress | ||||
| No | 4419 (76) | 1 | ||
| Yes | 1364 (24) | 2.10 | 1.91 | 2.31 |
| Arthritis | ||||
| No | 3520 (61) | 1 | ||
| Yes | 2287 (39) | 1.47 | 1.34 | 1.61 |
| Cardiometabolic diseases | ||||
| No | 5535 (95) | 1 | ||
| Yes | 272 (5) | 1.08 | 0.86 | 1.34 |
| Asthma | ||||
| No | 5570 (96) | 1 | ||
| Yes | 237 (4) | 1.30 | 1.06 | 1.60 |
| Cancer | ||||
| No | 5595 (96) | 1 | ||
| Yes | 212 (4) | 1.09 | 0.86 | 1.39 |
| Sleep duration before retirement | ||||
| Short (≤6.5 hours/24 hours) | 1729 (30) | 1.82 | 1.65 | 2.00 |
| Mid-range (7–8.5 hours/24 hours) | 3884 (67) | 1 | ||
| Long (≥9 hours/24 hours) | 154 (3) | 1.32 | 1.00 | 1.75 |
| Characteristics . | n (%) . | Sleep difficulties before retirementa . | ||
|---|---|---|---|---|
| RR . | 95% CI . | |||
| Gender | ||||
| Men | 1162 (20) | 1 | ||
| Women | 4645 (80) | 1.19 | 1.05 | 1.34 |
| Retirement age | ||||
| <60 | 691 (12) | 1 | 0.90 | 1.20 |
| 60–64 | 4266 (73) | 1.00 | ||
| >64 | 850 (15) | 1.19 | 0.99 | 1.43 |
| Occupational status | ||||
| Upper grade nonmanual | 2205 (38) | 1 | ||
| Lower grade nonmanual | 1551 (27) | 1.01 | 0.90 | 1.14 |
| Manual | 2023 (35) | 1.17 | 1.05 | 1.30 |
| Marital status | ||||
| Married | 4263 (74) | 1 | ||
| Not married | 1474 (26) | 0.92 | 0.83 | 1.03 |
| Shift/night work | ||||
| No | 4003 (70) | 1 | ||
| Yes | 1713 (30) | 0.93 | 0.83 | 1.04 |
| Job strain | ||||
| No | 4314 (75) | 1 | ||
| Yes | 1413 (25) | 1.26 | 1.13 | 1.40 |
| Physical activity | ||||
| Inactive | 1130 (20) | 1.20 | 1.05 | 1.37 |
| Low | 1304 (23) | 1.11 | 0.98 | 1.27 |
| Moderate | 1691 (29) | 1.04 | 0.92 | 1.18 |
| High | 1646 (29) | 1 | ||
| Alcohol use | ||||
| None | 918 (16) | 1 | ||
| Moderate | 4416 (77) | 1.02 | 0.90 | 1.17 |
| Heavy | 437 (8) | 1.35 | 1.11 | 1.64 |
| Smoking | ||||
| Never | 4234 (75) | 1 | ||
| Former | 943 (17) | 1.20 | 1.06 | 1.36 |
| Current | 498 (9) | 0.89 | 0.75 | 1.07 |
| Body mass index | ||||
| Underweight (<18.5 kg/m2) | 25 (0.5) | 1.24 | 0.64 | 2.39 |
| Normal weight (18.5–24.9 kg/m2) | 2382 (43) | 1 | ||
| Overweight (25–29.9 kg/m2) | 2279 (41) | 1.08 | 0.97 | 1.20 |
| Obese (≥30 kg/m2) | 898 (16) | 1.30 | 1.14 | 1.48 |
| Self-rated health | ||||
| Good | 3647 (63) | 1 | ||
| Suboptimal | 2126 (37) | 2.03 | 1.85 | 2.23 |
| Psychological distress | ||||
| No | 4419 (76) | 1 | ||
| Yes | 1364 (24) | 2.10 | 1.91 | 2.31 |
| Arthritis | ||||
| No | 3520 (61) | 1 | ||
| Yes | 2287 (39) | 1.47 | 1.34 | 1.61 |
| Cardiometabolic diseases | ||||
| No | 5535 (95) | 1 | ||
| Yes | 272 (5) | 1.08 | 0.86 | 1.34 |
| Asthma | ||||
| No | 5570 (96) | 1 | ||
| Yes | 237 (4) | 1.30 | 1.06 | 1.60 |
| Cancer | ||||
| No | 5595 (96) | 1 | ||
| Yes | 212 (4) | 1.09 | 0.86 | 1.39 |
| Sleep duration before retirement | ||||
| Short (≤6.5 hours/24 hours) | 1729 (30) | 1.82 | 1.65 | 2.00 |
| Mid-range (7–8.5 hours/24 hours) | 3884 (67) | 1 | ||
| Long (≥9 hours/24 hours) | 154 (3) | 1.32 | 1.00 | 1.75 |
aRisk ratios and their 95% confidence intervals for sleep difficulties at the study wave immediately before retirement (wave–1) are derived from log-binominal regression analyses. Analyses were adjusted for gender, retirement age, and occupational status.
RR = risk ratio; CI = confidence interval.
Characteristics of the Study Population (n = 5,807) Before Retirement.
| Characteristics . | n (%) . | Sleep difficulties before retirementa . | ||
|---|---|---|---|---|
| RR . | 95% CI . | |||
| Gender | ||||
| Men | 1162 (20) | 1 | ||
| Women | 4645 (80) | 1.19 | 1.05 | 1.34 |
| Retirement age | ||||
| <60 | 691 (12) | 1 | 0.90 | 1.20 |
| 60–64 | 4266 (73) | 1.00 | ||
| >64 | 850 (15) | 1.19 | 0.99 | 1.43 |
| Occupational status | ||||
| Upper grade nonmanual | 2205 (38) | 1 | ||
| Lower grade nonmanual | 1551 (27) | 1.01 | 0.90 | 1.14 |
| Manual | 2023 (35) | 1.17 | 1.05 | 1.30 |
| Marital status | ||||
| Married | 4263 (74) | 1 | ||
| Not married | 1474 (26) | 0.92 | 0.83 | 1.03 |
| Shift/night work | ||||
| No | 4003 (70) | 1 | ||
| Yes | 1713 (30) | 0.93 | 0.83 | 1.04 |
| Job strain | ||||
| No | 4314 (75) | 1 | ||
| Yes | 1413 (25) | 1.26 | 1.13 | 1.40 |
| Physical activity | ||||
| Inactive | 1130 (20) | 1.20 | 1.05 | 1.37 |
| Low | 1304 (23) | 1.11 | 0.98 | 1.27 |
| Moderate | 1691 (29) | 1.04 | 0.92 | 1.18 |
| High | 1646 (29) | 1 | ||
| Alcohol use | ||||
| None | 918 (16) | 1 | ||
| Moderate | 4416 (77) | 1.02 | 0.90 | 1.17 |
| Heavy | 437 (8) | 1.35 | 1.11 | 1.64 |
| Smoking | ||||
| Never | 4234 (75) | 1 | ||
| Former | 943 (17) | 1.20 | 1.06 | 1.36 |
| Current | 498 (9) | 0.89 | 0.75 | 1.07 |
| Body mass index | ||||
| Underweight (<18.5 kg/m2) | 25 (0.5) | 1.24 | 0.64 | 2.39 |
| Normal weight (18.5–24.9 kg/m2) | 2382 (43) | 1 | ||
| Overweight (25–29.9 kg/m2) | 2279 (41) | 1.08 | 0.97 | 1.20 |
| Obese (≥30 kg/m2) | 898 (16) | 1.30 | 1.14 | 1.48 |
| Self-rated health | ||||
| Good | 3647 (63) | 1 | ||
| Suboptimal | 2126 (37) | 2.03 | 1.85 | 2.23 |
| Psychological distress | ||||
| No | 4419 (76) | 1 | ||
| Yes | 1364 (24) | 2.10 | 1.91 | 2.31 |
| Arthritis | ||||
| No | 3520 (61) | 1 | ||
| Yes | 2287 (39) | 1.47 | 1.34 | 1.61 |
| Cardiometabolic diseases | ||||
| No | 5535 (95) | 1 | ||
| Yes | 272 (5) | 1.08 | 0.86 | 1.34 |
| Asthma | ||||
| No | 5570 (96) | 1 | ||
| Yes | 237 (4) | 1.30 | 1.06 | 1.60 |
| Cancer | ||||
| No | 5595 (96) | 1 | ||
| Yes | 212 (4) | 1.09 | 0.86 | 1.39 |
| Sleep duration before retirement | ||||
| Short (≤6.5 hours/24 hours) | 1729 (30) | 1.82 | 1.65 | 2.00 |
| Mid-range (7–8.5 hours/24 hours) | 3884 (67) | 1 | ||
| Long (≥9 hours/24 hours) | 154 (3) | 1.32 | 1.00 | 1.75 |
| Characteristics . | n (%) . | Sleep difficulties before retirementa . | ||
|---|---|---|---|---|
| RR . | 95% CI . | |||
| Gender | ||||
| Men | 1162 (20) | 1 | ||
| Women | 4645 (80) | 1.19 | 1.05 | 1.34 |
| Retirement age | ||||
| <60 | 691 (12) | 1 | 0.90 | 1.20 |
| 60–64 | 4266 (73) | 1.00 | ||
| >64 | 850 (15) | 1.19 | 0.99 | 1.43 |
| Occupational status | ||||
| Upper grade nonmanual | 2205 (38) | 1 | ||
| Lower grade nonmanual | 1551 (27) | 1.01 | 0.90 | 1.14 |
| Manual | 2023 (35) | 1.17 | 1.05 | 1.30 |
| Marital status | ||||
| Married | 4263 (74) | 1 | ||
| Not married | 1474 (26) | 0.92 | 0.83 | 1.03 |
| Shift/night work | ||||
| No | 4003 (70) | 1 | ||
| Yes | 1713 (30) | 0.93 | 0.83 | 1.04 |
| Job strain | ||||
| No | 4314 (75) | 1 | ||
| Yes | 1413 (25) | 1.26 | 1.13 | 1.40 |
| Physical activity | ||||
| Inactive | 1130 (20) | 1.20 | 1.05 | 1.37 |
| Low | 1304 (23) | 1.11 | 0.98 | 1.27 |
| Moderate | 1691 (29) | 1.04 | 0.92 | 1.18 |
| High | 1646 (29) | 1 | ||
| Alcohol use | ||||
| None | 918 (16) | 1 | ||
| Moderate | 4416 (77) | 1.02 | 0.90 | 1.17 |
| Heavy | 437 (8) | 1.35 | 1.11 | 1.64 |
| Smoking | ||||
| Never | 4234 (75) | 1 | ||
| Former | 943 (17) | 1.20 | 1.06 | 1.36 |
| Current | 498 (9) | 0.89 | 0.75 | 1.07 |
| Body mass index | ||||
| Underweight (<18.5 kg/m2) | 25 (0.5) | 1.24 | 0.64 | 2.39 |
| Normal weight (18.5–24.9 kg/m2) | 2382 (43) | 1 | ||
| Overweight (25–29.9 kg/m2) | 2279 (41) | 1.08 | 0.97 | 1.20 |
| Obese (≥30 kg/m2) | 898 (16) | 1.30 | 1.14 | 1.48 |
| Self-rated health | ||||
| Good | 3647 (63) | 1 | ||
| Suboptimal | 2126 (37) | 2.03 | 1.85 | 2.23 |
| Psychological distress | ||||
| No | 4419 (76) | 1 | ||
| Yes | 1364 (24) | 2.10 | 1.91 | 2.31 |
| Arthritis | ||||
| No | 3520 (61) | 1 | ||
| Yes | 2287 (39) | 1.47 | 1.34 | 1.61 |
| Cardiometabolic diseases | ||||
| No | 5535 (95) | 1 | ||
| Yes | 272 (5) | 1.08 | 0.86 | 1.34 |
| Asthma | ||||
| No | 5570 (96) | 1 | ||
| Yes | 237 (4) | 1.30 | 1.06 | 1.60 |
| Cancer | ||||
| No | 5595 (96) | 1 | ||
| Yes | 212 (4) | 1.09 | 0.86 | 1.39 |
| Sleep duration before retirement | ||||
| Short (≤6.5 hours/24 hours) | 1729 (30) | 1.82 | 1.65 | 2.00 |
| Mid-range (7–8.5 hours/24 hours) | 3884 (67) | 1 | ||
| Long (≥9 hours/24 hours) | 154 (3) | 1.32 | 1.00 | 1.75 |
aRisk ratios and their 95% confidence intervals for sleep difficulties at the study wave immediately before retirement (wave–1) are derived from log-binominal regression analyses. Analyses were adjusted for gender, retirement age, and occupational status.
RR = risk ratio; CI = confidence interval.
Changes in Sleep Difficulties Around Retirement
Figure 2 shows the estimated prevalence of any sleep difficulty before retirement, during the retirement transition, and after retirement after adjusting for gender, retirement age, and occupational status. A slightly increasing trend in the prevalence of sleep difficulties with increasing age was observed before the retirement transition. During the retirement transition, there was a decrease in the prevalence of any sleep difficulty from 30% in wave–1 to 26% in wave+1. The change in the prevalence of sleep difficulties also differed among the periods (period × time interaction, p < .0001). The RR for any sleep difficulty was 1.12 (95% CI 1.03–1.22) during the pre-retirement period (wave–2 compared with wave–3), 0.88 (95% CI 0.85–0.92) during the retirement transition (wave+1 compared with wave–1), and borderline significant RR 1.06 (95% 95 CI 0.98–1.15) during the post-retirement period (wave+3 compared with wave+2) when adjusted for gender, retirement age, and occupational status (Model 1) (Table 2). When the analyses were further adjusted for marital status, shift or night work, job strain, physical activity, alcohol use, smoking, BMI, self-rated health, psychological distress, arthritis, cardiometabolic diseases, asthma, cancer, and sleep duration before retirement (Model 2), the results remained very similar with only minor differences in the RRs and their 95% CIs.
Sleep difficulties in relation to retirement. Prevalence of any sleep difficulty in each study wave and 95% confidence interval derived from log-binominal regression analyses with generalized estimating equations. Time between each study wave is approximately 4 years. Adjusted for gender, retirement age, and occupational status. The period of the retirement transition is s hown in grey.
Prevalence estimates in each study wave around retirement are shown in Figure 3 for all four specific sleep difficulties. During the retirement transition, a decrease in the prevalence of waking up too early in the morning and nonrestorative sleep was observed, whereas the prevalence estimates of difficulties falling asleep and difficulties maintaining sleep seemed to remain at approximately the same level. As shown in Table 2, after adjustment for all covariates (Model 2), difficulties falling asleep increased during the pre-retirement period (RR 1.29, 95% CI 1.00–1.65), but not during the retirement transition or the post-retirement period. As it comes to difficulties maintaining sleep during the night, we observed an increase during the pre-retirement period (RR 1.23, 95% CI 1.11–1.36) and during the post-retirement period (RR 1.12, 95% CI 1.02–1.23), but not during the retirement transition. No statistically significant changes in waking up too early in the morning were observed during the pre-retirement or post-retirement periods, whereas a decrease was observed during the retirement transition (RR 0.76, 95% CI 0.70–0.83). Similarly, there were no changes in nonrestorative sleep during the pre-retirement and post-retirement periods, whereas during the retirement transition, a decrease was observed (RR 0.47, 95% CI 0.41–0.53).
Changes in Any Sleep Difficulty and the Specific Types of Sleep Difficulties During the Pre-retirement Period, the Retirement Transition, and the Post-retirement Period.
| . | Pre-retirement perioda . | Retirement transitionb . | Post-retirement periodc . | . |
|---|---|---|---|---|
| RR (95% CI) . | RR (95% CI) . | RR (95% CI) . | Interaction with time p . | |
| Any sleep difficulty | ||||
| Model 1 | 1.12 (1.03–1.22) | 0.88 (0.85–0.92) | 1.06 (0.98–1.15) | <.0001 |
| Model 2 | 1.12 (1.03–1.23) | 0.89 (0.85–0.93) | 1.08 (0.99–1.18) | <.0001 |
| Difficulties falling asleep | ||||
| Model 1 | 1.23 (0.96–1.56) | 0.91 (0.80–1.03) | 1.04 (0.84–1.29) | .063 |
| Model 2 | 1.29 (1.00–1.65) | 0.90 (0.79–1.04) | 1.05 (0.83–1.34) | .050 |
| Difficulties maintaining sleep during the night | ||||
| Model 1 | 1.23 (1.11–1.36) | 0.97 (0.92–1.02) | 1.08 (0.99–1.18) | <.0001 |
| Model 2 | 1.23 (1.11–1.36) | 0.98 (0.93–1.03) | 1.12 (1.02–1.23) | <.001 |
| Waking up too early in the morning | ||||
| Model 1 | 1.16 (1.00–1.33) | 0.75 (0.69–0.81) | 1.01 (0.86–1.19) | <.0001 |
| Model 2 | 1.13 (0.97–1.30) | 0.76 (0.70–0.83) | 1.08 (0.91–1.28) | <.0001 |
| Nonrestorative sleep | ||||
| Model 1 | 0.93 (0.80–1.07) | 0.46 (0.41–0.52) | 0.99 (0.77–1.27) | <.0001 |
| Model 2 | 0.91 (0.78–1.05) | 0.47 (0.41–0.53) | 1.06 (0.81–1.39) | <.0001 |
| . | Pre-retirement perioda . | Retirement transitionb . | Post-retirement periodc . | . |
|---|---|---|---|---|
| RR (95% CI) . | RR (95% CI) . | RR (95% CI) . | Interaction with time p . | |
| Any sleep difficulty | ||||
| Model 1 | 1.12 (1.03–1.22) | 0.88 (0.85–0.92) | 1.06 (0.98–1.15) | <.0001 |
| Model 2 | 1.12 (1.03–1.23) | 0.89 (0.85–0.93) | 1.08 (0.99–1.18) | <.0001 |
| Difficulties falling asleep | ||||
| Model 1 | 1.23 (0.96–1.56) | 0.91 (0.80–1.03) | 1.04 (0.84–1.29) | .063 |
| Model 2 | 1.29 (1.00–1.65) | 0.90 (0.79–1.04) | 1.05 (0.83–1.34) | .050 |
| Difficulties maintaining sleep during the night | ||||
| Model 1 | 1.23 (1.11–1.36) | 0.97 (0.92–1.02) | 1.08 (0.99–1.18) | <.0001 |
| Model 2 | 1.23 (1.11–1.36) | 0.98 (0.93–1.03) | 1.12 (1.02–1.23) | <.001 |
| Waking up too early in the morning | ||||
| Model 1 | 1.16 (1.00–1.33) | 0.75 (0.69–0.81) | 1.01 (0.86–1.19) | <.0001 |
| Model 2 | 1.13 (0.97–1.30) | 0.76 (0.70–0.83) | 1.08 (0.91–1.28) | <.0001 |
| Nonrestorative sleep | ||||
| Model 1 | 0.93 (0.80–1.07) | 0.46 (0.41–0.52) | 0.99 (0.77–1.27) | <.0001 |
| Model 2 | 0.91 (0.78–1.05) | 0.47 (0.41–0.53) | 1.06 (0.81–1.39) | <.0001 |
Risk ratios (RR) and their 95% confidence intervals (CI) in athe study wave–2 compared with the study wave–3, bthe study wave+1 compared with the study wave–1, and cthe study wave+3 compared with the study wave+2 are derived from log-binominal regression analyses with generalized estimating equations.
Model 1 is adjusted for gender, retirement age, and occupational status.
Model 2 is additionally adjusted for marital status, shift or night work, job strain, physical activity, alcohol use, smoking, BMI, self-rated health, psychological distress, arthritis, cardiometabolic diseases, asthma, cancer, and sleep duration before retirement.
BMI = body mass index.
Changes in Any Sleep Difficulty and the Specific Types of Sleep Difficulties During the Pre-retirement Period, the Retirement Transition, and the Post-retirement Period.
| . | Pre-retirement perioda . | Retirement transitionb . | Post-retirement periodc . | . |
|---|---|---|---|---|
| RR (95% CI) . | RR (95% CI) . | RR (95% CI) . | Interaction with time p . | |
| Any sleep difficulty | ||||
| Model 1 | 1.12 (1.03–1.22) | 0.88 (0.85–0.92) | 1.06 (0.98–1.15) | <.0001 |
| Model 2 | 1.12 (1.03–1.23) | 0.89 (0.85–0.93) | 1.08 (0.99–1.18) | <.0001 |
| Difficulties falling asleep | ||||
| Model 1 | 1.23 (0.96–1.56) | 0.91 (0.80–1.03) | 1.04 (0.84–1.29) | .063 |
| Model 2 | 1.29 (1.00–1.65) | 0.90 (0.79–1.04) | 1.05 (0.83–1.34) | .050 |
| Difficulties maintaining sleep during the night | ||||
| Model 1 | 1.23 (1.11–1.36) | 0.97 (0.92–1.02) | 1.08 (0.99–1.18) | <.0001 |
| Model 2 | 1.23 (1.11–1.36) | 0.98 (0.93–1.03) | 1.12 (1.02–1.23) | <.001 |
| Waking up too early in the morning | ||||
| Model 1 | 1.16 (1.00–1.33) | 0.75 (0.69–0.81) | 1.01 (0.86–1.19) | <.0001 |
| Model 2 | 1.13 (0.97–1.30) | 0.76 (0.70–0.83) | 1.08 (0.91–1.28) | <.0001 |
| Nonrestorative sleep | ||||
| Model 1 | 0.93 (0.80–1.07) | 0.46 (0.41–0.52) | 0.99 (0.77–1.27) | <.0001 |
| Model 2 | 0.91 (0.78–1.05) | 0.47 (0.41–0.53) | 1.06 (0.81–1.39) | <.0001 |
| . | Pre-retirement perioda . | Retirement transitionb . | Post-retirement periodc . | . |
|---|---|---|---|---|
| RR (95% CI) . | RR (95% CI) . | RR (95% CI) . | Interaction with time p . | |
| Any sleep difficulty | ||||
| Model 1 | 1.12 (1.03–1.22) | 0.88 (0.85–0.92) | 1.06 (0.98–1.15) | <.0001 |
| Model 2 | 1.12 (1.03–1.23) | 0.89 (0.85–0.93) | 1.08 (0.99–1.18) | <.0001 |
| Difficulties falling asleep | ||||
| Model 1 | 1.23 (0.96–1.56) | 0.91 (0.80–1.03) | 1.04 (0.84–1.29) | .063 |
| Model 2 | 1.29 (1.00–1.65) | 0.90 (0.79–1.04) | 1.05 (0.83–1.34) | .050 |
| Difficulties maintaining sleep during the night | ||||
| Model 1 | 1.23 (1.11–1.36) | 0.97 (0.92–1.02) | 1.08 (0.99–1.18) | <.0001 |
| Model 2 | 1.23 (1.11–1.36) | 0.98 (0.93–1.03) | 1.12 (1.02–1.23) | <.001 |
| Waking up too early in the morning | ||||
| Model 1 | 1.16 (1.00–1.33) | 0.75 (0.69–0.81) | 1.01 (0.86–1.19) | <.0001 |
| Model 2 | 1.13 (0.97–1.30) | 0.76 (0.70–0.83) | 1.08 (0.91–1.28) | <.0001 |
| Nonrestorative sleep | ||||
| Model 1 | 0.93 (0.80–1.07) | 0.46 (0.41–0.52) | 0.99 (0.77–1.27) | <.0001 |
| Model 2 | 0.91 (0.78–1.05) | 0.47 (0.41–0.53) | 1.06 (0.81–1.39) | <.0001 |
Risk ratios (RR) and their 95% confidence intervals (CI) in athe study wave–2 compared with the study wave–3, bthe study wave+1 compared with the study wave–1, and cthe study wave+3 compared with the study wave+2 are derived from log-binominal regression analyses with generalized estimating equations.
Model 1 is adjusted for gender, retirement age, and occupational status.
Model 2 is additionally adjusted for marital status, shift or night work, job strain, physical activity, alcohol use, smoking, BMI, self-rated health, psychological distress, arthritis, cardiometabolic diseases, asthma, cancer, and sleep duration before retirement.
BMI = body mass index.
The specific sleep difficulties in relation to retirement: (A) difficulties falling asleep; (B) difficulties maintaining sleep; (C) waking up too early in the morning; and (D) nonrestorative sleep. Prevalence of sleep difficulties in each study wave and 95% confidence interval derived from log-binominal regression analyses with generalized estimating equations. Time between each study wave is approximately 4 years. Adjusted for gender, retirement age, and occupational status.
To examine the robustness of our findings, the analyses of any sleep difficulty were repeated with a lower cutoff point to define the sleep difficulties (i.e., sleep difficulties if frequency is higher than two nights per week). A highly similar trend in any sleep difficulty was observed in these analyses compared with the actual analyses. The only difference between the results from the sensitivity analyses and the actual analyses was that the prevalence estimates were higher in all the study waves when level of the occurrence for any sleep difficulty was lower. This is, however, unsurprising, as the prevalence estimates of the sensitivity analyses include both those participants in the actual analyses and those with milder sleep difficulties. The detailed results are shown in Supplementary Figure S1.
Finally, we examined the distributions of the frequencies of the four specific sleep difficulties in the study waves immediately before retirement (wave–1) and after retirement (wave+1). Comparison of the responses before and after retirement shows a considerable shift from higher to lower frequencies in both waking up too early in the morning and nonrestorative sleep. When it comes to difficulties falling asleep and difficulties maintaining sleep, in which no changes were observed during the retirement transition in the main analyses, there were only minor changes in the proportions throughout the frequency scales. The results for this analysis are shown in Supplementary Figure S2.
Pre-retirement Factors and Change in Sleep Difficulties
Table 3 shows the prevalence of any sleep difficulty in the study wave immediately before retirement (wave–1) and the changes in any sleep difficulty during the retirement transition by characteristics of the study population in wave–1. We found an interaction between retirement and job strain, self-rated health, psychological distress, and sleep duration in changes of any sleep difficulty. In all other groups categorized by characteristics before retirement, sleep difficulties changed similarly during the retirement transition with no differences in the extent of the changes across categories. A decrease in any sleep difficulty was observed during the retirement transition among those with job strain, suboptimal self-rated health, psychological distress, or short sleep duration (≤6.5 hours/24 hours) before retirement, whereas no changes in any sleep difficulty were observed among those in their reference groups. The most pronounced decrease in sleep difficulties was observed among those with psychological distress before retirement, among who the RR for any sleep difficulty in the study wave after retirement (wave+1), compared with the study wave before retirement (wave–1), was 0.69 (95% CI 0.62–0.78), whereas among those without psychological distress the corresponding RR was 1.01 (95% CI 0.93–1.10).
Prevalence of and Changes in Any Sleep Difficulty During the Transition to Retirement by Characteristics of the Study Population Before Retirement.
| . | Prevalence of any sleep difficulty before retirement (%)a . | Changeb . | Interaction with time . | ||
|---|---|---|---|---|---|
| Characteristics | RR | 95% CI | p | ||
| Gender | .615 | ||||
| Men | 27 | 0.91 | 0.81 | 1.01 | |
| Women | 32 | 0.88 | 0.84 | 0.92 | |
| Retirement age | .150 | ||||
| < 60 | 34 | 0.80 | 0.71 | 0.91 | |
| 60–64 | 32 | 0.89 | 0.84 | 0.93 | |
| >64 | 28 | 0.95 | 0.84 | 1.07 | |
| Marital status | .133 | ||||
| Married | 30 | 0.91 | 0.86 | 0.95 | |
| Not married | 34 | 0.84 | 0.77 | 0.91 | |
| Occupational status | .286 | ||||
| Upper grade nonmanual | 29 | 0.87 | 0.81 | 0.94 | |
| Lower grade nonmanual | 30 | 0.94 | 0.86 | 1.03 | |
| Manual | 34 | 0.86 | 0.80 | 0.92 | |
| Shift/night work | .985 | ||||
| No | 31 | 0.89 | 0.82 | 0.96 | |
| Yes | 32 | 0.88 | 0.78 | 1.00 | |
| Job strain | .037 | ||||
| No | 29 | 0.93 | 0.86 | 1.01 | |
| Yes | 38 | 0.79 | 0.70 | 0.90 | |
| Physical activity | .986 | ||||
| Inactive | 35 | 0.90 | 0.78 | 1.04 | |
| Low | 32 | 0.88 | 0.77 | 1.02 | |
| Moderate | 30 | 0.88 | 0.77 | 1.00 | |
| High | 29 | 0.87 | 0.76 | 0.99 | |
| Alcohol use | .281 | ||||
| None | 31 | 0.89 | 0.75 | 1.06 | |
| Moderate | 31 | 0.90 | 0.83 | 0.97 | |
| Heavy | 39 | 0.74 | 0.59 | 0.93 | |
| Smoking | .694 | ||||
| Never | 31 | 0.86 | 0.80 | 0.94 | |
| Former | 36 | 0.90 | 0.77 | 1.06 | |
| Current | 27 | 0.96 | 0.75 | 1.22 | |
| Body Mass Index | .947 | ||||
| Underweight (<18.5 kg/m2) | 36 | 1.11 | 0.45 | 2.73 | |
| Normal weight (18.5–24.9 kg/m2) | 29 | 0.90 | 0.81 | 1.01 | |
| Overweight (25–29.9 kg/m2) | 31 | 0.88 | 0.79 | 0.98 | |
| Obese (≥30 kg/m2) | 37 | 0.91 | 0.78 | 1.06 | |
| Self-rated health | .002 | ||||
| Good | 23 | 0.99 | 0.90 | 1.09 | |
| Suboptimal | 46 | 0.80 | 0.73 | 0.88 | |
| Psychological distress | <.0001 | ||||
| No | 25 | 1.01 | 0.93 | 1.10 | |
| Yes | 52 | 0.69 | 0.62 | 0.78 | |
| Arthritis | .642 | ||||
| No | 26 | 0.90 | 0.82 | 0.99 | |
| Yes | 39 | 0.87 | 0.79 | 0.96 | |
| Cardiometabolic diseases | .322 | ||||
| No | 31 | 0.88 | 0.82 | 0.94 | |
| Yes | 33 | 1.02 | 0.76 | 1.38 | |
| Asthma | .945 | ||||
| No | 31 | 0.88 | 0.83 | 0.95 | |
| Yes | 41 | 0.88 | 0.65 | 1.17 | |
| Cancer | .794 | ||||
| No | 31 | 0.89 | 0.83 | 0.95 | |
| Yes | 33 | 0.85 | 0.60 | 1.19 | |
| Sleep duration before retirement | .010 | ||||
| Short (≤6.5 hours/24 h) | 45 | 0.78 | 0.70 | 0.87 | |
| Mid-range (7–8.5 hours/24 h) | 25 | 0.97 | 0.88 | 1.06 | |
| Long (≥9 hours/24 h) | 34 | 0.87 | 0.58 | 1.29 | |
| . | Prevalence of any sleep difficulty before retirement (%)a . | Changeb . | Interaction with time . | ||
|---|---|---|---|---|---|
| Characteristics | RR | 95% CI | p | ||
| Gender | .615 | ||||
| Men | 27 | 0.91 | 0.81 | 1.01 | |
| Women | 32 | 0.88 | 0.84 | 0.92 | |
| Retirement age | .150 | ||||
| < 60 | 34 | 0.80 | 0.71 | 0.91 | |
| 60–64 | 32 | 0.89 | 0.84 | 0.93 | |
| >64 | 28 | 0.95 | 0.84 | 1.07 | |
| Marital status | .133 | ||||
| Married | 30 | 0.91 | 0.86 | 0.95 | |
| Not married | 34 | 0.84 | 0.77 | 0.91 | |
| Occupational status | .286 | ||||
| Upper grade nonmanual | 29 | 0.87 | 0.81 | 0.94 | |
| Lower grade nonmanual | 30 | 0.94 | 0.86 | 1.03 | |
| Manual | 34 | 0.86 | 0.80 | 0.92 | |
| Shift/night work | .985 | ||||
| No | 31 | 0.89 | 0.82 | 0.96 | |
| Yes | 32 | 0.88 | 0.78 | 1.00 | |
| Job strain | .037 | ||||
| No | 29 | 0.93 | 0.86 | 1.01 | |
| Yes | 38 | 0.79 | 0.70 | 0.90 | |
| Physical activity | .986 | ||||
| Inactive | 35 | 0.90 | 0.78 | 1.04 | |
| Low | 32 | 0.88 | 0.77 | 1.02 | |
| Moderate | 30 | 0.88 | 0.77 | 1.00 | |
| High | 29 | 0.87 | 0.76 | 0.99 | |
| Alcohol use | .281 | ||||
| None | 31 | 0.89 | 0.75 | 1.06 | |
| Moderate | 31 | 0.90 | 0.83 | 0.97 | |
| Heavy | 39 | 0.74 | 0.59 | 0.93 | |
| Smoking | .694 | ||||
| Never | 31 | 0.86 | 0.80 | 0.94 | |
| Former | 36 | 0.90 | 0.77 | 1.06 | |
| Current | 27 | 0.96 | 0.75 | 1.22 | |
| Body Mass Index | .947 | ||||
| Underweight (<18.5 kg/m2) | 36 | 1.11 | 0.45 | 2.73 | |
| Normal weight (18.5–24.9 kg/m2) | 29 | 0.90 | 0.81 | 1.01 | |
| Overweight (25–29.9 kg/m2) | 31 | 0.88 | 0.79 | 0.98 | |
| Obese (≥30 kg/m2) | 37 | 0.91 | 0.78 | 1.06 | |
| Self-rated health | .002 | ||||
| Good | 23 | 0.99 | 0.90 | 1.09 | |
| Suboptimal | 46 | 0.80 | 0.73 | 0.88 | |
| Psychological distress | <.0001 | ||||
| No | 25 | 1.01 | 0.93 | 1.10 | |
| Yes | 52 | 0.69 | 0.62 | 0.78 | |
| Arthritis | .642 | ||||
| No | 26 | 0.90 | 0.82 | 0.99 | |
| Yes | 39 | 0.87 | 0.79 | 0.96 | |
| Cardiometabolic diseases | .322 | ||||
| No | 31 | 0.88 | 0.82 | 0.94 | |
| Yes | 33 | 1.02 | 0.76 | 1.38 | |
| Asthma | .945 | ||||
| No | 31 | 0.88 | 0.83 | 0.95 | |
| Yes | 41 | 0.88 | 0.65 | 1.17 | |
| Cancer | .794 | ||||
| No | 31 | 0.89 | 0.83 | 0.95 | |
| Yes | 33 | 0.85 | 0.60 | 1.19 | |
| Sleep duration before retirement | .010 | ||||
| Short (≤6.5 hours/24 h) | 45 | 0.78 | 0.70 | 0.87 | |
| Mid-range (7–8.5 hours/24 h) | 25 | 0.97 | 0.88 | 1.06 | |
| Long (≥9 hours/24 h) | 34 | 0.87 | 0.58 | 1.29 | |
aPrevalence of any sleep difficulty in the study wave immediately prior to retirement (wave–1).
bRisk ratios (RR) for sleep difficulties and their 95% confidence interval (CI) in the study wave immediately after retirement (wave+1) compared with the study wave immediately prior to retirement (wave–1) (i.e., the retirement transition) are derived from log-binominal regression analyses with generalized estimating equations.
Analyses are adjusted for gender, retirement age, and occupational status.
Prevalence of and Changes in Any Sleep Difficulty During the Transition to Retirement by Characteristics of the Study Population Before Retirement.
| . | Prevalence of any sleep difficulty before retirement (%)a . | Changeb . | Interaction with time . | ||
|---|---|---|---|---|---|
| Characteristics | RR | 95% CI | p | ||
| Gender | .615 | ||||
| Men | 27 | 0.91 | 0.81 | 1.01 | |
| Women | 32 | 0.88 | 0.84 | 0.92 | |
| Retirement age | .150 | ||||
| < 60 | 34 | 0.80 | 0.71 | 0.91 | |
| 60–64 | 32 | 0.89 | 0.84 | 0.93 | |
| >64 | 28 | 0.95 | 0.84 | 1.07 | |
| Marital status | .133 | ||||
| Married | 30 | 0.91 | 0.86 | 0.95 | |
| Not married | 34 | 0.84 | 0.77 | 0.91 | |
| Occupational status | .286 | ||||
| Upper grade nonmanual | 29 | 0.87 | 0.81 | 0.94 | |
| Lower grade nonmanual | 30 | 0.94 | 0.86 | 1.03 | |
| Manual | 34 | 0.86 | 0.80 | 0.92 | |
| Shift/night work | .985 | ||||
| No | 31 | 0.89 | 0.82 | 0.96 | |
| Yes | 32 | 0.88 | 0.78 | 1.00 | |
| Job strain | .037 | ||||
| No | 29 | 0.93 | 0.86 | 1.01 | |
| Yes | 38 | 0.79 | 0.70 | 0.90 | |
| Physical activity | .986 | ||||
| Inactive | 35 | 0.90 | 0.78 | 1.04 | |
| Low | 32 | 0.88 | 0.77 | 1.02 | |
| Moderate | 30 | 0.88 | 0.77 | 1.00 | |
| High | 29 | 0.87 | 0.76 | 0.99 | |
| Alcohol use | .281 | ||||
| None | 31 | 0.89 | 0.75 | 1.06 | |
| Moderate | 31 | 0.90 | 0.83 | 0.97 | |
| Heavy | 39 | 0.74 | 0.59 | 0.93 | |
| Smoking | .694 | ||||
| Never | 31 | 0.86 | 0.80 | 0.94 | |
| Former | 36 | 0.90 | 0.77 | 1.06 | |
| Current | 27 | 0.96 | 0.75 | 1.22 | |
| Body Mass Index | .947 | ||||
| Underweight (<18.5 kg/m2) | 36 | 1.11 | 0.45 | 2.73 | |
| Normal weight (18.5–24.9 kg/m2) | 29 | 0.90 | 0.81 | 1.01 | |
| Overweight (25–29.9 kg/m2) | 31 | 0.88 | 0.79 | 0.98 | |
| Obese (≥30 kg/m2) | 37 | 0.91 | 0.78 | 1.06 | |
| Self-rated health | .002 | ||||
| Good | 23 | 0.99 | 0.90 | 1.09 | |
| Suboptimal | 46 | 0.80 | 0.73 | 0.88 | |
| Psychological distress | <.0001 | ||||
| No | 25 | 1.01 | 0.93 | 1.10 | |
| Yes | 52 | 0.69 | 0.62 | 0.78 | |
| Arthritis | .642 | ||||
| No | 26 | 0.90 | 0.82 | 0.99 | |
| Yes | 39 | 0.87 | 0.79 | 0.96 | |
| Cardiometabolic diseases | .322 | ||||
| No | 31 | 0.88 | 0.82 | 0.94 | |
| Yes | 33 | 1.02 | 0.76 | 1.38 | |
| Asthma | .945 | ||||
| No | 31 | 0.88 | 0.83 | 0.95 | |
| Yes | 41 | 0.88 | 0.65 | 1.17 | |
| Cancer | .794 | ||||
| No | 31 | 0.89 | 0.83 | 0.95 | |
| Yes | 33 | 0.85 | 0.60 | 1.19 | |
| Sleep duration before retirement | .010 | ||||
| Short (≤6.5 hours/24 h) | 45 | 0.78 | 0.70 | 0.87 | |
| Mid-range (7–8.5 hours/24 h) | 25 | 0.97 | 0.88 | 1.06 | |
| Long (≥9 hours/24 h) | 34 | 0.87 | 0.58 | 1.29 | |
| . | Prevalence of any sleep difficulty before retirement (%)a . | Changeb . | Interaction with time . | ||
|---|---|---|---|---|---|
| Characteristics | RR | 95% CI | p | ||
| Gender | .615 | ||||
| Men | 27 | 0.91 | 0.81 | 1.01 | |
| Women | 32 | 0.88 | 0.84 | 0.92 | |
| Retirement age | .150 | ||||
| < 60 | 34 | 0.80 | 0.71 | 0.91 | |
| 60–64 | 32 | 0.89 | 0.84 | 0.93 | |
| >64 | 28 | 0.95 | 0.84 | 1.07 | |
| Marital status | .133 | ||||
| Married | 30 | 0.91 | 0.86 | 0.95 | |
| Not married | 34 | 0.84 | 0.77 | 0.91 | |
| Occupational status | .286 | ||||
| Upper grade nonmanual | 29 | 0.87 | 0.81 | 0.94 | |
| Lower grade nonmanual | 30 | 0.94 | 0.86 | 1.03 | |
| Manual | 34 | 0.86 | 0.80 | 0.92 | |
| Shift/night work | .985 | ||||
| No | 31 | 0.89 | 0.82 | 0.96 | |
| Yes | 32 | 0.88 | 0.78 | 1.00 | |
| Job strain | .037 | ||||
| No | 29 | 0.93 | 0.86 | 1.01 | |
| Yes | 38 | 0.79 | 0.70 | 0.90 | |
| Physical activity | .986 | ||||
| Inactive | 35 | 0.90 | 0.78 | 1.04 | |
| Low | 32 | 0.88 | 0.77 | 1.02 | |
| Moderate | 30 | 0.88 | 0.77 | 1.00 | |
| High | 29 | 0.87 | 0.76 | 0.99 | |
| Alcohol use | .281 | ||||
| None | 31 | 0.89 | 0.75 | 1.06 | |
| Moderate | 31 | 0.90 | 0.83 | 0.97 | |
| Heavy | 39 | 0.74 | 0.59 | 0.93 | |
| Smoking | .694 | ||||
| Never | 31 | 0.86 | 0.80 | 0.94 | |
| Former | 36 | 0.90 | 0.77 | 1.06 | |
| Current | 27 | 0.96 | 0.75 | 1.22 | |
| Body Mass Index | .947 | ||||
| Underweight (<18.5 kg/m2) | 36 | 1.11 | 0.45 | 2.73 | |
| Normal weight (18.5–24.9 kg/m2) | 29 | 0.90 | 0.81 | 1.01 | |
| Overweight (25–29.9 kg/m2) | 31 | 0.88 | 0.79 | 0.98 | |
| Obese (≥30 kg/m2) | 37 | 0.91 | 0.78 | 1.06 | |
| Self-rated health | .002 | ||||
| Good | 23 | 0.99 | 0.90 | 1.09 | |
| Suboptimal | 46 | 0.80 | 0.73 | 0.88 | |
| Psychological distress | <.0001 | ||||
| No | 25 | 1.01 | 0.93 | 1.10 | |
| Yes | 52 | 0.69 | 0.62 | 0.78 | |
| Arthritis | .642 | ||||
| No | 26 | 0.90 | 0.82 | 0.99 | |
| Yes | 39 | 0.87 | 0.79 | 0.96 | |
| Cardiometabolic diseases | .322 | ||||
| No | 31 | 0.88 | 0.82 | 0.94 | |
| Yes | 33 | 1.02 | 0.76 | 1.38 | |
| Asthma | .945 | ||||
| No | 31 | 0.88 | 0.83 | 0.95 | |
| Yes | 41 | 0.88 | 0.65 | 1.17 | |
| Cancer | .794 | ||||
| No | 31 | 0.89 | 0.83 | 0.95 | |
| Yes | 33 | 0.85 | 0.60 | 1.19 | |
| Sleep duration before retirement | .010 | ||||
| Short (≤6.5 hours/24 h) | 45 | 0.78 | 0.70 | 0.87 | |
| Mid-range (7–8.5 hours/24 h) | 25 | 0.97 | 0.88 | 1.06 | |
| Long (≥9 hours/24 h) | 34 | 0.87 | 0.58 | 1.29 | |
aPrevalence of any sleep difficulty in the study wave immediately prior to retirement (wave–1).
bRisk ratios (RR) for sleep difficulties and their 95% confidence interval (CI) in the study wave immediately after retirement (wave+1) compared with the study wave immediately prior to retirement (wave–1) (i.e., the retirement transition) are derived from log-binominal regression analyses with generalized estimating equations.
Analyses are adjusted for gender, retirement age, and occupational status.
To examine the interactions more closely, we examined whether the four specific sleep difficulties also changed differently during the retirement transition among the groups that were found to have different changes in any sleep difficulty. As seen in Table 4, difficulties falling asleep and difficulties maintaining sleep decreased statistically significantly more (p < .02) among those with suboptimal self-rated health, psychological distress, and short sleep duration before retirement. In waking up too early in the morning and nonrestorative sleep, we observed a decrease among all groups except those with mid-range or long sleep duration. In addition, the greatest decreases in waking up too early in the morning and nonrestorative sleep were observed among those with psychological distress and these decreases were significantly greater compared with those without psychological distress.
Changes in the Four Specific Sleep Difficulties During the Transition to Retirement by Those Pre-retirement Factors That Predicted Changes in Any Sleep Difficulty During the Retirement Transition (Seen in Table 3).
| . | Difficulties falling asleep . | Difficulties maintaining sleep . | Waking up too early in the morning . | Nonrestorative sleep . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Change . | Interaction with time . | Change . | Interaction with time . | Change . | Interaction with time . | Change . | Interaction with time . | |||||||||
| Characteristics . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | ||||
| Job strain | .391 | .066 | .904 | .415 | ||||||||||||
| No | 0.95 | 0.78 | 1.16 | 1.02 | 0.93 | 1.11 | 0.75 | 0.66 | 0.86 | 0.49 | 0.41 | 0.58 | ||||
| Yes | 0.83 | 0.63 | 1.08 | 0.87 | 0.76 | 1.00 | 0.74 | 0.61 | 0.90 | 0.43 | 0.34 | 0.54 | ||||
| Self-rated health | .020 | .005 | .29 | .23 | ||||||||||||
| Good | 1.15 | 0.88 | 1.49 | 1.08 | 0.97 | 1.20 | 0.79 | 0.68 | 0.93 | 0.52 | 0.41 | 0.66 | ||||
| Suboptimal | 0.78 | 0.64 | 0.95 | 0.88 | 0.79 | 0.97 | 0.71 | 0.61 | 0.82 | 0.44 | 0.37 | 0.52 | ||||
| Psychological distress | .003 | <.0001 | .002 | .005 | ||||||||||||
| No | 1.13 | 0.91 | 1.39 | 1.09 | 1.00 | 1.19 | 0.86 | 0.75 | 0.99 | 0.58 | 0.47 | 0.70 | ||||
| Yes | 0.70 | 0.55 | 0.88 | 0.77 | 0.68 | 0.88 | 0.61 | 0.51 | 0.72 | 0.39 | 0.32 | 0.47 | ||||
| Sleep duration before retirement | .001 | .0183 | .015 | .92 | ||||||||||||
| Short (≤6.5 h/24 h) | 0.70 | 0.56 | 0.86 | 0.86 | 0.76 | 0.96 | 0.65 | 0.56 | 0.75 | 0.46 | 0.38 | 0.55 | ||||
| Mid-range (7–8.5 h/24 h) | 1.30 | 1.01 | 1.67 | 1.06 | 0.96 | 1.17 | 0.88 | 0.75 | 1.03 | 0.47 | 0.38 | 0.57 | ||||
| Long (≥9 h/24 h) | 0.97 | 0.40 | 2.32 | 0.94 | 0.60 | 1.47 | 1.06 | 0.48 | 2.32 | 0.53 | 0.26 | 1.06 | ||||
| . | Difficulties falling asleep . | Difficulties maintaining sleep . | Waking up too early in the morning . | Nonrestorative sleep . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Change . | Interaction with time . | Change . | Interaction with time . | Change . | Interaction with time . | Change . | Interaction with time . | |||||||||
| Characteristics . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | ||||
| Job strain | .391 | .066 | .904 | .415 | ||||||||||||
| No | 0.95 | 0.78 | 1.16 | 1.02 | 0.93 | 1.11 | 0.75 | 0.66 | 0.86 | 0.49 | 0.41 | 0.58 | ||||
| Yes | 0.83 | 0.63 | 1.08 | 0.87 | 0.76 | 1.00 | 0.74 | 0.61 | 0.90 | 0.43 | 0.34 | 0.54 | ||||
| Self-rated health | .020 | .005 | .29 | .23 | ||||||||||||
| Good | 1.15 | 0.88 | 1.49 | 1.08 | 0.97 | 1.20 | 0.79 | 0.68 | 0.93 | 0.52 | 0.41 | 0.66 | ||||
| Suboptimal | 0.78 | 0.64 | 0.95 | 0.88 | 0.79 | 0.97 | 0.71 | 0.61 | 0.82 | 0.44 | 0.37 | 0.52 | ||||
| Psychological distress | .003 | <.0001 | .002 | .005 | ||||||||||||
| No | 1.13 | 0.91 | 1.39 | 1.09 | 1.00 | 1.19 | 0.86 | 0.75 | 0.99 | 0.58 | 0.47 | 0.70 | ||||
| Yes | 0.70 | 0.55 | 0.88 | 0.77 | 0.68 | 0.88 | 0.61 | 0.51 | 0.72 | 0.39 | 0.32 | 0.47 | ||||
| Sleep duration before retirement | .001 | .0183 | .015 | .92 | ||||||||||||
| Short (≤6.5 h/24 h) | 0.70 | 0.56 | 0.86 | 0.86 | 0.76 | 0.96 | 0.65 | 0.56 | 0.75 | 0.46 | 0.38 | 0.55 | ||||
| Mid-range (7–8.5 h/24 h) | 1.30 | 1.01 | 1.67 | 1.06 | 0.96 | 1.17 | 0.88 | 0.75 | 1.03 | 0.47 | 0.38 | 0.57 | ||||
| Long (≥9 h/24 h) | 0.97 | 0.40 | 2.32 | 0.94 | 0.60 | 1.47 | 1.06 | 0.48 | 2.32 | 0.53 | 0.26 | 1.06 | ||||
Risk ratios (RR) and their 95% confidence intervals (CI) in the study wave immediately after retirement (wave+1) compared with the study wave immediately prior to retirement (wave–1) (i.e., the retirement transition) are derived from log-binominal regression analyses with generalized estimating equations and presented for each specific sleep difficulty.
Analyses are adjusted for gender, retirement age, and occupational status.
Changes in the Four Specific Sleep Difficulties During the Transition to Retirement by Those Pre-retirement Factors That Predicted Changes in Any Sleep Difficulty During the Retirement Transition (Seen in Table 3).
| . | Difficulties falling asleep . | Difficulties maintaining sleep . | Waking up too early in the morning . | Nonrestorative sleep . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Change . | Interaction with time . | Change . | Interaction with time . | Change . | Interaction with time . | Change . | Interaction with time . | |||||||||
| Characteristics . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | ||||
| Job strain | .391 | .066 | .904 | .415 | ||||||||||||
| No | 0.95 | 0.78 | 1.16 | 1.02 | 0.93 | 1.11 | 0.75 | 0.66 | 0.86 | 0.49 | 0.41 | 0.58 | ||||
| Yes | 0.83 | 0.63 | 1.08 | 0.87 | 0.76 | 1.00 | 0.74 | 0.61 | 0.90 | 0.43 | 0.34 | 0.54 | ||||
| Self-rated health | .020 | .005 | .29 | .23 | ||||||||||||
| Good | 1.15 | 0.88 | 1.49 | 1.08 | 0.97 | 1.20 | 0.79 | 0.68 | 0.93 | 0.52 | 0.41 | 0.66 | ||||
| Suboptimal | 0.78 | 0.64 | 0.95 | 0.88 | 0.79 | 0.97 | 0.71 | 0.61 | 0.82 | 0.44 | 0.37 | 0.52 | ||||
| Psychological distress | .003 | <.0001 | .002 | .005 | ||||||||||||
| No | 1.13 | 0.91 | 1.39 | 1.09 | 1.00 | 1.19 | 0.86 | 0.75 | 0.99 | 0.58 | 0.47 | 0.70 | ||||
| Yes | 0.70 | 0.55 | 0.88 | 0.77 | 0.68 | 0.88 | 0.61 | 0.51 | 0.72 | 0.39 | 0.32 | 0.47 | ||||
| Sleep duration before retirement | .001 | .0183 | .015 | .92 | ||||||||||||
| Short (≤6.5 h/24 h) | 0.70 | 0.56 | 0.86 | 0.86 | 0.76 | 0.96 | 0.65 | 0.56 | 0.75 | 0.46 | 0.38 | 0.55 | ||||
| Mid-range (7–8.5 h/24 h) | 1.30 | 1.01 | 1.67 | 1.06 | 0.96 | 1.17 | 0.88 | 0.75 | 1.03 | 0.47 | 0.38 | 0.57 | ||||
| Long (≥9 h/24 h) | 0.97 | 0.40 | 2.32 | 0.94 | 0.60 | 1.47 | 1.06 | 0.48 | 2.32 | 0.53 | 0.26 | 1.06 | ||||
| . | Difficulties falling asleep . | Difficulties maintaining sleep . | Waking up too early in the morning . | Nonrestorative sleep . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Change . | Interaction with time . | Change . | Interaction with time . | Change . | Interaction with time . | Change . | Interaction with time . | |||||||||
| Characteristics . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | RR . | 95% CI . | p . | ||||
| Job strain | .391 | .066 | .904 | .415 | ||||||||||||
| No | 0.95 | 0.78 | 1.16 | 1.02 | 0.93 | 1.11 | 0.75 | 0.66 | 0.86 | 0.49 | 0.41 | 0.58 | ||||
| Yes | 0.83 | 0.63 | 1.08 | 0.87 | 0.76 | 1.00 | 0.74 | 0.61 | 0.90 | 0.43 | 0.34 | 0.54 | ||||
| Self-rated health | .020 | .005 | .29 | .23 | ||||||||||||
| Good | 1.15 | 0.88 | 1.49 | 1.08 | 0.97 | 1.20 | 0.79 | 0.68 | 0.93 | 0.52 | 0.41 | 0.66 | ||||
| Suboptimal | 0.78 | 0.64 | 0.95 | 0.88 | 0.79 | 0.97 | 0.71 | 0.61 | 0.82 | 0.44 | 0.37 | 0.52 | ||||
| Psychological distress | .003 | <.0001 | .002 | .005 | ||||||||||||
| No | 1.13 | 0.91 | 1.39 | 1.09 | 1.00 | 1.19 | 0.86 | 0.75 | 0.99 | 0.58 | 0.47 | 0.70 | ||||
| Yes | 0.70 | 0.55 | 0.88 | 0.77 | 0.68 | 0.88 | 0.61 | 0.51 | 0.72 | 0.39 | 0.32 | 0.47 | ||||
| Sleep duration before retirement | .001 | .0183 | .015 | .92 | ||||||||||||
| Short (≤6.5 h/24 h) | 0.70 | 0.56 | 0.86 | 0.86 | 0.76 | 0.96 | 0.65 | 0.56 | 0.75 | 0.46 | 0.38 | 0.55 | ||||
| Mid-range (7–8.5 h/24 h) | 1.30 | 1.01 | 1.67 | 1.06 | 0.96 | 1.17 | 0.88 | 0.75 | 1.03 | 0.47 | 0.38 | 0.57 | ||||
| Long (≥9 h/24 h) | 0.97 | 0.40 | 2.32 | 0.94 | 0.60 | 1.47 | 1.06 | 0.48 | 2.32 | 0.53 | 0.26 | 1.06 | ||||
Risk ratios (RR) and their 95% confidence intervals (CI) in the study wave immediately after retirement (wave+1) compared with the study wave immediately prior to retirement (wave–1) (i.e., the retirement transition) are derived from log-binominal regression analyses with generalized estimating equations and presented for each specific sleep difficulty.
Analyses are adjusted for gender, retirement age, and occupational status.
DISCUSSION
In a large Finnish cohort of public sector employees, a decrease in the prevalence of sleep difficulties was observed following a transition from full-time work to statutory retirement. Divergent changes were observed around retirement when four specific types of sleep difficulties were examined. During the retirement transition, a decrease was observed in waking up too early in the morning and nonrestorative sleep, whereas difficulties falling asleep and difficulties maintaining sleep did not change during this transition. The decreases observed in sleep difficulties were most pronounced among those with psychological distress, suboptimal self-rated health, short sleep duration, or job strain before retirement. The decrease in any sleep difficulty was mainly driven by decreases of sleep difficulties among those with psychological distress and suboptimal self-rated health before retirement.
Changes in Sleep Difficulties Around Retirement
Our findings of the decrease in the prevalence of sleep difficulties following retirement are in line with the few previous longitudinal studies examining changes in sleep around retirement.13,14 We found the prevalence of sleep difficulties to decrease from 30% to 26% during the 4-year retirement transition. In the GAZEL study, 26% lower odds of sleep disturbance (described as an affirmative answer to a survey question about sleep disturbances during the past 12 months) were observed in the post-retirement phase, compared with the pre-retirement phase, both phases comprising 7 years of annual surveys in a large cohort of French gas and electricity company workers.13 In their study, the prevalence rates for sleep disturbance fell from 24% in the last year before retirement to 18% in the first year after retirement. However, the prevalence rates in our study and the GAZEL study are not strictly comparable due to differences in the measurement of sleep difficulties and the time intervals between the repeated surveys (4 years in our study, compared with 1 year in the GAZEL). The French workers also retired at a fairly young age (55 years, on average) and with a fairly generous retirement scheme (80% of their salary, paid by the company). In addition, the majority of the GAZEL study population was males (80%), whereas our study population was female-dominated (80% women). Despite the differences in study designs and populations between our study and the GAZEL study, highly similar trends in sleep difficulties were observed around retirement.
The novelty of our study was that we were able to track changes in different types of sleep difficulties before, during, and after the transition to retirement. Throughout the follow-up period, the prevalence estimates for difficulties falling asleep were lower than difficulties maintaining sleep and waking up too early in the morning, which is in line with the findings that difficulties maintaining sleep rather than difficulties initiating sleep are more common among insomnia patients and the elderly population.28,29 Previously, changes in specific sleep difficulties have been examined in the French VISAT cohort by comparing two measurement occasions around retirement among those who retired and those who continued working.14 In that study, premature awakenings were found to reduce among those who retired (n = 111), whereas retirement was not associated with changes in other sleep difficulties that were difficulties falling sleep, maintaining sleep, and getting back to sleep. Corresponding with their findings of reduced-premature awakenings, we found a decrease in waking up too early in the morning.
One of the most interesting findings in our study is how very different trends were observed in the specific sleep difficulties around retirement. The prevalence of both waking up too early in the morning and nonrestorative sleep decreased substantially during the retirement transition with no changes during the other study periods. In addition, the proportion of those with either of these two sleep difficulties at least once per week was observed to decrease from the study wave before retirement to the study wave after retirement, whereas the proportion of those reporting never having these sleep difficulties increased remarkably. These decreases could result from the removal of work-related stressors and could also be partly explained by the increased sleep duration following retirement,8 as supported by our finding of a significantly greater benefit in terms of sleep difficulties associating with job strain and short sleep duration before retirement. After retirement, there is particularly a possibility to acquire more restorative sleep, as sleep timings are not dominated by working hours and it is possible to sleep more.
As it comes to difficulties falling asleep and difficulties maintaining sleep, no changes were observed during the retirement transition when the whole study population was considered. In addition, when the distributions of the frequencies of these sleep difficulties in the study waves immediately before and after retirement were compared, the proportions of the responses remained fairly similar throughout the scale. Only change in difficulties falling asleep, or often referred to as sleep onset latency, was the increase observed during the pre-retirement period. Difficulties falling asleep could reflect not only state dependent arousal associated with psychological stress, but also trait vulnerability to hyperarousal.30 For example, cognitive hyperarousal, such as the tendency for pre-sleep rumination or worry, may disturb the attempts to fall asleep.31 It is possible that retirement may not greatly affect the individual’s vulnerability to hyperarousal and thus is not associated with changes in difficulties falling asleep on population level. We also found increases in difficulties maintaining sleep during both the pre-retirement and post-retirement periods, along with a temporary plateauing during the retirement transition. Both of these findings are also in line with the findings on age-related changes in sleep among healthy adults. Previous meta-analysis found only subtle increases in sleep latency with normal aging,32 whereas the increases of difficulties maintaining sleep may reflect the age-related decrease in the ability to sleep, or namely, the increased fragmentation of the sleep phase that is associated with aging.2,3 This fragmentation and the increasing sleep complaints have especially been associated with age-related conditions and comorbidities rather than biological aging per se.2,33,34
Pre-retirement Factors Associated with Changes in Sleep Difficulties
To identify subgroups that especially seem to benefit from retirement, we examined how various pre-retirement sociodemographic and work-related factors as well as health-related behaviors and factors were associated with the changes in sleep difficulties during the transition to retirement. Although a decrease in sleep difficulties was observed during the retirement transition when all groups were considered, when the different groups categorized by pre-retirement factors were examined individually, both decreases and no changes in sleep difficulties were observed. These findings are somewhat discrepant to those of the GAZEL study, where sleep difficulties decreased in all groups following retirement, the only exception being those retired on health grounds (which, in our study, were excluded).13 Another exception to their findings is that we did not find gender-based differences in the changes in sleep difficulties during the retirement transition, whereas in the GAZEL study, women were less likely to benefit from retirement. This discrepancy might be explained by the lower retirement age in their study (53.9 years on average, range 37–62), as post-menopausal symptoms may have contributed to poorer sleep in women in their fifties, whereas in our study the average retirement age among women was 61.8 years (range 55–69).
Even though many pre-retirement factors were associated with sleep difficulties before retirement, only job strain, self-rated health, psychological distress, and sleep duration predicted changes in any sleep difficulty during the transition to retirement. No changes were observed among those with no job strain, good self-rated health, and no psychological distress before retirement when any sleep difficulty was considered. When the associations between these pre-retirement factors and the specific sleep difficulties were examined individually, the greatest decreases were observed among those with psychological distress before retirement, and in fact, all the specific sleep difficulties were observed to decrease among this group. This is interesting, as no changes in difficulties falling asleep or difficulties maintaining sleep were observed when the whole study population was considered, and thus, only the examination of changes among the pre-retirement subgroups revealed these decreases. Although decreases in waking up too early in the morning and nonrestorative sleep were also observed among those without psychological distress, the decreases among those with psychological distress were nevertheless statistically significantly greater. The association between sleep difficulties, and depressive symptoms, such as psychological distress in our study, has been suggested to be bidirectional; insomnia is more common among those with mood disorders, such as depression, but sleep difficulties have also been found to predict symptoms of depression.35,36 Thus, one possible reason for the decrease in sleep difficulties during the transition to retirement could be the improvement in mental health after retirement.13,37,38
Similarly, there was a statistically significantly greater decrease in difficulties falling asleep and difficulties maintaining sleep among those with suboptimal health or short sleep duration before retirement than among their reference groups, as well as in waking up too early in the morning among those with short sleep duration before retirement. These results suggests that the decreases in sleep difficulties could also be due to improvement of well-being in general or the possibility to sleep more. Supporting our findings, improvement of self-rated health and decrease of fatigue and depressive symptoms, correlates of sleep difficulties, have been found to follow retirement.39 In addition, those with short sleep duration (≤6.5 hours/24 hours) have previously been found to have the greatest increases in sleep duration following retirement.10
We observed a greater decrease in any sleep difficulty among those with job strain compared with those without it, but no differences were observed between these groups, when the specific sleep difficulties were examined individually. Job strain, defined in our study as high demands and low control on job, has been associated with disturbed sleep and sleep complaints.6,7,40 Results from a recent study suggest that disappearance of job strain may reduce insomnia symptoms among those with sleeping problems,7 and full-time retirement does indeed remove job strain and other work-related stressors. In fact, the decrease in sleep difficulties has been attributed, at least partly, to the removal of work-related stressors,13 and our findings support this hypothesis.
Strengths and Limitations
A major strength of our study was the large sample with repeated measurements of sleep difficulties. The data were linked to an objectively determined retirement date and allowed us to trace changes in sleep difficulties before, during, and after the transition to statutory retirement, the follow-up period extending up to 8–12 years. In addition to examining changes in sleep difficulties in general, we were able to examine the changes in four specific types of sleep difficulties. The occurrence of the specific sleep difficulties was assessed at the same time of the calendar year in each survey, thus limiting the possible confounding effect of, for example, the amount of light.
The main limitation in our study was the reliance on self-reports of sleep difficulties, which may be influenced, for example, by gender1 and psychosocial characteristics.41 Subjective evaluations of sleep difficulties are nevertheless important, as a person may experience sleep difficulties although objectively their sleep would be considered “normal,”42,43 and the self-reported sleep difficulties may in any case be relevant for their well-being. In fact, it has been suggested that objective measurements of sleep may capture different dimensions of sleep from subjective evaluations.44 An additional limitation of our study is that possible instant effects of retirement on sleep difficulties may be underestimated, as the interval between the study waves around the actual retirement date was approximately 4 years. To address this limitation, future studies should use shorter measurement intervals to study changes in sleep difficulties around retirement. Finally, the generalizability of these findings may be limited, as this large cohort consisted of relatively healthy public sector employees of European origin in a Nordic welfare state retiring on a statutory basis with a relatively generous retirement scheme. Thus, our results cannot be generalized into workers retiring due to work disability or other reasons. However, the same illnesses that lead to work disability could also affect sleep, a bias less probable in our more homogeneous group of statutory retirees. Future research is also needed to examine whether our findings are generalizable to other working sectors, countries, and cultures.
CONCLUSION
This study suggests that transition from full-time work to statutory retirement is associated with a decrease in sleep difficulties. These findings suggest that sleep, a major component of well-being, may be worse during the last working years than following retirement. Improving sleep and well-being in elderly employees is a challenge for many Western governments aiming at extending working careers. Divergent trends were observed in the specific types of sleep difficulties during retirement transition, as waking up too early in the morning and nonrestorative sleep decreased substantially, whereas difficulties falling asleep and difficulties maintaining sleep did not change during the retirement transition. The decreases in sleep difficulties were observed to be mainly driven by the decreases of sleep difficulties among those with suboptimal self-rated health and psychological distress before retirement.
SUPPLEMENTARY MATERIAL
Supplementary material is available at SLEEP online.
FUNDING
This study was financially supported by the Academy of Finland (grant numbers 286294 and 294154 to SS and 311492 to MK); the Finnish Ministry of Education and Culture (to SS); the Juho Vainio Foundation (to SS); and NordForsk, the Nordic Programme for Health and Welfare (grant number 75021 to MK).
WORK PERFORMED
Department of Public Health, University of Turku, FI-20014 University of Turku, Finland. Fax: +35 82 945 05 040
DISCLOSURE STATEMENT
None declared.



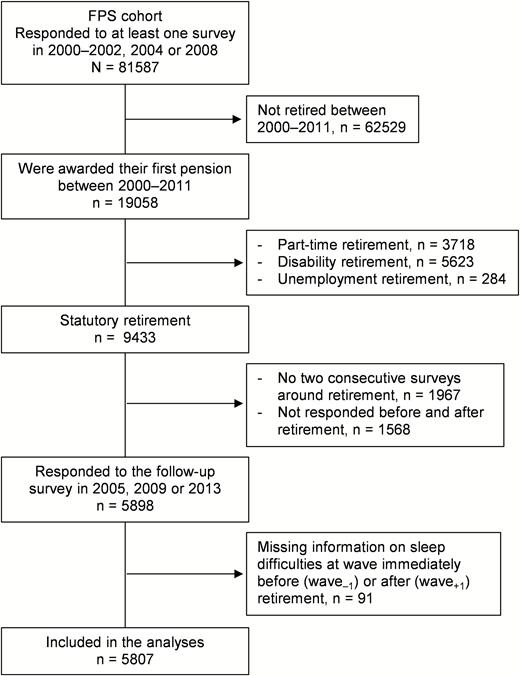
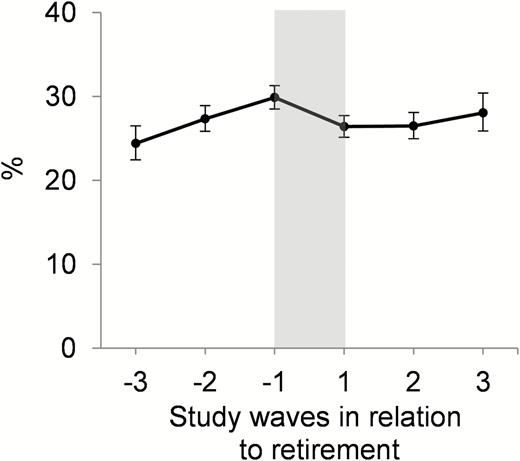
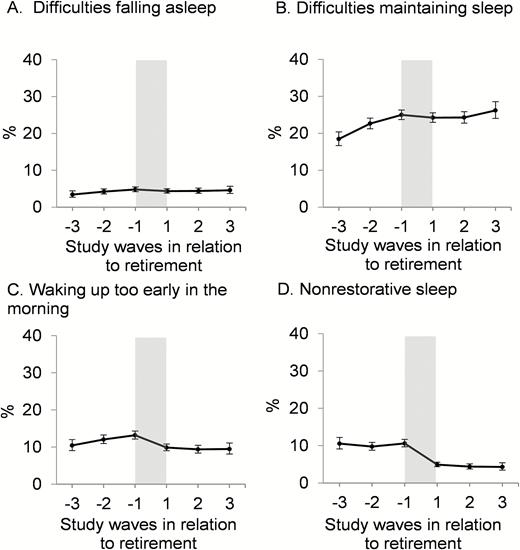

Comments