-
PDF
- Split View
-
Views
-
Cite
Cite
Bradley E. Karlin, Michele J. Karel, National Integration of Mental Health Providers in VA Home-Based Primary Care: An Innovative Model for Mental Health Care Delivery With Older Adults, The Gerontologist, Volume 54, Issue 5, October 2014, Pages 868–879, https://doi.org/10.1093/geront/gnt142
Close - Share Icon Share
Abstract
Purpose of the Study: To promote mental health (MH) service access and quality for veterans with complex and chronic medical, social, and behavioral conditions, the U.S. Department of Veterans Affairs (VA) has integrated a full-time MH provider into each VA home-based primary care (HBPC) team. The goal of the current evaluation is to examine the nature and extent to which MH care processes and practices have been integrated into HBPC nationally. Design and Methods: Separate surveys assessing the integration of a wide range of MH care practices and HBPC team processes were sent to MH providers and program directors in each HBPC program in 2010. Results: A total of 132 MH providers representing 119 HBPC programs, and 112 program directors completed the surveys. The most common clinical issues addressed by MH providers were depression, coping with illness and disability, anxiety, caregiver/family stress, and cognitive evaluation. Other team members typically conducted initial MH screenings, with MH providers’ time focusing on cases with identified needs. Approximately 40% of MH providers’ time was devoted to direct clinical care. Significant time was also spent on team activities, driving, and charting. Implications: Integration of MH services into HBPC is feasible and facilitates service access for a vulnerable population. Mental health care delivery in HPBC generally involves a high degree of interdisciplinary practice. Mental health integration into HBPC may serve as a model for other systems interested in promoting MH care delivery among homebound and other older individuals.
The Veterans Health Administration (VHA), the health care component of the U.S. Department of Veterans Affairs (VA), cares for a large aging veteran population through interdisciplinary, integrated, and innovative services across a broad continuum of care (Karlin, Zeiss, & Burris, 2010; Shay & Burris, 2008). Over the past two decades, VHA has placed an increasing emphasis on community-based care to help veterans, including those with very complex care needs, remain in noninstitutional home and community settings.
One of VHA’s largest and innovative noninstitutional geriatric care programs is home-based primary care (HBPC). HBPC provides comprehensive, interdisciplinary, and longitudinal care for mostly older veterans with complex and chronic medical, social, and behavioral conditions (Edes, 2010). Approximately two thirds of veterans served by HBPC in 2012 were aged 75 or older. The program’s goals are to help enrolled veterans maximize function, minimize institutionalization, and maintain quality of life. Historically, the HBPC team has included nurses, physicians, social workers, dieticians, physical and occupational therapists, and pharmacists, who work together on a patient-centered plan of care to address the veteran’s goals of care and the goals of family caregivers. HBPC care is associated with reduced hospital and nursing home admissions and bed days of care and overall decreased cost of care, including HBPC costs (Beales & Edes, 2009; Cooper & Edes, 2012). These positive outcomes have recently led the Center for Medicare and Medicaid Services (CMS) to develop a Medicare demonstration project based on HBPC (Kinosian & Edes, 2010).
Although the majority of veterans enrolled in HBPC have chronic medical illnesses including heart disease, diabetes, lung disease, dementia, and other neurologic conditions, mental health (MH) conditions are also rather common. In fact, depression, anxiety, posttraumatic stress disorder (PTSD), substance use disorder, and schizophrenia represent 5 of the top 10 overall diagnoses among the HBPC population (Edes, 2010). Further, veterans with mental illness or dementia are more likely than those without these diagnoses to be admitted to HBPC (Miller & Rosenheck, 2007). Beyond their direct consequences, MH conditions contribute to excess disability, premature institutionalization, increased mortality, and reduced quality of life among homebound (Davitt & Gellis, 2011; Qiu et al., 2010; Zeltzer & Kohn, 2006) and nonhomebound older adults (Callahan et al., 1998; Lenze et al., 2001; Schulz et al., 2000; Spitzer et al., 1995).
Growing research evidence supports the integration of geriatric MH services through collaborative, care management, and/or stepped care approaches in primary care (Alexopoulos et al., 2009; Ayalon, Areán, Linkins, Lynch, & Estes, 2007; Bartels et al., 2004; Emery, Lapidos, Eisenstein, Ivan, & Golden, 2012; Hunkeler et al., 2006) and home care settings (Bruce et al., 2007; Ciechanowski et al., 2004). In recent years, VHA has been transforming the delivery of MH services in the VA health care system to support integrated, interdisciplinary, and evidence-based MH care for older and younger veterans across the range of care settings. These efforts include, but are not limited to, MH integration in general primary care settings (Post, Metzger, Dumas, & Lehmann, 2010; Zeiss & Karlin, 2008) and a range of geriatric care settings (Karlin & Zeiss, 2010).
The integration of MH care into HBPC is a major initiative associated with the transformation of MH care in VHA and, specifically, with the integration of MH care into geriatrics settings. The integration of MH care into HBPC is intended to promote MH service access and quality for older individuals who may have or be at risk for mental illness. Older individuals have consistently been shown to receive MH care in specialty MH settings at very low rates (Byers, Areán, & Yaffe, 2012; Karlin, Duffy, & Gleaves, 2008). This is especially the case among homebound individuals (Davitt & Gellis, 2011; Qiu et al., 2010; Zeltzer & Kohn, 2006). Prior to the integration of MH care into HBPC, veterans in HBPC typically received MH services—particularly psychological services—at VA medical centers or community-based outpatient clinics (CBOCs), which, by definition, would be quite challenging for these individuals. Basic psychotropic (e.g., antidepressant) medications were sometimes prescribed by a nurse practitioner or physician on the HBPC team, and some HBPC teams had psychopharmacotherapy consultation support from psychiatry. Furthermore, social workers on some HBPC teams had provided supportive counseling in addition to social service and admission/discharge functions. The broader range of psychological assessment and treatment services, however, was not as readily accessed.
The HBPC MH initiative, initiated in 2007, involved the placement of a full-time, doctoral-level MH provider (typically a psychologist or in some cases a psychiatrist) on each of approximately 120 HBPC teams nationally. The focus on doctoral-level providers, namely psychologists, was based on the range of psychological services often required by the HBPC patient population. In addition to more standard psychosocial treatment services, HBPC patients often require cognitive and psychological assessment (e.g., brief dementia evaluation, assessment of medical decision making, or independent living capacity) and more complex intervention services that are not generally within the scope of practice of masters-level clinicians. In 2008, the inclusion of a full-time MH provider as a core member of the interdisciplinary HBPC team was established as national policy in VHA, thereby making this as an enduring national requirement (U.S. Department of Veterans Affairs, 2008). In guiding hiring for these positions, the national position description included a wide range of professional functions including evidence-based assessment and treatment of mental disorders, assessment of decision-making and functional capacities, services for families and caregivers, promotion of interdisciplinary team communication and functioning, and prevention-oriented services.
Mental health integration in HBPC represents a new model of interdisciplinary, home-based MH care for the 21st century whereby MH services are integrated (and interwoven) into the interdisciplinary team delivering services in the home. Beyond enhancing patient access to a MH specialist, the ultimate goal is to systemically integrate MH education and care processes (e.g., screening, psychoeducation, and follow-up) into the fabric of interdisciplinary team care and for the MH provider to help inform and facilitate other aspects of the treatment plan and care delivery (e.g., by increasing medical adherence, promoting primary care provider–patient interactions). Through screening and stepped care approaches, the MH provider may then work with the team to identify veterans that would benefit from specialized MH evaluation or treatment. The model of care is informed by evidence-based components of integrated care, including collaborative, colocated, and stepped care approaches (AGS Geriatrics Interdisciplinary Advisory Group, 2006; Bartels et al., 2004; Hunkeler et al., 2006; Hunter & Goodie, 2010; Katon et al., 1999; van’t Veer-Tazelaar et al., 2009), as well as evidence-based geropsychological and geropsychiatric evaluation and treatment approaches (Blazer & Steffens, 2012; Lichtenberg, 2010; Scogin & Shah, 2012).
The goal of this article is to describe the nature and extent to which MH care has been integrated into HBPC with the addition of the MH provider as part of the HBPC team, based on program evaluation data derived from national surveys of HBPC MH providers and HBPC program directors. Specifically, the aims of the current evaluation are to characterize (a) the MH issues identified and addressed in HBPC; (b) strategies for MH screening, evaluation, and intervention; (c) how time was being spent by the integrated MH providers in various professional activities; (d) the extent of integration into team functioning; and (e) ongoing educational needs. This is, to our knowledge, the first article to empirically report on and describe care process and practices associated with the integration of doctoral-level MH providers into home-based care. In addition to describing the landscape of MH care practice and delivery in HBPC in the VA health care system, the article seeks to begin to shed light on best practices for MH integration in primary care provided in the home setting.
Methods
As part of national program evaluation efforts, two surveys were developed and administered to HBPC MH providers and HBPC program directors, respectively. The program director (usually a nurse or social worker) maintains administrative oversight of the HBPC program, team meetings, and HPBC team members. Surveys were sent to and returned by each HBPC program in the spring of 2010. If an HBPC program had more than one MH provider, each provider was asked to complete the HBPC MH provider survey. One program director per site was asked to complete the program director survey.
Program Evaluation Measures
HBPC MH Provider Survey.
The HBPC MH provider survey included 52 items, some with multiple ratings required, assessing 12 major domains through a combination of scaled or multiple-choice items and open-ended questions: (a) identifying and descriptive information, (b) HBPC MH provider characteristics, (c) clinical issues addressed by HBPC MH providers, (d) identification of HBPC veterans in need of MH care, (e) MH evaluation by HBPC MH providers, (f) MH intervention by HBPC MH providers, (g) clinical pathways for MH care in HBPC, (h) transitions in care and HBPC MH, (i) HBPC team functioning, (j) implementation resources, (k) MH trainees in HBPC, and (l) HBPC MH provider activities. Participants were invited to provide additional comments at the end of the survey.
HBPC Program Director Survey.
The HBPC program director survey included 33 items, some with multiple ratings required, assessing six core domains through a combination of scaled or multiple-choice items and open-ended questions: (a) identifying and descriptive information, (b) HBPC program characteristics, (c) integration of HBPC MH provider on HBPC team, (d) implementation resources, (e) impact of integrating MH in HBPC, and (f) overall progress in integrating MH care in HBPC. Participants were invited to provide additional comments at the end of the survey.
Sample and Program Description
HBPC MH Providers.
A total of 132 MH providers representing 119 HBPC programs completed the HBPC MH provider survey. Seven HBPC teams had more than one MH provider respond to the survey (from two to four at each site). Four additional MH providers from another four HBPC programs returned the survey but did not complete it (e.g., had just started the job and did not feel able to answer most questions). Of 132 respondents, 126 (95.5%) were psychologists and 6 (4.5%) were psychiatrists.
At the time of the survey, 46.6% of MH providers reported having worked for HBPC for more than 2 years. Thirteen percent had been with the program for less than 6 months, whereas the remainder served as HBPC MH providers for 7–12 months (16.0%), 13–18 months (9.9%), or 19–24 months (14.5%). The majority of respondents (56%) reported spending sometime each week providing MH services in other VHA programs, both geriatric (30.3%) and nongeriatric (37.9%) care settings. Only 58 respondents (44%) reported working full time for HBPC. Most MH providers reported having office space that was colocated with their HBPC teams (62.9%). A minority were in separate space, in the same building (12.1%), different building but same campus (15.2%), different campus (3.8%), or other (6.1%).
HBPC Program Directors.
A total of 116 HBPC program directors returned the survey. At the time, 101 program directors (87.1%) reported having at least one dedicated MH provider working in their program; 112 HBPC program directors completed the survey and comprise the sample for this evaluation.
HBPC Programs.
HBPC programs varied widely in terms of program size, number of HBPC teams at the facility (e.g., covering different geographical areas), urbanicity, and travel distances and times to veterans’ homes. The mean average daily census (ADC) reported by the program directors (n = 112) was 189 (SD = 120, range = 22–670). Number of teams per program ranged from one to eight, with a mean of 2.0 teams per facility (SD = 1.4). Some VHA facilities serve veterans across large geographical regions, requiring two or more HBPC teams to cover the full catchment area. Program directors categorized programs as highly or somewhat rural (37.4%), highly or somewhat urban (33.9%), or mixed or neither (28.7%). Maximum reported travel distances from the office to veterans’ homes ranged from 15 to 150 miles, with a mean of 52.9 miles (SD = 23.8). Maximum reported travel times ranged from 25 to 180min, with a mean maximum travel time of 68.5min (SD = 28.6). Average maximum travel distances and travel times were greatest among rural and least among urban programs (F(2, 112) = 7.1, p < .001, and F(2, 112) = 4.1, p < .05, respectively).
Results
Team Integration of MH Services
The majority of MH providers reported that MH services had been moderately (39%) to fully (49%) integrated into their HBPC program and that their team members were moderately (45%) or extremely (42%) knowledgeable regarding their role and services. Likewise, MH provider responses related to interdisciplinary versus multidisciplinary functioning of the team (based on a continuum where “1” indicated fully multidisciplinary and “5” indicated fully interdisciplinary) indicated that teams were more highly distributed toward interdisciplinary functioning (1 = 1.5%, 2 = 13.8%, 3 = 27.7%, 4 = 39.2%, and 5 = 17.7%). MH providers reported making only occasional home visits with other HBPC team members, with 45% reporting “never or rarely,” 45% reporting “occasionally,” and 10% reporting “often” or “frequently.”
Furthermore, in response to an open-ended question related to activities or processes, the HBPC team engages in promoting team collaboration or cohesion, MH providers reported most frequently responses reflecting themes related to having regular team meetings (n = 67), celebrations of special occasions at work (n = 41), occasional lunches or other meals together (n = 39), open and respectful communication (n = 24), and in-services or other trainings together (n = 22). In response to a question about activities they implemented to promote team collaboration and cohesion, MH providers most frequently identified offering in-services or other trainings related to MH topics (n = 31), facilitating team communication (n = 15), having informal discussions for case collaboration (n = 12), having an open-door policy to discuss issues with team members (n = 11), and offering emotional support to team members (e.g., related to bereavement when patients die; n = 11). Twenty-one MH providers responded “N/A” or “none” in response to this question.
HBPC program directors also reported a high degree of MH service integration into their programs (Figure 1). More than three quarters of program directors reported that MH services have been “truly integrated into your HBPC Program” either “a lot” or “a great deal.” Among the most positive impacts of MH integration identified by program directors were increased likelihood of identifying MH problems in enrolled veterans and increased likelihood that veterans would receive MH care.
Perceptions of mental health integration among home-based primary care (HBPC) program directors. Note: Graph reflects the percent of HBPC program directors who responded “Not at all” or “Slightly,” “Somewhat,” and “A Lot” or “A Great Deal” in response to the question: “To what degree have the following issues been influenced by the integration of mental health services into your HBPC Program?” (n = 112). Graph does not include small percentages off “N/A” responses; thus, bars do not total to 100%.
Moreover, in response to an open-ended question, “Please comment on the impact of having an HBPC MH provider as part of your HBPC team,” the most common themes identified by program directors were helping the team to understand complex behavioral and MH issues, including family dynamics (n = 26); increasing veteran access to MH services (n = 24); helping the team to develop strategies for working with veterans/families struggling with behavioral and MH concerns (n = 13); enhancing overall program quality of care (n = 12); increasing the team’s holistic conceptualization and approach to patient care (n = 11); helping family members to cope better (n = 9); supporting team development and cohesion (n = 8); and availability to consult with team members as needed (n = 8).
Processes for MH Screening, Assessment, and Referral
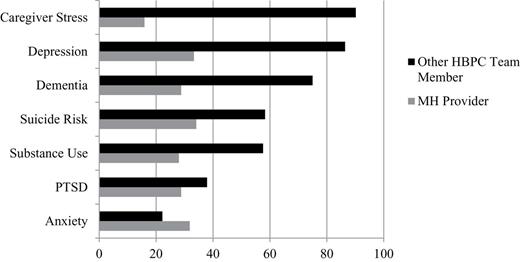
HBPC MH provider responses to questions related to how often the MH provider or other team members conduct initial screening of patients upon admission to HBPC are reported in Figure 2. As Figure 2 reveals, other members of the interdisciplinary team overwhelmingly conduct initial screenings for caregiver stress, depression, and dementia. Further, only 10% of MH providers reported having contact with every veteran enrolled in their HBPC program. Rather than seeing all enrolled HBPC patients, the majority of MH providers reported that team members alert them when there is an indication that a veteran needs MH care (92%) and/or they see veterans based on discussions in HBPC interdisciplinary team meetings (85%). MH providers reported that requests to see patients come from a variety of team members, including most commonly, social workers (93%), registered nurses (89%), advance practice nurses (67%), or physicians (60%).
Initial screening/assessment for mental health (MH) issues upon home-based primary care (HBPC) admission. Note: Graph reflects the percent of MH providers reporting initial screening/assessment by MH provider and/or other HBPC team member (N = 132).
When MH providers do see a veteran for a MH evaluation, the majority (79%) reported that they “often” or “frequently” then provide a full MH intervention, whereas many (53%) also reported “often” or “frequently” providing an abbreviated intervention (1–3 sessions). Referrals to other VA specialty MH programs do occur on occasion; 48% of MH providers reported referring to other VA programs “never” or “rarely,” 44% “occasionally,” 9% “often,” and none “frequently.”
Psychotropic medication services for veterans in HBPC are provided most often by the primary care provider on the team (80%) and/or through as-needed, formal consultation with psychiatry (at the VA medical center or CBOC). Very few MH providers reported having integrated psychiatrists on the team, either full time (8%) or part time (3%). About one third (39%) of MH providers did report using as-needed, informal consultation with psychiatry (e.g., a phone call to receive suggestions for care).
Mental and Behavioral Health Issues in HBPC
HBPC MH provider responses to questions related to how often various clinical issues were a focus of their work with veterans in HBPC through direct services and/or team consultation are displayed in Table 1. Clinical issues rated as most frequently an area of focus were depression, coping with illness/disability, anxiety, caregiver/family stress, cognitive/dementia evaluation, and adherence issues. Problems that were less commonly a focus of regular attention were traumatic brain injury, weight management, substance misuse/abuse/dependence, and serious mental illness. MH providers were asked to indicate “other” clinical issues they address in HBPC that were not specifically asked about. Responses included marital/family issues, end-of-life care, suicide risk, smoking cessation, personality disorders, and specific medical illnesses (e.g., Parkinson’s disease, stroke).
Mental and Behavioral Health Issues Addressed by Home-Based Primary Care Mental Health Providers
| Clinical issue . | Mean (SD) . | Never or rarely (%) . | Occasionally (%) . | Often or frequently (%) . |
|---|---|---|---|---|
| Depression | 4.8 (0.4) | 0 | 0.8 | 99.2 |
| Coping with illness/disability | 4.6 (0.7) | 0.8 | 6.8 | 92.4 |
| Anxiety | 4.5 (0.6) | 0 | 6.2 | 93.8 |
| Caregiver/family stress | 4.3 (0.7) | 1.5 | 11.4 | 87.1 |
| Cognitive/dementia evaluation | 4.2 (0.9) | 4.5 | 13.6 | 81.9 |
| Adherence | 4.0 (0.8) | 3.8 | 23.7 | 72.5 |
| Insomnia | 3.9 (0.8) | 2.3 | 29.8 | 67.9 |
| Chronic pain | 3.8 (0.9) | 8.3 | 28.0 | 63.7 |
| Grief and loss | 3.8 (0.8) | 3.8 | 36.4 | 59.8 |
| Behavior management | 3.7 (0.8) | 3.0 | 37.9 | 59.1 |
| Decision-making capacity | 3.7 (0.9) | 11.4 | 29.5 | 59.1 |
| PTSD | 3.6 (0.9) | 7.7 | 42.0 | 50.3 |
| Serious mental illness | 3.0 (0.8) | 30.5 | 48.9 | 20.6 |
| Substance misuse/abuse/dependence | 3.0 (0.7) | 18.9 | 61.4 | 19.7 |
| Weight management | 3.0 (1.0) | 31.1 | 39.4 | 29.5 |
| Traumatic brain injury | 2.3 (0.7) | 69.0 | 26.2 | 4.8 |
| Clinical issue . | Mean (SD) . | Never or rarely (%) . | Occasionally (%) . | Often or frequently (%) . |
|---|---|---|---|---|
| Depression | 4.8 (0.4) | 0 | 0.8 | 99.2 |
| Coping with illness/disability | 4.6 (0.7) | 0.8 | 6.8 | 92.4 |
| Anxiety | 4.5 (0.6) | 0 | 6.2 | 93.8 |
| Caregiver/family stress | 4.3 (0.7) | 1.5 | 11.4 | 87.1 |
| Cognitive/dementia evaluation | 4.2 (0.9) | 4.5 | 13.6 | 81.9 |
| Adherence | 4.0 (0.8) | 3.8 | 23.7 | 72.5 |
| Insomnia | 3.9 (0.8) | 2.3 | 29.8 | 67.9 |
| Chronic pain | 3.8 (0.9) | 8.3 | 28.0 | 63.7 |
| Grief and loss | 3.8 (0.8) | 3.8 | 36.4 | 59.8 |
| Behavior management | 3.7 (0.8) | 3.0 | 37.9 | 59.1 |
| Decision-making capacity | 3.7 (0.9) | 11.4 | 29.5 | 59.1 |
| PTSD | 3.6 (0.9) | 7.7 | 42.0 | 50.3 |
| Serious mental illness | 3.0 (0.8) | 30.5 | 48.9 | 20.6 |
| Substance misuse/abuse/dependence | 3.0 (0.7) | 18.9 | 61.4 | 19.7 |
| Weight management | 3.0 (1.0) | 31.1 | 39.4 | 29.5 |
| Traumatic brain injury | 2.3 (0.7) | 69.0 | 26.2 | 4.8 |
Notes: N = 132. Items were rated on a 5-point Likert scale, ranging from 1 (never) to 5 (frequently). For display in this table, responses were combined for “never” and “rarely” and for “often” and “frequently.”
Mental and Behavioral Health Issues Addressed by Home-Based Primary Care Mental Health Providers
| Clinical issue . | Mean (SD) . | Never or rarely (%) . | Occasionally (%) . | Often or frequently (%) . |
|---|---|---|---|---|
| Depression | 4.8 (0.4) | 0 | 0.8 | 99.2 |
| Coping with illness/disability | 4.6 (0.7) | 0.8 | 6.8 | 92.4 |
| Anxiety | 4.5 (0.6) | 0 | 6.2 | 93.8 |
| Caregiver/family stress | 4.3 (0.7) | 1.5 | 11.4 | 87.1 |
| Cognitive/dementia evaluation | 4.2 (0.9) | 4.5 | 13.6 | 81.9 |
| Adherence | 4.0 (0.8) | 3.8 | 23.7 | 72.5 |
| Insomnia | 3.9 (0.8) | 2.3 | 29.8 | 67.9 |
| Chronic pain | 3.8 (0.9) | 8.3 | 28.0 | 63.7 |
| Grief and loss | 3.8 (0.8) | 3.8 | 36.4 | 59.8 |
| Behavior management | 3.7 (0.8) | 3.0 | 37.9 | 59.1 |
| Decision-making capacity | 3.7 (0.9) | 11.4 | 29.5 | 59.1 |
| PTSD | 3.6 (0.9) | 7.7 | 42.0 | 50.3 |
| Serious mental illness | 3.0 (0.8) | 30.5 | 48.9 | 20.6 |
| Substance misuse/abuse/dependence | 3.0 (0.7) | 18.9 | 61.4 | 19.7 |
| Weight management | 3.0 (1.0) | 31.1 | 39.4 | 29.5 |
| Traumatic brain injury | 2.3 (0.7) | 69.0 | 26.2 | 4.8 |
| Clinical issue . | Mean (SD) . | Never or rarely (%) . | Occasionally (%) . | Often or frequently (%) . |
|---|---|---|---|---|
| Depression | 4.8 (0.4) | 0 | 0.8 | 99.2 |
| Coping with illness/disability | 4.6 (0.7) | 0.8 | 6.8 | 92.4 |
| Anxiety | 4.5 (0.6) | 0 | 6.2 | 93.8 |
| Caregiver/family stress | 4.3 (0.7) | 1.5 | 11.4 | 87.1 |
| Cognitive/dementia evaluation | 4.2 (0.9) | 4.5 | 13.6 | 81.9 |
| Adherence | 4.0 (0.8) | 3.8 | 23.7 | 72.5 |
| Insomnia | 3.9 (0.8) | 2.3 | 29.8 | 67.9 |
| Chronic pain | 3.8 (0.9) | 8.3 | 28.0 | 63.7 |
| Grief and loss | 3.8 (0.8) | 3.8 | 36.4 | 59.8 |
| Behavior management | 3.7 (0.8) | 3.0 | 37.9 | 59.1 |
| Decision-making capacity | 3.7 (0.9) | 11.4 | 29.5 | 59.1 |
| PTSD | 3.6 (0.9) | 7.7 | 42.0 | 50.3 |
| Serious mental illness | 3.0 (0.8) | 30.5 | 48.9 | 20.6 |
| Substance misuse/abuse/dependence | 3.0 (0.7) | 18.9 | 61.4 | 19.7 |
| Weight management | 3.0 (1.0) | 31.1 | 39.4 | 29.5 |
| Traumatic brain injury | 2.3 (0.7) | 69.0 | 26.2 | 4.8 |
Notes: N = 132. Items were rated on a 5-point Likert scale, ranging from 1 (never) to 5 (frequently). For display in this table, responses were combined for “never” and “rarely” and for “often” and “frequently.”
Professional Activities of MH Providers
The proportion of time spent per week by MH providers in various professional activities is displayed in Table 2. MH providers working full time for their HBPC Program reported spending most of their weekly time in direct clinical contact with veterans and/or family members, driving to/from visits, and completing chart review and documentation. In addition, MH providers reported spending an average of almost 6hr/week in team activities (team meetings, consultation, and training). MH providers working full time in HBPC programs serving highly or somewhat urban areas reported spending significantly less time on the phone with veterans/caregivers (M = 2.1hr/week, SD = 1.6) than those MH providers working in HBPC programs serving rural (M = 3.8, SD = 1.9) or mixed rural/urban (M = 3.5, SD = 2.2) areas (F(2, 48) = 3.67, p = .03).
Time Spent per Week by Mental Health (MH) Provider in Various Professional Activities
| Activity . | Mean hr/week . | SD . | Range . |
|---|---|---|---|
| In-person with veteran or family | 12.7 | 4.7 | 0–23 |
| On phone with veteran or family | 3.1 | 2.8 | 0–14 |
| Team meetings | 3.4 | 2.1 | 1–13 |
| Team consultation and training | 2.5 | 1.5 | 0–7 |
| Driving to/from home visits/meetings | 9.3 | 3.9 | 0–17 |
| Chart review, preparation, documentation | 6.8 | 3.2 | 0–15 |
| Administration or training activities | 2.2 | 3.0 | 0–16 |
| Activity . | Mean hr/week . | SD . | Range . |
|---|---|---|---|
| In-person with veteran or family | 12.7 | 4.7 | 0–23 |
| On phone with veteran or family | 3.1 | 2.8 | 0–14 |
| Team meetings | 3.4 | 2.1 | 1–13 |
| Team consultation and training | 2.5 | 1.5 | 0–7 |
| Driving to/from home visits/meetings | 9.3 | 3.9 | 0–17 |
| Chart review, preparation, documentation | 6.8 | 3.2 | 0–15 |
| Administration or training activities | 2.2 | 3.0 | 0–16 |
Note: Figures reported above are for MH providers assigned full time to home-based primary care (n = 58) and are adjusted for 40-hr work week.
Time Spent per Week by Mental Health (MH) Provider in Various Professional Activities
| Activity . | Mean hr/week . | SD . | Range . |
|---|---|---|---|
| In-person with veteran or family | 12.7 | 4.7 | 0–23 |
| On phone with veteran or family | 3.1 | 2.8 | 0–14 |
| Team meetings | 3.4 | 2.1 | 1–13 |
| Team consultation and training | 2.5 | 1.5 | 0–7 |
| Driving to/from home visits/meetings | 9.3 | 3.9 | 0–17 |
| Chart review, preparation, documentation | 6.8 | 3.2 | 0–15 |
| Administration or training activities | 2.2 | 3.0 | 0–16 |
| Activity . | Mean hr/week . | SD . | Range . |
|---|---|---|---|
| In-person with veteran or family | 12.7 | 4.7 | 0–23 |
| On phone with veteran or family | 3.1 | 2.8 | 0–14 |
| Team meetings | 3.4 | 2.1 | 1–13 |
| Team consultation and training | 2.5 | 1.5 | 0–7 |
| Driving to/from home visits/meetings | 9.3 | 3.9 | 0–17 |
| Chart review, preparation, documentation | 6.8 | 3.2 | 0–15 |
| Administration or training activities | 2.2 | 3.0 | 0–16 |
Note: Figures reported above are for MH providers assigned full time to home-based primary care (n = 58) and are adjusted for 40-hr work week.
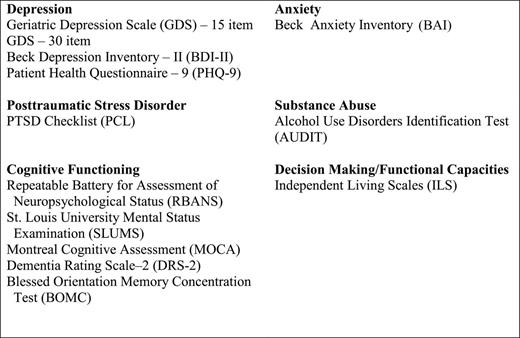
The proportion of time spent per week by MH providers in specific clinical activities is displayed in Table 3. As Table 3 reveals, MH providers varied considerably in how they reported spending their clinical time with veterans and/or caregivers. Among the various clinical activities performed, MH providers reported spending the greatest amount of time, on average, providing psychotherapy. Although ranges varied considerably, other clinical activities taking up significant time were team consultation, family/caregiver support and education, brief screening/assessment, and brief cognitive/dementia evaluation. Figure 3 lists the most common screening and assessment measures used by MH providers and their teams.
Percent of Clinical Time Spent by Home-Based Primary Care Mental Health (MH) Provider in Specific Clinical Activities Each Month
| Clinical activity . | Mean percent clinical time each month . | SD . | Range . |
|---|---|---|---|
| Individual psychotherapy | 36.9 | 18.2 | 0–75 |
| Team consultation | 12.1 | 8.7 | 5–50 |
| Brief screening/assessment | 11.3 | 11.3 | 0–50 |
| Brief cognitive/dementia evaluation | 11.2 | 10.3 | 0–50 |
| Family/caregiver support and education | 9.4 | 6.6 | 0–25 |
| Family/couples psychotherapy | 8.5 | 9.1 | 0–40 |
| Capacity/functional evaluation | 5.2 | 4.7 | 0–15 |
| Full neuropsychological evaluation | 2.1 | 4.1 | 0–20 |
| Psychological/personality evaluation | 1.7 | 3.5 | 0–20 |
| Medication management | 1.5 | 7.5 | 0–50 |
| Clinical activity . | Mean percent clinical time each month . | SD . | Range . |
|---|---|---|---|
| Individual psychotherapy | 36.9 | 18.2 | 0–75 |
| Team consultation | 12.1 | 8.7 | 5–50 |
| Brief screening/assessment | 11.3 | 11.3 | 0–50 |
| Brief cognitive/dementia evaluation | 11.2 | 10.3 | 0–50 |
| Family/caregiver support and education | 9.4 | 6.6 | 0–25 |
| Family/couples psychotherapy | 8.5 | 9.1 | 0–40 |
| Capacity/functional evaluation | 5.2 | 4.7 | 0–15 |
| Full neuropsychological evaluation | 2.1 | 4.1 | 0–20 |
| Psychological/personality evaluation | 1.7 | 3.5 | 0–20 |
| Medication management | 1.5 | 7.5 | 0–50 |
Note: Figures reported above are for MH providers with percentages of time totaling 100% (n = 46).
Percent of Clinical Time Spent by Home-Based Primary Care Mental Health (MH) Provider in Specific Clinical Activities Each Month
| Clinical activity . | Mean percent clinical time each month . | SD . | Range . |
|---|---|---|---|
| Individual psychotherapy | 36.9 | 18.2 | 0–75 |
| Team consultation | 12.1 | 8.7 | 5–50 |
| Brief screening/assessment | 11.3 | 11.3 | 0–50 |
| Brief cognitive/dementia evaluation | 11.2 | 10.3 | 0–50 |
| Family/caregiver support and education | 9.4 | 6.6 | 0–25 |
| Family/couples psychotherapy | 8.5 | 9.1 | 0–40 |
| Capacity/functional evaluation | 5.2 | 4.7 | 0–15 |
| Full neuropsychological evaluation | 2.1 | 4.1 | 0–20 |
| Psychological/personality evaluation | 1.7 | 3.5 | 0–20 |
| Medication management | 1.5 | 7.5 | 0–50 |
| Clinical activity . | Mean percent clinical time each month . | SD . | Range . |
|---|---|---|---|
| Individual psychotherapy | 36.9 | 18.2 | 0–75 |
| Team consultation | 12.1 | 8.7 | 5–50 |
| Brief screening/assessment | 11.3 | 11.3 | 0–50 |
| Brief cognitive/dementia evaluation | 11.2 | 10.3 | 0–50 |
| Family/caregiver support and education | 9.4 | 6.6 | 0–25 |
| Family/couples psychotherapy | 8.5 | 9.1 | 0–40 |
| Capacity/functional evaluation | 5.2 | 4.7 | 0–15 |
| Full neuropsychological evaluation | 2.1 | 4.1 | 0–20 |
| Psychological/personality evaluation | 1.7 | 3.5 | 0–20 |
| Medication management | 1.5 | 7.5 | 0–50 |
Note: Figures reported above are for MH providers with percentages of time totaling 100% (n = 46).
Standardized measures most commonly used for mental health screening and assessment in home-based primary care.
MH providers reported using a wide range of clinical interventions. A large majority reported providing cognitive behavioral therapy (86%). Other commonly endorsed therapeutic approaches included cognitive training for the use of compensatory strategies (65%), interpersonal psychotherapy (40%), problem-solving therapy (35%), and acceptance and commitment therapy (31%). In all of these cases, only about one quarter to one third reported using a particular treatment protocol/manual. Relatively few MH providers reported using cognitive processing therapy or prolonged exposure therapy for PTSD (19% and 6%, respectively), first-line treatments for PTSD. Across treatment approaches, the average number of therapy sessions ranged from 7.0 to 10.8 (with the exception of fewer sessions for cognitive training, with an average of 5.9 sessions). The average length of time for sessions ranged from 57 to 63min.
Educational Needs
MH providers and program directors were each asked to indicate educational topics that would be valuable for their work in HBPC, or useful for their entire HBPC team. The topics endorsed by more than half of the MH providers were behavioral interventions for dementia (80%), capacity assessment (79%), dementia evaluation (65%), family caregiver interventions (63%), grief and loss (59%), motivational interviewing (56%), and team MH training (55%). The topics endorsed by at least half of the program directors were managing difficult behaviors in dementia (87%); overview of dementia/dementia evaluation (81%); working with families and caregivers (80%); preventing burnout (70%); grief, loss, death, and dying (68%); and enhancing team functioning (65%).
Discussion
This is the first examination to date of MH provider delivery practices and clinical processes associated with the integration of MH care in a national HBPC program. Survey results from HBPC MH providers and program directors reveal a number of positive findings and developments associated with the integration of MH in HBPC. These results provide an important snapshot of early program implementation that can be used as a baseline comparison for ongoing program evaluation efforts. The integration of MH providers in HBPC and greater attention to screening for MH issues has allowed a wide range of mental and behavioral health needs to be identified and addressed in this population. MH providers’ and program directors’ survey responses converged to indicate perceptions of good integration of MH services into the overall team model and care processes. Further, program directors reported multiple benefits of MH care integration, including greater access for veterans to MH services and greater team understanding of and skills for addressing MH and behavioral issues. MH providers are clearly being utilized in and valued by this primary care program.
The survey findings further shed light on best practices related to the delivery of integrated MH care in HBPC. Consistent with integrated MH services developing in general clinic-based primary care settings, many HBPC MH providers and teams are using components of colocated, collaborative, and stepped care approaches to most efficiently and effectively meet the needs of HBPC patients and leverage the support of interdisciplinary team members (e.g., Bartels et al., 2004; Hunkeler et al., 2006; Katon et al., 1999). MH providers generally do not see every veteran enrolled in HBPC; rather, other team members often conduct initial screenings for MH conditions freeing up the MH providers to focus on cases with identified and more challenging MH needs. Initial nursing and/or social work assessments often include standardized screenings for depression, dementia warning signs, substance use, caregiver strain, PTSD, and/or other MH issues. MH providers typically provide direct services to veterans when, on the basis of team screenings and discussion, they are alerted to a specialized need.
MH providers reported spending an average of 40% of their time each week providing clinical services, in person or by phone, to veterans and their caregivers. Significant time was devoted to driving to/from visits, team activities, and documentation. These findings indicate that standards for clinical productivity—across disciplines—must be adjusted for the realities of home-based care. This model of MH care delivery differs significantly from traditional, outpatient MH care delivery models. For example, it is evident that it is not realistic to expect 25–30 direct services hours/week, which is typical in clinic-based MH settings, in HBPC with an average of 9hr/week required for driving and 6hr/week devoted to team treatment planning and training activities.
Survey results demonstrate significant variability in the relative time spent by MH providers in specific clinical activities (e.g., psychotherapy, cognitive evaluation, and team consultation). This variability may, in part, reflect important differences in the needs of patients served by different HBPC teams. For example, some HBPC teams may care for a large number of veterans with dementia, whereas other teams care for fewer such patients, who often require and benefit from different kinds of services than veterans without dementia. Beyond variability among patients served by different HBPC teams, the MH provider’s training and expertise may also influence the specific types of services most often provided. HBPC MH providers provide services across a wide range of psychological assessment and intervention activities and include individuals trained as health psychologists, geropsychologists, neuropsychologists, general clinical or counseling psychologists, and psychiatrists. Further, many of these providers began working in HBPC with little knowledge of or experience with interdisciplinary colocated or collaborative care models. In addition, differences among MH providers in relative time spent in various professional activities may reflect differences among teams in the level of MH provider support (with some teams having more than one MH provider) and ADC. Lastly, it is worth highlighting that the overall HBPC program is itself variable and flexible to allow for individual programs to best meet the needs of the catchment areas and patients they serve. Of note, eligibility requirements for HBPC have historically been more flexible than the eligibility requirements for home care and the definition of homebound under Medicare.
The current findings suggest several important challenges and areas for continued growth for MH care integration in HBPC. Although there is good evidence of interdisciplinary team functioning and collaboration around MH screening, not all of the HBPC MH providers had training or experience in interdisciplinary team-based, integrated care. On an interdisciplinary geriatric health care team, the MH provider can play an important role in facilitating team communication and collaboration, in addition to providing direct clinical services to patients. It is notable that a sizeable minority of HBPC MH providers reported engaging in few, if any, activities to promote team collaboration and cohesion. As many of these providers were relatively new to their teams at the time of the surveys were conducted, and the program was still fairly new at the time, they may not have yet felt empowered to play a role in supporting team functioning. Supporting team-based, collaborative care is an important area for ongoing education and training for the overall initiative.
Another identified challenge involves implementing and adapting evidence-based psychotherapy interventions for the HBPC population and setting. Although there is a growing research base on evidence-based MH interventions for older adults (Ayers, Sorrell, Thorp, & Wetherell, 2007; Logsdon, McCurry, & Teri, 2007; Scogin, Welsh, Hanson, Stump, & Coates, 2005), including recent interventions developed for the home setting (Ciechanowski et al., 2004; Ell et al., 2007; Gellis et al., 2008; Kaufman, Scogin, MaloneBeach, Baumhover, & McKendree-Smith, 2000; Kiosses, Arean, Teri, & Alexopoulos, 2010), these interventions often must be adapted and integrated for this frail population with complex and interacting needs (Alexopoulos et al., 2011; Areán et al., 2010; Satre, Knight, & David, 2006). Moreover, delivering MH services in the home setting can raise a host of unfamiliar ethical, clinical, and logistical challenges (Hicken & Plowhead, 2010; Yang, Garis, Jackson, & McClure, 2009). Further, it can be difficult to provide consistent, weekly therapy sessions required by some evidence-based psychotherapy protocols, given the realities of caseloads, patient illnesses, and travel time demands. Of note, many HBPC teams have received training in Resources for Enhancing Alzheimer’s Caregiver Health in VA (REACH-VA), an evidence-based intervention adapted for caregivers of veterans with dementia (Nichols, Martindale-Adams, Burns, Graney, & Zuber, 2011). An abbreviated version of REACH-VA has been developed for feasibility of implementation in HBPC. There is significant need for additional evidence-based psychological approaches validated with and feasible for implementation with older homebound individuals.
Summary and Future Directions
The current findings suggest that there is an important and innovative role for MH providers in the delivery of HBPC. Although there are a number of promising models of integrated geriatric MH care (Alexopoulos et al., 2009; Emery et al., 2012; Hunkeler et al., 2006), MH care delivery in HBPC is clearly distinct from other MH care delivery models due to features of the care setting (veterans’ homes), the team-based nature of service delivery, and the patient population (i.e., mostly older veterans with complex and chronic medical, social, and behavioral conditions). The results reported herein suggest significant benefit and feasibility associated with the integration of MH care into interdisciplinary, home-based care for older veterans with multiple, chronic conditions. As integral members of the interdisciplinary HBPC team, psychologists and psychiatrists can provide direct MH assessment and intervention services to veterans and families as well as collaborate with the team in consultation, training, and support activities. At the same time, this innovative model for geriatric MH care raises important clinical, logistical, and productivity issues and necessitates training in interdisciplinary, collaborative models of integrated MH care delivery.
The current findings have contributed to a number of strategic developments and quality improvement initiatives for the HBPC MH initiative. These include (a) continued development and adoption across HBPC programs of an interdisciplinary MH care model in HBPC whereby non-MH team members can support MH assessment and treatment-related activities and allow the MH provider to focus on more challenging cases and needs of the team, (b) development of a national web-based training program for promoting MH interdisciplinary care practices and competencies in HBPC, (c) providing additional educational opportunities and resources regarding evidence-based MH assessment and intervention relevant to the HBPC population, and (d) ongoing program evaluation activities related to MH care integration in HBPC and examination of MH utilization and outcomes for HBPC veterans. In addition, based on the current program evaluation results and related program data, MH workload and staffing guidelines were developed for VHA HBPC programs nationally. The guidelines provide for approximately 10–15 clinical contact hours per week, in person or via telephone, for a MH provider assigned full time to HBPC. The guidelines also recommend staffing one full-time MH provider per HBPC program ADC of 120–140 patients and note that some programs, such as those in highly rural areas, will require greater MH capacity (e.g., one full-time MH provider per 100 ADC). These staffing guidelines will likely be helpful to the increasing number of expanding HBPC programs that have seen their ADCs grow significantly since the initial development of the HBPC MH initiative.
Finally, just as the overall HBPC program has served as a successful model for providing health care for homebound older adults that is currently being tested within Medicare, the HBPC MH initiative may serve as a useful—and timely—example to other health care systems (and the Medicare Program, in particular) for providing MH care to homebound older individuals and for reducing enduring, high rates of unmet MH need among the elderly adults. Significantly, the implementation of MH parity in Medicare, which will be fully phased in by 2014, will increase financial access to psychological services for many Medicare beneficiaries and will place renewed emphasis on—and provide new opportunities for—increased MH care provision with older individuals.
Funding
This project was supported by Mental Health Services, U.S. Department of Veterans Affairs Central Office .
Acknowledgments
Portions of this article were presented at the 65th Annual Scientific Meeting of the Gerontological Society of America (November 2012), San Diego, CA. The authors would like to thank Jocelyn Shealy McGee, PhD, Thomas Edes, MD, Peggy Becker, LCSW, and Antonette Zeiss, PhD, for their support and leadership related to the VA HBPC MH initiative.
References
Author notes
Decision Editor: Kimberly Van Haitsma, PhD