-
PDF
- Split View
-
Views
-
Cite
Cite
McVin Hua Heng Cheen, Chong Ping Goon, Wan Chee Ong, Paik Shia Lim, Choon Nam Wan, Mei Yan Leong, Giat Yeng Khee, Evaluation of a care transition program with pharmacist-provided home-based medication review for elderly Singaporeans at high risk of readmissions, International Journal for Quality in Health Care, Volume 29, Issue 2, April 2017, Pages 200–205, https://doi.org/10.1093/intqhc/mzw150
Close - Share Icon Share
Abstract
This study aimed to determine whether pharmacist-provided home-based medication review (HBMR) can reduce readmissions in the elderly.
Retrospective cohort study.
Patient's home.
Records of patients referred to a care transition program from March 2011 through March 2015 were reviewed. Patients aged 60 years and older taking more than 5 medications and had at least 2 unplanned admissions within 3 months preceding the first home visit were included.
Pharmacist-provided HBMR.
Primary outcome was readmission rate over 6 months after the first home visit. Secondary outcomes included emergency department (ED) visits, outpatient visits and mortality. Drug-related problems (DRPs) were reported for the HBMR group. Multivariate incidence rate ratios (IRR) and hazard ratio (HR) were calculated with adjustments for covariates.
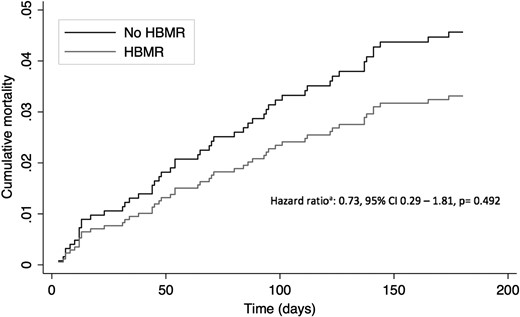
The study included 499 patients (97 HBMR, 402 no HBMR). Pharmacist-provided HBMR reduced readmissions by 26% (IRR = 0.74, 95% CI: 0.59–0.92, P = 0.007), reduced ED visits by 20% (IRR = 0.80, 95% CI: 0.66–0.98, P = 0.030) and increased outpatient visits by 16% (IRR = 1.16, 95% CI: 0.95–1.41, P = 0.150). There were 8 and 44 deaths in the HBMR and no HBMR groups respectively (HR = 0.73, 95% CI: 0.29–1.81, P = 0.492). Pharmacists identified 464 DRPs, with 169 (36.4%) resolved within 1 month after the home visit.
The study suggests that pharmacist-provided HBMR is effective in reducing readmissions and ED visits in the elderly. More studies in the Asian population are needed to determine its long term benefits and patient's acceptability.
Introduction
Hospital readmission is one of the serious post-discharge complications that can result in increased risk of morbidity and mortality [1–4]. In the United States (US), 3.3 million readmissions were reported in 2011, of which 1.8 million were contributed by the elderly, defined as adults aged 65 years and above [5]. In addition, it was reported that 1 in 6 elderly was readmitted within 30 days post-discharge. The situation is more worrying in Singapore, with 1 in 5 elderly being readmitted within 30 days post-discharge [6]. Managing readmissions in the elderly cost the US $24 billion annually [5], and this figure is likely to rise if kept unchecked.
Care transition programs have been implemented in different settings to reduce readmissions and improve patient outcomes with mixed results [7–10]. It has been consistently reported that drug-related problems (DRPs), defined as events or circumstances involving drug therapy that actually or potentially interfere with desired health outcomes [11], are one of the many factors associated with readmissions [12, 13]. These DRPs account for 5.6–20% of hospital readmissions [14–16], of which many are avoidable. This highlights the importance of pharmacists in stemming the rise in readmissions among the elderly through medication review. Conducting medication review in the patients’ home is likely to be convenient for the elderly patient and provides the opportunity to understand their medication taking behavior in their own environment. However, two randomized controlled trials conducted in the past decade—HOMER [17] and POLYMED [18], failed to demonstrate the benefits of pharmacist-provided home-based medication review (HBMR) on readmissions. HOMER reported a significantly higher risk of readmissions in the HBMR group. The patients included in the trial were taking an average of 6 medications daily, with no information on DRPs identified. In addition, pharmacists only received a 2-day training course prior to the home visits, and recommendations were communicated to the physicians by letters and occasional phone calls without further follow-up. These could have undermined the potential benefits of HBMR. POLYMED reported a non-significant reduction in hospital admissions. However, the trial included community-dwelling elderly who were considerably healthier than those in HOMER, and thus HBMR may not be beneficial. Furthermore, as the problem of readmission continues to grow, the provision of care transition has become standard of care, making comparison of HBMR to usual care less favorable in current practice.
A more targeted approach is necessary in order for the benefits of HBMR to be realized. This includes careful selection of patients, where only those at high risk for readmission and DRPs are chosen to receive HBMR. In addition, components of medication review that have been shown to improve outcomes (e.g. having access to detailed past medical history, medication records and closer liaison with physicians) should be included in HBMR [19, 20]. Thus, this study aimed to determine whether pharmacist-provided HBMR can improve outcomes of elderly Singaporeans at high risk of readmissions who were enrolled in a care transition program.
Methods
Study setting
This study involved patients enrolled into the Aged Care TransiTION (ACTION) program, a nationwide program initiated by the government to improve post-discharge outcomes [21]. Teams of care coordinators, who are nurses trained in care transition, are stationed at the various acute care hospitals to facilitate patients’ transition from hospital to their home and community. Pharmacists are involved in ACTION at Singapore General Hospital (SGH), a 1600-bed academic medical center, to help improve medication use among those enrolled into the program.
Study design and patient selection
This was a single-center, retrospective observational study of elderly patients referred to the ACTION program at SGH between 1st March 2011 and 31st March 2015. The study was reviewed and approved by the SingHealth Centralized Institutional Review Board (Reference no.: 2015/2493). Records of patients were reviewed and included if they met the criteria for high risk of DRPs and readmissions: aged 60 years and older, taking more than 5 medications and had at least 2 unplanned hospital admissions within 3 months preceding the first home visit. Patients enrolled in care transition programs other than ACTION were excluded. Patients visited by both the care coordinator and pharmacist were assigned to the ‘HBMR’ group, while those visited only by the care coordinator were assigned to the ‘no HBMR’ group.
Details of intervention
The details of the ACTION program have been described elsewhere [22]. Briefly, the program receives referrals from physicians during inpatient admission. Upon referral to the program, the care coordinator conducts a bedside interview to identify care issues that require post-discharge follow-up. Home visits were then conducted within 2 weeks of discharge to resolve outstanding care issues. Each week, a pharmacist will review the list of patients scheduled for home visits to identify and prioritize those at high risk of DRPs by reviewing the medication history, comorbidities, recent admissions and laboratory parameters. Examples of risk factors for DRPs include polypharmacy, renal and/or hepatic impairment, frequent hospital admissions and high comorbidity burden [23, 24]. The pharmacist then visits these patients together with the care coordinator. During the home visit, the pharmacist provides comprehensive medication review, disease management and medication counseling. Any DRPs identified will be resolved during the home visit wherever possible. In the event that a physician's involvement is necessary in order to resolve the DRP, the pharmacist will communicate the recommendations either via telephone calls or typewritten letters, and any unresolved DRPs will be followed until resolution.
Pharmacists conducting HBMR have to possess at least 1 year of experience in performing comprehensive medication review. In addition, they need to undergo a 6-week training by a pharmacist with experience in HBMR, which involves observation as well as conducting HBMR under supervision, before they are allowed to conduct HBMR independently.
Outcomes
The primary outcome was the incidence of readmissions over 6 months after the first home visit. Secondary outcomes included incidence of emergency department (ED) visits, outpatient visits, and mortality over 6 months after the first home visit. Additional secondary outcome for the HBMR group included DRPs identified and resolved by the pharmacists.
Data on patient demographics, clinical characteristics, healthcare utilization (i.e. readmissions, ED and outpatient visits) and mortality were obtained from SGH's electronic medical records and inpatient discharge summaries. Data on DRPs identified were obtained from a database managed by the pharmacists. The DRPs were classified using a modified Hepler and Strand classification scheme [25], with an additional ‘others’ category for DRPs that did not fall into any of the categories mentioned. In this study, DRPs that were not resolved after 1 month from the home visit were deemed unresolved.
Sample size calculation
A readmission rate of 1.6 per patient over 6 months was assumed for the no HBMR group, which was double the rate employed by the HOMER and POLYMED trials as this study focused on patients with a much higher baseline admission rate. This study aimed to demonstrate a 25% lower rate of readmissions in the HBMR group compared with no HBMR. This was a reasonable effect size as suggested by previous studies [17, 18, 26]. Using a normal approximation to the Poisson distribution and a ratio of 1 HBMR:4 no HBMR due to the anticipated smaller numbers in the HBMR group, it was estimated that 450 patients were required (i.e. 90 HBMR, 360 no HBMR) to detect the 25% reduction in readmissions with 80% statistical power at the 5% significance level.
Statistical analysis
Patient demographics and clinical characteristics were summarized using descriptive statistics. Categorical variables were compared using χ2 or Fisher's exact tests, continuous variables were compared using two-sample t-test and count variables were compared using univariate Poisson regression. All-cause unplanned readmissions, ED and outpatient visits were compared between groups using Poisson regression and reported as incidence rate ratios (IRR). Cox proportional hazards model was used to compare mortality between groups and reported as hazard ratio (HR). The regression analyses were adjusted for covariates. All analyses were performed using Stata SE 13.2 (StataCorp, College Station, TX: StataCorp LP.) at the 5% significance level.
Results
Patient demographics and clinical characteristics
A total of 4210 patients were enrolled into the ACTION program during the study period, out of which 499 (97 HBMR and 402 no HBMR) met the study's inclusion criteria and were analyzed.
Patient demographics and clinical characteristics are detailed in Table 1. Age, gender and ethnic distributions were comparable between groups. Patients in both groups had high comorbidity burden as indicated by the Charlson comorbidity index (6.8 ± 2.3 vs. 6.4 ± 2.4, P = 0.226). Notably, patients in the HBMR group had a significantly higher baseline hospital admission rate (2.80 vs. 2.42, P = 0.032) and were taking more medications (14.9 ± 4.3 vs. 9.8 ± 3.3, P < 0.001) compared with the no HBMR group. The proportion of patients who were visited more than once were higher in the HBMR group compared with the no HBMR group (50.5 vs. 14.2%, P < 0.001).
Demographics and clinical characteristics of patients included in the analysis
| Characteristics . | HBMR (n = 97) . | No HBMR (n = 402) . | P value . |
|---|---|---|---|
| Age, mean (SD) years | 73.6 (8.7) | 74.8 (10.9) | 0.345 |
| Gender, n (%) | 0.510 | ||
| Male | 48 (49.5) | 184 (45.8) | |
| Female | 49 (50.5) | 218 (54.2) | |
| Ethnicity, n (%) | 0.397 | ||
| Chinese | 81 (83.5) | 327 (81.3) | |
| Malay | 4 (4.1) | 36 (9.0) | |
| Indian | 10 (10.3) | 31 (7.7) | |
| Others | 2 (2.1) | 8 (2.0) | |
| Charlson comorbidity index, mean (SD) | 6.8 (2.3) | 6.4 (2.4) | 0.226 |
| Baseline hospital admission rate, 3 months preceding index visit | 2.80 | 2.42 | 0.032 |
| Total medications, mean (SD) | 14.9 (4.3) | 9.8 (3.3) | <0.001 |
| Duration of follow up, mean (SD) days | 170 (35) | 168 (38) | 0.555 |
| Number of visits conducted, median (IQR) | 2 (1 – 4) | 1 (1 – 3) | <0.001 |
| Number of visits conducted per patient, n (%) | <0.001 | ||
| 1 | 48 (49.5) | 345 (85.8) | |
| 2 | 33 (34.0) | 43 (10.7) | |
| 3 | 11 (11.3) | 11 (2.7) | |
| 4 | 4 (4.1) | 2 (0.5) | |
| 5 | 1 (1.1) | 1 (0.3) |
| Characteristics . | HBMR (n = 97) . | No HBMR (n = 402) . | P value . |
|---|---|---|---|
| Age, mean (SD) years | 73.6 (8.7) | 74.8 (10.9) | 0.345 |
| Gender, n (%) | 0.510 | ||
| Male | 48 (49.5) | 184 (45.8) | |
| Female | 49 (50.5) | 218 (54.2) | |
| Ethnicity, n (%) | 0.397 | ||
| Chinese | 81 (83.5) | 327 (81.3) | |
| Malay | 4 (4.1) | 36 (9.0) | |
| Indian | 10 (10.3) | 31 (7.7) | |
| Others | 2 (2.1) | 8 (2.0) | |
| Charlson comorbidity index, mean (SD) | 6.8 (2.3) | 6.4 (2.4) | 0.226 |
| Baseline hospital admission rate, 3 months preceding index visit | 2.80 | 2.42 | 0.032 |
| Total medications, mean (SD) | 14.9 (4.3) | 9.8 (3.3) | <0.001 |
| Duration of follow up, mean (SD) days | 170 (35) | 168 (38) | 0.555 |
| Number of visits conducted, median (IQR) | 2 (1 – 4) | 1 (1 – 3) | <0.001 |
| Number of visits conducted per patient, n (%) | <0.001 | ||
| 1 | 48 (49.5) | 345 (85.8) | |
| 2 | 33 (34.0) | 43 (10.7) | |
| 3 | 11 (11.3) | 11 (2.7) | |
| 4 | 4 (4.1) | 2 (0.5) | |
| 5 | 1 (1.1) | 1 (0.3) |
Demographics and clinical characteristics of patients included in the analysis
| Characteristics . | HBMR (n = 97) . | No HBMR (n = 402) . | P value . |
|---|---|---|---|
| Age, mean (SD) years | 73.6 (8.7) | 74.8 (10.9) | 0.345 |
| Gender, n (%) | 0.510 | ||
| Male | 48 (49.5) | 184 (45.8) | |
| Female | 49 (50.5) | 218 (54.2) | |
| Ethnicity, n (%) | 0.397 | ||
| Chinese | 81 (83.5) | 327 (81.3) | |
| Malay | 4 (4.1) | 36 (9.0) | |
| Indian | 10 (10.3) | 31 (7.7) | |
| Others | 2 (2.1) | 8 (2.0) | |
| Charlson comorbidity index, mean (SD) | 6.8 (2.3) | 6.4 (2.4) | 0.226 |
| Baseline hospital admission rate, 3 months preceding index visit | 2.80 | 2.42 | 0.032 |
| Total medications, mean (SD) | 14.9 (4.3) | 9.8 (3.3) | <0.001 |
| Duration of follow up, mean (SD) days | 170 (35) | 168 (38) | 0.555 |
| Number of visits conducted, median (IQR) | 2 (1 – 4) | 1 (1 – 3) | <0.001 |
| Number of visits conducted per patient, n (%) | <0.001 | ||
| 1 | 48 (49.5) | 345 (85.8) | |
| 2 | 33 (34.0) | 43 (10.7) | |
| 3 | 11 (11.3) | 11 (2.7) | |
| 4 | 4 (4.1) | 2 (0.5) | |
| 5 | 1 (1.1) | 1 (0.3) |
| Characteristics . | HBMR (n = 97) . | No HBMR (n = 402) . | P value . |
|---|---|---|---|
| Age, mean (SD) years | 73.6 (8.7) | 74.8 (10.9) | 0.345 |
| Gender, n (%) | 0.510 | ||
| Male | 48 (49.5) | 184 (45.8) | |
| Female | 49 (50.5) | 218 (54.2) | |
| Ethnicity, n (%) | 0.397 | ||
| Chinese | 81 (83.5) | 327 (81.3) | |
| Malay | 4 (4.1) | 36 (9.0) | |
| Indian | 10 (10.3) | 31 (7.7) | |
| Others | 2 (2.1) | 8 (2.0) | |
| Charlson comorbidity index, mean (SD) | 6.8 (2.3) | 6.4 (2.4) | 0.226 |
| Baseline hospital admission rate, 3 months preceding index visit | 2.80 | 2.42 | 0.032 |
| Total medications, mean (SD) | 14.9 (4.3) | 9.8 (3.3) | <0.001 |
| Duration of follow up, mean (SD) days | 170 (35) | 168 (38) | 0.555 |
| Number of visits conducted, median (IQR) | 2 (1 – 4) | 1 (1 – 3) | <0.001 |
| Number of visits conducted per patient, n (%) | <0.001 | ||
| 1 | 48 (49.5) | 345 (85.8) | |
| 2 | 33 (34.0) | 43 (10.7) | |
| 3 | 11 (11.3) | 11 (2.7) | |
| 4 | 4 (4.1) | 2 (0.5) | |
| 5 | 1 (1.1) | 1 (0.3) |
Primary outcome
Table 2 details the results of the analysis of readmissions. Both groups saw a decline in readmission rates over 6 months after the first home visit as compared with baseline. Analysis using the Poisson regression model demonstrated a 26% reduction in readmissions in the HBMR group after adjusting for covariates (IRR = 0.74, 95% CI: 0.59–0.92, P = 0.007).
Comparison of incidence of hospital readmissions, emergency department and outpatient visits over 6 months after the first home visit
| Outcome measure . | Incidence (95% CI) . | Incidence rate ratioa (95% CI) . | P valuea . | |
|---|---|---|---|---|
| HBMR (n = 97) . | No HBMR (n = 402) . | |||
| Hospital readmissions | 1.22 (1.00–1.45) | 1.66 (1.51–1.80) | 0.74 (0.59–0.92) | 0.007 |
| Emergency department visits | 1.48 (1.24–1.71) | 1.84 (1.68–2.00) | 0.80 (0.66–0.98) | 0.030 |
| Outpatient visits | 2.10 (1.74–2.46) | 1.81 (1.68–1.95) | 1.16 (0.95–1.41) | 0.150 |
| Outcome measure . | Incidence (95% CI) . | Incidence rate ratioa (95% CI) . | P valuea . | |
|---|---|---|---|---|
| HBMR (n = 97) . | No HBMR (n = 402) . | |||
| Hospital readmissions | 1.22 (1.00–1.45) | 1.66 (1.51–1.80) | 0.74 (0.59–0.92) | 0.007 |
| Emergency department visits | 1.48 (1.24–1.71) | 1.84 (1.68–2.00) | 0.80 (0.66–0.98) | 0.030 |
| Outpatient visits | 2.10 (1.74–2.46) | 1.81 (1.68–1.95) | 1.16 (0.95–1.41) | 0.150 |
aAdjusted for age, gender, ethnicity, Charlson comorbidity index, total medications, baseline hospital admission rate, total number of home visits conducted and follow-up duration
Comparison of incidence of hospital readmissions, emergency department and outpatient visits over 6 months after the first home visit
| Outcome measure . | Incidence (95% CI) . | Incidence rate ratioa (95% CI) . | P valuea . | |
|---|---|---|---|---|
| HBMR (n = 97) . | No HBMR (n = 402) . | |||
| Hospital readmissions | 1.22 (1.00–1.45) | 1.66 (1.51–1.80) | 0.74 (0.59–0.92) | 0.007 |
| Emergency department visits | 1.48 (1.24–1.71) | 1.84 (1.68–2.00) | 0.80 (0.66–0.98) | 0.030 |
| Outpatient visits | 2.10 (1.74–2.46) | 1.81 (1.68–1.95) | 1.16 (0.95–1.41) | 0.150 |
| Outcome measure . | Incidence (95% CI) . | Incidence rate ratioa (95% CI) . | P valuea . | |
|---|---|---|---|---|
| HBMR (n = 97) . | No HBMR (n = 402) . | |||
| Hospital readmissions | 1.22 (1.00–1.45) | 1.66 (1.51–1.80) | 0.74 (0.59–0.92) | 0.007 |
| Emergency department visits | 1.48 (1.24–1.71) | 1.84 (1.68–2.00) | 0.80 (0.66–0.98) | 0.030 |
| Outpatient visits | 2.10 (1.74–2.46) | 1.81 (1.68–1.95) | 1.16 (0.95–1.41) | 0.150 |
aAdjusted for age, gender, ethnicity, Charlson comorbidity index, total medications, baseline hospital admission rate, total number of home visits conducted and follow-up duration
Secondary outcomes
Analysis of mortality over 6 months after the first home visit.
Table 3 summarizes the various types of DRPs identified in the HBMR group. Pharmacists identified a total of 464 DRPs, corresponding to an average of about 5 DRPs per patient. The most commonly identified DRPs were non-adherence (38.6%), untreated indication (22.4%) and overdosage (9.9%). Pharmacists resolved 36.4% of DRPs within 1 month of the home visit.
Drug-related problems identified by pharmacists
| Drug-related problems . | n (%) . |
|---|---|
| Total identified | 464 |
| Mean (SD) | 4.9 (3.4) |
| Categories | |
| Non-adherence | 179 (38.6) |
| Untreated indication | 104 (22.4) |
| Overdosage | 46 (9.9) |
| Improper selection | 37 (8.0) |
| No indication | 33 (7.1) |
| Underdosage | 27 (5.8) |
| Adverse reaction | 19 (4.1) |
| Interactions | 6 (1.3) |
| Others | 13 (2.8) |
| Resolved | 169 (36.4) |
| Drug-related problems . | n (%) . |
|---|---|
| Total identified | 464 |
| Mean (SD) | 4.9 (3.4) |
| Categories | |
| Non-adherence | 179 (38.6) |
| Untreated indication | 104 (22.4) |
| Overdosage | 46 (9.9) |
| Improper selection | 37 (8.0) |
| No indication | 33 (7.1) |
| Underdosage | 27 (5.8) |
| Adverse reaction | 19 (4.1) |
| Interactions | 6 (1.3) |
| Others | 13 (2.8) |
| Resolved | 169 (36.4) |
Drug-related problems identified by pharmacists
| Drug-related problems . | n (%) . |
|---|---|
| Total identified | 464 |
| Mean (SD) | 4.9 (3.4) |
| Categories | |
| Non-adherence | 179 (38.6) |
| Untreated indication | 104 (22.4) |
| Overdosage | 46 (9.9) |
| Improper selection | 37 (8.0) |
| No indication | 33 (7.1) |
| Underdosage | 27 (5.8) |
| Adverse reaction | 19 (4.1) |
| Interactions | 6 (1.3) |
| Others | 13 (2.8) |
| Resolved | 169 (36.4) |
| Drug-related problems . | n (%) . |
|---|---|
| Total identified | 464 |
| Mean (SD) | 4.9 (3.4) |
| Categories | |
| Non-adherence | 179 (38.6) |
| Untreated indication | 104 (22.4) |
| Overdosage | 46 (9.9) |
| Improper selection | 37 (8.0) |
| No indication | 33 (7.1) |
| Underdosage | 27 (5.8) |
| Adverse reaction | 19 (4.1) |
| Interactions | 6 (1.3) |
| Others | 13 (2.8) |
| Resolved | 169 (36.4) |
Discussion
As the population continues to age, the demand for healthcare resources will continue to increase. Care transition programs with pharmacist-provided HBMR have gained traction in Singapore in an effort to reduce unnecessary readmissions and conserve healthcare resources. This study suggests that HBMR can reduce readmissions in the high risk elderly. It addressed some of the limitations of previously published studies and provided insights to the effectiveness of this service in the Asian population. Being in Southeast Asia where patient safety and quality of care transition is a problem among the developing countries in the region [27], this study forms the basis for the development of new models of care to help patients make safe transitions between healthcare settings. In addition, the duration of outcomes assessment was 6 months as compared with recent studies that reported 30-day readmission rates [7, 28–30]. The longer duration adopted in this study was appropriate as the benefits of HBMR was unlikely to be realized immediately, since the effects of the optimization of pharmacotherapy can only be seen much later.
The findings of this study contradict that of HOMER and POLYMED that reported HBMR was no better than usual care, and may result in increased risk of readmissions. However, there were limitations in the trial design that could have influenced the study findings. In addition, important information necessary to interpret the findings was not explicitly stated in these trials. These will be elaborated in the following paragraphs.
First, this study adopted a more stringent criterion to identify elderly patients at high risk for readmissions and DRPs compared with HOMER and POLYMED. The significant findings suggest that the benefits of pharmacist-provided HBMR can be realized among the high risk patients. Resolving DRPs, improving medication management and achieving therapy goals could have reduced readmissions and improved outcomes in this group of patients to a greater extent as compared with those at lower risk. The possible inclusion of low risk patients in HOMER and POLYMED could have diluted the benefits of HBMR, resulting in the non-significant findings.
Second, pharmacists involved in HBMR had to undergo rigorous training in the provision of medication review services. This was necessary because patients selected for HBMR often have multiple comorbidities, high prevalence of polypharmacy and medication management issues. Improving the outcomes of these patients will require extensive pharmacotherapy knowledge as well as clinical experience in identifying and resolving DRPs. This was in contrast with that of HOMER, where pharmacists only underwent a 2-day training course prior to conducting HBMR.
Third, care coordinators were involved in the management of the patients in both groups. This would have minimized any social or care issues that predispose patients to unnecessary readmissions, allowing for a more robust evaluation of the benefits of HBMR. However, it was unclear if the pharmacists in HOMER and POLYMED addressed the social factors of readmissions. While they could have resolved DRPs, the unresolved social or care issues might have resulted in readmissions and mitigated the benefits of HBMR.
Fourth, this study reported the types of DRPs identified by pharmacists, including the proportion resolved at 1 month after the home visit. This was in line with a recent review that recommended future studies to report DRPs to better evaluate the impact of medication reviews [31]. In contrast, only medication adherence was reported in HOMER and POLYMED, and it was not known if DRPs were prevalent among the study participants. A low DRP prevalence could have limited the effectiveness of HBMR.
There was a non-significant increase in outpatient visits in the HBMR group. This could be due to patient's better understanding of their medical conditions and medications that resulted in timely follow-up at the outpatient clinic. In addition, pharmacists could have initiated early physician referrals to address DRPs that require a physician's attention. Therefore, the increase in outpatient visits could have contributed to the reduction in readmissions in the HBMR group. Since the cost of outpatient visits is generally lower than that of hospital admissions, and the benefits of reduced readmissions outweigh the inconvenience of more frequent outpatient visits, the slight increase in outpatient visits is potentially an acceptable tradeoff to both patients and providers.
The proportion of DRPs that remained unresolved warrants attention. In this study, 65.4% of DRPs remained unresolved at 1 month. Given that each patient had 5 DRPs identified on average, pharmacists had to prioritize the DRPs that required urgent attention. These DRPs often had direct impact on patient outcomes such as risk for readmission. For example, the caregiver of a patient on nasogastric tube feeding was serving dabigatran by opening the capsules, which can result in increased bioavailability and thus increased risk of bleeding. This was identified by the pharmacist during HBMR and a recommendation was made to switch to warfarin. In another example, the pharmacist identified overdosage of warfarin by the patient, and an immediate referral was made to the outpatient clinic for coagulation monitoring and warfarin was held off temporarily due to overanticoagulation. The remaining DRPs, though unresolved at 1 month, may not adversely affect readmissions if left unresolved until a later date. For these non-urgent DRPs, the pharmacist would write a letter detailing the DRPs identified and recommendations, and this would be handed to the physician during the patient's next outpatient visit. Subsequent outpatient visits often occurred after the 1-month time frame, resulting in these DRPs being classified as unresolved in this study. However, pharmacists actively followed up on these DRPs to ensure that they were either resolved or brought to the physician's attention, but this information was not available due to the retrospective nature of the study. In addition, poor medication adherence was prevalent among patients in the HBMR group. Overcoming poor medication adherence in the elderly is challenging compared with the younger adults. Barriers to medication adherence including living alone, low health literacy, lack of perceived need for medication and cost of medication require time and involvement of other healthcare professionals to overcome. Therefore, it was unlikely to see improvement in medication adherence within a short period of time.
There are limitations to this study. First, while the same study criterion was applied to both groups, selection bias could not be eliminated due to the retrospective nature of the study. For example, information on DRPs in the no HBMR group was not available, so potential imbalance in risk for readmissions could not be excluded. However, extensive covariates adjustment was performed for all regression analyses to minimize confounding. Second, pharmacists conducted only 1 home visit per patient, and subsequent visits were conducted by the care coordinators. Thus, the benefits observed in this study may not be sustainable if pharmacists do not conduct follow-up HBMR due to changes in patients’ disease status and medications. Third, the study included only a small proportion of patients enrolled into ACTION (499 of 4210 patients), as many were enrolled predominantly due to social or care issues where HBMR was unlikely to beneficial. Caution should be exercised when integrating HBMR into transition care programs.
Conclusions
This study suggests that pharmacist-provided HBMR for high risk elderly Singaporeans decreased readmissions and ED visits. Mortality benefit is unclear, though there was a trend towards reduced mortality among those who received HBMR. More studies in the Asian population are needed to determine the long-term benefits and patient's acceptability.
Acknowledgement
The authors would like to thank the ACTION care coordinators and pharmacists. They would also like to acknowledge Weiqing Chen for his assistance in obtaining information from the electronic medical records.
Funding
None.