-
PDF
- Split View
-
Views
-
Cite
Cite
Matthew J. Smith, William P. Horan, Derin J. Cobia, Tatiana M. Karpouzian, Jaclyn M. Fox, James L. Reilly, Hans C. Breiter, Performance-Based Empathy Mediates the Influence of Working Memory on Social Competence in Schizophrenia, Schizophrenia Bulletin, Volume 40, Issue 4, July 2014, Pages 824–834, https://doi.org/10.1093/schbul/sbt084
Close - Share Icon Share
Abstract
Empathic deficits have been linked to poor functioning in schizophrenia, but this work is mostly limited to self-report data. This study examined whether performance-based empathy measures account for incremental variance in social competence and social attainment above and beyond self-reported empathy, neurocognition, and clinical symptoms. Given the importance of working memory in theoretical models of empathy and in the prediction of functioning in schizophrenia, we also examined whether empathy mediates the relationship between working memory and functioning. Sixty outpatients and 45 healthy controls were compared on performance-based measures of 3 key components of empathic responding, including facial affect perception, emotional empathy (affective responsiveness), and cognitive empathy (emotional perspective-taking). Participants also completed measures of self-reported empathy, neurocognition, clinical symptoms, and social competence and attainment. Patients demonstrated lower accuracy than controls across the 3 performance-based empathy measures. Among patients, these measures showed minimal relations to self-reported empathy but significantly correlated with working memory and other neurocognitive functions as well as symptom levels. Furthermore, cognitive empathy explained significant incremental variance in social competence (∆R2 = .07, P < .05) and was found to mediate the relation between working memory and social competence. Performance-based measures of empathy were sensitive to functionally relevant disturbances in schizophrenia. Working memory deficits appear to have an important effect on these disruptions in empathy. Empathy is emerging as a promising new area for social cognitive research and for novel recovery-oriented treatment development.
Introduction
A substantial literature indicates that neurocognitive deficits contribute to schizophrenia patients’ poor functioning.1–8 For example, working memory (WM) deficits have been extensively documented in schizophrenia9–11 and show consistent relations to poor functioning.12–17 More recent evidence highlights the unique functional relevance of social cognitive impairments and how they interact with neurocognitive deficits to impact functioning. Social cognitive deficits appear to correlate more strongly with functioning than neurocognitive impairments,18 to explain unique variance in functioning,19–23 and even mediate the relationship between neurocognitive impairment and functioning.24–29 Although these findings demonstrate social cognition’s “added value” for identifying novel recovery-oriented treatment targets, most studies have focused on a narrow range of social cognitive domains, particularly affect perception and basic Theory of Mind.18,19 In addition, theory-based models of how specific social cognitive and neurocognitive processes interact to impact functioning are rare. The current study addressed these issues by evaluating the functional significance of empathy, a key social cognitive process that has received limited attention in schizophrenia.
Empathy has been extensively studied in social cognitive neuroscience and is regarded as critical for adaptive functioning.30–33 Empathy is a multidimensional construct that can be broadly defined as sharing and understanding the same emotional experiences as others.34 Empathic processes involved in evaluating and responding to others’ emotions in real-time are believed to interact closely and recursively with basic neurocognitive functions.35,36 According to Zaki and Ochsner,37 empathic accuracy involves the ability to cognitively process the behaviors and emotional cues (eg, via facial and vocal expression) displayed by others during interactions. These processes, in turn, feed into “emotional” and “cognitive” empathy subcomponents.37,38 Emotional empathy involves simulating and sharing others’ emotions, while cognitive empathy involves understanding the emotional perspective of others and separating one’s own feelings from the experiences of others.39
Among the neurocognitive processes required for empathic responding, interactions with WM are particularly relevant. Social interactions require the capacity to flexibly maintain and incorporate information about fluctuating social cues, one’s own emotional state, and schema-based knowledge about social norms. The importance of WM draws support from recent evidence that social WM-based neural activation correlates with cognitive empathy.40 Impaired empathy has also been observed following lesions of the dorsolateral prefrontal cortex,41 a region associated with a larger distributed network supporting WM.42,43 The role of WM in empathy may be particularly relevant for schizophrenia given recent speculation that WM plays a critical role in abnormal cognition-emotion interactions. For example, Gold, Strauss, and colleagues have proposed that WM deficits disrupt key processes such as maintaining representations of reward value and decision-making in schizophrenia,44–46 which could also be expected to impact empathic processes.
Research on empathy in schizophrenia is sparse and largely based on self-report questionnaires, which suggest that patients report disturbances in both cognitive and emotional empathy.47–50 The one study that examined the functional correlates of self-reported empathy found that cognitive empathy explained unique variance in social competence (ie, performance-based social simulations that index one’s abilities under controlled conditions) and social attainment (ie, interview-based assessments of what one actually does in the community) above and beyond neurocognition and symptoms.49 Although these studies shed light on how patients view their own empathic abilities, less is known about how patients actually perform on tasks designed to measure empathic processes.
A few studies using performance-based tasks reported impairment in global empathic accuracy48 or one particular aspect of emotional51–53 or cognitive52,54 empathy in schizophrenia. Derntl et al52 in Germany developed a paradigm to assess 3 core components required for empathic responding: facial affect perception, affective responsiveness (emotional empathy), and emotional perspective-taking (cognitive empathy). They found that a mixed sample (n = 24) of inpatients and outpatients performed worse than controls across all 3 components. In addition, affective responsiveness and emotional perspective-taking showed somewhat different relations to scores from a brief neuropsychological battery but were generally unrelated to self-reported empathy. Further validation of performance-based empathy measures (ie, behavioral paradigms that index performance accuracy), particularly with regard to prediction of functioning, would be very useful as endpoints in clinical trials of new social cognitive treatments and as platforms for developing neuroimaging tasks.
The current study examined an adapted version of Derntl and colleagues’ empathy paradigm and its relations to self-reported empathy, neurocognition, symptoms, and functioning in community-dwelling outpatients with schizophrenia.52 Building on initial findings,52 we hypothesized that (1) schizophrenia patients would demonstrate impaired performance on an English language version of Derntl’s empathy paradigm; (2) performance-based empathy would significantly relate to self-reported empathy, neurocognition (particularly WM), and symptoms among schizophrenia patients; (3) performance-based empathy would account for unique incremental variance in functioning (ie, social competence and social attainment) among schizophrenia patients; and (4) performance-based empathy would mediate the relation between WM and functioning.
Methods
Participants
Participants were recruited through the Northwestern University Schizophrenia Research Group and included 60 schizophrenia patients and 45 healthy control subjects. Patients were also recruited through outpatient mental health services, advertisements in surrounding neighborhoods, the National Alliance for Mental Illness, and online. A diagnosis of schizophrenia (not schizoaffective disorder) was required for study participation and determined through the Structured Clinical Interview for the DSM-IV (SCID)55 and validated by a semistructured interview performed by a research psychiatrist. Patients were clinically stable prior to study participation and treated with antipsychotic medications.
Healthy controls were recruited through advertisements in neighborhoods near service providers and online. Exclusion criteria included having (1) a lifetime history of any Axis I psychiatric disorder according to SCID criteria, (2) a first-degree relative with a psychotic disorder (including bipolar disorder), or (3) met DSM-IV criteria for mental retardation. Additional exclusion criteria for both groups were: DSM-IV criteria for substance abuse or dependence within the past 6 months or a documented neurological injury or disorder. Northwestern University Feinberg School of Medicine’s Institutional Review Board approved the study protocol and all participants provided informed consent.
Measures
Performance-Based Measure of Empathy.
An adapted version of the Derntl et al52 paradigm included 3 computerized tasks that assess: facial affect perception, affective responsiveness (emotional empathy), and emotional perspective-taking (cognitive empathy). The developers translated the directions and tasks from German into English and worked with the principal investigator (MJS) to edit the text for readability. Each task used a 2-alternative, forced-choice response format with standardized face stimuli.56 Accuracy (ie, percent correct) and reaction times (RT) were recorded for each task. Sample stimuli from the 3 tasks are presented in online Supplementary Data. The accuracy scores on these measures were used to index ‘performance-based’ empathy.
Facial Affect Perception.
This task presented 30 faces displaying happiness, sadness, fear, disgust, anger, and neutrality (5 each). Participants were asked to select the appropriate emotional expression from 2 emotion labels (a correct option and a randomized option) presented on each side of the face for a maximum of 5 seconds.
Affective Responsiveness.
Participants judged how they would feel in various emotional scenarios presented as 150 brief sentences describing emotional (ie, happiness, sadness, anger, fear, disgust) and neutral situations (25 stimuli per emotion). The sentences were presented for 6 seconds and a response slide displaying 2 emotional faces was presented for a maximum of 4 seconds. Participants selected the emotional expression that reflected how they would feel in the scenario; one face correctly depicted how most people would feel in the scenario and the other face was a randomized option.
Emotional Perspective-Taking.
Participants were shown 60 scenes of 2 actors engaged in social interactions depicting the 5 aforementioned emotions and neutrality (10 scenes each). The face of one actor was masked and participants were asked to select which of the 2 faces reflected how the masked character would feel in each interaction. Each scene was displayed for 4 seconds followed by a response slide that presented 2 faces for a maximum of 4 seconds.
Self-report Measures of Empathy
The 28-item Interpersonal Reactivity Index (IRI)57 was used to measure 4 areas theorized to reflect cognitive and emotional aspects of empathy: fantasy (shifting one’s feelings to fictional characters), perspective-taking (understanding the perspective of others), empathic concern (generating affective concern for others), and personal distress (becoming upset when others are in difficult situations). Standardized scores were computed for each subscale using sample means and SDs.
Neurocognitive Assessments
Neurocognition was measured by combining scores from a battery of neuropsychological tests that approximate the measures representing the 6 nonsocial cognitive domains measured in the Measurement and Treatment Initiative to Improve Cognition in Schizophrenia battery.58 “Speed of processing” included Trail Making Test Part A,59 category fluency (animals),60 and the Digit-Symbol Coding subtest from the Wechsler Adult Intelligence Scale-Third Edition (WAIS-III).61 “Attention” included the mean across the 2, 3, and 4-item d-prime scores from a continuous performance task.62 “Verbal WM” included performance on Letter-Number Sequencing and Digit Span subtests from the Wechsler Memory Scale-Third Edition (WMS-III).63 “Nonverbal WM” included the Spatial Span subtest from the WMS-III.63 “Verbal learning” included the total score of trials 1-5 on the California Verbal Learning Test-Second Edition.64 “Reasoning and problem solving” included scores from the Matrix Reasoning subtest of the WAIS-III61 and the Trail Making Test Part B.59 Each domain was computed by standardizing raw or scaled scores from individual subtests using z-score transformations with the current sample, and then averaging these scores within the domains.
Clinical Symptom Assessments
Positive, negative, and disorganized symptom domain scores were calculated using global ratings from the Scale for the Assessment of Positive Symptoms65 and the Scale for the Assessment of Negative Symptoms.66 The method to compute the domain scores is described here.49
Assessments of Functioning
Two distinct aspects of functioning, social competence and social attainment, were assessed using recommended measures.67,68 “Social competence” was assessed using the Social Skills Performance Assessment, a video-recorded test comprised of 2 role-play scenes that involved meeting a new neighbor and making a request from a landlord.69 Based on the work of Patterson and colleagues,69 each scene was rated on a 5-point scale across 8 criteria for the first scene and 9 criteria for the second scene. A final score was calculated by averaging the 2 role-play scores (ICC = .97 for 2 blinded raters on 25% of the videos). “Social attainment” was assessed using the total score from a participant interview version of the Specific Levels of Functioning (SLOF) scale, which measures interpersonal relationships, social acceptability, activities of daily living, and work skills.70
Data Analysis
Preliminary analyses of demographics used t-tests for continuous variables and X2 for categorical variables, and separate Multivariate Analyses of Variance (MANOVAs) evaluated group differences on the neurocognitive, symptom, and functioning measures. The primary research questions were evaluated in 4 stages: (1) Group differences across the empathy performance (accuracy and square-root transformed RT) and self-report measures were evaluated with separate Repeated Measures Analyses of Variance (RM-ANOVAs); (2) Within the schizophrenia group, relationships among the performance measures of empathy (accuracy), self-reported empathy, neurocognition, symptoms, and functioning were evaluated with Pearson correlations; (3) Hierarchical regression was used to examine whether empathy performance measures (that significantly correlated with either social competence or attainment) explained incremental variance (R2) in functioning after accounting for any self-reported empathy, neurocognitive, or clinical variables significantly correlated with functioning; (4) Building on the theoretical link between WM and empathy, and evidence that both relate to functioning in schizophrenia,18,49 we used the Preacher and Hayes71 bootstrapping technique to examine whether performance-based empathy mediated the relation between WM and functioning. This approach is robust to deviations from the assumption of normality that can occur in smaller samples.71
Results
Participant Characteristics
Patients and controls did not differ with respect to age, gender, parental socioeconomic status,72 or race (see table 1). Patients were chronically ill with a typical daily CPZ equivalent.73 Duration of illness correlated with social competence (r = −.32, P < .05), while the daily CPZ equivalent did not correlate with empathy or other measures (all P values >.10). MANOVAs revealed significant overall main effects for group across the 6 neurocognitive domain scores (F1,103 = 11.2, P < .001), the 3 domains of clinical symptoms (F1,103 = 112.1, P < .001), and the 2 measures of functioning (F1,83 = 33.9, P < .001). Patients demonstrated significantly worse scores on each measure (see table 1).
Demographic, Neurocognitive, and Clinical Characteristics of Study Sample
| . | CON (n = 45) . | SCZ (n = 60) . | χ2 /F Statistics . |
|---|---|---|---|
| Demographics | |||
| Mean age (SD) | 33.07 (8.87) | 35.36 (9.07) | −1.29 |
| Duration of illness, mean years (SD) | — | 14.40 (9.26) | — |
| Gender (% male) | 53.30 | 63.30 | 1.06 |
| Mean SES (SD)a | 26.91 (11.06) | 24.40 (12.06) | 1.06 |
| Race | |||
| % Caucasian | 48.90 | 43.30 | |
| % African American | 37.80 | 41.70 | 0.32 |
| % Other | 13.30 | 15.00 | |
| Chlorpromazine equivalent | — | 360.91 (220.45) | — |
| Neurocognitive domains | |||
| Speed of processing | .40 (.50) | −.30 (.68) | 34.08*** |
| Attention | .20 (.77) | −.16 (.57) | 7.43** |
| Verbal working memory | .46 (.84) | −.35 (.81) | 24.66*** |
| Nonverbal working memory | .47 (.89) | −.35 (.94) | 20.65*** |
| Verbal learning | .63 (.81) | −.47 (.86) | 44.11*** |
| Problem solving and reasoning | .39 (.72) | −.29 (.89) | 17.26*** |
| Clinical symptoms | |||
| Positive symptoms | −.81 (.07) | .61 (.88) | 116.92*** |
| Negative symptoms | −.88 (.09) | .66 (.57) | 324.52*** |
| Disorganized symptoms | −.63 (.12) | .47 (.76) | 91.91*** |
| Functioning measures | |||
| Social competenceb | 4.48 (.59) | 3.42 (.80) | 43.54*** |
| Social attainmentc | 142.15 (12.51) | 125.82 (11.81) | 37.15*** |
| . | CON (n = 45) . | SCZ (n = 60) . | χ2 /F Statistics . |
|---|---|---|---|
| Demographics | |||
| Mean age (SD) | 33.07 (8.87) | 35.36 (9.07) | −1.29 |
| Duration of illness, mean years (SD) | — | 14.40 (9.26) | — |
| Gender (% male) | 53.30 | 63.30 | 1.06 |
| Mean SES (SD)a | 26.91 (11.06) | 24.40 (12.06) | 1.06 |
| Race | |||
| % Caucasian | 48.90 | 43.30 | |
| % African American | 37.80 | 41.70 | 0.32 |
| % Other | 13.30 | 15.00 | |
| Chlorpromazine equivalent | — | 360.91 (220.45) | — |
| Neurocognitive domains | |||
| Speed of processing | .40 (.50) | −.30 (.68) | 34.08*** |
| Attention | .20 (.77) | −.16 (.57) | 7.43** |
| Verbal working memory | .46 (.84) | −.35 (.81) | 24.66*** |
| Nonverbal working memory | .47 (.89) | −.35 (.94) | 20.65*** |
| Verbal learning | .63 (.81) | −.47 (.86) | 44.11*** |
| Problem solving and reasoning | .39 (.72) | −.29 (.89) | 17.26*** |
| Clinical symptoms | |||
| Positive symptoms | −.81 (.07) | .61 (.88) | 116.92*** |
| Negative symptoms | −.88 (.09) | .66 (.57) | 324.52*** |
| Disorganized symptoms | −.63 (.12) | .47 (.76) | 91.91*** |
| Functioning measures | |||
| Social competenceb | 4.48 (.59) | 3.42 (.80) | 43.54*** |
| Social attainmentc | 142.15 (12.51) | 125.82 (11.81) | 37.15*** |
Note: SCZ, schizophrenia patients; CON, healthy control participants.
aCompleted by n = 41 CON and n = 58 SCZ.
bCompleted by n = 34 CON and n = 51 SCZ.
cCompleted by CON (n = 44).
***P < .001, **P < .01.
Demographic, Neurocognitive, and Clinical Characteristics of Study Sample
| . | CON (n = 45) . | SCZ (n = 60) . | χ2 /F Statistics . |
|---|---|---|---|
| Demographics | |||
| Mean age (SD) | 33.07 (8.87) | 35.36 (9.07) | −1.29 |
| Duration of illness, mean years (SD) | — | 14.40 (9.26) | — |
| Gender (% male) | 53.30 | 63.30 | 1.06 |
| Mean SES (SD)a | 26.91 (11.06) | 24.40 (12.06) | 1.06 |
| Race | |||
| % Caucasian | 48.90 | 43.30 | |
| % African American | 37.80 | 41.70 | 0.32 |
| % Other | 13.30 | 15.00 | |
| Chlorpromazine equivalent | — | 360.91 (220.45) | — |
| Neurocognitive domains | |||
| Speed of processing | .40 (.50) | −.30 (.68) | 34.08*** |
| Attention | .20 (.77) | −.16 (.57) | 7.43** |
| Verbal working memory | .46 (.84) | −.35 (.81) | 24.66*** |
| Nonverbal working memory | .47 (.89) | −.35 (.94) | 20.65*** |
| Verbal learning | .63 (.81) | −.47 (.86) | 44.11*** |
| Problem solving and reasoning | .39 (.72) | −.29 (.89) | 17.26*** |
| Clinical symptoms | |||
| Positive symptoms | −.81 (.07) | .61 (.88) | 116.92*** |
| Negative symptoms | −.88 (.09) | .66 (.57) | 324.52*** |
| Disorganized symptoms | −.63 (.12) | .47 (.76) | 91.91*** |
| Functioning measures | |||
| Social competenceb | 4.48 (.59) | 3.42 (.80) | 43.54*** |
| Social attainmentc | 142.15 (12.51) | 125.82 (11.81) | 37.15*** |
| . | CON (n = 45) . | SCZ (n = 60) . | χ2 /F Statistics . |
|---|---|---|---|
| Demographics | |||
| Mean age (SD) | 33.07 (8.87) | 35.36 (9.07) | −1.29 |
| Duration of illness, mean years (SD) | — | 14.40 (9.26) | — |
| Gender (% male) | 53.30 | 63.30 | 1.06 |
| Mean SES (SD)a | 26.91 (11.06) | 24.40 (12.06) | 1.06 |
| Race | |||
| % Caucasian | 48.90 | 43.30 | |
| % African American | 37.80 | 41.70 | 0.32 |
| % Other | 13.30 | 15.00 | |
| Chlorpromazine equivalent | — | 360.91 (220.45) | — |
| Neurocognitive domains | |||
| Speed of processing | .40 (.50) | −.30 (.68) | 34.08*** |
| Attention | .20 (.77) | −.16 (.57) | 7.43** |
| Verbal working memory | .46 (.84) | −.35 (.81) | 24.66*** |
| Nonverbal working memory | .47 (.89) | −.35 (.94) | 20.65*** |
| Verbal learning | .63 (.81) | −.47 (.86) | 44.11*** |
| Problem solving and reasoning | .39 (.72) | −.29 (.89) | 17.26*** |
| Clinical symptoms | |||
| Positive symptoms | −.81 (.07) | .61 (.88) | 116.92*** |
| Negative symptoms | −.88 (.09) | .66 (.57) | 324.52*** |
| Disorganized symptoms | −.63 (.12) | .47 (.76) | 91.91*** |
| Functioning measures | |||
| Social competenceb | 4.48 (.59) | 3.42 (.80) | 43.54*** |
| Social attainmentc | 142.15 (12.51) | 125.82 (11.81) | 37.15*** |
Note: SCZ, schizophrenia patients; CON, healthy control participants.
aCompleted by n = 41 CON and n = 58 SCZ.
bCompleted by n = 34 CON and n = 51 SCZ.
cCompleted by CON (n = 44).
***P < .001, **P < .01.
Performance-Based and Self-reported Empathy
Descriptive data are shown in table 2. For accuracy scores, a RM-ANOVA indicated significant main effects for group (F1,103 = 31.79, P < .001), with patients showing generally lower accuracy, and task (F1,103 = 44.07, P < .001), indicating that across groups, scores were highest for facial affect perception, intermediate for affective responsiveness, and lowest for emotional perspective-taking (all pairwise task comparisons, P < .001). In addition, a significant group-by-task interaction (F1,103 = 4.37, P < .001) indicated that although patients performed worse than controls on each measure (all P values < .01), the between-group difference for facial affect perception was smaller than the differences for emotional perspective-taking (t = 3.10, P < .01) and affective responsiveness (t = 2.36, P < .05), which did not significantly differ from each other (t = 1.09, P > .10).
Means and SDs for Empathy Measures
| . | CON (n = 45) . | SCZ (n = 60) . |
|---|---|---|
| Performance-based empathy | ||
| Facial affect perception (accuracy) | .91 (.08) | .85 (.11) |
| (Reaction time) | 1693.09 (368.29) | 2079.82 (480.70) |
| Affective responsiveness (accuracy) | .88 (.08) | .79 (.09) |
| (Reaction time) | 1250.05 (259.56) | 1550.23 (451.44) |
| Emotional perspective-taking (accuracy) | .84 (.08) | .74 (.10) |
| (Reaction time) | 1414.41 (261.94) | 1654.73 (349.92) |
| Self-reported empathy | ||
| IRI fantasy | .18 (1.01) | −.13 (.98) |
| IRI perspective-taking | .44 (.95) | −.33 (.91) |
| IRI empathic concern | .26 (.92) | −.19 (1.02) |
| IRI personal distress | −.47 (.83) | .35 (.97) |
| . | CON (n = 45) . | SCZ (n = 60) . |
|---|---|---|
| Performance-based empathy | ||
| Facial affect perception (accuracy) | .91 (.08) | .85 (.11) |
| (Reaction time) | 1693.09 (368.29) | 2079.82 (480.70) |
| Affective responsiveness (accuracy) | .88 (.08) | .79 (.09) |
| (Reaction time) | 1250.05 (259.56) | 1550.23 (451.44) |
| Emotional perspective-taking (accuracy) | .84 (.08) | .74 (.10) |
| (Reaction time) | 1414.41 (261.94) | 1654.73 (349.92) |
| Self-reported empathy | ||
| IRI fantasy | .18 (1.01) | −.13 (.98) |
| IRI perspective-taking | .44 (.95) | −.33 (.91) |
| IRI empathic concern | .26 (.92) | −.19 (1.02) |
| IRI personal distress | −.47 (.83) | .35 (.97) |
Abbreviations are explained in the first footnote to table 1.
Means and SDs for Empathy Measures
| . | CON (n = 45) . | SCZ (n = 60) . |
|---|---|---|
| Performance-based empathy | ||
| Facial affect perception (accuracy) | .91 (.08) | .85 (.11) |
| (Reaction time) | 1693.09 (368.29) | 2079.82 (480.70) |
| Affective responsiveness (accuracy) | .88 (.08) | .79 (.09) |
| (Reaction time) | 1250.05 (259.56) | 1550.23 (451.44) |
| Emotional perspective-taking (accuracy) | .84 (.08) | .74 (.10) |
| (Reaction time) | 1414.41 (261.94) | 1654.73 (349.92) |
| Self-reported empathy | ||
| IRI fantasy | .18 (1.01) | −.13 (.98) |
| IRI perspective-taking | .44 (.95) | −.33 (.91) |
| IRI empathic concern | .26 (.92) | −.19 (1.02) |
| IRI personal distress | −.47 (.83) | .35 (.97) |
| . | CON (n = 45) . | SCZ (n = 60) . |
|---|---|---|
| Performance-based empathy | ||
| Facial affect perception (accuracy) | .91 (.08) | .85 (.11) |
| (Reaction time) | 1693.09 (368.29) | 2079.82 (480.70) |
| Affective responsiveness (accuracy) | .88 (.08) | .79 (.09) |
| (Reaction time) | 1250.05 (259.56) | 1550.23 (451.44) |
| Emotional perspective-taking (accuracy) | .84 (.08) | .74 (.10) |
| (Reaction time) | 1414.41 (261.94) | 1654.73 (349.92) |
| Self-reported empathy | ||
| IRI fantasy | .18 (1.01) | −.13 (.98) |
| IRI perspective-taking | .44 (.95) | −.33 (.91) |
| IRI empathic concern | .26 (.92) | −.19 (1.02) |
| IRI personal distress | −.47 (.83) | .35 (.97) |
Abbreviations are explained in the first footnote to table 1.
For RT, there was a significant main effect of group (F1,103 = 21.91, P < .001) with patients showing generally longer RTs than controls. There was also a significant task effect (F1,103 = 106.66, P < .001) indicating that across groups, RTs were longest for facial affect perception, intermediate for emotional perspective-taking, and shortest for affective responsiveness (all pairwise comparisons P < .001). The group-by-task interaction was not significant (F1,103 = 2.27, P > .10).
Regarding self-reported empathy, although there were no group (F1,103 = 2.40, P > .10) or IRI subscale (F1,103 = .22, P > .10) effects, there was a significant group-by-subscale interaction (F1,103 = 10.96, P < .001). Patients scored lower than controls on perspective-taking (t = 4.18, P < .001) and empathic concern (t = 2.38, P < .05), and higher than controls on personal distress (t = −4.69, P < .001), but the groups did not differ on the fantasy subscale (t = 1.61, P > .10).
As expected, accuracy on the 3 performance measures were moderately to highly correlated among patients (range: r = .39, P < .005 to r = .55, P < .001) and controls (range: r = .65, P < .001 to r = .73, P < .001), while response time on the 3 performance measures were highly correlated among patients (range: r = .55, P < .001 to r = .79, P < .001) and controls (range: r = .69, P < .001 to r = .83, P < .001). The response times for the 3 performance measures demonstrated minimal relations with external variables and were not considered further. Task accuracies showed generally low and nonsignificant correlations with the self-report measures (see table 3). Aside from a borderline significant (p = .05) correlation between affective responsiveness and IRI perspective-taking, there were no other significant relations.
Correlations With Accuracy on Performance-Based Empathy Measures Among Schizophrenia Patients
| . | Facial Affect Perception . | Affective Responsiveness . | Emotional Perspective-Taking . |
|---|---|---|---|
| Self-reported empathy | |||
| IRI fantasy | −.10 | −.07 | −.17 |
| IRI perspective-taking | .20 | .25* | −.05 |
| IRI empathic concern | .23 | .19 | .10 |
| IRI personal distress | −.21 | −.17 | −.18 |
| Neurocognition | |||
| Speed of processing | .30* | .24 | .40** |
| Attention | .32* | .19 | .36** |
| Verbal working memory | .31* | .33** | .32* |
| Nonverbal working memory | .31* | .09 | .33* |
| Verbal learning | .39** | .31* | .22 |
| Problem solving and reasoning | .45*** | .26* | .33** |
| Clinical symptoms | |||
| Positive symptoms | −.03 | −.28* | −.06 |
| Negative symptoms | −.22 | −.45*** | −.26* |
| Disorganized symptoms | −.23 | −.30* | −.15 |
| Functioning measures | |||
| Social competencea | .17 | .32* | .36** |
| Social attainment | .15 | .23 | .13 |
| . | Facial Affect Perception . | Affective Responsiveness . | Emotional Perspective-Taking . |
|---|---|---|---|
| Self-reported empathy | |||
| IRI fantasy | −.10 | −.07 | −.17 |
| IRI perspective-taking | .20 | .25* | −.05 |
| IRI empathic concern | .23 | .19 | .10 |
| IRI personal distress | −.21 | −.17 | −.18 |
| Neurocognition | |||
| Speed of processing | .30* | .24 | .40** |
| Attention | .32* | .19 | .36** |
| Verbal working memory | .31* | .33** | .32* |
| Nonverbal working memory | .31* | .09 | .33* |
| Verbal learning | .39** | .31* | .22 |
| Problem solving and reasoning | .45*** | .26* | .33** |
| Clinical symptoms | |||
| Positive symptoms | −.03 | −.28* | −.06 |
| Negative symptoms | −.22 | −.45*** | −.26* |
| Disorganized symptoms | −.23 | −.30* | −.15 |
| Functioning measures | |||
| Social competencea | .17 | .32* | .36** |
| Social attainment | .15 | .23 | .13 |
aCompleted by n = 51 schizophrenia patients.
*P < .05, **P < .01, and ***P < .001.
Correlations With Accuracy on Performance-Based Empathy Measures Among Schizophrenia Patients
| . | Facial Affect Perception . | Affective Responsiveness . | Emotional Perspective-Taking . |
|---|---|---|---|
| Self-reported empathy | |||
| IRI fantasy | −.10 | −.07 | −.17 |
| IRI perspective-taking | .20 | .25* | −.05 |
| IRI empathic concern | .23 | .19 | .10 |
| IRI personal distress | −.21 | −.17 | −.18 |
| Neurocognition | |||
| Speed of processing | .30* | .24 | .40** |
| Attention | .32* | .19 | .36** |
| Verbal working memory | .31* | .33** | .32* |
| Nonverbal working memory | .31* | .09 | .33* |
| Verbal learning | .39** | .31* | .22 |
| Problem solving and reasoning | .45*** | .26* | .33** |
| Clinical symptoms | |||
| Positive symptoms | −.03 | −.28* | −.06 |
| Negative symptoms | −.22 | −.45*** | −.26* |
| Disorganized symptoms | −.23 | −.30* | −.15 |
| Functioning measures | |||
| Social competencea | .17 | .32* | .36** |
| Social attainment | .15 | .23 | .13 |
| . | Facial Affect Perception . | Affective Responsiveness . | Emotional Perspective-Taking . |
|---|---|---|---|
| Self-reported empathy | |||
| IRI fantasy | −.10 | −.07 | −.17 |
| IRI perspective-taking | .20 | .25* | −.05 |
| IRI empathic concern | .23 | .19 | .10 |
| IRI personal distress | −.21 | −.17 | −.18 |
| Neurocognition | |||
| Speed of processing | .30* | .24 | .40** |
| Attention | .32* | .19 | .36** |
| Verbal working memory | .31* | .33** | .32* |
| Nonverbal working memory | .31* | .09 | .33* |
| Verbal learning | .39** | .31* | .22 |
| Problem solving and reasoning | .45*** | .26* | .33** |
| Clinical symptoms | |||
| Positive symptoms | −.03 | −.28* | −.06 |
| Negative symptoms | −.22 | −.45*** | −.26* |
| Disorganized symptoms | −.23 | −.30* | −.15 |
| Functioning measures | |||
| Social competencea | .17 | .32* | .36** |
| Social attainment | .15 | .23 | .13 |
aCompleted by n = 51 schizophrenia patients.
*P < .05, **P < .01, and ***P < .001.
Correlations Among Empathy, Functioning, and Other Study Variables in Schizophrenia Patients
Facial affect perception significantly correlated with all 6 neurocognitive domains, but not with symptoms or either aspect of functioning (see table 3). Affective responsiveness significantly correlated with the verbal WM, verbal learning, and problem-solving and reasoning domain scores. Higher affective responsiveness also correlated with lower levels of each symptom domain and higher social competence. Finally, higher emotional perspective-taking correlated with lower negative symptoms, higher social competence, and higher neurocognitive scores in all domains except verbal learning.
Regarding other variables associated with functioning, social competence correlated with IRI perspective-taking (r = .28, P < .05), verbal WM (r = .30, P < .05) and, at a trend level, negative symptoms (r = −.27, p = .054). Social attainment significantly correlated with IRI perspective-taking (r = .40, P < .005), attention (r = .32, P < .05), positive symptoms (r = −.26, P < .05), and disorganized symptoms (r = −.37, P < .005).
Prediction of Incremental Variance in Functioning in Schizophrenia Patients
A hierarchical regression model examined the incremental variance explained by accuracies on emotional perspective-taking and affective responsiveness, which both significantly correlated with social competence (see table 4). In Block 1, we added verbal WM, negative symptoms, duration of illness and IRI perspective-taking, which explained 27.5% of the variance in social competence (F4,46 = 4.36, P < .005). Notably, IRI perspective-taking predicted social competence (β = .27, P < .05) during Block 2.
Regression Analyses for Incremental Prediction of Social Competencea
| . | Block 1 . | Block 2 . |
|---|---|---|
| Block 1 | ||
| Verbal working memory | .17 | .07 |
| Negative symptoms | −.27* | −.21 |
| Duration of illness | −.29* | −.29* |
| IRI perspective-taking | .21 | .27* |
| Block 2 | ||
| Affective responsiveness accuracy | — | −.04 |
| Emotional perspective-taking accuracy | — | .31* |
| Total R2 (R2 change) | .275**(.275**) | .345**(.070) |
| . | Block 1 . | Block 2 . |
|---|---|---|
| Block 1 | ||
| Verbal working memory | .17 | .07 |
| Negative symptoms | −.27* | −.21 |
| Duration of illness | −.29* | −.29* |
| IRI perspective-taking | .21 | .27* |
| Block 2 | ||
| Affective responsiveness accuracy | — | −.04 |
| Emotional perspective-taking accuracy | — | .31* |
| Total R2 (R2 change) | .275**(.275**) | .345**(.070) |
aCompleted by n = 51 schizophrenia patients.
*P < .05 and **P < .01.
Regression Analyses for Incremental Prediction of Social Competencea
| . | Block 1 . | Block 2 . |
|---|---|---|
| Block 1 | ||
| Verbal working memory | .17 | .07 |
| Negative symptoms | −.27* | −.21 |
| Duration of illness | −.29* | −.29* |
| IRI perspective-taking | .21 | .27* |
| Block 2 | ||
| Affective responsiveness accuracy | — | −.04 |
| Emotional perspective-taking accuracy | — | .31* |
| Total R2 (R2 change) | .275**(.275**) | .345**(.070) |
| . | Block 1 . | Block 2 . |
|---|---|---|
| Block 1 | ||
| Verbal working memory | .17 | .07 |
| Negative symptoms | −.27* | −.21 |
| Duration of illness | −.29* | −.29* |
| IRI perspective-taking | .21 | .27* |
| Block 2 | ||
| Affective responsiveness accuracy | — | −.04 |
| Emotional perspective-taking accuracy | — | .31* |
| Total R2 (R2 change) | .275**(.275**) | .345**(.070) |
aCompleted by n = 51 schizophrenia patients.
*P < .05 and **P < .01.
In Block 2, the inclusion of emotional perspective-taking and affective responsiveness explained an additional 7.0% of the variance in social competence (ΔF2,44 = 2.36, p = .106). Although the combination of the 2 measures only explained incremental variance near a trend level, the individual predictive value of emotional perspective-taking was significant (β = .31, P < .05), while affective responsiveness was not (β = −.04, P > .10). As a cross check on this result, a supplemental analysis indicated that when emotional perspective-taking was entered alone in Block 2 it significantly accounted for incremental variance in social competence (7.0%; ΔF1,45 = 4.78, P < .05) whereas when affective responsiveness was entered alone in Block 2 it did not (0.1%; ΔF1,45 = 0.55, P > .10). Furthermore, adding facial affect perception scores in Block 1 did not alter the explained variance of emotional perspective-taking (7.2%; ΔF1,44 = 4.87, P < .05) and affective responsiveness (0.0%; ΔF1,44 = 0.04, P > .10).
Although performance-based empathy was not significantly related to social attainment, we conducted a supplemental hierarchical regression analysis to determine if IRI perspective-taking accounted for incremental variance in social attainment. After accounting for attention, positive, and disorganized symptoms in Block 1 (R2 = .17, F3,56 = 3.9, P < .05), IRI perspective-taking was a significant predictor (β = .43, P < .001) and explained an additional 17% of the variance in social attainment (ΔF1,55 = 14.1, P < .001) (see online Supplementary Data).
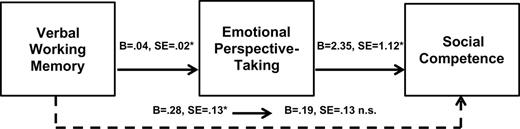
Mediation Model
The mediation results are presented in figure 1. There was a direct effect of verbal WM on emotional perspective-taking accuracy (F1,49 = 6.5, P < .05) and social competence (F1,49 = 4.7, P < .05). A single model using 5000 bootstrap resamples revealed that emotional perspective-taking significantly mediated the effect of verbal WM on social competence (B = .10, SE = .06; 95% CI LL = .02, UL = .29). The direct effect of verbal WM on social competence did not maintain significance (F1,49 = 1.9, P > .10), which supported full mediation.
Emotional perspective-taking mediates the relationship between verbal working memory and social competence. The Preacher and Hayes bootstrapping approach indicates the mediation is statistically significant (95% CI LL = 0.02, UL = 0.29) and supports that the association between verbal working memory and social competence changes from significant to nonsignificant (highlighted by the dashed line). n.s., P > .10; *P < .05; n = 51 schizophrenia patients completed the social competence measure.
Discussion
The current study demonstrates that schizophrenia patients’ self-reported empathic disturbances are accompanied by impaired performance on tasks measuring processes that are critical for adaptive empathic responding. The overall pattern, levels of performance, and score distributions (ie, lack of floor or ceiling effects among patients, which is required for use in clinical trials)74 were highly similar to those reported for the original German paradigm.52 Our findings that performance-based cognitive empathy predicted social competence and self-reported cognitive empathy predicted social attainment, above and beyond neurocognition and symptoms, suggests that empathic disturbances may be useful treatment targets in recovery-oriented interventions.
Schizophrenia patients showed substantially impaired accuracy across all 3 performance-based empathy tasks. Although impaired facial affect perception was expected based on numerous studies,75 only a few studies examined emotional perspective-taking and affective responsiveness. The patients’ impaired emotional perspective-taking is in line with the few prior studies using cognitive empathy tasks, such as making attributions about cartoon characters’ emotions or inferring emotions of people interacting in static images.52,54 The impairment on the affective responsiveness task may be somewhat surprising in light of evidence indicating normal responses to emotional stimuli in schizophrenia patients.76,77 The task, however, did not involve directly confronting participants with emotionally evocative stimuli. Patients appear to have difficulties processing emotions if not directly experiencing them, such as remembering or imagining,44 which could impact empathic processes.
Unexpectedly, we found that reaction times were longer on the facial affect perception task in both groups than the other 2 tasks. A speculative explanation is that the contextual information (eg, written or visual depictions of social situations, body language cues) provided in the emotional perspective-taking and affective responsiveness tasks may have facilitated responding compared with the affect perception task, in which judgments were based on a single face presented with no additional information. It should also be noted that although a significant group-by-task interaction suggested that patients’ accuracy was relatively worse on the emotional perspective-taking and affective responsiveness tasks, this must be interpreted cautiously because the 3 tasks were not psychometrically matched for discriminating power.78
Although patients showed both performance-based and self-reported empathic disturbances, these methods did not show substantial relations with each other. This divergence corresponds with Derntl et al52 and a recent study of performance-based empathic accuracy in schizophrenia48 which both used the IRI. Weak relations between these methods have also been reported in healthy subjects.79,80 These findings highlight the complexity of empathy and indicate that self-reported beliefs about one’s own empathic processes may show little relation to actual ability to understand and respond to others’ emotions. Interestingly, Derntl et al81 recently reported different patterns of performance across tasks and methods in patients with depression and bipolar disorder, suggesting that the schizophrenia patients’ pervasive pattern of impairment may have some diagnostic specificity. In future research, it will be useful to consider factors that may influence self-reported empathy in schizophrenia, including capacity for self-awareness and insight, which has been found to predict self-rater agreement on empathy measures.82
Regarding external correlates, all 3 empathy tasks related to several neurocognitive domains, similar to findings by Derntl et al.52 The magnitude of these relations was in the medium range, indicating that the empathy and neurocognitive measures, though related, are clearly not assessing redundant variance. We found that lower WM (particularly verbal) correlated with poorer performance across all 3 tasks, which is consistent with the notion that disturbances in the ability to hold and manipulate information online may adversely impact empathic processes. Regarding symptoms, lower affective responsiveness related to higher severity for all symptom types, while lower emotional perspective-taking related to higher negative symptoms. These results are at odds with Derntl et al52 who reported minimal relations with symptoms in a mixed inpatient/outpatient sample. Further research is needed on this issue as relationships between symptoms and both performance-based and self-reported empathy have been inconsistent.47,49,52,53,83,84
This study also demonstrated the unique functional relevance of performance-based empathic disturbances for social competence in schizophrenia. Although facial affect perception did not show relations to functioning as seen in prior research,23,85,86 both cognitive and emotional empathy significantly related to social competence. Furthermore, emotional perspective-taking accounted for incremental variance in social competence above and beyond WM and negative symptoms. Thus, the current study extends growing evidence that social cognition uniquely contributes to social competence21–23 via the domain of performance-based empathy.
Performance-based empathy did not contribute incremental variance to real-world social attainment. This nonsignificant relationship could partly reflect our use of patient-, rather than informant-, based SLOF interviews67; some patients may have overreported or underreported their level of functioning during the interview. It is noteworthy, however, that self-reported cognitive empathy did account for unique variance in real-world social attainment, which replicates our prior finding that self-reported cognitive empathy predicted patient interview-based assessments of social attainment.49 In addition, the current findings are consistent with recent integrative models of functioning that describe how basic perceptual and neurocognitive abilities ultimately impact real-world functioning. In these models, (eg,87–90), social cognition appears to be more proximal to social competence than to social attainment, rendering unique relations to social competence simpler to demonstrate. Scores on more distal measures of social attainment can be influenced by a variety of personal (eg, motivation, self-efficacy) and socioenvironmental (eg, disability policies, economic factors, cultural factors) variables. These complex influences can make it more challenging to detect relations with measures of social attainment.
The current mediation results are also consistent with integrative models of functioning in schizophrenia. While prior studies indicate that social cognitive variables mediate the well-established link between global neurocognition and functioning,18,26 our findings add to this literature by demonstrating that cognitive empathy mediates the link between WM and social competence. We focused on WM given the theoretical centrality of this construct for online empathic responding,40 the well-documented finding that WM impairments are associated with poor functioning,9,10,12–17 and recent proposals that WM deficits play a key role in abnormal cognition-emotion interactions in schizophrenia.44–46 In the case of cognitive empathy, impaired WM could interfere with the ability to maintain and integrate information about emotional cues, existing schemas about other people’s feelings, and the current social context, leading to misperceptions of and inappropriate responses to others (see40,91 for related discussions). In future research it will be useful to examine the relation between empathy and other relevant processes included in models of functioning in schizophrenia. For example, Lysaker and colleagues92 recently reported that metacognitive mastery (ie, using knowledge of mental states to manage distress) mediates the link between neurocognition and social competence, and research into the relation between metacognition and empathy could be informative.
This study should be interpreted in the context of some limitations. First, the analyses were based on cross-sectional data, whereas longitudinal designs are needed to confirm these findings and to determine whether the empathy paradigm demonstrates sufficient test-retest reliability for use in clinical trials.93 Second, although CPZ equivalents were not correlated with any study measures, research in unmedicated, early stage patients is needed to address potential medication effects and the generalizability of the findings. Third, no single paradigm measures all processes contributing to empathy and data from multiple tasks and levels of analysis (eg, self-report, behavioral, neural activity) will be necessary to fully characterize empathic disturbances in schizophrenia. For example, the social neuroscience model that guided this study38 does not explicitly incorporate whether one cares for or is motivated to respond to others,94–96 or if empathy is modulated by one’s capacity for self-reflection.97 Finally, we used a data driven approach to identify factors other than performance-based empathy that correlated with social competence and social attainment, and did not correct for multiple comparisons.
In summary, empathy is emerging as a promising new area for social cognitive research and treatment development in schizophrenia. Performance-based empathy measures are sensitive to functionally relevant impairments and may be useful as endpoints in clinical trials or behavioral probes in studies of neural correlates.98–100 Although several psychosocial approaches show promise for improving social cognition in schizophrenia, empathy has not been a focus in these programs.101 Pharmacological interventions (eg, treatment with oxytocin) may also be useful.102 Empathy is a cornerstone for developing meaningful and supportive relationships and efforts to enhance empathic processes may help promote functional recovery in schizophrenia.
Funding
Department of Psychiatry and Behavioral Sciences at Northwestern University Feinberg School of Medicine.
Acknowledgments
We would like to acknowledge the research staff at the Northwestern University Schizophrenia Research Group for study coordination and data collection, and our participants for volunteering their time. From Northwestern University, we would like to thank Dr John Csernansky for comments on an early draft of the manuscript and Dr Zoran Martinovich for his consultation on the statistical analyses. From RWTH Aachen University, Germany, we would like to thank Dr Birgit Derntl, Dr Eva-Marie Seidel, and Dr Ute Habel for providing the tasks and their assistance with translating the tasks into English. From Miami University Miller School of Medicine, we would like to thank Dr Phil Harvey for his recommendation on the functioning measures. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References