-
PDF
- Split View
-
Views
-
Cite
Cite
Jason Jiunshiou Lee, Hsiao-Yun Hu, Shu-Yi Lin, Chao-Ming Huang, Sheng-Jean Huang, Nicole Huang, Factors associated with having home care physicians as an integrated source of medications for chronic conditions among homebound patients, International Journal for Quality in Health Care, Volume 34, Issue 3, 2022, mzac055, https://doi.org/10.1093/intqhc/mzac055
Close - Share Icon Share
Abstract
Inappropriate management of medications is a major threat to homebound patients with chronic conditions. Despite many efforts in improving medication reconciliation in ambulatory and inpatient settings, little research has focused on home care settings. In 2016, Taiwan initiated the Integrated Home Health Care programme, which was intended to reduce potentially inappropriate medication management and risks of uncontrolled polypharmacy through the integration of different medication sources for chronic conditions among homebound patients. This study investigated factors associated with having home care physicians as an integrated source of medications for chronic conditions among homebound patients.
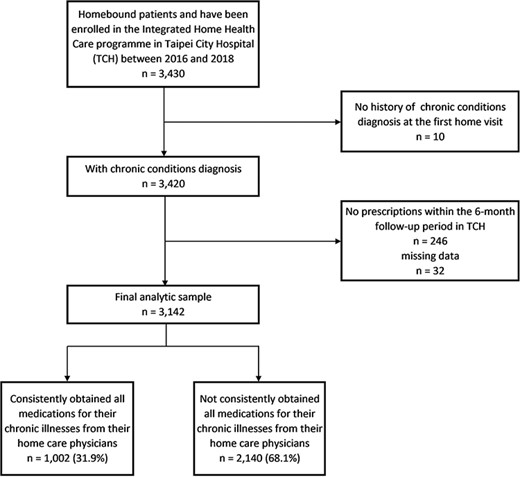
This retrospective cohort study enrolled 3142 community-dwelling homebound patients from Taipei City Hospital. Homebound patients’ adherence to using home care physicians as an integrated source of chronic condition medications was defined as having all prescriptions for their chronic conditions prescribed by a single home care physician for at least 6 months. Both patient and home care physician characteristics were analysed. Multivariable logistic regression was applied.
Of the 3142 patients with chronic conditions, 1002 (31.9%) had consistently obtained all medications for their chronic illnesses from their home care physicians for 6 months and 2140 (68.1%) had not. The most common chronic diseases among homebound patients were hypertension, diabetes mellitus, dementia, cerebrovascular disease and constipation. Oldest-old patients with poor functional status, fewer daily medications, no co-payment exemption and no recent inpatient experience were more likely to adhere to this medication integration system. In addition, patients whose outpatient physicians were also their home care physicians were more likely to adhere to the system.
The finding suggests that building trust and enhancing communication among homebound patients, caregivers and home care physicians are critical. Patient and provider variations highlight the need for further improvement and policy modification for medication reconciliation and management in home care settings. The improvement in medication management and care integration in home care settings may reduce misuse and polypharmacy and improve homebound patients’ safety.
Introduction
An increasing prevalence of chronic conditions has levied substantial financial and care burdens on families and societies. This has become a considerable challenge for many countries [1]; approximately one-third of adults worldwide suffer from a chronic condition or multiple chronic conditions (MCCs) [2]. MCCs are problematic in that they complicate medical regimes and care management, add additional burdens for patients and their caregivers and hinder patients’ mobility and functions [3, 4]. Homebound people are particularly susceptible to these health threats. The Nutrition, Aging, and Memory in Elders Study demonstrated that homebound older adults experienced more medical and psychiatric illnesses than non-homebound older adults did [5]. Approximately 7.3 million ageing Americans are partially homebound due to medical, functional, cognitive or social limitations [3]. In Taiwan, among older beneficiaries, 19 483 patients were identified as homebound and receiving home healthcare visits in 2004; this number increased rapidly to more than 100 000 in 2015 [6].
Providing appropriate care to people with MCCs may be overwhelming for patients, families and providers [7, 8]. People with MCCs have higher odds of receiving care from different health providers [9]. Multiple prescribers have been associated with drug misuse, polypharmacy, increased medical expenses and lower refill adherence [9, 10]. Due to limited mobility, environmental hindrances and inadequate physician–patient communications, homebound people are at an exceptionally high risk [11]. Many facing this reality are concerned that the healthcare system has not yet reoriented itself to accommodate this changing state of disease management and has insufficiently responded to the needs of the population [12–14]. Existing studies on integrating medications have predominantly focused on ambulatory care and inpatient settings [15, 16]. Because integrating and reconciling medication regimens is critical in ensuring the health of home health care patients, gaining a better understanding of such integration among homebound patients is essential.
Taiwan has launched a single-payer compulsory national health insurance (NHI) programme since 1995, which covers 99.6% of the entire population. People have complete flexibility to select or change any care provider anytime. The NHI system allows patients to access speciality services for a small co-payment (approximately $8 for regional hospitals and $14 for medical centres). No referral is needed. For socioeconomically or health disadvantaged subpopulations, their co-payments are exempted. Previous studies have reported that people in Taiwan have more than 13 visits per year and commonly bypass primary care providers to visit specialists for common health problems, including chronic disease treatments [17]. The ineffective referral system in Taiwan has led to poor continuity of care and a fragmented care delivery system [17, 18]. Taiwan has offered home healthcare services for homebound patients since the implementation of the NHI system in 1995 [19]. However, physicians were only allowed to review patients’ prescriptions and not to change medicines or prescribe new ones at patients’ homes [6]. The prescription restriction has posed a large barrier for more effective delivery of home care and reduced patients’ willingness to access home care services. The fragmented delivery system and restricted home care services might have compromised access to and quality of care among homebound patients in Taiwan. Hence, in March 2016, the NHI established the Integrated Home Health Care (IHHC) programme to relax the prescription restriction and allow more services to be offered in home care setting. With the newly established IHHC programme, physicians are now allowed to prescribe medications for homebound patients during home visits. But patients’ adherence to this integrated programme remains unclear. Therefore, the study aimed to identify factors associated with having home care physicians as an integrated source of medications for chronic conditions among homebound patients in Taiwan.
Methods
Study setting and the IHHC
Homebound patients who live at home, have definite medical or nursing needs and have difficulty leaving home (Barthel Index [BI] <60 points) for medical treatment or have chronic condition characteristics, such as those in severe dementia, are eligible for enrolment in the IHHC programme. This programme comprises home-based primary care (HBPC) in three stages: stage 1 is home healthcare (s1), stage 2 is advanced home healthcare (s2) and stage 3 is home-based palliative care (s3). Homebound patients in s1 have medical care needs. Patients in s2 tend to have higher levels of impairment; they need medical and nursing care. During the first home visit, a home care medical team performs a comprehensive geriatric assessment to determine the homebound patient’s medical conditions, mental health, functional capacity and social circumference and to develop a patient-centred care plan [13, 20]. In addition, the physician initiates medication reconciliation, which includes listing and comparing the patient’s current required medications from prescribing providers, developing a new list based on the comparison and communicating the contents of this list to the patient and caregivers. In the IHHC programme, initiation of medication reconciliation is required at the first home visit, and reminders to integrate sources are often given in subsequent home visits. However, the intensity of and willingness toward integration efforts may vary by patient and by physician preferences and practices.
Study design and cohort
This was a retrospective cohort study. All homebound patients enrolled in the Taipei City Hospital (TCH) IHHC programme between 2016 and 2018 were included. Each included patient was followed up for at least 6 months after their IHHC enrolment date. The final sample consisted of 3142 homebound patients with chronic conditions (Figure 1). We obtained the 2015–2019 hospital outpatient records from the TCH Health Information System. The system provided information regarding each participant’s demographic characteristics, medical history, use of services, functional status, home environment assessment and type of primary caregiver. The system also provides information about the physicians whom the patients visited either in an outpatient or home care setting. The names of individual patients and prescribers are encrypted, with unique and anonymous identifiers in the database for confidentiality and privacy assurance. The unique and encrypted physician identifiers can be used to identify the number of prescribers for each patient. The data quality is constantly monitored and maintained by TCH.
Dependent variable
The dependent variable in this study was the homebound patient’s adherence to using home care physicians as their integrated source for prescriptions for chronic diseases. The home care physician refers to the physician who provided medical care to homebound patients in their residential setting. The outpatient physician refers to the physician who provided medical care to patients at an outpatient department or outpatient clinic. This variable was modelled as a binary variable; patients who consistently obtained chronic disease prescriptions solely from their home care physicians for at least 6 months were designated as 1, and patients who did not consistently receive all medications for their chronic diseases from their home care physicians were designated as 0. We assessed the type of chronic conditions by using the chronic condition indicator and clinical classification system of the Agency for Healthcare Research and Quality [21].
Independent variables
The patient demographics and health characteristics included in the models were age, sex, type of primary caregiver, home environmental barriers, BI scores for activities of daily living, HBPC stages, number of daily medications, co-payment exemption status for outpatient care and history of hospitalization before and after enrolment. We categorized patients by age into middle-aged (age <65), youngest-old (age: 65–74 years), middle-old (age: 75–84 years) and oldest-old (age ≥85 years) groups. Patients who are veterans, with disabilities, catastrophic illnesses or whose household income is below the official poverty line are exempted from NHI co-payments. We assumed that homebound patients with different types of primary caregivers, home environmental barriers, functional status and HBPC stages were likely to have different care-seeking behaviours. The type of primary caregiver was categorized into living alone, foreign caregiver and family caregiver. The presence of home environmental barriers was classified as whether a patient was required to climb stairs to leave their home. Each patient’s functional status was estimated using BI scores and was categorized as minimally dependent (BI > 60), partially dependent (BI: 35–60) or severely dependent (BI < 35). We further determined whether each patient had a history of hospitalization before and after enrolment in HBPC; patients who undergo hospital–home transitions are more likely to seek prescriptions from more physicians [22]. Patient characteristics, except for history of hospitalization, were computed based on the characteristics at the date of enrolment. One physician variable was included for analyses: prescriber continuity. Prescriber continuity was defined as whether the patient’s outpatient physicians were also their home care physicians. We assumed that, if the patient’s outpatient physicians were also their home care physicians, the already established doctor–patient relationship would affect adherence to using home care physicians as the integrated source of their medications for chronic diseases.
Data analysis
The means and standard deviations for continuous characteristics and proportions of binary characteristics were calculated. The t-test and chi-square test were used to determine the univariate association. Multivariable logistic regression was used to investigate factors associated with consistent medication reconciliation among homebound patients. An odds ratio (OR) and 95% confidence interval (95% CI) were obtained, and statistical significance was set at P < 0.05. The analysis was performed using the SAS 9.3 statistical software package.
Results
The characteristics of study participants are listed in Table 1. Of the 3142 included home care patients, 1002 patients (31.89%) had their sources of medications for chronic conditions successfully integrated by home care physicians for at least 6 months. The integrated patient group was relatively older than the non-integrated group. A lower proportion of patients in the integrated group had a BI score higher than 60 (n = 47, 4.69%), had cost-sharing exemption (n = 477, 47.60%), were admitted to the hospital either before (n = 316, 31.54%) or after (n = 242, 24.15%) their IHHC enrolment and were classified as s2 patients (n = 351, 35.03%). On average, the integrated group had fewer daily medications (13.50 [SD: 8.52]) than the non-integrated group did (15.85 [SD: 9.36]). At the time of IHHC enrolment, a higher proportion of patients in the integrated group received prescriptions for chronic conditions from non-TCH physicians (n = 325, 32.44%) compared with the non-integrated group. For both patient groups, the top five prevalent chronic conditions are shown in Table 2.
Characteristics of HBPC patients in Taipei City Hospital
| . | . | Consistently obtained all medications for chronic illnesses from home care physicians (n = 1002) . | Not consistently obtained all medications for chronic illnesses from home care physicians (n = 2140) . | . | ||
|---|---|---|---|---|---|---|
| Variables . | Total (n = 3142) . | n . | % . | n . | % . | P value . |
| Age mean (SD) | 84.29 (SD 11.51) | 82.52 (SD 12.07) | <0.001 | |||
| <65 | 255 | 72 | 7.19 | 183 | 8.55 | 0.001 |
| 65–74 | 300 | 73 | 7.29 | 227 | 10.61 | |
| 75–84 | 875 | 265 | 26.45 | 610 | 28.50 | |
| ≥85 | 1712 | 592 | 59.08 | 1120 | 52.34 | |
| Sex | 0.55 | |||||
| Female | 1716 | 555 | 55.39 | 1161 | 54.25 | |
| Male | 1426 | 447 | 44.61 | 979 | 45.75 | |
| BI Score | 0.02 | |||||
| <35 | 2036 | 646 | 64.47 | 1390 | 64.95 | |
| 35–60 | 910 | 309 | 30.84 | 601 | 28.08 | |
| >60 | 196 | 47 | 4.69 | 149 | 6.96 | |
| With co-payment exemption benefits | <0.001 | |||||
| No | 1506 | 525 | 52.40 | 981 | 45.84 | |
| Yes | 1636 | 477 | 47.60 | 1159 | 54.16 | |
| Primary caregiver/household | 0.67 | |||||
| Living alone | 268 | 84 | 8.38 | 184 | 8.60 | |
| Foreign caregivers | 106 | 38 | 3.79 | 68 | 3.18 | |
| Family members | 2768 | 880 | 87.82 | 1888 | 88.22 | |
| Home environmental barriers | 0.11 | |||||
| No need to climb stairs | 1634 | 500 | 49.90 | 1134 | 52.99 | |
| Have to climb stairs | 1508 | 502 | 50.10 | 1006 | 47.01 | |
| Hospitalization history 90 days before the enrolment | <0.001 | |||||
| No | 1871 | 686 | 68.46 | 1185 | 55.37 | |
| Yes | 1271 | 316 | 31.54 | 955 | 44.63 | |
| Hospitalization history after the enrolment during the 6-month follow-up period | <0.001 | |||||
| No | 2155 | 760 | 75.85 | 1395 | 65.19 | |
| Yes | 987 | 242 | 24.15 | 745 | 34.81 | |
| Home care stage | <0.001 | |||||
| Stage 1 (s1) | 1348 | 509 | 50.80 | 839 | 39.21 | |
| Stage 2 (s2) | 1370 | 351 | 35.03 | 1019 | 47.62 | |
| Stage 3 (s3) | 424 | 142 | 14.17 | 282 | 13.18 | |
| Outpatient and the home care physicians | <0.001 | |||||
| No prescriptions history in the Taipei City Hospital before the enrolment | 621 | 325 | 32.44 | 296 | 13.83 | |
| The same prescriber | 776 | 254 | 25.35 | 522 | 24.39 | |
| Not the same prescriber | 1745 | 423 | 42.22 | 1322 | 61.78 | |
| Numbers of medications for chronic conditions daily (mean [SD]) | 13.50 (SD 8.52) | 15.85 (SD 9.36) | <0.001 | |||
| 0–10 | 1097 | 424 | 42.32 | 674 | 31.50 | <0.001 |
| 11–20 | 1279 | 395 | 39.42 | 884 | 41.31 | |
| >20 | 765 | 183 | 18.26 | 582 | 27.20 | |
| . | . | Consistently obtained all medications for chronic illnesses from home care physicians (n = 1002) . | Not consistently obtained all medications for chronic illnesses from home care physicians (n = 2140) . | . | ||
|---|---|---|---|---|---|---|
| Variables . | Total (n = 3142) . | n . | % . | n . | % . | P value . |
| Age mean (SD) | 84.29 (SD 11.51) | 82.52 (SD 12.07) | <0.001 | |||
| <65 | 255 | 72 | 7.19 | 183 | 8.55 | 0.001 |
| 65–74 | 300 | 73 | 7.29 | 227 | 10.61 | |
| 75–84 | 875 | 265 | 26.45 | 610 | 28.50 | |
| ≥85 | 1712 | 592 | 59.08 | 1120 | 52.34 | |
| Sex | 0.55 | |||||
| Female | 1716 | 555 | 55.39 | 1161 | 54.25 | |
| Male | 1426 | 447 | 44.61 | 979 | 45.75 | |
| BI Score | 0.02 | |||||
| <35 | 2036 | 646 | 64.47 | 1390 | 64.95 | |
| 35–60 | 910 | 309 | 30.84 | 601 | 28.08 | |
| >60 | 196 | 47 | 4.69 | 149 | 6.96 | |
| With co-payment exemption benefits | <0.001 | |||||
| No | 1506 | 525 | 52.40 | 981 | 45.84 | |
| Yes | 1636 | 477 | 47.60 | 1159 | 54.16 | |
| Primary caregiver/household | 0.67 | |||||
| Living alone | 268 | 84 | 8.38 | 184 | 8.60 | |
| Foreign caregivers | 106 | 38 | 3.79 | 68 | 3.18 | |
| Family members | 2768 | 880 | 87.82 | 1888 | 88.22 | |
| Home environmental barriers | 0.11 | |||||
| No need to climb stairs | 1634 | 500 | 49.90 | 1134 | 52.99 | |
| Have to climb stairs | 1508 | 502 | 50.10 | 1006 | 47.01 | |
| Hospitalization history 90 days before the enrolment | <0.001 | |||||
| No | 1871 | 686 | 68.46 | 1185 | 55.37 | |
| Yes | 1271 | 316 | 31.54 | 955 | 44.63 | |
| Hospitalization history after the enrolment during the 6-month follow-up period | <0.001 | |||||
| No | 2155 | 760 | 75.85 | 1395 | 65.19 | |
| Yes | 987 | 242 | 24.15 | 745 | 34.81 | |
| Home care stage | <0.001 | |||||
| Stage 1 (s1) | 1348 | 509 | 50.80 | 839 | 39.21 | |
| Stage 2 (s2) | 1370 | 351 | 35.03 | 1019 | 47.62 | |
| Stage 3 (s3) | 424 | 142 | 14.17 | 282 | 13.18 | |
| Outpatient and the home care physicians | <0.001 | |||||
| No prescriptions history in the Taipei City Hospital before the enrolment | 621 | 325 | 32.44 | 296 | 13.83 | |
| The same prescriber | 776 | 254 | 25.35 | 522 | 24.39 | |
| Not the same prescriber | 1745 | 423 | 42.22 | 1322 | 61.78 | |
| Numbers of medications for chronic conditions daily (mean [SD]) | 13.50 (SD 8.52) | 15.85 (SD 9.36) | <0.001 | |||
| 0–10 | 1097 | 424 | 42.32 | 674 | 31.50 | <0.001 |
| 11–20 | 1279 | 395 | 39.42 | 884 | 41.31 | |
| >20 | 765 | 183 | 18.26 | 582 | 27.20 | |
Characteristics of HBPC patients in Taipei City Hospital
| . | . | Consistently obtained all medications for chronic illnesses from home care physicians (n = 1002) . | Not consistently obtained all medications for chronic illnesses from home care physicians (n = 2140) . | . | ||
|---|---|---|---|---|---|---|
| Variables . | Total (n = 3142) . | n . | % . | n . | % . | P value . |
| Age mean (SD) | 84.29 (SD 11.51) | 82.52 (SD 12.07) | <0.001 | |||
| <65 | 255 | 72 | 7.19 | 183 | 8.55 | 0.001 |
| 65–74 | 300 | 73 | 7.29 | 227 | 10.61 | |
| 75–84 | 875 | 265 | 26.45 | 610 | 28.50 | |
| ≥85 | 1712 | 592 | 59.08 | 1120 | 52.34 | |
| Sex | 0.55 | |||||
| Female | 1716 | 555 | 55.39 | 1161 | 54.25 | |
| Male | 1426 | 447 | 44.61 | 979 | 45.75 | |
| BI Score | 0.02 | |||||
| <35 | 2036 | 646 | 64.47 | 1390 | 64.95 | |
| 35–60 | 910 | 309 | 30.84 | 601 | 28.08 | |
| >60 | 196 | 47 | 4.69 | 149 | 6.96 | |
| With co-payment exemption benefits | <0.001 | |||||
| No | 1506 | 525 | 52.40 | 981 | 45.84 | |
| Yes | 1636 | 477 | 47.60 | 1159 | 54.16 | |
| Primary caregiver/household | 0.67 | |||||
| Living alone | 268 | 84 | 8.38 | 184 | 8.60 | |
| Foreign caregivers | 106 | 38 | 3.79 | 68 | 3.18 | |
| Family members | 2768 | 880 | 87.82 | 1888 | 88.22 | |
| Home environmental barriers | 0.11 | |||||
| No need to climb stairs | 1634 | 500 | 49.90 | 1134 | 52.99 | |
| Have to climb stairs | 1508 | 502 | 50.10 | 1006 | 47.01 | |
| Hospitalization history 90 days before the enrolment | <0.001 | |||||
| No | 1871 | 686 | 68.46 | 1185 | 55.37 | |
| Yes | 1271 | 316 | 31.54 | 955 | 44.63 | |
| Hospitalization history after the enrolment during the 6-month follow-up period | <0.001 | |||||
| No | 2155 | 760 | 75.85 | 1395 | 65.19 | |
| Yes | 987 | 242 | 24.15 | 745 | 34.81 | |
| Home care stage | <0.001 | |||||
| Stage 1 (s1) | 1348 | 509 | 50.80 | 839 | 39.21 | |
| Stage 2 (s2) | 1370 | 351 | 35.03 | 1019 | 47.62 | |
| Stage 3 (s3) | 424 | 142 | 14.17 | 282 | 13.18 | |
| Outpatient and the home care physicians | <0.001 | |||||
| No prescriptions history in the Taipei City Hospital before the enrolment | 621 | 325 | 32.44 | 296 | 13.83 | |
| The same prescriber | 776 | 254 | 25.35 | 522 | 24.39 | |
| Not the same prescriber | 1745 | 423 | 42.22 | 1322 | 61.78 | |
| Numbers of medications for chronic conditions daily (mean [SD]) | 13.50 (SD 8.52) | 15.85 (SD 9.36) | <0.001 | |||
| 0–10 | 1097 | 424 | 42.32 | 674 | 31.50 | <0.001 |
| 11–20 | 1279 | 395 | 39.42 | 884 | 41.31 | |
| >20 | 765 | 183 | 18.26 | 582 | 27.20 | |
| . | . | Consistently obtained all medications for chronic illnesses from home care physicians (n = 1002) . | Not consistently obtained all medications for chronic illnesses from home care physicians (n = 2140) . | . | ||
|---|---|---|---|---|---|---|
| Variables . | Total (n = 3142) . | n . | % . | n . | % . | P value . |
| Age mean (SD) | 84.29 (SD 11.51) | 82.52 (SD 12.07) | <0.001 | |||
| <65 | 255 | 72 | 7.19 | 183 | 8.55 | 0.001 |
| 65–74 | 300 | 73 | 7.29 | 227 | 10.61 | |
| 75–84 | 875 | 265 | 26.45 | 610 | 28.50 | |
| ≥85 | 1712 | 592 | 59.08 | 1120 | 52.34 | |
| Sex | 0.55 | |||||
| Female | 1716 | 555 | 55.39 | 1161 | 54.25 | |
| Male | 1426 | 447 | 44.61 | 979 | 45.75 | |
| BI Score | 0.02 | |||||
| <35 | 2036 | 646 | 64.47 | 1390 | 64.95 | |
| 35–60 | 910 | 309 | 30.84 | 601 | 28.08 | |
| >60 | 196 | 47 | 4.69 | 149 | 6.96 | |
| With co-payment exemption benefits | <0.001 | |||||
| No | 1506 | 525 | 52.40 | 981 | 45.84 | |
| Yes | 1636 | 477 | 47.60 | 1159 | 54.16 | |
| Primary caregiver/household | 0.67 | |||||
| Living alone | 268 | 84 | 8.38 | 184 | 8.60 | |
| Foreign caregivers | 106 | 38 | 3.79 | 68 | 3.18 | |
| Family members | 2768 | 880 | 87.82 | 1888 | 88.22 | |
| Home environmental barriers | 0.11 | |||||
| No need to climb stairs | 1634 | 500 | 49.90 | 1134 | 52.99 | |
| Have to climb stairs | 1508 | 502 | 50.10 | 1006 | 47.01 | |
| Hospitalization history 90 days before the enrolment | <0.001 | |||||
| No | 1871 | 686 | 68.46 | 1185 | 55.37 | |
| Yes | 1271 | 316 | 31.54 | 955 | 44.63 | |
| Hospitalization history after the enrolment during the 6-month follow-up period | <0.001 | |||||
| No | 2155 | 760 | 75.85 | 1395 | 65.19 | |
| Yes | 987 | 242 | 24.15 | 745 | 34.81 | |
| Home care stage | <0.001 | |||||
| Stage 1 (s1) | 1348 | 509 | 50.80 | 839 | 39.21 | |
| Stage 2 (s2) | 1370 | 351 | 35.03 | 1019 | 47.62 | |
| Stage 3 (s3) | 424 | 142 | 14.17 | 282 | 13.18 | |
| Outpatient and the home care physicians | <0.001 | |||||
| No prescriptions history in the Taipei City Hospital before the enrolment | 621 | 325 | 32.44 | 296 | 13.83 | |
| The same prescriber | 776 | 254 | 25.35 | 522 | 24.39 | |
| Not the same prescriber | 1745 | 423 | 42.22 | 1322 | 61.78 | |
| Numbers of medications for chronic conditions daily (mean [SD]) | 13.50 (SD 8.52) | 15.85 (SD 9.36) | <0.001 | |||
| 0–10 | 1097 | 424 | 42.32 | 674 | 31.50 | <0.001 |
| 11–20 | 1279 | 395 | 39.42 | 884 | 41.31 | |
| >20 | 765 | 183 | 18.26 | 582 | 27.20 | |
Most common chronic conditions after enrolment in the Integrated Home Health Care programme in Taipei City Hospital
| Consistently obtained all medications for chronic illnesses from home care physicians (n = 1002) | Not consistently obtained all medications for chronic illnesses from home care physicians (n = 2140) | ||||||
| Rank | The most common chronic conditions | Total (n = 3142) | n | % | n | % | P value |
| 1 | Hypertension | 1743 | 595 | 59.38 | 1148 | 53.64 | 0.003 |
| 2 | Diabetes | 996 | 323 | 32.24 | 673 | 31.45 | 0.66 |
| 3 | Dementia | 996 | 312 | 31.14 | 684 | 31.96 | 0.64 |
| 4 | Cerebrovascular disease | 981 | 303 | 30.24 | 678 | 31.68 | 0.42 |
| 5 | Constipation | 833 | 292 | 29.14 | 541 | 25.28 | 0.02 |
| Consistently obtained all medications for chronic illnesses from home care physicians (n = 1002) | Not consistently obtained all medications for chronic illnesses from home care physicians (n = 2140) | ||||||
| Rank | The most common chronic conditions | Total (n = 3142) | n | % | n | % | P value |
| 1 | Hypertension | 1743 | 595 | 59.38 | 1148 | 53.64 | 0.003 |
| 2 | Diabetes | 996 | 323 | 32.24 | 673 | 31.45 | 0.66 |
| 3 | Dementia | 996 | 312 | 31.14 | 684 | 31.96 | 0.64 |
| 4 | Cerebrovascular disease | 981 | 303 | 30.24 | 678 | 31.68 | 0.42 |
| 5 | Constipation | 833 | 292 | 29.14 | 541 | 25.28 | 0.02 |
Most common chronic conditions after enrolment in the Integrated Home Health Care programme in Taipei City Hospital
| Consistently obtained all medications for chronic illnesses from home care physicians (n = 1002) | Not consistently obtained all medications for chronic illnesses from home care physicians (n = 2140) | ||||||
| Rank | The most common chronic conditions | Total (n = 3142) | n | % | n | % | P value |
| 1 | Hypertension | 1743 | 595 | 59.38 | 1148 | 53.64 | 0.003 |
| 2 | Diabetes | 996 | 323 | 32.24 | 673 | 31.45 | 0.66 |
| 3 | Dementia | 996 | 312 | 31.14 | 684 | 31.96 | 0.64 |
| 4 | Cerebrovascular disease | 981 | 303 | 30.24 | 678 | 31.68 | 0.42 |
| 5 | Constipation | 833 | 292 | 29.14 | 541 | 25.28 | 0.02 |
| Consistently obtained all medications for chronic illnesses from home care physicians (n = 1002) | Not consistently obtained all medications for chronic illnesses from home care physicians (n = 2140) | ||||||
| Rank | The most common chronic conditions | Total (n = 3142) | n | % | n | % | P value |
| 1 | Hypertension | 1743 | 595 | 59.38 | 1148 | 53.64 | 0.003 |
| 2 | Diabetes | 996 | 323 | 32.24 | 673 | 31.45 | 0.66 |
| 3 | Dementia | 996 | 312 | 31.14 | 684 | 31.96 | 0.64 |
| 4 | Cerebrovascular disease | 981 | 303 | 30.24 | 678 | 31.68 | 0.42 |
| 5 | Constipation | 833 | 292 | 29.14 | 541 | 25.28 | 0.02 |
The factors associated with patients integrating home care sources for their chronic condition medications and adhering to this integration are listed in Table 3. After adjustment for other variables, compared with the youngest-old (65–74 years), the oldest-old (≥85 years) had a 58% higher chance of consistently maintaining an integrated home care source for medications (P = 0.002). After adjustment, men and women did not differ significantly in whether their sources of medication were integrated. The type of primary caregiver and home environmental barriers were not significantly associated with whether the patient’s sources of medication were integrated.
Factors associated with consistently obtaining all medications for chronic illnesses from home care physicians
| . | Univariable analysis . | Multivariable analysis . | ||||
|---|---|---|---|---|---|---|
| Variables . | OR . | 95% CI . | P value . | OR . | 95% CI . | P value . |
| Age | ||||||
| <65 | 1.22 | 0.84, 1.79 | 0.30 | 1.08 | 0.72, 1.62 | 0.71 |
| 65–74 | 1.00 | 1.00 | ||||
| 75–84 | 1.35 | 1.00, 1.82 | 0.05 | 1.35 | 0.98, 1.85 | 0.06 |
| ≥85 | 1.64 | 1.24, 2.18 | <0.001 | 1.58 | 1.17, 2.13 | 0.003 |
| Sex | ||||||
| Female (reference) | 1.00 | 1.00 | ||||
| Male | 0.96 | 0.82, 1.11 | 0.55 | 1.10 | 0.93, 1.29 | 0.27 |
| BI Score | ||||||
| <35 | 1.47 | 1.05, 2.07 | 0.03 | 2.34 | 1.59, 3.44 | <0.001 |
| 35 ∼ 60 | 1.63 | 1.14, 2.33 | 0.01 | 1.90 | 1.29, 2.80 | 0.001 |
| >60 (reference) | 1.00 | 1.00 | ||||
| With co-payment exemption benefits | ||||||
| No (reference) | 1.30 | 1.12, 1.51 | 0.001 | 1.20 | 1.01, 1.42 | 0.03 |
| Yes | 1.00 | 1.00 | ||||
| Primary caregiver/household | ||||||
| Living alone (reference) | 1.00 | 1.00 | ||||
| Foreign caregivers | 1.22 | 0.76, 1.97 | 0.40 | 1.13 | 0.68, 1.87 | 0.65 |
| Family members | 1.02 | 0.78, 1.34 | 0.88 | 1.09 | 0.81, 1.46 | 0.57 |
| Home environmental barriers | ||||||
| No need to climb stairs (reference) | 1.00 | 1.00 | ||||
| Have to climb stairs | 1.13 | 0.97, 1.32 | 0.11 | 1.08 | 0.92, 1.27 | 0.34 |
| Hospitalization history 90 days before the enrolment | ||||||
| No | 1.75 | 1.49, 2.05 | <0.001 | 1.32 | 1.11, 1.58 | 0.002 |
| Yes (reference) | 1.00 | 1.00 | ||||
| Hospitalization history after the enrolment during the 6-month follow-up period | ||||||
| No | 1.68 | 1.42, 1.99 | <0.001 | 1.37 | 1.14, 1.64 | <0.001 |
| Yes (reference) | 1.00 | 1.00 | ||||
| Home care stage | ||||||
| Stage 1 (s1) | 1.76 | 1.50, 2.08 | <0.001 | 1.58 | 1.30, 1.93 | <0.001 |
| Stage 2 (s2) (reference) | 1.00 | 1.00 | ||||
| Stage 3 (s3) | 1.46 | 1.16, 1.85 | 0.002 | 1.52 | 1.19, 1.95 | <0.001 |
| Outpatient and the home care physicians | ||||||
| No prescription history in the Taipei City Hospital | 3.43 | 2.83, 4.16 | <0.001 | 2.85 | 2.32, 3.50 | <0.001 |
| The same prescriber | 1.52 | 1.26, 1.83 | <0.001 | 1.40 | 1.15, 1.71 | <0.001 |
| Not the same prescriber (reference) | 1.00 | 1.00 | ||||
| Numbers of medications for chronic conditions daily | ||||||
| 0–10 | 2.00 | 1.63, 2.46 | <0.001 | 1.68 | 1.34, 2.09 | <0.001 |
| 11–20 | 1.42 | 1.16, 1.74 | 0.001 | 1.32 | 1.07, 1.63 | 0.011 |
| >20 (reference) | 1.00 | 1.00 | ||||
| . | Univariable analysis . | Multivariable analysis . | ||||
|---|---|---|---|---|---|---|
| Variables . | OR . | 95% CI . | P value . | OR . | 95% CI . | P value . |
| Age | ||||||
| <65 | 1.22 | 0.84, 1.79 | 0.30 | 1.08 | 0.72, 1.62 | 0.71 |
| 65–74 | 1.00 | 1.00 | ||||
| 75–84 | 1.35 | 1.00, 1.82 | 0.05 | 1.35 | 0.98, 1.85 | 0.06 |
| ≥85 | 1.64 | 1.24, 2.18 | <0.001 | 1.58 | 1.17, 2.13 | 0.003 |
| Sex | ||||||
| Female (reference) | 1.00 | 1.00 | ||||
| Male | 0.96 | 0.82, 1.11 | 0.55 | 1.10 | 0.93, 1.29 | 0.27 |
| BI Score | ||||||
| <35 | 1.47 | 1.05, 2.07 | 0.03 | 2.34 | 1.59, 3.44 | <0.001 |
| 35 ∼ 60 | 1.63 | 1.14, 2.33 | 0.01 | 1.90 | 1.29, 2.80 | 0.001 |
| >60 (reference) | 1.00 | 1.00 | ||||
| With co-payment exemption benefits | ||||||
| No (reference) | 1.30 | 1.12, 1.51 | 0.001 | 1.20 | 1.01, 1.42 | 0.03 |
| Yes | 1.00 | 1.00 | ||||
| Primary caregiver/household | ||||||
| Living alone (reference) | 1.00 | 1.00 | ||||
| Foreign caregivers | 1.22 | 0.76, 1.97 | 0.40 | 1.13 | 0.68, 1.87 | 0.65 |
| Family members | 1.02 | 0.78, 1.34 | 0.88 | 1.09 | 0.81, 1.46 | 0.57 |
| Home environmental barriers | ||||||
| No need to climb stairs (reference) | 1.00 | 1.00 | ||||
| Have to climb stairs | 1.13 | 0.97, 1.32 | 0.11 | 1.08 | 0.92, 1.27 | 0.34 |
| Hospitalization history 90 days before the enrolment | ||||||
| No | 1.75 | 1.49, 2.05 | <0.001 | 1.32 | 1.11, 1.58 | 0.002 |
| Yes (reference) | 1.00 | 1.00 | ||||
| Hospitalization history after the enrolment during the 6-month follow-up period | ||||||
| No | 1.68 | 1.42, 1.99 | <0.001 | 1.37 | 1.14, 1.64 | <0.001 |
| Yes (reference) | 1.00 | 1.00 | ||||
| Home care stage | ||||||
| Stage 1 (s1) | 1.76 | 1.50, 2.08 | <0.001 | 1.58 | 1.30, 1.93 | <0.001 |
| Stage 2 (s2) (reference) | 1.00 | 1.00 | ||||
| Stage 3 (s3) | 1.46 | 1.16, 1.85 | 0.002 | 1.52 | 1.19, 1.95 | <0.001 |
| Outpatient and the home care physicians | ||||||
| No prescription history in the Taipei City Hospital | 3.43 | 2.83, 4.16 | <0.001 | 2.85 | 2.32, 3.50 | <0.001 |
| The same prescriber | 1.52 | 1.26, 1.83 | <0.001 | 1.40 | 1.15, 1.71 | <0.001 |
| Not the same prescriber (reference) | 1.00 | 1.00 | ||||
| Numbers of medications for chronic conditions daily | ||||||
| 0–10 | 2.00 | 1.63, 2.46 | <0.001 | 1.68 | 1.34, 2.09 | <0.001 |
| 11–20 | 1.42 | 1.16, 1.74 | 0.001 | 1.32 | 1.07, 1.63 | 0.011 |
| >20 (reference) | 1.00 | 1.00 | ||||
Factors associated with consistently obtaining all medications for chronic illnesses from home care physicians
| . | Univariable analysis . | Multivariable analysis . | ||||
|---|---|---|---|---|---|---|
| Variables . | OR . | 95% CI . | P value . | OR . | 95% CI . | P value . |
| Age | ||||||
| <65 | 1.22 | 0.84, 1.79 | 0.30 | 1.08 | 0.72, 1.62 | 0.71 |
| 65–74 | 1.00 | 1.00 | ||||
| 75–84 | 1.35 | 1.00, 1.82 | 0.05 | 1.35 | 0.98, 1.85 | 0.06 |
| ≥85 | 1.64 | 1.24, 2.18 | <0.001 | 1.58 | 1.17, 2.13 | 0.003 |
| Sex | ||||||
| Female (reference) | 1.00 | 1.00 | ||||
| Male | 0.96 | 0.82, 1.11 | 0.55 | 1.10 | 0.93, 1.29 | 0.27 |
| BI Score | ||||||
| <35 | 1.47 | 1.05, 2.07 | 0.03 | 2.34 | 1.59, 3.44 | <0.001 |
| 35 ∼ 60 | 1.63 | 1.14, 2.33 | 0.01 | 1.90 | 1.29, 2.80 | 0.001 |
| >60 (reference) | 1.00 | 1.00 | ||||
| With co-payment exemption benefits | ||||||
| No (reference) | 1.30 | 1.12, 1.51 | 0.001 | 1.20 | 1.01, 1.42 | 0.03 |
| Yes | 1.00 | 1.00 | ||||
| Primary caregiver/household | ||||||
| Living alone (reference) | 1.00 | 1.00 | ||||
| Foreign caregivers | 1.22 | 0.76, 1.97 | 0.40 | 1.13 | 0.68, 1.87 | 0.65 |
| Family members | 1.02 | 0.78, 1.34 | 0.88 | 1.09 | 0.81, 1.46 | 0.57 |
| Home environmental barriers | ||||||
| No need to climb stairs (reference) | 1.00 | 1.00 | ||||
| Have to climb stairs | 1.13 | 0.97, 1.32 | 0.11 | 1.08 | 0.92, 1.27 | 0.34 |
| Hospitalization history 90 days before the enrolment | ||||||
| No | 1.75 | 1.49, 2.05 | <0.001 | 1.32 | 1.11, 1.58 | 0.002 |
| Yes (reference) | 1.00 | 1.00 | ||||
| Hospitalization history after the enrolment during the 6-month follow-up period | ||||||
| No | 1.68 | 1.42, 1.99 | <0.001 | 1.37 | 1.14, 1.64 | <0.001 |
| Yes (reference) | 1.00 | 1.00 | ||||
| Home care stage | ||||||
| Stage 1 (s1) | 1.76 | 1.50, 2.08 | <0.001 | 1.58 | 1.30, 1.93 | <0.001 |
| Stage 2 (s2) (reference) | 1.00 | 1.00 | ||||
| Stage 3 (s3) | 1.46 | 1.16, 1.85 | 0.002 | 1.52 | 1.19, 1.95 | <0.001 |
| Outpatient and the home care physicians | ||||||
| No prescription history in the Taipei City Hospital | 3.43 | 2.83, 4.16 | <0.001 | 2.85 | 2.32, 3.50 | <0.001 |
| The same prescriber | 1.52 | 1.26, 1.83 | <0.001 | 1.40 | 1.15, 1.71 | <0.001 |
| Not the same prescriber (reference) | 1.00 | 1.00 | ||||
| Numbers of medications for chronic conditions daily | ||||||
| 0–10 | 2.00 | 1.63, 2.46 | <0.001 | 1.68 | 1.34, 2.09 | <0.001 |
| 11–20 | 1.42 | 1.16, 1.74 | 0.001 | 1.32 | 1.07, 1.63 | 0.011 |
| >20 (reference) | 1.00 | 1.00 | ||||
| . | Univariable analysis . | Multivariable analysis . | ||||
|---|---|---|---|---|---|---|
| Variables . | OR . | 95% CI . | P value . | OR . | 95% CI . | P value . |
| Age | ||||||
| <65 | 1.22 | 0.84, 1.79 | 0.30 | 1.08 | 0.72, 1.62 | 0.71 |
| 65–74 | 1.00 | 1.00 | ||||
| 75–84 | 1.35 | 1.00, 1.82 | 0.05 | 1.35 | 0.98, 1.85 | 0.06 |
| ≥85 | 1.64 | 1.24, 2.18 | <0.001 | 1.58 | 1.17, 2.13 | 0.003 |
| Sex | ||||||
| Female (reference) | 1.00 | 1.00 | ||||
| Male | 0.96 | 0.82, 1.11 | 0.55 | 1.10 | 0.93, 1.29 | 0.27 |
| BI Score | ||||||
| <35 | 1.47 | 1.05, 2.07 | 0.03 | 2.34 | 1.59, 3.44 | <0.001 |
| 35 ∼ 60 | 1.63 | 1.14, 2.33 | 0.01 | 1.90 | 1.29, 2.80 | 0.001 |
| >60 (reference) | 1.00 | 1.00 | ||||
| With co-payment exemption benefits | ||||||
| No (reference) | 1.30 | 1.12, 1.51 | 0.001 | 1.20 | 1.01, 1.42 | 0.03 |
| Yes | 1.00 | 1.00 | ||||
| Primary caregiver/household | ||||||
| Living alone (reference) | 1.00 | 1.00 | ||||
| Foreign caregivers | 1.22 | 0.76, 1.97 | 0.40 | 1.13 | 0.68, 1.87 | 0.65 |
| Family members | 1.02 | 0.78, 1.34 | 0.88 | 1.09 | 0.81, 1.46 | 0.57 |
| Home environmental barriers | ||||||
| No need to climb stairs (reference) | 1.00 | 1.00 | ||||
| Have to climb stairs | 1.13 | 0.97, 1.32 | 0.11 | 1.08 | 0.92, 1.27 | 0.34 |
| Hospitalization history 90 days before the enrolment | ||||||
| No | 1.75 | 1.49, 2.05 | <0.001 | 1.32 | 1.11, 1.58 | 0.002 |
| Yes (reference) | 1.00 | 1.00 | ||||
| Hospitalization history after the enrolment during the 6-month follow-up period | ||||||
| No | 1.68 | 1.42, 1.99 | <0.001 | 1.37 | 1.14, 1.64 | <0.001 |
| Yes (reference) | 1.00 | 1.00 | ||||
| Home care stage | ||||||
| Stage 1 (s1) | 1.76 | 1.50, 2.08 | <0.001 | 1.58 | 1.30, 1.93 | <0.001 |
| Stage 2 (s2) (reference) | 1.00 | 1.00 | ||||
| Stage 3 (s3) | 1.46 | 1.16, 1.85 | 0.002 | 1.52 | 1.19, 1.95 | <0.001 |
| Outpatient and the home care physicians | ||||||
| No prescription history in the Taipei City Hospital | 3.43 | 2.83, 4.16 | <0.001 | 2.85 | 2.32, 3.50 | <0.001 |
| The same prescriber | 1.52 | 1.26, 1.83 | <0.001 | 1.40 | 1.15, 1.71 | <0.001 |
| Not the same prescriber (reference) | 1.00 | 1.00 | ||||
| Numbers of medications for chronic conditions daily | ||||||
| 0–10 | 2.00 | 1.63, 2.46 | <0.001 | 1.68 | 1.34, 2.09 | <0.001 |
| 11–20 | 1.42 | 1.16, 1.74 | 0.001 | 1.32 | 1.07, 1.63 | 0.011 |
| >20 (reference) | 1.00 | 1.00 | ||||
Regarding health status, compared with those with a BI score >60 points, those with a score <35 and between 35 and 60 were 2.34 (95% CI: 1.59, 3.44) and 1.90 (95% CI: 1.29, 2.80) times more likely to consistently use their home care physician as an integrated medication source. The patients without any hospitalization 90 days before IHHC enrolment or during the 6-month follow-up period had a 32% (95% CI: 1.11, 1.58) and 37% (95% CI: 1.14, 1.64) higher chance of receiving their medications for chronic conditions solely from their home healthcare providers (P = 0.002 and P = 0.001), respectively. Similar to the findings for other health status variables, home care patients at the highest stage of home care requirement (s3) had a significantly higher likelihood of having their medications integrated (adjusted OR (aOR) : 1.52, 95% CI: 1.19, 1.95). In addition, patients at the lowest level of home care requirement (s1) were significantly more likely to have their home care physicians as their integrated source of medications than patients at a moderate level of home care requirement (s2) were (aOR: 1.58, 95% CI: 1.30, 1.93). Furthermore, an inverse dose-response pattern was observed between the number of daily medications and the likelihood of having integrated medication sources. Patients who took 10 or fewer daily medications had the highest likelihood of consistently having their home care physicians as the sole source of medications for their chronic conditions (aOR: 1.68, 95% CI: 1.34, 2.09), followed by those who took 11–20 daily medications (aOR: 1.32, 95% CI: 1.07, 1.63) and those who took more than 20 daily medications.
Home care patients who were not exempted from NHI co-payments were 20% more likely to consistently have their home care physicians as their sole source of medications (P = 0.034). Furthermore, patients who had previously had their medications prescribed by non-TCH physicians were more likely to have integrated sources of medications and their home care physicians as the sole source (aOR: 2.85, 95% CI: 2.32, 3.50). Of the patients whose primary care provider was TCH before IHHC enrolment, those whose ambulatory care physicians were also their home care physicians had a higher likelihood of having their sources of medication integrated (aOR: 1.40, 95% CI: 1.15, 1.71) than those who had different physicians for ambulatory and home care.
Discussion
Statement of principal findings
This study found that approximately one-third of the included home care patients agreed to have their sources of medications for chronic conditions integrated by their home care physicians and adhered to this system of integration for at least 6 months. The oldest-old homebound patients who had poor functional status, fewer daily medications, no co-payment exemption and recent inpatient experience were more likely to adhere to this system of medication integration. In addition, patients whose outpatient physicians were also their home care physicians were more likely to have their home care physicians as the sole source of prescriptions. The continuous therapeutic relationship between the physician and the patient is highly valued and leads to higher trust between physicians and patients, especially the patient would feel they have more control over their health [23, 24]. Also, patients may feel more comfortable, and care delivery may be more efficient when they are cared for by the same doctors. Long-term physician–patient collaboration is associated with better patient adherence. The relationship between collaboration and adherence is sustained for patients with chronic conditions and primary physicians and specialists [23, 25]. The significant results for patient and provider variations highlight the need for further improvement and policy modification for medication reconciliation and management in home care settings.
Interpretation within the context of the wider literature
Pharmacotherapy and prescriptions for older and homebound adults are complicated due to age-related physiological changes, MCCs, multiple prescribers and polypharmacy [26]. This study has revealed several key factors associated with using home care physicians as homebound patients’ integrated source of chronic condition medications. First, homebound patients older than 85 were more likely to adhere to the system of medication integration than youngest-old patients were. One plausible explanation is that the caregivers of the oldest-old homebound patients tended to be relatives, who may also be older adults. Navigating different care providers for patients with complex health needs may be burdensome and stressful for older caregivers; hence, they may be more appreciative of integrated services.
Second, similar to reports of previous studies, financial barriers were revealed to play a significant role in adherence to the system. Patients who had NHI co-payment exemption for outpatient services were less likely to use this home care integration service than those who did not. The integrated medication service provided by home care physicians reduces patients’ need to seek outpatient services for individual chronic conditions and, therefore, relieves the financial burden of homebound patients who do not have co-payment exemptions. Third, patients who had recent inpatient experiences were less likely to participate in this integrated system; this may be explained by concerns regarding poor communication or loss of essential information during transitions between the different healthcare settings [27]. Notably, for patients with MCCs, drug therapy problems are more common during care transitions [28]. In Taiwan, the information transmission or communication between hospital and out-of-hospital physicians is relatively poor. Although the NHI ‘MediCloud system’ allows either hospital or out-of-hospital physicians to access information on patients’ medications and examinations within 3 months, the information recorded in the MediCloud system is still relatively limited. Patients and their families remain the main common threads of information transmission or communication between hospital and out-of-hospital physicians. Outpatient or ambulatory care physicians mainly rely on their patients or families for the patient’s hospital admissions or treatment information during their encounters following discharges. Because hospitalization may increase the risks of medication discrepancies or unintentional discontinuation of chronic medications, timely and effective communication is essential to enhance the safety and continuity of medication and chronic condition care between inpatient and home care physicians [29, 30].
From a provider’s perspective, a qualitative study discussed medication complexity in home healthcare and how a fragmented healthcare system may lead to a breakdown of information and communication. The lack of trust in new providers contributes to system fragmentation [29]. Our study revealed that prescriber continuity was a key in patients’ decisions to have home care physicians as their sole source of chronic condition medications. Patients who had their outpatient physicians as their home care physicians had a 40% higher chance of participating in the integration programme. Building trust in the quality of care offered by home care physicians among homebound patients and caregivers is critical for increasing participation in such an integrated medication programme. Efforts to strengthen information sharing among patients, caregivers and home care teams may also assist in this regard [31].
The rapidly ageing population with an increased prevalence of multiple chronic diseases has been a global phenomenon. It poses severe challenges to health care systems, particularly in countries with a fragmented delivery system. Enhancing integration among different services and health care providers has been the most popular strategic approach. However, many integrative care models predominantly target care offered in physician’s offices, clinics, hospitals and post-acute care institutions. These prior efforts may not optimally benefit chronically ill and homebound patients. Hence, many countries, including the USA, Canada, Japan and European countries, have launched home-based models to provide patient-centred integrative care [32–34]. Our findings may help shed light on the areas for further improvement and policy modification in medication reconciliation efforts in home care settings.
Strengths and limitations
To our knowledge, this was the first quantitative study to identify patient- and physician-level factors associated with using home care physicians as an integrated source of prescriptions for chronic conditions among homebound patients. This study had a few notable limitations. First, the data set used in this study only included the patients who sought care from TCH. Therefore, our study may have overestimated the incidence of homebound patients using home care physicians as their integrated source of medications for chronic conditions. We might also have misclassified patients who were admitted to hospitals other than TCH because they did not have inpatient experience before or after enrolment. Second, due to the nature of the study design and data limitations, only limited provider characteristics could be assessed in this study. Future studies with a population-based design and more data on provider characteristics may further contribute to the literature in this regard. Third, due to data limitations, we were unable to explore the factors and options patients and caregivers may have discussed in their joint decision-making process. Qualitative data may supplement our understanding of this process. Fourth, the generalizability of the findings may be a source of concern; our data were obtained from a single hospital. However, because TCH is a prominent healthcare organization dedicated to providing home care and has cared for the most home care patients since the IHHC programme began, the results obtained from TCH may assist in understanding the implementation and performance of the medication integration policy for homebound patients within the NHI programme.
Implications for policy, practice and research
The findings of this study suggest that building trust and enhancing communication among homebound patients, caregivers and home care physicians are critical. Home care teams must expend time and effort for integration programmes to succeed. However, the financial incentives provided by the IHHC programme are extremely stringent, and more reasonable provider payment plans may be required. In addition, providing better access to patient information systems in the home care settings and reducing bureaucratic administrative processes may further facilitate trust-building and communication.
Moreover, efforts to increase nonhome care physicians’ understanding of and trust in home care services’ quality should not be overlooked. Otherwise, nonhome care physicians may have limited confidence and understanding of the IHHC programme. Furthermore, if nonhome care physicians prescribe medications to homebound patients without visiting these patients, this may hinder medication integration policies.
Conclusions
Patients’ demographic characteristics, health status and prescriber continuity were associated with having their home care physicians as the sole providers of medications for chronic conditions. Significant patient and provider variations highlight the areas in which further improvement and policy modification might be made in home care settings to minimize care fragmentation. Better coordination, trust-building, enhanced communication and management of medication in home care settings can improve homebound patients’ safety, reduce misuse and polypharmacy and improve adherence to systems of integration.
Data availability statement
The data underlying this article will be shared on reasonable request to the corresponding author.
Acknowledgements
The authors thank the Centre for Public Health, Department of Education and Research, Taipei City Hospital, for their valuable contributions to data management and statistical analysis. This manuscript was edited by Wallace Academic Editing.
Funding
No funding was received for this project.
Contributorship
All authors were responsible for the study design and interpreting the results. J.J.L, H.H., S.-Y.L., C.-M.H., S.-J.H. and N.H. conceptualized the study and developed the study design. C.-M.H. and S.-J.H. made substantial contributions to the data collections, and C.-M.H. extracted the data. J.J.L. drafted the manuscript. J.J.L., H.-Y.H. and S.-Y.L. did all the analyses. N.H. revised the manuscript critically. All authors reviewed the manuscript and approved the final version.
Ethics and other permissions
The study was approved by the Taipei City Hospital Research Ethics Committee (TCHIRB-10712105-E). All methods were conducted in accordance with the relevant guidelines and regulations of the Taipei City Hospital Research Ethics Committee.