-
PDF
- Split View
-
Views
-
Cite
Cite
Jane Wills, Nicola Crichton, Ava Lorenc, Muireann Kelly, Using population segmentation to inform local obesity strategy in England, Health Promotion International, Volume 30, Issue 3, September 2015, Pages 658–666, https://doi.org/10.1093/heapro/dau004
Close - Share Icon Share
Abstract
Little is known about the views of obese people and how best to meet their needs. Amongst London boroughs Barking and Dagenham has the highest prevalence of adult obesity at 28.7%; the lowest level of healthy eating and of physical activity; and is the 22nd most deprived area of England. The study aimed to gain insight into the attitudes, motivations and priorities of people who are obese or overweight to inform the social marketing of an obesity strategy. Two hundred and ten obese or overweight adults were recruited through visual identification in public thoroughfares to attempt to recruit those seldom seen in primary care. One hundred and eighty-one street-intercept and 52 in-depth interviews were conducted. Thematic analysis was followed by psychographic segmentation. Eleven population segments were identified based on their readiness to change, the value accorded to tackling obesity, identified enabling factors and barriers to weight management and perceived self-efficacy. This population showed considerable variation in its readiness to change and perceived control over obesity but considerable similarity in the exchange value they attributed to tackling their obesity. Even within a relatively homogenous socio-demographic community, there needs to be a range of interventions and messages tailored for different population segments that vary in their readiness to change and confidence about tackling obesity. The dominant emphasis of policy and practice on the health consequences of obesity does not reflect the priorities of this obese population for whom the exchange value of addressing obesity was daily functioning especially in relation to family life.
INTRODUCTION
Obesity in England is at its highest prevalence since recording began in 1993, with 26% of adults now classed as obese (NHS Information Centre for Health and Social Care, 2012). Notwithstand-ing the complex web of biological and societal factors that have contributed to this increase (Butland et al., 2007), the accumulation of excess body fat can be attributed to food and drink consumption exceeding energy expended through the body's metabolism and physical activity. At the individual level, obesity is a product of the slow ‘drip drip’ effect of poor diet and sedentary lifestyles. The behaviours that lead to obesity become routine, unconscious and resilient to change; a problem compounded by a long lag phase between cause and effect. Research with obese individuals has tended to treat this group as one homogenous cluster, with little acknowledgement that beliefs, lifestyle, attitudes or demographic characteristics vary greatly within this population (Thomas et al., 2008). A difference has been noted between public health messages around obesity and the experiences of obese individuals (Lewis et al., 2010), and a recent report commissioned by the Department of Health concluded that the ‘one-size-fits-all’ approach to weight management be dismissed in favour of more individualized, tailored methods (Department of Health, 2010a). In order to positively influence people's engagement in addressing obesity, a deeper understanding of what matters most to obese people and why is required to better impact on the real-world barriers to particular choices and likely motivating factors for change. The evidence on the motivations for behaviour change amongst obese populations is limited, usually gathered from patients or participants in commercial weight loss programmes. Thus, the existing evidence of obese people's motivations to change reflects only those who choose to engage in such programmes, which is likely to be a minority of obese people. Attitudinal evidence can illuminate whether obesity is perceived as a health risk (Lewis et al., 2010) or whether individuals believe that it is possible to be healthy at every size (Rothblum and Solway, 2009); what the likely motivating factors for weight management may be (Befort et al., 2008; Greener et al., 2010; Ogden and Clementi, 2010; Lewis et al., 2011) and how easy or difficult losing weight is perceived to be (Befort et al., 2008; Herriot et al., 2008; Thomas et al., 2008, Thomas et al., 2010; Lewis et al., 2011; Wiklund et al., 2011).
The wide range of constructs which affect individual behaviour that are derived from theories of behaviour have been highlighted by Michie et al.(Michie et al., 2008) and includes a person's intention, perceived behavioural control, self-efficacy and their expectation of a particular outcome. Michie's Com-B model (Michie et al., 2011) shows clearly there are three necessary conditions for behaviour change to occur: the psychological or physical ability to enact the behaviour including having the necessary knowledge and skills (capability), reflective or automatic mechanisms that activate or inhibit behaviour including habit and emotion (motivation) and a physical or social environment that encourages the behaviour (opportunity). Self-efficacy and the decisional balance are the two main constructs used in the Transtheoretical Model of Change (Prochaska and DiClemente, 1983; Prochaska and Velicer, 1997) which is the widely adopted framework that attempts to explain readiness to act and provides a process by which to guide individuals through the stages of change towards ultimately adopting the desired behaviour. Psychological theories may variously identify the factors that influence motivation including beliefs about both the causes and consequences of current behaviour, the expected outcomes of a new behaviour, the extent to which there may be a reward from it and perceptions of social norms (Ajzen and Fishbein, 1980). Yet as Teixeira et al.(Teixeira et al. 2012) have pointed out such theories do not examine the nature of goals and the quality of motivation behind the desire to lose weight. Whilst a whole range of interventions attempt to address capability through health education and improving health literacy and address opportunity through improving food access and incentivizing weight management, understanding motivation and why some people do not attempt to change provides a challenge for obesity strategy.
Health-related social marketing is a process that identifies how to communicate a message based on what will motivate individuals to change behaviour and the offers that might encourage that change based on a principle of ‘exchange value’—what a person might be prepared to give up or lose by making a change (French and Blair-Stevens, 2005). Exchange theory illuminates the benefits of any change as perceived by people themselves and the full costs to them, including financial, physical, social, time and effort involved in gaining the benefits. The English Public Health White Paper reaffirmed government commitment to social marketing, declaring ‘Central government will sequence social marketing for public health throughout the life course … using emerging ideas from behavioural science, such as the use of social norms, changing defaults and providing incentives’ (Department of Health, 2010b, p. 44). One of the most important components of a social marketing approach is audience segmentation, or the identification of distinct, definable population subgroups whose members have unique barriers and motivations around a particular behaviour and for whom different messages or incentives may be necessary.
Traditionally, obesity strategies and service delivery have targeted distinct subgroups of the population based on socio-demographic characteristics, usually socioeconomic status but also life stage (Tapp et al., 2006; Powell et al., 2007; Tapp et al., 2008). Geo-demographic profiles are also widely used in the UK to target services as they can provide a detailed small area analysis of aspects of social status and consumption at a postcode level. Previous research has noted that segmentation relying solely on demographic variables may have limited worth when identifying segments that are homogeneous with respect to health-related outcomes (Boslaugh et al., 2005), and would not uncover the different motivations each segment may have for health-related behaviour change. Psychographic segmentation helps to reveal these patterns or differences between groups of people who may be similar in age, gender or socioeconomic status. This addition of psychographic variables to behavioural insight adds information about ‘why’ to the ‘who’ and ‘where’ provided by socio-demographic and geo-demographic information (French et al., 2011). Psychographic segmentation has been employed in relation to physical activity (Sport England, 2009) and dietary choices (Byrd-Bredbenner et al., 2008) using additional information gathered from insight research. The Department of Health Change4Life campaign used segmentation to divide families into six clusters depending on their attitude towards diet and physical activity, levels of obesity and food consumption and demographic make-up to enable interventions to promote healthy weight in families to be more effectively targeted and delivered (Department of Health, 2008). Table 1 illustrates how different types of segmentation have been used in recent studies of health behaviour.
Examples of segmentation methods
| Segmentation type . | Used by . | Description . | Sample segment . |
|---|---|---|---|
| Geodemographic | Mosaic UK profiling tool (Experian, 2004) | Classifications identify neighbourhood household types and person types based on demographic data (e.g. age, sex, socioeconomic status, property characteristics, location) and financial measures indicating behaviour | Bright Young Things: Well-educated young singles paying high rents to live in smart inner-city apartments |
| Psychographic | Sport England: market segmentation (Sport England, 2009) | Used results from the Active People survey to identify nineteen sporting segments in order to better understand the nation's attitudes to sports and motivations for action | Sports Team Lads: Young blokes enjoying football, pints and pool |
| Life course | Healthy Foundations segmentation model (Department of Health, 2010c) | Classification based on life stages which can encourage healthy or unhealthy behaviours. Nine life stages were identified | Young Settlers: People aged between 16 and 44 who have a partner. No children in the household, no caring responsibilities and are not retired |
| Pen portraits | Maximizing the appeal of weight management services (Department of Health, 2010a) | Based on interviews and focus groups, this study identified nine people segments based on motivations, barriers and ideal services | Younger women: Aspiring to ‘body beautiful’. Desire a youthful and glamorous service that is active and energizing |
| Segmentation type . | Used by . | Description . | Sample segment . |
|---|---|---|---|
| Geodemographic | Mosaic UK profiling tool (Experian, 2004) | Classifications identify neighbourhood household types and person types based on demographic data (e.g. age, sex, socioeconomic status, property characteristics, location) and financial measures indicating behaviour | Bright Young Things: Well-educated young singles paying high rents to live in smart inner-city apartments |
| Psychographic | Sport England: market segmentation (Sport England, 2009) | Used results from the Active People survey to identify nineteen sporting segments in order to better understand the nation's attitudes to sports and motivations for action | Sports Team Lads: Young blokes enjoying football, pints and pool |
| Life course | Healthy Foundations segmentation model (Department of Health, 2010c) | Classification based on life stages which can encourage healthy or unhealthy behaviours. Nine life stages were identified | Young Settlers: People aged between 16 and 44 who have a partner. No children in the household, no caring responsibilities and are not retired |
| Pen portraits | Maximizing the appeal of weight management services (Department of Health, 2010a) | Based on interviews and focus groups, this study identified nine people segments based on motivations, barriers and ideal services | Younger women: Aspiring to ‘body beautiful’. Desire a youthful and glamorous service that is active and energizing |
Examples of segmentation methods
| Segmentation type . | Used by . | Description . | Sample segment . |
|---|---|---|---|
| Geodemographic | Mosaic UK profiling tool (Experian, 2004) | Classifications identify neighbourhood household types and person types based on demographic data (e.g. age, sex, socioeconomic status, property characteristics, location) and financial measures indicating behaviour | Bright Young Things: Well-educated young singles paying high rents to live in smart inner-city apartments |
| Psychographic | Sport England: market segmentation (Sport England, 2009) | Used results from the Active People survey to identify nineteen sporting segments in order to better understand the nation's attitudes to sports and motivations for action | Sports Team Lads: Young blokes enjoying football, pints and pool |
| Life course | Healthy Foundations segmentation model (Department of Health, 2010c) | Classification based on life stages which can encourage healthy or unhealthy behaviours. Nine life stages were identified | Young Settlers: People aged between 16 and 44 who have a partner. No children in the household, no caring responsibilities and are not retired |
| Pen portraits | Maximizing the appeal of weight management services (Department of Health, 2010a) | Based on interviews and focus groups, this study identified nine people segments based on motivations, barriers and ideal services | Younger women: Aspiring to ‘body beautiful’. Desire a youthful and glamorous service that is active and energizing |
| Segmentation type . | Used by . | Description . | Sample segment . |
|---|---|---|---|
| Geodemographic | Mosaic UK profiling tool (Experian, 2004) | Classifications identify neighbourhood household types and person types based on demographic data (e.g. age, sex, socioeconomic status, property characteristics, location) and financial measures indicating behaviour | Bright Young Things: Well-educated young singles paying high rents to live in smart inner-city apartments |
| Psychographic | Sport England: market segmentation (Sport England, 2009) | Used results from the Active People survey to identify nineteen sporting segments in order to better understand the nation's attitudes to sports and motivations for action | Sports Team Lads: Young blokes enjoying football, pints and pool |
| Life course | Healthy Foundations segmentation model (Department of Health, 2010c) | Classification based on life stages which can encourage healthy or unhealthy behaviours. Nine life stages were identified | Young Settlers: People aged between 16 and 44 who have a partner. No children in the household, no caring responsibilities and are not retired |
| Pen portraits | Maximizing the appeal of weight management services (Department of Health, 2010a) | Based on interviews and focus groups, this study identified nine people segments based on motivations, barriers and ideal services | Younger women: Aspiring to ‘body beautiful’. Desire a youthful and glamorous service that is active and energizing |
The present report forms part of a larger study in one London borough, Barking and Dagenham, which has the highest prevalence of adult obesity in London at 28.7% [Association of Public Health Observatories (APHO), 2012]; the lowest level of healthy eating and of physical activity; and is the 22nd most deprived area of England, based on the Index of Multiple Deprivation (Department for Communities and Local Government, 2011). The Borough Health and Wellbeing strategy called for a radical shift in expectations around lifestyle (Barking and Dagenham Local Strategic Partner-ship, 2010, p. 8). The aim of the whole study was to understand the motivations, experiences and behaviours of people who are obese and have a common socio-demographic background. This paper considers the social marketing segmentation of the population who share the characteristics of obesity and common socio-demographic background.
METHODS
To explore the ways in which those who are obese perceive their obesity and any weight loss intention, the study sought to access obese people in the public places in which they live their lives. Studies typically recruit from people who have been identified as obese by health services. Such patients are more likely to associate their obesity with a health or medical condition and to have received advice and/or referral to weight management services. In order to reduce the bias arising from recruiting those whose motivation to tackle their obesity has already been prompted, this study recruited obese people in the street.
Participants over 18 years old were recruited on public thoroughfares including in the marketplace, on the high street and in the main shopping centre. A validated visual rating scale (Harris et al., 2008), which portrays people of different visual shape and size and classifies their obesity, was used to identify potential participants. Verification between two researchers took place where possible. Posters and snowball sampling were also used to widen recruitment. Participants took part in a short 15 min street-intercept interview and/or a longer biographic interview which lasted about an hour. Recruitment continued until saturation was reached regarding emergent themes. Participants provided informed written consent and after the interview were given a shopping voucher to thank them for their participation in the potentially sensitive discussion.
Biographic interviews took place in café areas or a quiet area of the shopping centre or in the library. Participants were prompted to describe their weight, how it compared with others in the area and, using their preferred terminology to describe their weight, to suggest what caused their obesity. Participants were asked whether they wanted to change weight and if so, why, and to recount any previous attempts they had made to lose weight and what had helped them and what caused most challenges. The aim of this part of the conversation was to identify and explore the nature of any motivational statements and change talk and what participants would and wouldn't do to lose weight. Eliciting questions helped to probe how important losing weight was to the participant and the costs that might be involved.
The interviews were digitally recorded, transcribed verbatim and entered into QSR Nvivo v9. Framework analysis was used across all interviews using the constructs of intention, motivation, self-efficacy and barriers and enablers to weight management. This is a highly structured and systematic approach which allows for searches within and between groups and provides an explicitly clear map of how analysis and interpretation were performed (Ritchie and Spencer, 1994). Data were grouped into themes and subthemes and data in each subtheme were examined for similarities, differences and explanatory accounts. The credibility of analysis was established by ‘weighting’ themes according to frequency and extensiveness of comments, specific reference to person and experience, intensity or depth of feeling (Ritchie et al., 2003; Denzin and Lincoln, 2008). The aim of segmentation is to uncover nuanced differences in a population that pertain to the beliefs people hold and their perceived self-efficacy and capability. Analysis of the biographic interviews was used to develop 11 distinct population segments. The street-intercept interviews were then examined for any similarities and differences to these 11 segments and some segments were consequently refined. All study participants were able to be assigned to a segment, each of which was discrete.
Ethical approval for this study was granted by London South Bank University Research Ethics Committee in August 2011 (UREC, 1120).
RESULTS
Six hundred and thirty-nine people were appro-ached in total. Two hundred and eleven consented to interview, a response rate of 33%. One hundred and eighty-one people took part in street-intercept interviews and 52 people took part in longer biographic interviews (22 people did both). The majority of participants were female (79%), aged 25–64 (81%), White (77% compared with a borough figure of 72.8%) and employed (58% compared with a borough figure of 78.2%). There were some differences between those approached who agreed to take part and those who refused to take part. Younger and more overweight people were less likely to agree to take part (p = 0.011 and p < 0.001, respectively). There was no difference in ethnicity. As the distribution of obesity in this borough is not known, it is not possible to say the extent to which this sample is representative of all obese people.
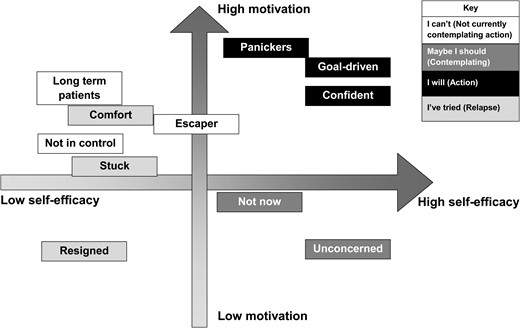
The striking finding of the study is that within one borough the adult obese population showed considerable variation in its intentions and readiness to change and perceived control over weight loss, but considerable similarity in the exchange value they attributed to tackling their obesity. Eleven discrete segments emerged, that can be distinguished according to their motivation to change and their perceived self-efficacy. The majority of participants had high motivation but low self-efficacy and can be differentiated from those whose willingness and readiness to change was less. Segments which were similar in their ‘stage of change’ (Prochaska and Velicer, 1997) were grouped into four categories: currently not prepared to take action (I can't); contemplating action (Maybe I should); relapse (I've tried) and action (I will). Whilst the I can't category was not contemplating action hindered by their low perceived self-efficacy, despite being highly motivated to lose weight those in the Maybe I should category evidenced low levels of motivation coupled with high perceived self-efficacy and so could be described as stuck in a contemplation stage. Individuals in the Relapse stage (I tried) were often ‘weight cyclers’ who reported frequent weight loss and subsequent regain. They varied in terms of motivation but generally evidenced low perceived self-efficacy in losing weight. All of those in the I will category (Action stage) evidenced high levels of motivation and high perceived self-efficacy.
Within each of these categories of change were different segments that could be distinguished according to their attributions for their obesity and the importance they attached to being obese. There are segments in which obesity was attributed to factors beyond their control (‘Escapers’; ‘Not in control’; ‘Long-term patients’) but whose motivation remains high should barriers to weight loss attempts such as time or a specific health condition be removed. ‘Escapers’ were perplexed by their obesity and did not acknowledge any roots in their own behaviour. A narrative of extenuating circumstances became apparent in relation to these individuals. Although these participants recognized their own obesity and acknowledged their desire to lose weight, they felt that there were barriers that prevented them from doing so. These barriers were both intrinsic and extrinsic. Intrinsic barriers encompassed mental health issues and chronic illness, as well as low perceived self-efficacy or willpower. There was also a strong mitigation discourse about the lack of opportunity to regulate eating behaviour in the face of powerful cues in this borough to eat easily available, cheap, palatable, calorie-dense food.
Those who had previously tried to lose weight could be distinguished between those who would continue with weight loss attempts (‘Stuck’; ‘and ‘Comfort eaters’) and those who would not (‘Resigned’); those who were engaged in weight loss attempts (‘Panickers’; ‘Confident’; and ‘Goal driven’) could also be clearly distinguished according to whether they were intrinsically or extrinsically motivated. There were also segments who were confident that they could lose weight when they so chose and for whom the issue was not salient (‘Not Now’ and ‘Unconcerned’). Figure 1 depicts each segment in relation to a continuum of motivation to lose weight and perceived self-efficacy in losing weight. The relative positions are indicative of the ways in which participants described their levels of motivation and self-efficacy. For example, those who have been termed ‘Panickers’ had been told to lose weight and were extremely concerned about their long-term health but their self-efficacy was not high because of previous failures at weight loss. They can be distinguished from other weight cyclers such as the ‘Resigned’ segment whose current motivation and belief that they can change is very low. The figure shows the relative position of each segment but their relative size is not shown as the aim of segmentation is to uncover the nuanced differences between groups.
The majority of participants were highly motivated to lose weight and had similar reasons driving this motivation as shown in Table 2. The value in losing weight lay in improved functioning in daily life, particularly in relation to family demands which, for some, outweighed the perceived potential difficulties. Participants identified different enabling factors and barriers based on their attributions for their obesity, perception of themselves and their experiences of weight loss. Table 2 shows how there are different messages and interventions that are more likely to appeal to each of these segments.
Barriers and enablers for weight management for each population
| . | Segment . | What motivates them? . | Do they intend to lose weight? . | What helps them lose weight? . | What prevents them from losing weight? . | What are their preferences for weight management services? . |
|---|---|---|---|---|---|---|
| ‘I can't’ | Escapers | Health Feeling better about self | Can't do anything and have tried everything | Seeing results Friends and family support | Previous lack of success Embarrassment Cost of services | Group and community activities Sensitive services |
| Not in control | Health Appearance | Not possible and have been more obese in the past | Professional advice | Perceived lack of control Lack of encouragement | Prefer exercise to dieting Health care services | |
| Long-term patients | Health Fitness Mobility | Would like to lose weight but feel they can't | Prompt from GP or nurse, who are seen frequently Perseverance and determination | Lack of mobility and fitness Cost of services | Exercise they can do, to which they are referred by a healthcare professional | |
| ‘Maybe I should’ | Unconcerned | Health Fitness Not vanity | No. Do not perceive themselves as obese | Having a specific health problem Easy opportunities for exercise | Do not recognize they are obese Feel healthy Always been this way Don't want to change | Group activities Expert advice Prefer lifestyle activities to structured programmes |
| Not now | Better self-esteem Children or relationships | Should do but haven't given it much thought | Clear information Opportunities that fit with family demands | Irregular working hours and busy life No ‘me time’ Lack of disposable income | Family activities | |
| ‘I will’ | Panickers | Being told they have to lose weight Fear | Will try | Warning from GP or nurse Threat of health problem | Adhering to diets | A structured programme in a setting that provides medical reassurance |
| Confident | Health Feeling better and happier Family Making the decision | Yes | Making a personal decision A lifestyle overhaul | Family commitments Sustaining change Staying committed | Individualized action plan Flexible activities | |
| Goal-driven | Future mobility | Yes | Enjoyment Feeling better after exercise A life event A target | Work Lack of disposable income Temptation of fast food | Gym or sports with friends | |
| ‘I've tried’ | Stuck | Specific health complaints Children or grandchildren | Not immediately—frustrated with constant weight loss attempts | Motivation from others | Temptation Don't believe anything will work and give up | Structured programme with one-to-one support |
| Resigned | Feeling better Preventing health problems Fitting into clothes | No. It is too big a hurdle and only depresses | Prompts from health care professionals Being told exactly what to do | Low self-esteem and self-efficacy Lack of information Lack of confidence in any method Cost of services | Structured group activities Motivational strategies | |
| Comfort eaters | Preventing future weight gain and health problems Being able to run around after the kids | Unlikely as like food too much | Feeling responsibility for others Support from family, friends and professionals | Comfort eating Temptation Stress | Need a variety of methods addressing diet, exercise and psychological support |
| . | Segment . | What motivates them? . | Do they intend to lose weight? . | What helps them lose weight? . | What prevents them from losing weight? . | What are their preferences for weight management services? . |
|---|---|---|---|---|---|---|
| ‘I can't’ | Escapers | Health Feeling better about self | Can't do anything and have tried everything | Seeing results Friends and family support | Previous lack of success Embarrassment Cost of services | Group and community activities Sensitive services |
| Not in control | Health Appearance | Not possible and have been more obese in the past | Professional advice | Perceived lack of control Lack of encouragement | Prefer exercise to dieting Health care services | |
| Long-term patients | Health Fitness Mobility | Would like to lose weight but feel they can't | Prompt from GP or nurse, who are seen frequently Perseverance and determination | Lack of mobility and fitness Cost of services | Exercise they can do, to which they are referred by a healthcare professional | |
| ‘Maybe I should’ | Unconcerned | Health Fitness Not vanity | No. Do not perceive themselves as obese | Having a specific health problem Easy opportunities for exercise | Do not recognize they are obese Feel healthy Always been this way Don't want to change | Group activities Expert advice Prefer lifestyle activities to structured programmes |
| Not now | Better self-esteem Children or relationships | Should do but haven't given it much thought | Clear information Opportunities that fit with family demands | Irregular working hours and busy life No ‘me time’ Lack of disposable income | Family activities | |
| ‘I will’ | Panickers | Being told they have to lose weight Fear | Will try | Warning from GP or nurse Threat of health problem | Adhering to diets | A structured programme in a setting that provides medical reassurance |
| Confident | Health Feeling better and happier Family Making the decision | Yes | Making a personal decision A lifestyle overhaul | Family commitments Sustaining change Staying committed | Individualized action plan Flexible activities | |
| Goal-driven | Future mobility | Yes | Enjoyment Feeling better after exercise A life event A target | Work Lack of disposable income Temptation of fast food | Gym or sports with friends | |
| ‘I've tried’ | Stuck | Specific health complaints Children or grandchildren | Not immediately—frustrated with constant weight loss attempts | Motivation from others | Temptation Don't believe anything will work and give up | Structured programme with one-to-one support |
| Resigned | Feeling better Preventing health problems Fitting into clothes | No. It is too big a hurdle and only depresses | Prompts from health care professionals Being told exactly what to do | Low self-esteem and self-efficacy Lack of information Lack of confidence in any method Cost of services | Structured group activities Motivational strategies | |
| Comfort eaters | Preventing future weight gain and health problems Being able to run around after the kids | Unlikely as like food too much | Feeling responsibility for others Support from family, friends and professionals | Comfort eating Temptation Stress | Need a variety of methods addressing diet, exercise and psychological support |
Barriers and enablers for weight management for each population
| . | Segment . | What motivates them? . | Do they intend to lose weight? . | What helps them lose weight? . | What prevents them from losing weight? . | What are their preferences for weight management services? . |
|---|---|---|---|---|---|---|
| ‘I can't’ | Escapers | Health Feeling better about self | Can't do anything and have tried everything | Seeing results Friends and family support | Previous lack of success Embarrassment Cost of services | Group and community activities Sensitive services |
| Not in control | Health Appearance | Not possible and have been more obese in the past | Professional advice | Perceived lack of control Lack of encouragement | Prefer exercise to dieting Health care services | |
| Long-term patients | Health Fitness Mobility | Would like to lose weight but feel they can't | Prompt from GP or nurse, who are seen frequently Perseverance and determination | Lack of mobility and fitness Cost of services | Exercise they can do, to which they are referred by a healthcare professional | |
| ‘Maybe I should’ | Unconcerned | Health Fitness Not vanity | No. Do not perceive themselves as obese | Having a specific health problem Easy opportunities for exercise | Do not recognize they are obese Feel healthy Always been this way Don't want to change | Group activities Expert advice Prefer lifestyle activities to structured programmes |
| Not now | Better self-esteem Children or relationships | Should do but haven't given it much thought | Clear information Opportunities that fit with family demands | Irregular working hours and busy life No ‘me time’ Lack of disposable income | Family activities | |
| ‘I will’ | Panickers | Being told they have to lose weight Fear | Will try | Warning from GP or nurse Threat of health problem | Adhering to diets | A structured programme in a setting that provides medical reassurance |
| Confident | Health Feeling better and happier Family Making the decision | Yes | Making a personal decision A lifestyle overhaul | Family commitments Sustaining change Staying committed | Individualized action plan Flexible activities | |
| Goal-driven | Future mobility | Yes | Enjoyment Feeling better after exercise A life event A target | Work Lack of disposable income Temptation of fast food | Gym or sports with friends | |
| ‘I've tried’ | Stuck | Specific health complaints Children or grandchildren | Not immediately—frustrated with constant weight loss attempts | Motivation from others | Temptation Don't believe anything will work and give up | Structured programme with one-to-one support |
| Resigned | Feeling better Preventing health problems Fitting into clothes | No. It is too big a hurdle and only depresses | Prompts from health care professionals Being told exactly what to do | Low self-esteem and self-efficacy Lack of information Lack of confidence in any method Cost of services | Structured group activities Motivational strategies | |
| Comfort eaters | Preventing future weight gain and health problems Being able to run around after the kids | Unlikely as like food too much | Feeling responsibility for others Support from family, friends and professionals | Comfort eating Temptation Stress | Need a variety of methods addressing diet, exercise and psychological support |
| . | Segment . | What motivates them? . | Do they intend to lose weight? . | What helps them lose weight? . | What prevents them from losing weight? . | What are their preferences for weight management services? . |
|---|---|---|---|---|---|---|
| ‘I can't’ | Escapers | Health Feeling better about self | Can't do anything and have tried everything | Seeing results Friends and family support | Previous lack of success Embarrassment Cost of services | Group and community activities Sensitive services |
| Not in control | Health Appearance | Not possible and have been more obese in the past | Professional advice | Perceived lack of control Lack of encouragement | Prefer exercise to dieting Health care services | |
| Long-term patients | Health Fitness Mobility | Would like to lose weight but feel they can't | Prompt from GP or nurse, who are seen frequently Perseverance and determination | Lack of mobility and fitness Cost of services | Exercise they can do, to which they are referred by a healthcare professional | |
| ‘Maybe I should’ | Unconcerned | Health Fitness Not vanity | No. Do not perceive themselves as obese | Having a specific health problem Easy opportunities for exercise | Do not recognize they are obese Feel healthy Always been this way Don't want to change | Group activities Expert advice Prefer lifestyle activities to structured programmes |
| Not now | Better self-esteem Children or relationships | Should do but haven't given it much thought | Clear information Opportunities that fit with family demands | Irregular working hours and busy life No ‘me time’ Lack of disposable income | Family activities | |
| ‘I will’ | Panickers | Being told they have to lose weight Fear | Will try | Warning from GP or nurse Threat of health problem | Adhering to diets | A structured programme in a setting that provides medical reassurance |
| Confident | Health Feeling better and happier Family Making the decision | Yes | Making a personal decision A lifestyle overhaul | Family commitments Sustaining change Staying committed | Individualized action plan Flexible activities | |
| Goal-driven | Future mobility | Yes | Enjoyment Feeling better after exercise A life event A target | Work Lack of disposable income Temptation of fast food | Gym or sports with friends | |
| ‘I've tried’ | Stuck | Specific health complaints Children or grandchildren | Not immediately—frustrated with constant weight loss attempts | Motivation from others | Temptation Don't believe anything will work and give up | Structured programme with one-to-one support |
| Resigned | Feeling better Preventing health problems Fitting into clothes | No. It is too big a hurdle and only depresses | Prompts from health care professionals Being told exactly what to do | Low self-esteem and self-efficacy Lack of information Lack of confidence in any method Cost of services | Structured group activities Motivational strategies | |
| Comfort eaters | Preventing future weight gain and health problems Being able to run around after the kids | Unlikely as like food too much | Feeling responsibility for others Support from family, friends and professionals | Comfort eating Temptation Stress | Need a variety of methods addressing diet, exercise and psychological support |
DISCUSSION
Whilst age, gender, social class and ethnicity all have a potentially significant impact on individuals' propensity to obesity and weight management aspirations, this study showed that there is far more variation in terms of what might motivate different individuals or that they would find appealing in weight management services. ‘Stages of change’ theory (Prochaska and Velicer, 1997) has been applied to target interventions according to a readiness to change but a more nuanced analysis has enabled us to distinguish degrees of motivation based on perceived causes and consequences of obesity, barriers and enablers for change that include self-efficacy and social norms. Most participants subscribed to the dominant biomedical perspective of excess weight, as well as media representations of obesity. Framed in these perspectives, the obese body was seen as unhealthy, unattractive and disgusting. Accordingly, it was unsurprising that most of the sample expressed a desire to lose weight. However, the strength of obese individuals' motivation for weight loss is frequently underestimated by physicians and by politicians' intent to encourage a shared responsibility of state and individuals (Department of Health, 2010b). A visual representation of population segments (Figure 1) graphically illustrates however, that far from the obese population having ‘given up’ on their health and lacking motivation, rather they perceive there to be insurmountable challenges in addressing their obesity. The clearly identifiable segments of those who made frequent weight loss attempts and those who intend to lose weight but do not, indicate how motivation is not enough for those seeking to make a change or for those who want to stay with a new behaviour (Webb and Sheeran, 2006). Figure 1 shows the importance of self-efficacy or capability (Michie et al., 2011) coupled with motivation for behaviour change (Byrne, 2002; Teixeira et al., 2005). For many of these participants, confidence in their ability to make changes and to maintain weight loss through the demands of everyday life was the biggest perceived challenge.
Behaviour change is a complex process and there are dozens of theories and models to draw from to design interventions, although it has been claimed that interventions pay insufficient attention to theory in their design (Michie et al., 2011). Whilst there is much to be gained through understanding how an individual's plans, beliefs, wants and needs shape their intentions (West, 2006), the promise of social marketing is its overall focus on influencing population groups to achieve change objectives. Social marketing theory posits that for sustainable behaviour change to occur, success lies not only in understanding behaviour, but then offering an exchange that is valued by the target population. Current obesity strategy and guidelines for intervention operate under the assumption that awareness of high BMI would raise awareness of being high risk for many health problems and thus lead to behaviour change. In the present study each segment had different motivations for weight loss, but family values were particularly important to all participants, overriding the benefit of change for individual health alone. Using a psychographic approach revealed the place and priority given to weight loss by participants in the face of more pressing concerns and needs. The study reveals that any communication and messages of an obesity strategy need to stress the benefits of weight loss for daily functioning and appeal to the individual's role in family life.
This type of segmentation begins to identify the interventions likely to appeal to particular groups who are aware of their obesity but unsure what next steps to take and those who are very well informed but are dispirited by frequent weight loss attempts. These preferences do not fall neatly across gender, ethnicity or socio-economic lines. Nor do they match to different ‘stages of change’ or intentional states. This process of segmentation has shown that conventional targeting according to either socio-demographic characteristics or stages of change is unlikely to accord with people's values and needs. The preferences of participants in this study who varied in stages of readiness is determined by the exchange value given to weight management which partly derives from their individual attributions for obesity together with their perceived self-efficacy.
Equally important in this study were the perceived opportunities to change and the critical role social networks play in maintaining behaviours and propagating change. Social interactions affect behaviours, and social networks appear to be a key factor in the ‘spread’ of obesity (Christakis and Fowler, 2007). For those segments that fell within the ‘I can't’ category, motivation was reduced by a perceived lack of control over their obesity. This lack of control was in itself influenced by participants' physical and social capital, which was in turn compromised by negative life events such as unemployment or single parenthood. Harnessing the social ties of likely ‘influencers’ within their peer group, or designing interventions which acknowledge social capital and community norms may be effective for halting the spread of obesity (Christakis and Fowler, 2007).
To our knowledge, this study is one of the largest of its kind and the first to use street-intercept methods to investigate obesity. The anticipated difficulties in approaching people because they had been visually identified as obese were not experienced. Younger people and those who were more obese were less likely to consent to participation, but they are represented in the study sample. As no information is available about the age distribution of obese people in the borough it is difficult to assess whether the higher refusal rate amongst younger people has resulted in them being underrepresented in the study. Conducting recruitment in public places may have meant that those less likely to be outside the home, e.g. older people and people with serious illness were underrepresented.
CONCLUSION
Despite the obese population in this borough being a group that appeared to be relatively homogenous in terms of socioeconomic status and geographic location, each segment had different attributions, values, motivations and barriers to weight loss irrespective of life stage (Department of Health, 2010c) from which appropriate interventions for weight loss could be suggested. This study confirms that consumer research methods to understand what motivates people to change and the values they attach to change together with social marketing segmentation offer a more nuanced form of targeting than simplistic high risk approaches. These can inform the design of weight management interventions that more closely accord to individual needs and preferences (Stead et al., 2007).
FUNDING
Funding for this study was provided by NHS Barking and Dagenham, London, UK.