-
PDF
- Split View
-
Views
-
Cite
Cite
Victoria Shepherd, Fiona Wood, Kerenza Hood, Establishing a set of research priorities in care homes for older people in the UK: a modified Delphi consensus study with care home staff, Age and Ageing, Volume 46, Issue 2, March 2017, Pages 284–290, https://doi.org/10.1093/ageing/afw204
Close - Share Icon Share
Abstract
currently, there is little evidence base for much of the care provided for older people in care homes. Given the wide range of topics that require further investigation, and limited resources, one solution is to identify the priorities for future research.
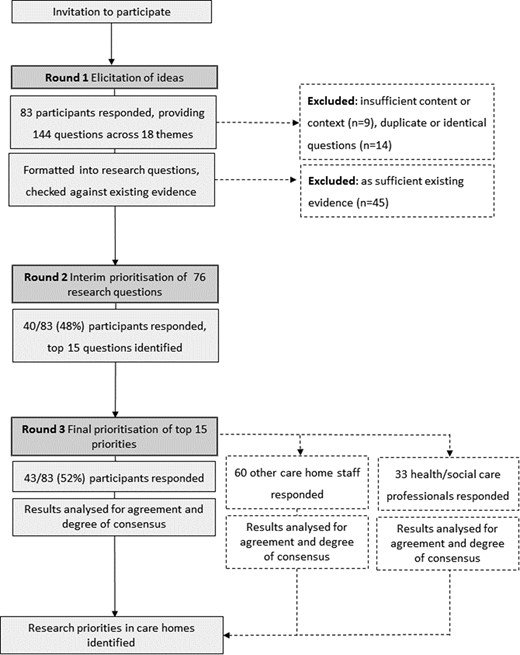
a modified Delphi technique was used to identify research topics and develop consensus among care home staff participants. The survey was conducted across three rounds. Firstly to elicit topics that were considered by participants to require further research, secondly to prioritise the long list of research questions, followed by a third round to reach a consensus on the highest ranked 15 questions.
eighty-three participants responded to the initial survey, providing 144 questions. Following analysis and review against existing evidence, 76 research questions remained. Of note, 40/83 participants responded to the interim prioritisation round and 43/83 participants responded to the final round, which ranked the top 15 research questions by importance. Two other groups of health and social care professionals also participated in the final ranking. The results from these groups had a similar ordering to those of the original cohort of participants.
this is the first study to establish a set of research priorities for older people in the UK care homes. It is hoped that sharing these results with clinicians, researchers and funding bodies will help to begin the process of ensuring that the future research agenda can be focused on the areas of greatest need. Further work to identify the priorities of other key stakeholders is required.
Introduction
The ageing UK population is associated with a corresponding rise in the number of people requiring long-term care [1], with those entering long-term care having increasingly complex healthcare needs [2]. Currently, there is little evidence for much of the care provided in care homes [3, 4], and concerns about the quality of care [5] have led to calls for a more structured and evidence-based approach to healthcare provision within care homes [6]. However, research involving frail, older people living in care homes is more complex and resource intensive than in other healthcare settings [7–10]. Given the wide range of questions that require further investigation, and limited research resources, one solution is to encourage stakeholders to participate in decisions regarding the prioritisation of topics for future research.
Research priority setting methods can assist researchers and policymakers to effectively target research that has the greatest potential benefit [11, 12], with a number of research funders incorporating the findings into their prioritisation processes [13].
Recent priority setting partnerships [14] have focussed on identifying priorities for research into the treatment of specific age-related health conditions [15, 16]. However, care provided in care homes is unique as it encompasses a range of conditions and incorporates aspects of social care as well as healthcare.
The aim of this study was to develop an informed set of research priorities within the care home setting. Care home staff were selected as the ‘expert panel’ as they have expertise in caring for older people in care homes [17] and a unique perspective not shared by the wider multidisciplinary team during limited visits or appointments. There is also a strong relationship between engagement of stakeholders in the planning and design of research and the subsequent quality, utilisation and outcomes [18, 19]; therefore, involving care home staff is essential in order to develop care homes as a research environment.
Methods
The Delphi method [20] is a structured process that uses an iterative series (or rounds) of questionnaires to gather information, and rounds are continued until group consensus is reached [21]. This widely used method [22] allows for the inclusion of a large number of individuals across diverse geographic locations and, unlike a face-to-face meeting, avoids the situation where a specific expert may dominate the consensus process [23]. However, it is not without its methodological difficulties. Commentators caution that it should be viewed as expert opinion rather than indisputable fact and that a clear decision trail is vital to ensure credibility [24].
Care homes providing nursing care (nursing homes) and those without nursing care (residential homes) were included in order to maximise generalisability of the results. Incorporating diverse viewpoints, such as those from different care environments, is considered to improve the quality and acceptability of results in Delphi exercises [24]. Other stakeholders, such as care home residents, their families and friends, and healthcare professionals were not included as it was considered that their perspectives may be too heterogeneous to be combined into one priority setting exercise conducted entirely using remote survey techniques. A number of priority setting exercises have exclusively used a single group of healthcare professionals [25–27].
There are many differing forms of Delphi in existence, with few researchers using a uniform method of the Delphi technique [22]. This study used a modified Delphi approach, which utilised a combination of online surveys, postal questionnaires and workshops while retaining the essential elements of the technique: achieving consensus through using a forecasting process to determine, predict and explore group attitudes, needs and priorities [22]. The study was piloted with staff from care homes participating in a separate study conducted by the same researchers [28].
This project was conducted by the South East Wales Trials Unit as part of a portfolio of research involving the older person. Ethical approval was granted by Cardiff University School of Medicine Research Ethics Committee (ref 15/05).
Participant selection
Care home staff were defined as those who considered themselves as providing care for older adults in care homes, which included registered nurses, care assistants and matrons/managers. Participants were identified through partner organisations and networks, such as the National Institute for Health Research Enabling Research in Care Homes (NIHR ENRICH) programme [29] in England and Scotland (excludes Northern Ireland) who disseminated the information via email and newsletters, and care homes in Wales that had previously participated in research and who were, therefore, known to the researchers. Information about the project was also shared by websites that are commonly accessed by care home staff.
Potential participants were invited to take part by completing an online survey accessed via a URL link, completing and returning a printed questionnaire or (in the first round only) by attending a local workshop event hosted by Comprehensive Research Networks, part of the ENRICH network.
Project design
The survey was conducted across three rounds. Demographic data and method of completion of the survey were also recorded.
Round 1: Elicitation of research topics
Participants were asked to identify areas where they felt there were uncertainties or questions about the care provided on a day-to-day basis in care homes. Participants could provide as many or as few questions as they wished within a large free text space provided.
Refining research topics/questions
The ‘raw’ questions were collated, analysed and formatted by one of the researchers with a clinical background and an interest in acute care in older populations (V.L.S.) into researchable questions. A random 20% selection was also formatted in parallel by another researcher, a medical sociologist with an interest in patient-centred care (F.W.), blinded to the refined question generated by the first researcher. These ‘double assessed’ questions were compared and, where significant differences were found in either the interpretation of the question or question wording, agreement was reached on the final refined question. Similar or duplicate questions were combined where appropriate. Questions that were considered impossible to formulate into a research question (insufficient detail or too vague) were removed.
A pragmatic literature search was undertaken for each topic identified. Research questions that were considered to have sufficient existing evidence, and therefore not true uncertainties, were removed. The remaining ‘long list’ of questions was taken forward into the next round for building consensus.
Round 2: Building consensus on priorities
Round 2 was the interim stage, to proceed from a long list of research questions to a shorter list. The research questions were categorised by the identified themes, in order to provide structure and aid completion by participants. These were sent to participants via post or email as indicated by their stated preference in their response to the first round. The participants were asked to rate how much they agreed or disagreed with the statement ‘This topic is very important to me’ for each question, using a 5-point Likert-type scale, 1 being the most important and 5 the least important.
Median scores and interquartile ranges (IQRs) were calculated for the participants’ responses to each question. Median scores were calculated per question in order to characterise the answer category above and below which 50% of the answers fall. IQRs, which form the distance between the 25th and the 75th percentiles, were used to represent the spread of the data and to assess the level of consensus per question. Responses where the median was ≤2 (high level of agreement that the topic is important) with a small IQR were considered important research questions that have reached consensus. Those with a median ≥4 with small IQR were considered to have reached consensus on a lack of importance. The 15 most important questions were shortlisted for the third round.
Round 3: Reaching consensus on priorities
In the final round, the highest rated research questions from round 2 were randomly listed and the participants were asked to rank how much of a priority each research question was from 1 to 10 (where 1 was the most important and 10 was the least important of their chosen 10 topics). Participants were asked to use each number only once, leaving those that they felt were not so important blank. Incorrectly scored or illegible responses were not included in the analysis.
Responses were inversely scored and collated. Priorities were defined as the research questions receiving the highest total scores.
Results
Round 1
Participant data—all rounds
| . | Round 1 (n = 83) . | Round 2 (n = 40) . | Round 3 (n = 43) . |
|---|---|---|---|
| Country, n (%) | 63 | 38 | 43 |
| England | 47 (74.6) | 33 (86.8) | 30 (69.7) |
| Scotland | 2 (3.2) | 1 (2.6) | 3 (69.7) |
| Wales | 14 (22.2) | 3 (8.0) | 10 (23.3) |
| Missing/ineligible data | 0 | 1 | 0 |
| Role, n (%) | 63 | 38 | 42 |
| Care Assistant | 6 (9.5) | 2 (5.2) | 3 (7.1) |
| Senior Care Assistant | 4 (6.3) | 1 (2.6) | 0 |
| Registered Nurse | 9 (14.2) | 1 (2.6) | 1 (2.4) |
| Nurse Manager | 2 (3.1) | 6 (15.7) | 10 (23.8) |
| Matron | 0 | 0 | 0 |
| Manager | 28 (44.4) | 26 (68.4) | 25 (59.5) |
| Other | 14 (22.2) | 2 (5.2) | 3 (7.1) |
| Type of care home, n (%) | 62 | 38 | 43 |
| Nursing | 11 (17.7) | 5 (13.1) | 11 (25.6) |
| Residential | 12 (19.3) | 15 (39.4) | 15 (34.9) |
| Combined residential and nursing | 36 (58.0) | 18 (47.3) | 14 (32.6) |
| Other | 3 (4.8) | 0 | 3 (7.0) |
| Length worked in care sector, n (%) | 62 | 38 | 43 |
| Less than 6 months | 1 (1.6) | 1 (2.6) | 0 |
| Between 6 and 12 months | 2 (3.2) | 0 | 2 (4.6) |
| 1–2 years | 4 (6.4) | 2 (5.3) | 3 (7.0) |
| 2–5 years | 11 (17.7) | 6 (15.8) | 8 (18.6) |
| 5 years or more | 44 (71.0) | 29 (76.3) | 30 (70.0) |
| Method of completing survey | |||
| Paper, n (%) | 43 | 22 | 19 |
| Workshop/event | 24 (55.8) | 0 | 1 (5.2) |
| Visit from researcher to care home | 5 (11.6) | 1 (4.3) | 1 (5.2) |
| Received it by post | 3 (7.0) | 19 (82.6) | 16 (84.2) |
| Other | 11 (25.6) | 2 (8.6) | 1 (5.2) |
| Online, n (%) | 20 | 16 | 23 |
| Desktop computer | 12 (60.0) | 11 (68.7) | 10 (43.5) |
| Laptop | 5 (25.0) | 3 (18.8) | 8 (34.5) |
| Mobile phone | 2 (10.0) | 1 (6.2) | 2 (8.7) |
| Tablet | 1 (5.0) | 1 (6.2) | 3 (13.0) |
| Where survey was completed n (%) | 20 | 16 | 24 |
| In work | 12 (60.0) | 13 (81.2) | 19 (79.1) |
| Outside work/from home | 8 (40.0) | 3 (18.7) | 5 (20.8) |
| . | Round 1 (n = 83) . | Round 2 (n = 40) . | Round 3 (n = 43) . |
|---|---|---|---|
| Country, n (%) | 63 | 38 | 43 |
| England | 47 (74.6) | 33 (86.8) | 30 (69.7) |
| Scotland | 2 (3.2) | 1 (2.6) | 3 (69.7) |
| Wales | 14 (22.2) | 3 (8.0) | 10 (23.3) |
| Missing/ineligible data | 0 | 1 | 0 |
| Role, n (%) | 63 | 38 | 42 |
| Care Assistant | 6 (9.5) | 2 (5.2) | 3 (7.1) |
| Senior Care Assistant | 4 (6.3) | 1 (2.6) | 0 |
| Registered Nurse | 9 (14.2) | 1 (2.6) | 1 (2.4) |
| Nurse Manager | 2 (3.1) | 6 (15.7) | 10 (23.8) |
| Matron | 0 | 0 | 0 |
| Manager | 28 (44.4) | 26 (68.4) | 25 (59.5) |
| Other | 14 (22.2) | 2 (5.2) | 3 (7.1) |
| Type of care home, n (%) | 62 | 38 | 43 |
| Nursing | 11 (17.7) | 5 (13.1) | 11 (25.6) |
| Residential | 12 (19.3) | 15 (39.4) | 15 (34.9) |
| Combined residential and nursing | 36 (58.0) | 18 (47.3) | 14 (32.6) |
| Other | 3 (4.8) | 0 | 3 (7.0) |
| Length worked in care sector, n (%) | 62 | 38 | 43 |
| Less than 6 months | 1 (1.6) | 1 (2.6) | 0 |
| Between 6 and 12 months | 2 (3.2) | 0 | 2 (4.6) |
| 1–2 years | 4 (6.4) | 2 (5.3) | 3 (7.0) |
| 2–5 years | 11 (17.7) | 6 (15.8) | 8 (18.6) |
| 5 years or more | 44 (71.0) | 29 (76.3) | 30 (70.0) |
| Method of completing survey | |||
| Paper, n (%) | 43 | 22 | 19 |
| Workshop/event | 24 (55.8) | 0 | 1 (5.2) |
| Visit from researcher to care home | 5 (11.6) | 1 (4.3) | 1 (5.2) |
| Received it by post | 3 (7.0) | 19 (82.6) | 16 (84.2) |
| Other | 11 (25.6) | 2 (8.6) | 1 (5.2) |
| Online, n (%) | 20 | 16 | 23 |
| Desktop computer | 12 (60.0) | 11 (68.7) | 10 (43.5) |
| Laptop | 5 (25.0) | 3 (18.8) | 8 (34.5) |
| Mobile phone | 2 (10.0) | 1 (6.2) | 2 (8.7) |
| Tablet | 1 (5.0) | 1 (6.2) | 3 (13.0) |
| Where survey was completed n (%) | 20 | 16 | 24 |
| In work | 12 (60.0) | 13 (81.2) | 19 (79.1) |
| Outside work/from home | 8 (40.0) | 3 (18.7) | 5 (20.8) |
Participant data—all rounds
| . | Round 1 (n = 83) . | Round 2 (n = 40) . | Round 3 (n = 43) . |
|---|---|---|---|
| Country, n (%) | 63 | 38 | 43 |
| England | 47 (74.6) | 33 (86.8) | 30 (69.7) |
| Scotland | 2 (3.2) | 1 (2.6) | 3 (69.7) |
| Wales | 14 (22.2) | 3 (8.0) | 10 (23.3) |
| Missing/ineligible data | 0 | 1 | 0 |
| Role, n (%) | 63 | 38 | 42 |
| Care Assistant | 6 (9.5) | 2 (5.2) | 3 (7.1) |
| Senior Care Assistant | 4 (6.3) | 1 (2.6) | 0 |
| Registered Nurse | 9 (14.2) | 1 (2.6) | 1 (2.4) |
| Nurse Manager | 2 (3.1) | 6 (15.7) | 10 (23.8) |
| Matron | 0 | 0 | 0 |
| Manager | 28 (44.4) | 26 (68.4) | 25 (59.5) |
| Other | 14 (22.2) | 2 (5.2) | 3 (7.1) |
| Type of care home, n (%) | 62 | 38 | 43 |
| Nursing | 11 (17.7) | 5 (13.1) | 11 (25.6) |
| Residential | 12 (19.3) | 15 (39.4) | 15 (34.9) |
| Combined residential and nursing | 36 (58.0) | 18 (47.3) | 14 (32.6) |
| Other | 3 (4.8) | 0 | 3 (7.0) |
| Length worked in care sector, n (%) | 62 | 38 | 43 |
| Less than 6 months | 1 (1.6) | 1 (2.6) | 0 |
| Between 6 and 12 months | 2 (3.2) | 0 | 2 (4.6) |
| 1–2 years | 4 (6.4) | 2 (5.3) | 3 (7.0) |
| 2–5 years | 11 (17.7) | 6 (15.8) | 8 (18.6) |
| 5 years or more | 44 (71.0) | 29 (76.3) | 30 (70.0) |
| Method of completing survey | |||
| Paper, n (%) | 43 | 22 | 19 |
| Workshop/event | 24 (55.8) | 0 | 1 (5.2) |
| Visit from researcher to care home | 5 (11.6) | 1 (4.3) | 1 (5.2) |
| Received it by post | 3 (7.0) | 19 (82.6) | 16 (84.2) |
| Other | 11 (25.6) | 2 (8.6) | 1 (5.2) |
| Online, n (%) | 20 | 16 | 23 |
| Desktop computer | 12 (60.0) | 11 (68.7) | 10 (43.5) |
| Laptop | 5 (25.0) | 3 (18.8) | 8 (34.5) |
| Mobile phone | 2 (10.0) | 1 (6.2) | 2 (8.7) |
| Tablet | 1 (5.0) | 1 (6.2) | 3 (13.0) |
| Where survey was completed n (%) | 20 | 16 | 24 |
| In work | 12 (60.0) | 13 (81.2) | 19 (79.1) |
| Outside work/from home | 8 (40.0) | 3 (18.7) | 5 (20.8) |
| . | Round 1 (n = 83) . | Round 2 (n = 40) . | Round 3 (n = 43) . |
|---|---|---|---|
| Country, n (%) | 63 | 38 | 43 |
| England | 47 (74.6) | 33 (86.8) | 30 (69.7) |
| Scotland | 2 (3.2) | 1 (2.6) | 3 (69.7) |
| Wales | 14 (22.2) | 3 (8.0) | 10 (23.3) |
| Missing/ineligible data | 0 | 1 | 0 |
| Role, n (%) | 63 | 38 | 42 |
| Care Assistant | 6 (9.5) | 2 (5.2) | 3 (7.1) |
| Senior Care Assistant | 4 (6.3) | 1 (2.6) | 0 |
| Registered Nurse | 9 (14.2) | 1 (2.6) | 1 (2.4) |
| Nurse Manager | 2 (3.1) | 6 (15.7) | 10 (23.8) |
| Matron | 0 | 0 | 0 |
| Manager | 28 (44.4) | 26 (68.4) | 25 (59.5) |
| Other | 14 (22.2) | 2 (5.2) | 3 (7.1) |
| Type of care home, n (%) | 62 | 38 | 43 |
| Nursing | 11 (17.7) | 5 (13.1) | 11 (25.6) |
| Residential | 12 (19.3) | 15 (39.4) | 15 (34.9) |
| Combined residential and nursing | 36 (58.0) | 18 (47.3) | 14 (32.6) |
| Other | 3 (4.8) | 0 | 3 (7.0) |
| Length worked in care sector, n (%) | 62 | 38 | 43 |
| Less than 6 months | 1 (1.6) | 1 (2.6) | 0 |
| Between 6 and 12 months | 2 (3.2) | 0 | 2 (4.6) |
| 1–2 years | 4 (6.4) | 2 (5.3) | 3 (7.0) |
| 2–5 years | 11 (17.7) | 6 (15.8) | 8 (18.6) |
| 5 years or more | 44 (71.0) | 29 (76.3) | 30 (70.0) |
| Method of completing survey | |||
| Paper, n (%) | 43 | 22 | 19 |
| Workshop/event | 24 (55.8) | 0 | 1 (5.2) |
| Visit from researcher to care home | 5 (11.6) | 1 (4.3) | 1 (5.2) |
| Received it by post | 3 (7.0) | 19 (82.6) | 16 (84.2) |
| Other | 11 (25.6) | 2 (8.6) | 1 (5.2) |
| Online, n (%) | 20 | 16 | 23 |
| Desktop computer | 12 (60.0) | 11 (68.7) | 10 (43.5) |
| Laptop | 5 (25.0) | 3 (18.8) | 8 (34.5) |
| Mobile phone | 2 (10.0) | 1 (6.2) | 2 (8.7) |
| Tablet | 1 (5.0) | 1 (6.2) | 3 (13.0) |
| Where survey was completed n (%) | 20 | 16 | 24 |
| In work | 12 (60.0) | 13 (81.2) | 19 (79.1) |
| Outside work/from home | 8 (40.0) | 3 (18.7) | 5 (20.8) |
Just over a third (37%, 45/121) were considered to already have sufficient evidence. A total of 76 research questions remained for prioritisation in the next round (Appendix 2).
Round 2
Forty participants responded to the second round, 95% (38/40) provided some demographic data. Participants’ responses showed a high level of importance across all 76 research questions, with few participants providing a response that they ‘strongly disagreed’ with the statement that the question was important (Appendix 3). The 15 research questions receiving responses where the median was ≤2 and had a small IQR ≤1.52 were considered important research questions that had reached consensus (Appendix 4).
Round 3
Forty-three participants responded to the third round and all provided demographic data, with a further six questionnaires received which were incorrectly completed and excluded from the analysis. The top 15 ranked topics are shown in Table 2.
Round 3 ranked research priorities
| Rank . | Research question . |
|---|---|
| 1 | How can person-centred care be provided in care homes appropriate to the person's individualised needs? |
| 2 | How can dignity be enhanced for residents in care home settings? |
| =3 | What are appropriate staffing levels in relation to the number of residents in care homes and their relative care needs? |
| =3 | What are the attitudes of inexperienced care home staff towards providing person-centred care, and can training and support improve awareness of the need for person-centred care? |
| 5 | What are the essential elements required when training carers working with older people in care homes? |
| 6 | How can early and appropriate discussion with older people in care homes about end-of-life care be supported? |
| 7 | How can recruitment of carers with essential qualities such as compassion and empathy be improved by care homes? |
| 8 | How can best interest decisions made for care home residents with dementia be properly documented in care plans? |
| 9 | How can care homes be made to feel more like a home? |
| 10 | What is the public and media perception of care homes compared with other care settings, and what is the impact on care home staff attitudes? |
| 11 | What is the impact of levels of oral hygiene on the nutritional status of older people living in care homes? |
| 12 | How can families and healthcare professionals contribute to improving end-of-life care for older people in care homes? |
| 13 | What activities can improve the quality of life for care home residents with impaired vision or hearing? |
| 14 | How can the provision of visual aids enhance the quality of life of people with end stage dementia? |
| 15 | Can education strategies improve care home staff attitudes towards the use of power and authority in their relationship with older people with cognitive impairments? |
| Rank . | Research question . |
|---|---|
| 1 | How can person-centred care be provided in care homes appropriate to the person's individualised needs? |
| 2 | How can dignity be enhanced for residents in care home settings? |
| =3 | What are appropriate staffing levels in relation to the number of residents in care homes and their relative care needs? |
| =3 | What are the attitudes of inexperienced care home staff towards providing person-centred care, and can training and support improve awareness of the need for person-centred care? |
| 5 | What are the essential elements required when training carers working with older people in care homes? |
| 6 | How can early and appropriate discussion with older people in care homes about end-of-life care be supported? |
| 7 | How can recruitment of carers with essential qualities such as compassion and empathy be improved by care homes? |
| 8 | How can best interest decisions made for care home residents with dementia be properly documented in care plans? |
| 9 | How can care homes be made to feel more like a home? |
| 10 | What is the public and media perception of care homes compared with other care settings, and what is the impact on care home staff attitudes? |
| 11 | What is the impact of levels of oral hygiene on the nutritional status of older people living in care homes? |
| 12 | How can families and healthcare professionals contribute to improving end-of-life care for older people in care homes? |
| 13 | What activities can improve the quality of life for care home residents with impaired vision or hearing? |
| 14 | How can the provision of visual aids enhance the quality of life of people with end stage dementia? |
| 15 | Can education strategies improve care home staff attitudes towards the use of power and authority in their relationship with older people with cognitive impairments? |
Round 3 ranked research priorities
| Rank . | Research question . |
|---|---|
| 1 | How can person-centred care be provided in care homes appropriate to the person's individualised needs? |
| 2 | How can dignity be enhanced for residents in care home settings? |
| =3 | What are appropriate staffing levels in relation to the number of residents in care homes and their relative care needs? |
| =3 | What are the attitudes of inexperienced care home staff towards providing person-centred care, and can training and support improve awareness of the need for person-centred care? |
| 5 | What are the essential elements required when training carers working with older people in care homes? |
| 6 | How can early and appropriate discussion with older people in care homes about end-of-life care be supported? |
| 7 | How can recruitment of carers with essential qualities such as compassion and empathy be improved by care homes? |
| 8 | How can best interest decisions made for care home residents with dementia be properly documented in care plans? |
| 9 | How can care homes be made to feel more like a home? |
| 10 | What is the public and media perception of care homes compared with other care settings, and what is the impact on care home staff attitudes? |
| 11 | What is the impact of levels of oral hygiene on the nutritional status of older people living in care homes? |
| 12 | How can families and healthcare professionals contribute to improving end-of-life care for older people in care homes? |
| 13 | What activities can improve the quality of life for care home residents with impaired vision or hearing? |
| 14 | How can the provision of visual aids enhance the quality of life of people with end stage dementia? |
| 15 | Can education strategies improve care home staff attitudes towards the use of power and authority in their relationship with older people with cognitive impairments? |
| Rank . | Research question . |
|---|---|
| 1 | How can person-centred care be provided in care homes appropriate to the person's individualised needs? |
| 2 | How can dignity be enhanced for residents in care home settings? |
| =3 | What are appropriate staffing levels in relation to the number of residents in care homes and their relative care needs? |
| =3 | What are the attitudes of inexperienced care home staff towards providing person-centred care, and can training and support improve awareness of the need for person-centred care? |
| 5 | What are the essential elements required when training carers working with older people in care homes? |
| 6 | How can early and appropriate discussion with older people in care homes about end-of-life care be supported? |
| 7 | How can recruitment of carers with essential qualities such as compassion and empathy be improved by care homes? |
| 8 | How can best interest decisions made for care home residents with dementia be properly documented in care plans? |
| 9 | How can care homes be made to feel more like a home? |
| 10 | What is the public and media perception of care homes compared with other care settings, and what is the impact on care home staff attitudes? |
| 11 | What is the impact of levels of oral hygiene on the nutritional status of older people living in care homes? |
| 12 | How can families and healthcare professionals contribute to improving end-of-life care for older people in care homes? |
| 13 | What activities can improve the quality of life for care home residents with impaired vision or hearing? |
| 14 | How can the provision of visual aids enhance the quality of life of people with end stage dementia? |
| 15 | Can education strategies improve care home staff attitudes towards the use of power and authority in their relationship with older people with cognitive impairments? |
A wider group than anticipated responded to the final round as a result of the link to the online survey being shared by interested individuals, groups and organisations to individuals who had not participated in the first two rounds but wished to be involved. The scores from these are not included in the main prioritisation findings but were analysed separately to assess the degree of consistency between the findings from the main cohort and two further groups: a similar group of 60 care home staff who had not participated in the previous rounds, and 33 professionals from both health and social care sectors including occupational therapists, doctors, social workers and care regulators.
The results from these groups had a similar ordering to the original cohort of participants (Appendix 5).
Discussion
This is the first study to establish research priorities for older people requiring long-term care in the UK. The top 15 research priorities identified by care home staff include questions on person-centred care, dignity, appropriate staffing levels, and training and support requirements for care home staff. A previous international survey of care home experts identified priority areas for future research, rather than specific research questions [30]. Although the authors note the heterogeneous nature of the nursing home population internationally, some common priorities with our study included a focus on the needs of cognitively impaired residents and palliative/end-of-life care [30].
The highest ranked priority in our study (person-centred care) may have been as a result of recent policy developments across the UK, which have highlighted the importance of a more ‘person-centred’ approach within care services. Despite ‘person-centred care’ being common parlance in older person literature in the UK and internationally, there is a lack of consistency in how the term is understood. This broad theme may have been rated highly as it incorporated a range of philosophical and practical approaches to care, or it may have been due to its heightened prominence as a key aspect of quality care.
Questions relating to staffing levels, quality and training were ranked highly in our study, which may reflect the persistent challenges in providing appropriate staffing and quality care. In contrast to the USA, few EU Member States have systematic compiling and reporting of key quality indicators for long-term care. However, the situation is changing, with more countries developing national, standardised quality measurement systems.
End-of-life care is increasingly being provided in care homes. Residents in care homes are in the last years of life and often present with multiple health needs, cognitive impairment and particular palliative care needs due to their advanced age. Questions relating to early and appropriate discussions about end-of-life care, and the role of families and healthcare professionals in improving end-of-life care were considered important.
Limitations
Residents and their families and friends were not included as participants in this study. The majority of participants were care home managers, who may have less involvement in providing care for residents and whose views may not be representative of the wider group of care home staff. Care home mangers may have a heightened awareness of issues such as staff training and levels of staffing, and exposure to current topical issues such as person-centred care, in comparison to other groups of care home staff, which may have influenced the ranking of these topics. The relatively small number of participants meant we were unable to compare responses by different occupational groups or by care home type.
Using a modified Delphi approach, there was a loss of participants during the three rounds, which may have impacted on emerging consensus over time. It was difficult to conclusively identify and track participants across every round, which may account for small inconsistencies in the demographic data reported.
Responses from two additional groups showed a high degree of consistency with the original cohort of participants; however, the research questions had been determined prior to their involvement. Research topics identified by health and social care professionals, commissioners, care regulators and the broader research community working with care homes may differ significantly from those identified by the participants in this study.
It is not known why participants allocated particular rankings. This may be due to some topics being considered lower in importance, less problematic or that participants felt there was less uncertainty about the evidence underpinning them.
Conclusion
A set of research priorities for older people in care homes have been identified by a key stakeholder group and endorsed by other professionals involved in their care. It is hoped that sharing these results with clinicians, researchers and funding bodies will help to begin the process of ensuring that the future research agenda can be focused on the areas of greatest need. Addressing research questions identified as priorities during this study may contribute to the development of a more evidence-based approach to care provision within care homes.
Further research to identify the research priorities of other key stakeholders such as health and social care professionals, commissioners, care home residents and their friends and families is required in order to identify a more definitive set of priorities.
An increasing number of older people are requiring long-term care, many of whom have complex healthcare needs.
Currently, there is little evidence basis for much of the care provided for older people resident in care homes.
Setting research priorities assists researchers and policymakers to effectively target research that has the greatest benefit.
The research priorities included person-centred care, dignity, appropriate staffing levels, and staff training and support.
This is the first study to establish a set of research priorities for older people in UK care homes.
Supplementary data
Supplementary data mentioned in the text are available to subscribers in Age and Ageing online.
Acknowledgements
We would like to acknowledge the support of the South East Wales Trials Unit who funded the study and provided administrative support (Jackie Swain, Laura Winney) and database development (Sam Clarkstone). The South East Wales Trials Unit is funded by Health and Care Research Wales. We wish to thank the National Institute for Health Research Enabling Research in Care Homes (ENRICH) programme and the Clinical Research Networks for their invaluable support, and other organisations who shared the information about the study (including Scottish Care and carehomes.co.uk). We would particularly like to thank the care home staff and other healthcare professionals who participated in the study, without whom this study would not have been possible.
Authors’ contributions
V.L.S. designed and project managed the study, developed the study questionnaires, led the analysis and drafted the manuscript. F.W. contributed to the study design, analysis, contributed to the reporting of results, commented on draft manuscripts and approved the final manuscript. K.H. contributed to the study design, supervised the analysis, contributed to the reporting of results, commented on draft manuscripts and approved the final manuscript.
Conflicts of interest
All authors declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Funding
The work was supported by the South East Wales Trials Unit as part of the development of a portfolio of research involving older people.



Comments