-
PDF
- Split View
-
Views
-
Cite
Cite
Claudio L. DeLorenzi, Barbed Sutures: Rationale and Technique, Aesthetic Surgery Journal, Volume 26, Issue 2, March 2006, Pages 223–229, https://doi.org/10.1016/j.asj.2006.01.009
Close - Share Icon Share
Abstract
The author provides a comprehensive overview of barbed suture technology, explaining the hypothesized underlying cellular mechanism. He then describes the procedure, including patient selection, materials, and technique.
Claudio L. DeLorenzi, MD, Kitchener, ON is a board certified plastic surgeon and an ASAPS member.
The enthusiasm for barbed sutures has been largely patient driven. Although some aesthetic surgeons have embraced this technique, many more express doubts about its safety and efficacy. As surgeons, we are quite justified in being skeptical about new procedures, especially if they sound too good to be true. We need assurance that the procedure is safe and effective, and we need proof of its ultimate efficacy.
Barbed sutures are typically manufactured from a monofilament suture material. Although several different technologies have been used over the past few years, they all involve hooking the tissues onto barbed sutures so that they subsequently become encased in fibrous tissues, inciting a biologic response. The response achieved by the diminution of tensile forces on skin is the opposite of the response achieved when tension is applied (tissue expansion). The use of barbed sutures may be the first step in understanding and taking advantage of tissue expansion's reciprocal process, which for lack of a better term may be called tissue contraction (see sidebar “Biological Opposite of Tissue Expansion”).
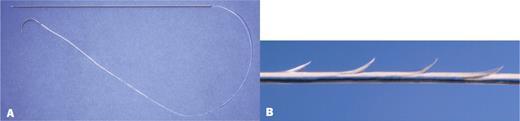
Here, I report primarily on the Contour Thread (Surgical Specialties Inc., Reading, PA), a suture designed to be anchored to a fixed structure, such as the deep temporal fascia. In contrast, the APTOS thread (Kolster Methods, Inc., Anaheim, CA) is designed to be used in freely mobile tissues. With APTOS, bidirectional cogs capture tissues and compress them toward the midpoint of the thread (Figure 1).13 APTOS devices are designed to “bunch up” the tissues, relying on the relative fixation of certain tissue planes for elevation. However, like Contour Threads, APTOS threads rely on the cell death or apoptosis noted in all tissues that have had tensile forces reduced or removed.
A, Bidirectional thread. B, Polarized photomicrograph of typical bidirectional thread. The cogs (barbs) are meant to gather tissue towards the center of the device. C, Example of a failed thread.
Materials
Contour Threads, available since January 2005, are FDA approved for use in the brow, midface, and neck. Threads previously used for facial tissue contouring, described by Sulamanidze et al,13 consisted of bidirectional cogs on a polypropylene thread (Figure 1, A). Sulamanidze's procedure involved 2 steps: first, a spinal needle was passed into the proposed pathway of the bidirectional thread; second, a bidirectional thread was then placed into the lumen of the needle. The thread end was held so that when the needle was removed, the thread remained in place. Because all the cogs pointed toward the center of the thread, the device compressed the tissues so that tissues at the center point were tension free (Figure 1, A and B). With these bidirectional threads, no knots are used. It is very important that there are a similar number of barbs on either end of these devices because otherwise, as in a tug of war, the stronger side (with more barbs) will prevail and the thread will be pulled towards the prevailing side. These devices are slightly easier to deploy but require greater precision to ensure that they do not migrate to a distant site. (The change in skin tension is a significant recurring theme.)
In contrast to bidirectional barbed sutures, which were only about 12 to 15 cm in total length, Contour Threads have a 7-inch straight deployment needle, a 2-inch nonbarbed portion, a 4-inch (10-cm) barbed portion, and a 4-inch (10-cm) nonbarbed portion attached to a 26-mm half-circle needle to be used for fixation purposes (Figure 2).
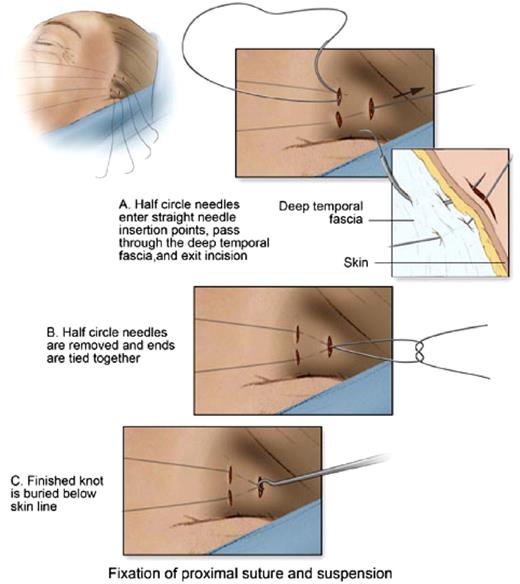
Deployment of Contour Threads is fundamentally different in several ways. First, the needle is passed through soft tissues that are not under tension (Figure 3). Using the long needle, the suture is passed through the tissues to be elevated. The curved needle at the opposite end of the suture is then used to secure the device to fibrous tissue, or alternatively, to tie it to another barbed suture, creating an inverted “U” (with the knot at the base of the U). Once the knot is seated into the fixation port, tension can then be applied on the distal barbed threads. Lax tissues are tightened, and the redundancy is shifted toward the anchoring point in the scalp. Tension is removed from the distal tissues as tissue is ratcheted up the cogs toward the anchored knot. This process is termed contouring.
Illustration of typical fixation technique. A long needle with attached thread is passed through deployment ports into the tissues to be treated. The short curved needle is passed through toward fixation port after taking a bite of deeper fixed tissues. The knot is tied in the proximal fixation port. Thus, a bidirectional device has been created with a fixation point in the middle.
Tissue expansion has historically been practiced by many cultures, but the cellular processes responsible were clarified in the 1980s. While cells stretch initially, they soon increase in number and eventually re-establish their original size and architecture. Although it is recognized that tension and even gravity1–3 operate at the cellular level, compression can slow growth and may lead to apoptosis.4 The cell survives and thrives while it is under some tension, but when tension is removed, some cells die in response. The growth of all noncirculating (bloodborne) cells is mediated by the attachments of their cell membrane receptors, integrins, to extracellular ligands.4–6 Mechanical stimuli (simple tension and compression) are important in many different systems. For example, embryonic muscle cells will grow and become organized into fascicular structures when subjected to physiologically relevant load cycles.7–9 Absence of tension prevents development, just as absence of light prevents development of vision (amblyopia). Not only are mechanical stimuli necessary to the normal development of muscles, they are also important to maintain function. For example, astronauts rapidly lose muscle mass in low-gravity environments. Conversely, transplanted muscles must be sutured under some minimal tension along their fibers; otherwise, they will undergo atrophy and fibrosis.11,12 These findings provide support, although indirectly, for the premise that tissue elevation with barbed sutures causes changes that eventually result in attrition of excess skin.
During this procedure the tissues are lifted toward the upper part of the thread, causing visible tissue gathering that may alarm patients. Patients must understand that gathering will occur and will also dissipate over time, depending on the volume of the displaced tissue. Skin wrinkling is a result of tissue displacement and will occur towards the knot in Contour threads, or towards the midline of bidirectional threads. In traditional surgery, we cut out excess skin but with barbed thread techniques, we do not cut away extra skin, we simply displace it. The displaced skin will tend to shrink away over a period of time similar to how wrinkles and folds disappear in vertical breast reduction techniques. It should be noted that Surgical Specialties Corporation has recently introduced a device with two opposing unidirectional barbed sections and a smooth suture gap section, which has been FDA-approved for the midface and brow.
Patient selection
The ideal patient will have mild to moderate laxity, as evidenced by moderately deep nasolabial folds or jowl formation. The ideal age is (perhaps) 35 to 55, but chronological age is not as relevant as biological age. There may be some skin wrinkling, but this procedure does not improve skin wrinkles to any degree; therefore, patients without significant solar elastosis are superior candidates. Patients who have thin translucent skin and minimal or absent subcutaneous fat are poor candidates, as are patients who are morbidly obese and have tight facial skin.
Patients must be given informed consent that skin will be elevated, causing significant gathering in the soft tissues because skin will not be excised as would occur with traditional methods. Typically, for treatment of the midface, gathering occurs in the lateral cheek and temple regions; for treatment of the neck, gathering occurs in the retro and infra auricular areas.
The surgeon can predict success by checking with gentle finger pressure to see if soft tissue elevation occurs. If the skin cannot be lifted with a finger, it will not be lifted with a barbed suture. Deep-tissue scarring, or any process that prevents tissue mobility when checked with the examiner's finger pressure, will also impede elevation with barbed sutures and must be considered a contraindication.
Procedure
The patient is marked in the upright position and, similar to other aesthetic procedures, plays an active role in determining objectives. While looking into a handheld mirror and applying skin pressure with the fingertip, the patient is asked to demonstrate the aesthetic effect that she or he is seeking. Using the patient's feedback, the surgeon draws vectors on the skin and notes asymmetry or other relevant issues.
The barbed suture procedure is typically performed using a local anesthetic unless it is combined with other aesthetic surgical procedures that require a general anesthetic. Local anesthetic with epinephrine is infiltrated along the proposed suture pathway. Typically, I use 0.5% lidocaine with 1:200,000 epinephrine, a total of about 3 mL per thread. The thread is then inserted and fixed to fascia according to the manufacturer's instructions.
Usually, it is necessary to place 2 threads in each area to lift the area appropriately (2 threads in each jowl, mid cheek, lateral brow area, etc.). Failure of these devices is most commonly not because of thread breakage but because of an incorrectly tied knot (a half hitch instead of a square knot). This is easily prevented by tying the sutures over the tip of a needle holder, which is held in place by an assistant, to ensure that the knot is tied square and tight.
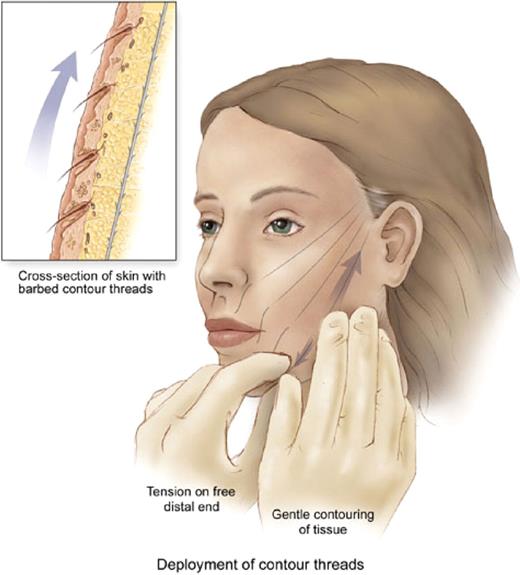
The final step is to contour the face by holding the thread in the nondominant hand and applying pressure on the tissues to engage the barbs on the sutures. This is most easily done with the patient upright so that the effects of gravity are taken into account; however, I sometimes perform this contouring step with the patient recumbent.
If a patient undergoes the procedure under general anesthesia or is too sedated to cooperate, a small dressing (antibiotic ointment and a tape bandage) may be applied to the exit sites of the threads on the skin. The tissues may then be elevated on the following day, with the patient fully awake and cooperative. This will minimize risk of damaging the barbs with excessive tension followed by excessive stress by external pressure. This is an important detail because excessive tension on the barbs followed by correction will result in breaking of the barbs with fewer barbs capable of holding the tissues in place long enough to achieve the biologic goals.
For this reason, I no longer significantly overcorrect when elevating tissues (Figure 4). Further, the endpoint I use for tissue elevation has changed over the last several months. The original procedure involved overcorrection of all sites. Now, I recommend moderate tension only, so that tissues are held in a position that appears natural when the patient is lying down. In fact, if I can maintain the tissues in the same position when the patient is standing as is evident when she or he is lying down, then I have achieved a successful rejuvenation. Results from a typical procedure are shown in Figure 5.
Contouring procedure. Tension is held on the end of the suture exiting the skin. The skin is manipulated to engage the barbs on the sutures. The weight of the tissues is then maintained and distributed among the barbs, each one holding a small amount of weight.
A, C, E, Preoperative views of a 54-year-old patient. B, D, F, Postoperative view 4 months after Contour Thread treatment to the cheek and jowls (4 threads per side, 8 threads in total).
Postoperative management
In fully awake patients who have undergone the procedure with a local anesthetic, no further steps are necessary, assuming patients are compliant. Ideally, there should be no pressure or tension applied to the treated areas for several days until edema resolves and scar collagen builds up around each suture. Although it is impossible to completely avoid pressure on the face, immobilizing the skin with a few strips of skin-colored tape is helpful for several reasons. It splints the tissues somewhat and reminds the patient not to laugh or cause sudden tissue stretching while healing.
My goal in the postoperative period is to minimize risk of patients dislodging the tissues from the barbs. One of the greatest risks of losing support from the sutures occurs during sleep. Direct pressure on the face from a pillow may result in release of tissue support during the early phase of healing before collagen has been deposited around the barbed sutures. The use of skin tape, a travel pillow, or a recliner for sleeping may be helpful for a few days, if only to remind the patient not to lie directly on the areas.
Regardless of these precautions, some patients will lose a degree of lift by inadvertently pressing or pulling down on the face before the biologic processes have been completed. Typically, this will occur on one side or the other, but eventually both sides tend to become symmetrical, almost as if these threads auto-adjust to the correct level. If there is complete loss of support, it may be possible to reposition the barbed segment, especially in the brow; you may be able to stabilize the lower end of the thread with the fingertip while upwardly adjusting the tissues cephalad. However, this is not always possible, and some patients will need to undergo further treatment.
Discussion
My longest follow-up for Contour Threads is from January 2005. In my hands, about 80% of patients have been satisfied with results. However, results vary; in fact, in about 10% to 20% of patients, I could not see any results when comparing preoperative and postoperative photos. So far, I have not been able to predict who will be a good responder. It is possible that some patients may have a genetic predisposition toward this (purported) mechanism of action.
A review of US statistics presented by the American Society for Aesthetic Plastic Surgery14 shows huge gains for minimally invasive procedures. I attribute this trend to patients who are apprehensive of unnatural-looking outcomes from surgical procedures, possibly arising from their impressions of the abnormal appearance of celebrities and others appearing in the popular press. Unfortunately, poor or “operated” results are the only ones that receive public attention, since “natural” results are, by definition, less dramatic. Therefore, although aesthetic surgeons certainly can and do create a natural outcome with traditional techniques, many people are reluctant to have surgery.
I believe that the era of the nondetectable result is upon us. “Nondetectable” does not mean (as critics of barbed suture techniques claim) that the results are so minimal as to be literally undetectable, but rather that the results are subtle, natural, and do not look operated. Patients are willing to accept a less dramatic result, as long as they look natural. In addition, barbed sutures may be an attractive alternative for patients because they are perceived as less invasive and inherently safer. My view is that this procedure does not cannibalize an aesthetic surgery practice but, instead, attracts new patients that may otherwise not surface.
I was trained in conservative methods; the concept of closing wounds under tension was regarded as ill advised and ill conceived. Surgery consisted of delamination (separation of layers) of tissues along natural cleavage planes, followed by repositioning under no tension, followed by careful closure and support until healing occurred. Recent trends in face lifting have questioned this approach, at least some of the time. The 10-year result of the twin facelift study comparing the different techniques of Sam Hamra with those of Dan Baker (presented at the annual meeting of the American Society for Aesthetic Plastic Surgery in New Orleans, 2005) reveals that taking tissues apart completely may be unnecessary, adding layers of complexity, tissue trauma, and prolonged recovery for little or no permanent benefit.
From existing scientific studies, do we have enough evidence to define a mechanism of action for the process occurring with barbed sutures? Probably not completely, but it is interesting to entertain the possibility that we have uncovered the biological opposite of tissue expansion. The work that needs to be done now is to elucidate the parameters that modulate this effect, as well as to define it more thoroughly. Of course, there will be those that doubt the existence of these phenomena, just as there were those who doubted the existence of tissue expansion as a legitimate medical process. I am convinced that there is a real effect here, and that what we have seen is the first attempt at capitalization of that effect.
References
1
2
3
4
5
6
7
8
9
10
11
12
13
14
Author notes
Editor's Note: The author has been paid by Surgical Specialties Corporation to conduct research and training preceptorships.