-
PDF
- Split View
-
Views
-
Cite
Cite
Lars Søndergaard, Antti Saraste, Christina Christersson, Alec Vahanian, The year in cardiology 2017: valvular heart disease, European Heart Journal, Volume 39, Issue 8, 21 February 2018, Pages 650–657, https://doi.org/10.1093/eurheartj/ehx772
Close - Share Icon Share
Preamble
A new joint European Society of Cardiology (ESC) and European Association of Cardiothoracic Surgeons (EACTS) guidelines on management of valvular heart disease (VHD) was published in 2017.1 These guidelines are more focused, and are linked to the upcoming ESC textbook. The main changes concern the role of transcatheter valve treatment, indications for surgery as well as medical therapy. The guidelines present a new concept of Heart Valve Centres with recommended requirements, including multidisciplinary teams with competencies in various interventions and diagnostic techniques for VHD, the availability of important collaborative services, standardized processes and recording of performance data.2 Some of changes in the latest guidelines are highlighted in this article.
Epidemiology of valvular disease
The association between traditional cardiovascular risk factors and incident, severe aortic stenosis (AS) was highlighted in a large unselected elderly population.3 Another study found that in a population-based prospective cohort with 1297 incident cases of AS during 15 years of follow-up both overall obesity reflected by body mass index (BMI) and abdominal adiposity based on waist circumference were positively associated with incidence of AS, with similar associations in men and women.4 Individuals with BMI ≥30 kg/m2 had a significantly [hazard ratio (HR) 1.81, 95% confidence interval (CI) 1.47–2.23] increased risk for incident AS compared with lean individuals. The increasing prevalence of obesity may both determine the increased prevalence of AS and be an important modifiable risk factor for AS.
Using data from national statistics, the prevalence of VHD in ESC member countries is approximately 13.3 million.5 The access to both surgical and transcatheter heart valve treatment is better developed in high-income when compared with middle-income ESC member countries.
The health-related burden of rheumatic heart disease has declined worldwide, but high rates of disease persist in some of the developing countries. In a systematically review of fatal and non-fatal rheumatic heart disease over the last 25 years, it was estimated that global age-standardized mortality due to the disease fell by 47.8% from 1990 to 2015.6 However, there were still more than 30 million cases of rheumatic heart disease and around 300 000 deaths in 2015; the highest mortality was observed in Oceania, South Asia, and central sub-Saharan Africa.
Aortic stenosis
Echocardiography is the first-line imaging technique for the evaluation of patients with VHD, but other imaging modalities can be used to obtain complementary information, and to aid risk stratification in individual patients.7 Aortic valve calcification detected by cardiac computed tomography (CT) is listed in the guidelines among criteria for differentiating severe low-flow, low-gradient AS from moderate disease, particularly in the presence of preserved ejection fraction (EF). The 2017 VHD guidelines also contain a new recommendation that CT coronary angiography should be considered as an alternative to invasive angiography before valve surgery in patients with a low probability of coronary artery disease; it may also be considered when invasive coronary angiography is either technically not feasible or associated with increased risk.
The management of asymptomatic severe AS remains controversial. However, in the 2017 VHD guidelines, markedly elevated plasma natriuretic peptide levels or severe pulmonary hypertension without other explanation have been added as risk factors warranting consideration for surgery in asymptomatic severe AS with normal EF. Currently, aortic valve replacement (AVR) is not indicated in these patients, but it will be evaluated in the randomized EARLY TAVR trial (NCT03042104) and EVoLVeD trial (NCT03094143). An observational study demonstrated that patients with concomitant moderate AS and left ventricle systolic dysfunction are at high risk for clinical events,8 which is the focus of the transcatheter aortic valve replacement (TAVR)-UNLOAD trial (NCT02661451).
Two studies demonstrated the utility of clinical scores for detecting frailty and predicting 1-year mortality after AVR in elderly patients.9 , 10 The burden of mitral annular calcification is also associated with outcomes after AVR; there are now similar data in patients undergoing aortic valve implantation (TAVI).11 Severe mitral annular calcification was encountered in 10% of patients; this was an independent predictor of both overall mortality (HR 2.35, 95% CI 1.19–4.66) and permanent pacemaker implantation [odds ratio (OR) 2.83, 95% CI 1.08–7.47] following TAVI.
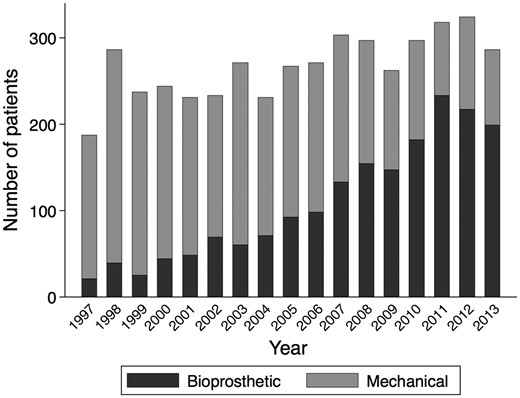
Data from surgical registries describe an increase in the use of biological aortic valves even in the age groups were mechanical valves are usually recommended, Figure 1.12 , 13 There is still a gap in evidence regarding the optimal age cut-off at which a biological valve prosthesis should be preferred. In a propensity-matched study of patients aged 50–69 years treated with biological and mechanical aortic valve prostheses, survival was higher in the group with mechanical prostheses (HR 1.34, 95% CI 1.09–1.66), and the risk of reoperation was lower.13 In a sub-analysis the benefit persisted in those aged 50–59 years, but not for those aged 60–69 years. In a meta-analysis of patients aged 18–55 years treated with mechanical valve prostheses, microsimulation was used to calculate life expectancy and lifetime event-risk.14 Estimated life expectancy was shortened in patients with mechanical prostheses, and the risk of thromboembolism and re-intervention was 18% and 10%, respectively. A recent study stratified patients into different age groups on the basis of valve position [aortic vs. mitral valve (MV)], and found the long-term mortality benefit associated with a mechanical prosthesis, as compared with a biological prosthesis, persisted until 55 years of age among those undergoing aortic-valve replacement, and until 70 years of age among patients undergoing mitral-valve replacement.15
Number of aortic valve replacements per year. Number of patients aged 50–69 years who had undergone aortic valve replacements with mechanical or bioprosthetic valves in Sweden between 1997 and 2013. From Glaser et al. 13
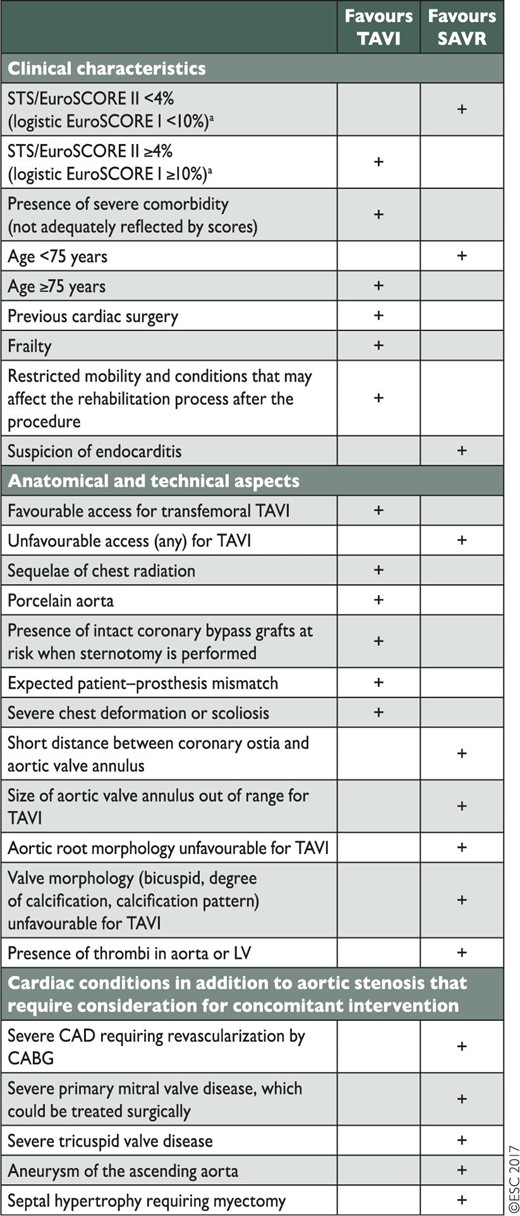
The choice of intervention with TAVI and surgical AVR (SAVR) depends on careful individual evaluation by the Heart Team, taking into consideration the risks and benefits of each approach (Table 1). Although, TAVI is an accepted alternative to surgery in patients with severe AS who are at high surgical risk, the SURTAVI trial provided additional data concerning intermediate risk patients.16 The SURTAVI trial included 1746 patients and showed that TAVI with a self-expanding prosthesis was non-inferior to SAVR with regards to estimated incidence of all-cause mortality and disabling stroke at 24 months (12.6% vs. 14.0%). Surgery was associated with higher rates of acute kidney injury, atrial fibrillation, and transfusion requirements, whereas TAVI had higher rates of residual aortic regurgitation (AR) and need for pacemaker implantation.
Aspects to be considered by the Heart Team for the decision between surgical aortic valve replacement and transcatheter aortic valve implantation in patients at increased surgical risk
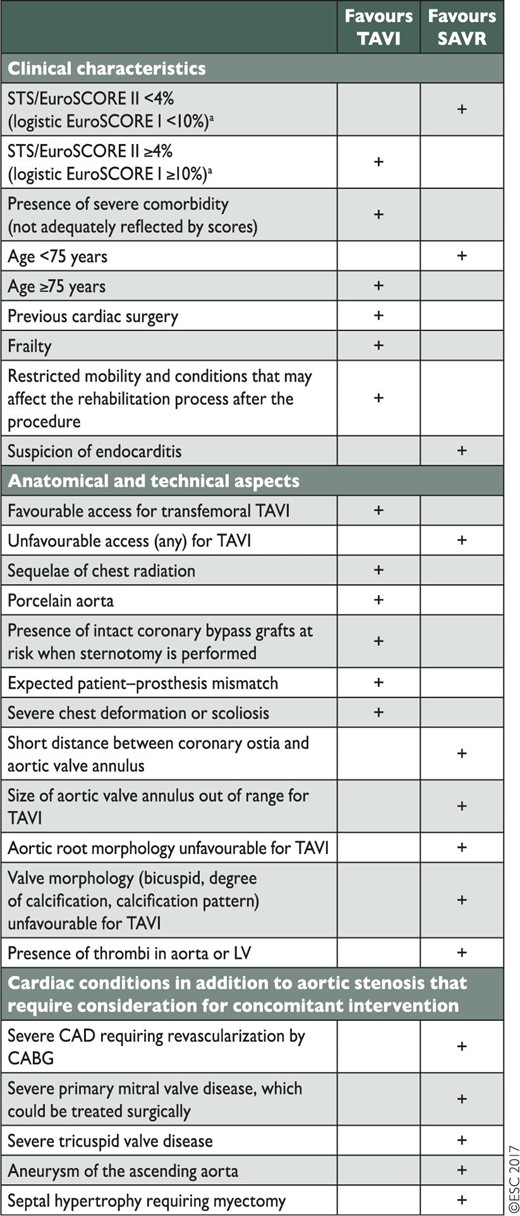 |
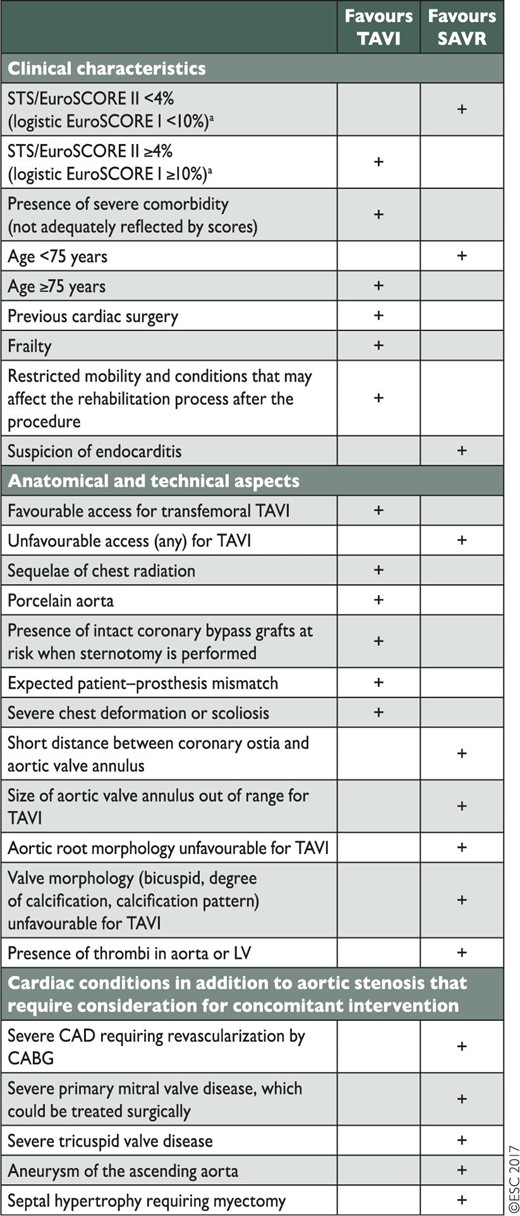 |
Reproduced from Baumgartner et al. 1
CABG, coronary artery bypass grafting; CAD, coronary artery disease; EuroSCORE, European System for Cardiac Operative Risk Evaluation; LV, left ventricle; STS, Society of Thoracic Surgeons.
STS score (calculator: http://riskcalc.sts.org/stswebriskcalc/#/calculate); EuroSCORE II (calculator: http://www.euroscore.org/calc.html); logistic EuroSCORE I (calculator: http://www. euroscore.org/calcge.html). Scores have major limitations for practical use in this setting by insufficiently considering disease severity and not including major risk factors such as frailty, porcelain aorta, chest radiation etc. EuroSCORE I markedly overestimates 30-day mortality and should therefore be replaced by the better performing EuroSCORE II with this regard; it is nevertheless provided here for comparison since it has been used in many TAVI studies/registries and may still be useful to identify the subgroups of patients for decision between intervention modalities and to predict 1-year mortality.
Aspects to be considered by the Heart Team for the decision between surgical aortic valve replacement and transcatheter aortic valve implantation in patients at increased surgical risk
 |
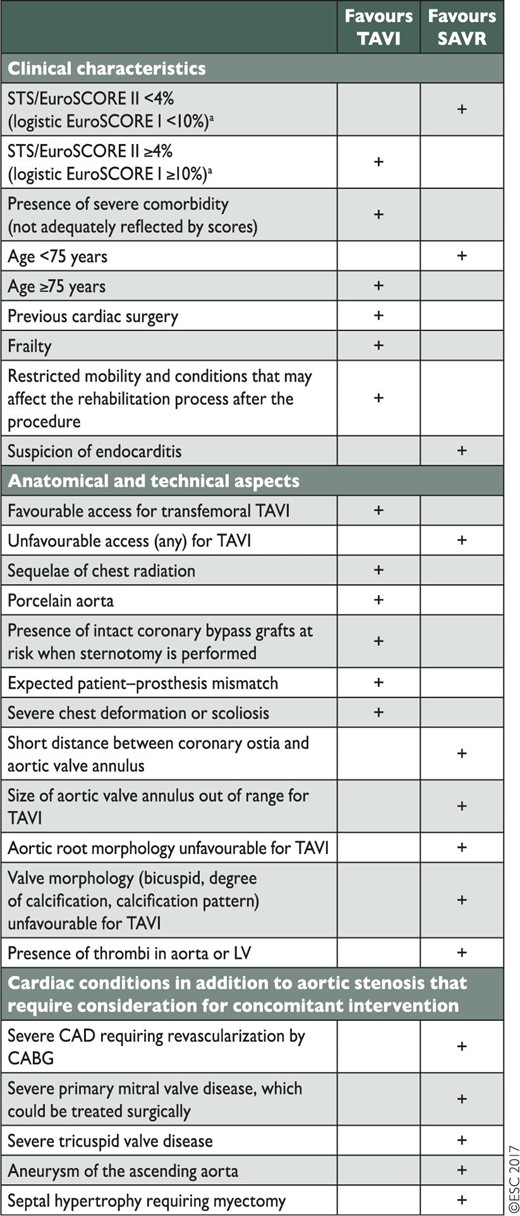 |
Reproduced from Baumgartner et al. 1
CABG, coronary artery bypass grafting; CAD, coronary artery disease; EuroSCORE, European System for Cardiac Operative Risk Evaluation; LV, left ventricle; STS, Society of Thoracic Surgeons.
STS score (calculator: http://riskcalc.sts.org/stswebriskcalc/#/calculate); EuroSCORE II (calculator: http://www.euroscore.org/calc.html); logistic EuroSCORE I (calculator: http://www. euroscore.org/calcge.html). Scores have major limitations for practical use in this setting by insufficiently considering disease severity and not including major risk factors such as frailty, porcelain aorta, chest radiation etc. EuroSCORE I markedly overestimates 30-day mortality and should therefore be replaced by the better performing EuroSCORE II with this regard; it is nevertheless provided here for comparison since it has been used in many TAVI studies/registries and may still be useful to identify the subgroups of patients for decision between intervention modalities and to predict 1-year mortality.
Even though randomized trials support the use of TAVI for the treatment of AS in high- and intermediate-risk patients, the generalizability of these results to clinical practice may be challenged. However, in 9464 propensity-matched intermediate- and high-risk U.S. patients who underwent TAVI or SAVR, there were similar rates of death, stroke, and days alive and out-of-hospital to 1 year, but TAVI patients were more likely to be discharged home.17
With the increased clinical experience and newer generation devices,18–20 TAVI is expected to expand to younger patients, where bicuspid aortic valves are more common. Early experience with TAVI in bicuspid aortic valves revealed difficulties with optimal valve positioning and more paravalvular leak. In a multi-centre registry, 561 patients with bicuspid AS and 4546 patients with tricuspid AS were compared after propensity score matching, assembling 546 pairs of patients with similar baseline characteristics.21 Compared with TAVI for tricuspid AS, treatment in bicuspid AS was associated with a similar prognosis, but a lower device success rate. However, expansion of TAVI to younger patients can only be supported with the availability of long-term data, which are still lacking.
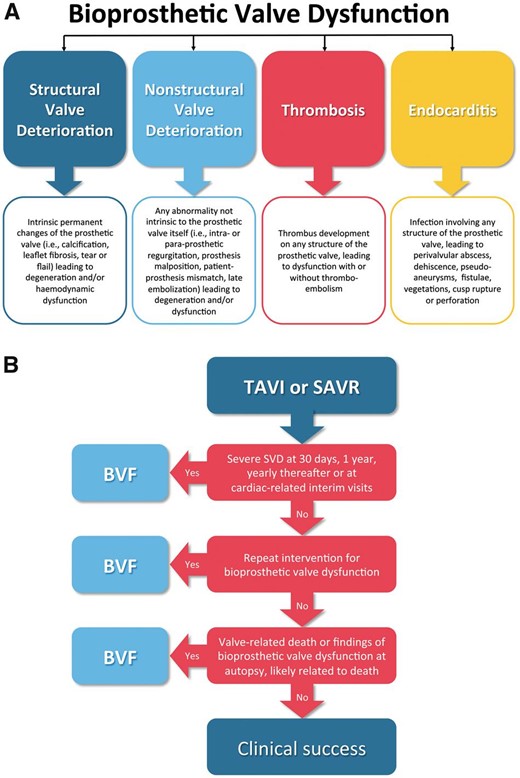
Longevity of bioprosthetic heart valves is an extremely important issue. However, comparisons of valve brands, as well as surgical and transcatheter implantation, have been difficult because different valve durability criteria have been used. The definitions of bioprosthetic valve dysfunction and failure have now been standardized for use in future studies in a consensus publication from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) endorsed by ESC and EACTS,22 Figure 2. Valve-in-valve TAVI should be considered as an option by the Heart Team for treating degenerated surgical bioprostheses depending on the risk of reoperation and the type and size of prosthesis. Thus, TAVI for bioprosthetic aortic valve failure has been associated with a relatively low complication rates and mortality, improved haemodynamics, and excellent functional and quality-of-life outcomes.23 , 24 Furthermore, transcatheter closure may be considered for clinically significant paravalvular leaks in surgical high-risk patients.25
(A) Causes of bioprosthetic valve dysfunction. (B) Suggested assessment of bioprosthetic valve failure (BVF) in outcome studies of transcatheter aortic valve implantation or surgical aortic valve replacement (SAVR). SVD, structural valve deterioration. From Capodanno et al. 22
Aortic regurgitation
The 2017 VHD guidelines recommends that, in selected cases and in experienced centres, aortic valve repair, and valve-sparing aortic surgery, rather than AVR, should be considered by Heart Team for the treatment of severe AR. Consideration of valve sparing surgery, using re-implantation or remodelling with aortic annuloplasty techniques, is especially recommended in young patients with aortic root dilatation and tricuspid aortic valves, when performed by experienced surgeons. The timing of surgery in asymptomatic patients with severe AR and preserved EF remains controversial, although long-term (mean follow-up 6.6 years) survival after surgery is similar to an age- and sex-matched population.26
TAVI for non-calcified native aortic valve regurgitation has been challenging with prosthesis embolization and high rate of paravalvular leakage. However, newer generation TAVI systems has improved the outcome with fewer patients needing a second valve (10%) and having significant residual AR (3%).27
Mitral regurgitation
Echocardiography is essential to assess the aetiology of mitral regurgitation (MR), but quantitative grading remains challenging. The 2017 VHD guidelines state that the thresholds used to define severe secondary MR remain controversial and need to be evaluated with regards to their impact on prognosis after MV intervention. Integration of echocardiography-derived Doppler mitral flow and CT-derived cross-sectional mitral anatomical regurgitant orifice area to calculate mitral regurgitant volume has been evaluated.28 In 73 patients undergoing TAVI, who also had either primary or secondary MR, this approach resulted in reclassification of MR from severe to non-severe in 10% and from non-severe to severe in 14% of the patients providing a proof-of-concept of this integrated approach.
A study validated a risk score (The Mitral Regurgitation International Database (MIDA) mortality risk score) integrating various clinical and echocardiographic parameters endorsed by guidelines for predicting short- and long-term mortality risk in patients with severe degenerative MR either under medical or surgical treatment.29 In patients with severe MR and preserved left ventricular EF, worsening of global longitudinal strain using speckle-tracking resting echocardiography is independently associated with mortality during 8.3 years of follow-up, providing additive prognostic utility to reduced capacity on exercise testing and other previously known predictors.30 Importantly, in the recent guideline, MV surgery in patients with moderate secondary MR undergoing coronary artery bypass surgery is no longer recommended in the guidelines.
Mitral valve repair is recommended over MV replacement in degenerative MR and this recommendation is backed-up by multicentre registry data analysed with propensity score matching.31 The operative mortality was lower in the MV repair group (0.2% vs. 4.4%, P < 0.001) and 20-year survival was better (41% vs. 24%, P < 0.001). In secondary MR, sub-valvular intervention may be added to annuloplasty with a ring. In a recent review of 397 patients, there was less recurrence of MR (relative risk (RR) 0.43, 95% CI 0.27–0.66; P = 0.0002), and more positive remodelling of the left ventricle in the group with the combined intervention as compared to those treated with just annuloplasty.32
Transcatheter MV repair has been dominated by the MitraClip system. However, the first-in-man study on the Edwards PASCAL system in compassionate cases with symptomatic, severe functional, degenerative, or mixed MR has been reported.33 The Edwards PASCAL system implements a central spacer, and allows for independent leaflet grasping resulting in procedural residual MR of Grade 2+ or less in 22 of 23 patients. Although the study established feasibility of the Edwards PASCAL system, further research is needed on procedural and long-term clinical outcomes.
While transcatheter MV repair has been shown to reduce heart failure symptoms, the prognostic impact of these therapies is lacking. However, large randomised trials are ongoing, e.g. COAPT (NCT01626079), French MITRA-FR (NCT01920698), RESHAPE-HF2 (NCT02444338), and MATTERHORN (NCT02371512).
The outcome of transcatheter MV implantation in failed degenerated surgical MV prostheses (176 patients; ‘valve-in-valve’) and failed annuloplasty rings (72 patients; ‘valve-in-ring’) has been evaluated in a multicentre registry.34 Overall technical and device success rates were acceptable, at 92.3% and 85.5%, respectively. However, compared with the valve-in-valve treatment, the valve-in-ring treatment had lower technical and device success, and was associated with more MR, life-threatening bleeding, acute kidney injury, and higher mortality.
Transcatheter MV implantation in native non-calcified MR has attracted much attention during the last 5 years. The technique has been associated with high mortality, risk of left ventricular outflow tract obstruction and prosthesis dislocation. However, a recent report on 30 selected patients with primarily functional MR and high surgical risk, transapical implantation of the tendyne valve was successful in 28 patients with no acute deaths. At 30 days only one patient had mild MR whereas the remaining patients had no residual MR, and 75% of the patients reported mild or no symptoms.35
Tricuspid regurgitation
A meta-analysis including 15 studies and 2840 patients has demonstrated the benefit of TV repair during surgery for left heart valve disease, with reduced cardiac mortality (OR 0.38, 95% CI 0.25–0.58).36 Tricuspid valve (TV) replacement is uncommon and data comparing biological and mechanical prosthesis is scarce. In a single centre study of 120 interventions with TV replacement described a high mortality rate both early (21.7%) and during mean 7 years follow-up (37.5%); no difference was found comparing mechanical and biological TV replacement.37
Percutaneous transcatheter TV therapy is an evolving treatment option for patients with significant tricuspid regurgitation (TR), who are not candidates for open heart surgery.38 A recent study proposed a systematic approach to define those patients suitable for transcatheter TV devices based on evaluation of the TV annulus geometry, right ventricle, vena cava dimensions, and spatial relationships between the TV and the right coronary artery using CT.39
Transcatheter repair of chronic severe TR with the MitraClip system has been studied in 64 consecutive patients deemed unsuitable for surgery.40 The MitraClip device was successfully implanted in the TV in 97% of the cases, and TR was reduced by at least one grade in 91% of the patients with no intra-procedural deaths. Functional class and 6-min walking distance improved significantly.
Anti-thrombotic therapy
The 2017 VHD guidelines states that Vitamin K antagonists (VKA) are the only recommended anticoagulant therapy in patients with mechanical valve prostheses. Novel oral anti-coagulants (NOAC) are contraindicated based on the results seen with the direct thrombin inhibitor dabigatran.41 Factor Xa inhibition acts upstream in the coagulation cascade and may therefore have an advantage by influencing both the extrinsic and contact activation coagulation pathways with minimal antagonism of existing thrombin needed to maintain haemostasis. In a porcine model with aortic heterotopic valves, short-term, intravenous apixaban treatment was associated with a reduced weight of valve thrombus as compared to warfarin and no bleeding events occurred in the apixaban group.42 This concept is of interest given the clinical relevance of bleeding complications because of VKA.
The optimal antithrombotic regime and duration of treatment in biological prosthetic valves is not fully explored and further randomized trials are needed. Dual antiplatelet therapy is recommended for most patients after TAVI. However, a meta-analysis of four studies including 640 patients found no benefit of dual over single antiplatelet therapy regarding the risk of stroke or mortality, but an increased frequency of major and lethal bleeding events during the first 30 days after intervention.43
Increasing attention is being been paid to subclinical leaflet thrombosis after biological SAVR and TAVI, as well as its association with antithrombotic regimes. Leaflet thickening and reduced leaflet motion on CT have been referred to as hypo-attenuating leaflet thickening (HALT) and the more severe hypo-attenuation affecting motion (HAM), respectively. Observations suggest that HALT and HAM are two stages of the same phenomenon, with leaflet thickening affecting leaflet motion at a more advanced stage. Uncontrolled data indicate that HAM may be more common after TAVI (13%) than after SAVR (4%).44 Among several suggested risk factors, regional stent frame underexpansion has been associated with an increased risk of leaflet thickening, and post-dilatation of self-expanding transcatheter heart valves as well as a supra-annular valve position seemed to reduce the occurrence of this phenomenon.45
As the finding of an increase gradient is uncommon with HAM, it is conceivable that the true incidence of HAM is underestimated with the echocardiography assessment.44 , 46 Registry data suggest that the phenomenon may be associated with a higher prevalence of TIA, but not stroke.44 However, these findings must be interpreted with caution due to a temporal separation between the CT and the clinical event, and prospective clinical studies are warranted. Both VKA and NOAC seem to protect against leaflet thrombosis, though neither single or dual anti-platelet therapy have the same effect.44 When present, the subclinical leaflet thrombosis may be resolved by VKA or NOAC; however, the temporal dynamics of these phenomena are poorly understood.47 It is possible that subclinical leaflet thrombosis may develop or regress early or late after valve replacement despite no change in anti-thrombotic regime. These preliminary findings complicate recommendations regarding optimal anti-thrombotic therapy after TAVR or SAVR. Patients only seem to be protected against leaflet thrombosis whilst on anti-coagulation therapy, and life-long treatment is associated with an increased bleeding risk. The ongoing trials on anti-thrombotic therapy after TAVI, such as ARTE (NCT01559298), ATLANTIS (NCT02664649), AUREA (NCT01642134) AVATAR (NCT02735902), GALILEO (NCT02556203), and POPULAR-TAVI (NCT02247128), will hopefully add information regarding the optimal treatment.
Valvular disease and pregnancy
Obstructive valvular disease is associated with increased maternal and foetal risk during pregnancy especially in women with severe mitral stenosis. Results from The Registry on Pregnancy and Cardiac Disease (ROPAC), which is part of the European Observational Registry Program, also underline the importance of identifying and evaluating women with AS before pregnancy. In pregnant women with severe AS, defined as a peak gradient ≥64 mmHg, 35.3% were hospitalized because of cardiac reasons compared with 12.9% of the women with moderate AS (P = 0.02); the risk of heart failure during pregnancy was significantly higher in symptomatic AS patients.48
When valve replacement is indicated in women with child-bearing potential, a biological rather than mechanical prosthesis is recommended; women with mechanical prostheses treated with VKA have a higher risk of valve thrombosis and bleeding during pregnancy combined with an increased risk for the foetus. Recently, a meta-analysis of 18 studies with 800 pregnancies evaluated four different antithrombotic regimes [VKA, low molecular weight heparin (LMWH), LMWH + VKA, and unfractionated heparin + VKA] in mechanical valves during pregnancy.49 The study confirms previous findings that VKA is preferred from a maternal perspective. Dose-adjusted LMWH throughout the pregnancy was associated with a lower foetal risk when compared to other regimes, but the foetal risk was similar to risk in the group taken a dose of VKA ≤5 mg/day (HR 0.9, 95% CI 0.3–2.4). These results support previous findings that the teratogen effect by VKA seems to be dose-dependent. In a similar meta-analysis of 46 studies, VKA was associated with fewest maternal complications but also with fewest live births. Sequential treatment with heparin during first-trimester followed by VKA did not eliminate anticoagulant-related foetal/neonatal adverse events. Low molecular weight heparin is associated with the highest number of live births. The safety of unfractionated heparin throughout pregnancy and first-trimester VKA ≤5 mg/day remains unconfirmed.50
Endocarditis
Transoesophageal echocardiography (TOE) remains the recommended imaging modality for the diagnosis of infectious endocarditis (IE), whereas CT can be used as an alternative or for detection of abscesses/pseudo-aneurysm. In a small imaging study (n = 49) of patients with both native and prosthetic valve IE, preoperative TOE and CT findings were compared to those at surgery.51 There was no difference in the diagnostic sensitivity of the two methods, but TOE identified numerically more vegetations, leaflet perforation, and paravalvular leakage.
Radionuclide imaging of inflammation with 18 F-fluorodeoxyglucose or radioactively-labelled white blood cells can help in the detection of prosthetic valve endocarditis. Developments with novel cadmium-zinc telluride detector single-photon emission computed tomography (SPECT) cameras provide higher count sensitivity and spatial resolution compared with standard gamma cameras; these promise enhanced 111In imaging of endocarditis. A study evaluated the feasibility and diagnostic accuracy of simultaneous imaging of inflammation with 111In-labelled white blood cells and myocardial perfusion with 99mTc, for localization of white blood cells relative to the valve plane in suspected endocarditis.52 The results support the usefulness of a novel approach to increase sensitivity and accuracy of white blood cell imaging in endocarditis.
Work has also considered the risks of endocarditis in patients with prosthetic valves. In a population-based cohort study of 138 867 patients with a prosthetic valve (median follow-up 1.7 years) the incidence rate of oral streptococcal IE was 93.7/100 000 patient-years.53 No increased rate of IE was found within three months of exposure to invasive dental procedure, but in a case crossover analysis a dental procedure was more frequent in IE periods (5.1% vs. 3.2%, OR 1.66; 95% CI 1.05–2.63; P = 0.03). In the CONCOR registry, including patients with congenital heart disease, the incidence of IE was 1.33 cases/1000 patient-years.54 Prosthetic valves were associated with an increased risk of IE (HR 5.48, 95% CI 3.58–8.38) compared with no prosthetic valve. This increased risk was found both early and during long-term follow-up after surgery. In a registry-based observational study of both biological and mechanical aortic prostheses (mean follow-up 6.2 years), the incidence of prosthetic valve IE was 0.57%/person-year; the risk was highest during the first year after surgery.55 The risk of prosthetic valve IE was higher in the group with biological prostheses (HR 1.54, 95% CI 1.29–1.83) as compared with those with mechanical prostheses. These studies have confirmed the risk of IE in patients with prosthetic valves and support the continued recommendation of antibiotic prophylaxis in all such patients.
Perspectives
With the rapid adaptation of TAVI in patients with AS and increased surgical risk, the role of TAVI in patients at low surgical risk is currently being explored. Since patients in these trials have longer life-expectancy, these trials may also add important information on longevity of bioprosthetic aortic valves.
As several transcatheter repair and replacement techniques are emerging, evidence for the benefit of intervention in particular functional MR is still missing. The COAPT and French MITRA-FR trials investigate MitraClip in this setting and study results are foreseen during 2018. Furthermore, the impact of transcatheter MV replacement and tricuspidal valve repair is also under investigation.
Conflict of interest: Lars Søndergaard has received consultancy fee and institutional research grant from Abbott, Boston Scientific, Edwards Lifescience, Medtronic, and Symetis.
References
Author notes
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.