-
PDF
- Split View
-
Views
-
Cite
Cite
Sean W. Mulvaney, James H. Lynch, Jason de Leeuw, Matthew Schroeder, Shawn Kane, Neurocognitive Performance is Not Degraded After Stellate Ganglion Block Treatment for Post-Traumatic Stress Disorder: A Case Series, Military Medicine, Volume 180, Issue 5, May 2015, Pages e601–e604, https://doi.org/10.7205/MILMED-D-14-00504
Close - Share Icon Share
ABSTRACT
Objective: To measure key neurocognitive performance effects following stellate ganglion block (SGB) administered to treat post-traumatic stress disorder (PTSD) symptoms. Methods: Eleven patients diagnosed, screened, and scheduled for SGB to treat their PTSD symptoms were administered a panel of eight cognitive measures before and 1 to 3 weeks after undergoing this procedure. PTSD symptoms were evaluated using the Posttraumatic Stress Disorder Checklist—Military. Results: One to three weeks post-SGB, none of the patients showed any statistically significant decline in neurocognitive performance. Rather, there was a clear trend in improvement, with four out of eight measures reaching statistical significance following SGB. All patients improved in PTSD symptoms with a mean improvement on Posttraumatic Stress Disorder Checklist—Military of 29. Conclusion: In this case series of 11 patients, SGB effectively treated PTSD symptoms and did not impair reaction time, memory, or concentration. Therefore, SGB should be considered as a viable treatment option for personnel with PTSD symptoms who will be placed in demanding conditions such as combat.
INTRODUCTION
Stellate ganglion block (SGB), a procedure employed for more than 70 years, has increasingly gained acceptance as a novel treatment for post-traumatic stress disorder (PTSD) symptoms.1,–5 The beneficial effects of this technique are described elsewhere and are outside the scope of this article. Hypothesized mechanism of action may include blockade of the cervical sympathetic chain effectively resetting an individual's “fight or flight” response, correcting dysfunctional increased sympathetic tone (e.g., combat). The beneficial effects of this technique are described elsewhere and are outside the scope of this article. SGB at the level of C-6 (right side) has improved PTSD symptoms in multiple case series in military combat personnel, including a large case series by Mulvaney et al5 in which 166 patients were followed for 3 months. Although this emerging treatment has been quite effective in treating PTSD symptoms, several questions remain regarding potential effects upon cognitive performance. As many service members being treated with SGB are still actively training and deploying back to combat zones, it is critical to ascertain the effects of SGB on such important domains as reaction time, memory, and concentration, which could potentially impact combat effectiveness and survivability on the battlefield. Of additional concern was whether patients' reaction times might suffer immediately following SGB administration.
Although PTSD symptoms such as hypervigilance and irritability improve following SGB, this procedure would not be as viable for those returning to the battlefield if it slowed reaction time or decreased concentration.1 For the highly trained military service members who continue to serve in frontline combat units, maintaining their tactical edge is of utmost importance. Any negative effect on these service members' “fight or flight” responses might adversely impact combat performance. The authors of this article have had close follow-up with several hundred military patients treated with SGB who returned to combat operations overseas without difficulty. This population's subjective self-report has been positive without any remarks of negative effects upon duty performance. In fact, many service members described improvements in their overall functioning. To investigate these anecdotal reports, this case study sought to empirically answer these questions through baseline and postprocedure administration of an automated battery of psychometric tests.
METHODS
PTSD patients whose scores on the PTSD Checklist—Military (PCL-M) exceeded the National Center for PTSD's recommended cutoff of 50 were eligible for inclusion in the case series.6 The 11 patients included in the study volunteered for cognitive testing that was performed after it had been determined they would receive SGB to improve PTSD symptoms. The automated battery of psychometric measures consisted of the eight tests available from Joggle Research (https://admin.joggleresearch.com/www.joggleresearch.com). The battery was administered on an electronic tablet testing platform (Apple iPad). The testing protocol was administered in a quiet room free of any extraneous distractions. The Joggle battery yields a score for each of the eight measures. Baseline measures were obtained within 48 hours before receiving an ultrasound-guided right-sided SGB at the C-6 level per previously published descriptions of this technique.7,–11 In each patient, post-SGB, successful sympathetic blockade was confirmed by the presence of Horner's syndrome within 5 minutes of completion of the procedure. Six patients repeated one of the tests, a psychomotor vigilance test (PVT) 1 hour after SGB to see if SGB reduced reaction time or vigilance in the immediate post-SGB period. All patients repeated the PCL-M and the same battery of eight neurocognitive tests under the same conditions at follow-up within 3 weeks.
This project was approved by the Womack Army Medical Center (Fort Bragg, North Carolina) Institutional Review Board.
Psychometric Testing
PTSD symptomatology: PTSD symptoms were measured using the PCL-M. The PCL-M is a 17-item self-report one-page questionnaire endorsed by the National Center for PTSD, which has been shown to have strong internal consistency, test–retest reliability, and convergent validity with other PTSD measures.12 The PCL has been validated for screening for PTSD, diagnosing PTSD, and for determining response to treatment interventions.12,–14 Patients scoring greater than 50 on the PCL-M were made aware of this study and asked whether they would be interested in participating. All potential participants were informed that inclusion in this study would not affect access to care or the quality of treatment they would receive.
Cognitive Function
Cognitive testing was conducted using automated psychometric measures commercially available through Joggle Research. Joggle applications have been used in academic research, several branches of the U.S. military, Fortune 500 companies, and the U.S. Department of Transportation. This neurobehavioral measurement tool was chosen for its simplicity and ease of implementation for busy tactical organizations with many other competing demands for service members' time. In an effort to maximize the likelihood we would detect any potential cognitive deficit created by the procedure, all eight tests available from Joggle Research were administered. The selected battery of tests included Motor Praxis (MPT), Visual Object Learning (VOLT), Fractal 2-Back (NBACK), Abstract Matching (AM), Line Orientation (LOT), Digit Symbol Substitution (DSST), Balloon Analog Risk (BART), and PVT. These tests measure a variety of cognitive functions to include sensorimotor speed (MPT), visual learning and spatial working memory (VOLT), working memory (NBACK), abstraction (AM), spatial orientation (LOT), complex scanning and visual tracking (DSST), risk decision making (BART), and vigilant attention (PVT). Total testing time was 18 minutes, so patient fatigue was not a significant issue. Baseline readings were administered within 48 hours before the procedure. Follow-up testing was administered 2 to 25 days following the SGB.
CASE SERIES
The patients for this case series were active duty military personnel with more than three combat deployments, (average age 36.6 years, 10 male/1 female). In addition to their PCL-M score being greater than 50, a senior military physician with extensive experience treating PTSD diagnosed all patients with PTSD. Patients were not receiving treatment, pharmacologic or otherwise, for at least 6 months before inclusion in this case series. Standard PTSD therapies were made available to all patients, including on-site psychology treatment and pharmacologic treatment. No patients sought additional treatment, pharmacologic or otherwise, between baseline and post-SGB procedure test administration.
RESULTS
Change in mean results of neurocognitive tests from baseline to follow-up was assessed using paired t-tests. Pearson correlation coefficients were used to determine if a relationship existed between time to follow-up and change in test results. Significance for all statistical tests was established a priori at alpha 0.05.
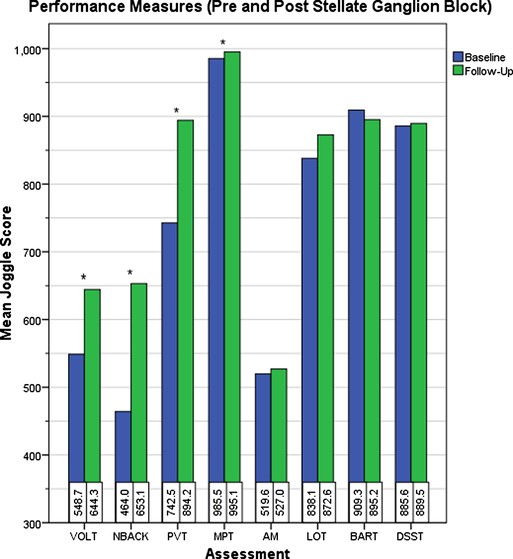
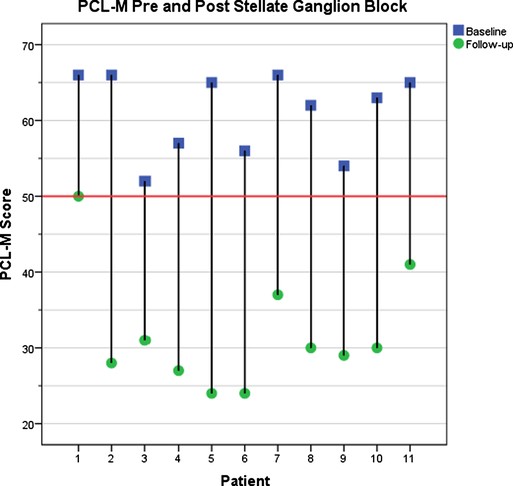
Mean baseline PCL-M score was 61.0 (range: 52–66) and mean age of patients was 36.6 (range: 26–49). Significant improvement in mean response was observed for VOLT (mean change: 95.6; [95% CI, 35.15–155.94]; p = 0.005), NBACK (mean change: 189.1; [95% CI, 84.52–293.66]; p = 0.002), PVT (mean change: 151.6; [95% CI, 25.48–277.79]; p = 0.023), and MPT (mean change: 9.64; [95% CI, 3.09–16.18]; p = 0.008) (Figure 1, Table I). Although nonsignificant, AM, LOT, and DSST demonstrated positive mean changes, whereas BART was the only test that declined from baseline to follow-up (Table I). A significant decrease in PCL-M score from baseline to follow-up was also observed (mean change: −29.18; [95% CI, −34.09 to −24.27]; p < 0.001) (Fig. 2). This result is in agreement with previous work.5 Time to follow-up was not correlated to any mean change in test results.
Change in neurocognitive test scores from baseline to follow-up among 11 patients. *Indicates a significant change (p ≤ 0.05).
Mean Change From Baseline to Follow-Up
| . | N . | Mean Baseline . | Mean Follow-Up . | Mean Δ . | 95% CI . | Significance . |
|---|---|---|---|---|---|---|
| PCL | 11 | 61.09 | 31.91 | −29.18 | −34.09, −24.27 | 0.000 |
| MPT | 11 | 985.45 | 995.09 | 9.64 | 3.09, 16.18 | 0.008 |
| VOLT | 11 | 548.73 | 644.27 | 95.55 | 35.15, 155.94 | 0.005 |
| NBACK | 11 | 464.00 | 653.09 | 189.09 | 84.52, 293.66 | 0.002 |
| AM | 11 | 519.64 | 527.00 | 7.36 | −69.09, 83.82 | 0.834 |
| LOT | 11 | 838.09 | 827.64 | 34.55 | −1.39, 70.48 | 0.058 |
| DSST | 11 | 885.64 | 889.55 | 3.91 | −55.29, 63.11 | 0.886 |
| BART | 11 | 909.27 | 895.18 | −14.09 | −115.35, 87.17 | 0.763 |
| PVT | 11 | 742.55 | 894.18 | 151.64 | 25.48, 277.79 | 0.023 |
| . | N . | Mean Baseline . | Mean Follow-Up . | Mean Δ . | 95% CI . | Significance . |
|---|---|---|---|---|---|---|
| PCL | 11 | 61.09 | 31.91 | −29.18 | −34.09, −24.27 | 0.000 |
| MPT | 11 | 985.45 | 995.09 | 9.64 | 3.09, 16.18 | 0.008 |
| VOLT | 11 | 548.73 | 644.27 | 95.55 | 35.15, 155.94 | 0.005 |
| NBACK | 11 | 464.00 | 653.09 | 189.09 | 84.52, 293.66 | 0.002 |
| AM | 11 | 519.64 | 527.00 | 7.36 | −69.09, 83.82 | 0.834 |
| LOT | 11 | 838.09 | 827.64 | 34.55 | −1.39, 70.48 | 0.058 |
| DSST | 11 | 885.64 | 889.55 | 3.91 | −55.29, 63.11 | 0.886 |
| BART | 11 | 909.27 | 895.18 | −14.09 | −115.35, 87.17 | 0.763 |
| PVT | 11 | 742.55 | 894.18 | 151.64 | 25.48, 277.79 | 0.023 |
Mean Change From Baseline to Follow-Up
| . | N . | Mean Baseline . | Mean Follow-Up . | Mean Δ . | 95% CI . | Significance . |
|---|---|---|---|---|---|---|
| PCL | 11 | 61.09 | 31.91 | −29.18 | −34.09, −24.27 | 0.000 |
| MPT | 11 | 985.45 | 995.09 | 9.64 | 3.09, 16.18 | 0.008 |
| VOLT | 11 | 548.73 | 644.27 | 95.55 | 35.15, 155.94 | 0.005 |
| NBACK | 11 | 464.00 | 653.09 | 189.09 | 84.52, 293.66 | 0.002 |
| AM | 11 | 519.64 | 527.00 | 7.36 | −69.09, 83.82 | 0.834 |
| LOT | 11 | 838.09 | 827.64 | 34.55 | −1.39, 70.48 | 0.058 |
| DSST | 11 | 885.64 | 889.55 | 3.91 | −55.29, 63.11 | 0.886 |
| BART | 11 | 909.27 | 895.18 | −14.09 | −115.35, 87.17 | 0.763 |
| PVT | 11 | 742.55 | 894.18 | 151.64 | 25.48, 277.79 | 0.023 |
| . | N . | Mean Baseline . | Mean Follow-Up . | Mean Δ . | 95% CI . | Significance . |
|---|---|---|---|---|---|---|
| PCL | 11 | 61.09 | 31.91 | −29.18 | −34.09, −24.27 | 0.000 |
| MPT | 11 | 985.45 | 995.09 | 9.64 | 3.09, 16.18 | 0.008 |
| VOLT | 11 | 548.73 | 644.27 | 95.55 | 35.15, 155.94 | 0.005 |
| NBACK | 11 | 464.00 | 653.09 | 189.09 | 84.52, 293.66 | 0.002 |
| AM | 11 | 519.64 | 527.00 | 7.36 | −69.09, 83.82 | 0.834 |
| LOT | 11 | 838.09 | 827.64 | 34.55 | −1.39, 70.48 | 0.058 |
| DSST | 11 | 885.64 | 889.55 | 3.91 | −55.29, 63.11 | 0.886 |
| BART | 11 | 909.27 | 895.18 | −14.09 | −115.35, 87.17 | 0.763 |
| PVT | 11 | 742.55 | 894.18 | 151.64 | 25.48, 277.79 | 0.023 |
Change in PCL-M score from baseline to follow-up among 11 patients. Average decrease in PCL-M score, 29.2.
A 1-hour post-SGB PVT was administered to 6 of the 11 patients to assess the short-term effect of SGB on reaction time and vigilance. Surprisingly, a significant increase in PVT score was observed (mean change: 127.33; [95% CI, 69.10–185.57]; p = 0.002), indicating a decrease in reaction time.
DISCUSSION
With growing interest in this procedure among experienced combat veterans, we sought to determine what effects SGB has on critical performance skills such as reaction times, memory, and concentration. The conclusions we can draw from a small case series are limited. However, in this comprehensive evaluation of neurocognitive performance, all patients had both clinically and statistically significant reduction in their PTSD symptom scores as had been demonstrated in past publications (average PCL-M score improvement of 27 points).2 In each of the eight areas evaluated by the Joggle battery, there were no patients who showed any statistically significant decline in neurocognitive performance. Rather, there was a clear trend in improvement. In four of the tests (MPT, VOLT, NBACK, and PVT), scores significantly improved in the 7 to 20 days between baseline and postprocedure test administration. Such improvements indicate that following SGB sensorimotor speed, visual learning and spatial working memory, working memory, and vigilant attention improved. It is unclear whether the improvements are because of reduced PTSD symptoms or because of some primary effect of the SGB. Repetitive administration of tests may effectively constitute practice, which could contribute to improved performance over time. In this particular instance, the amount of time between repeat administrations, the nature of test items (e.g., complex visual patterns), and the small number of test administrations suggest practice effects are unlikely to explain the improvements we observed. Regardless, there is no evidence within our study to suggest that the SGB procedure harmed patients' reaction time, memory, or concentration at 1 to 2 weeks post-SGB.
Further research is necessary to evaluate these effects for longer periods of time as well as how best to translate these results into combat effectiveness. We can draw from the large body of sports research to make some assumptions for “tactical athletes.”15,16 For example, a soldier's shooting skills such as target discrimination require a similar expertise in spatial orientation and sensorimotor speed as does a baseball player's batting skills or a hockey goalie's defensive skills. Numerous studies in the literature demonstrate superior neurocognitive performance in elite vs. novice athletes.17,–21 Neurocognitive testing on policemen has demonstrated correlation with accuracy on shooting skills.22 In addition, military-relevant perceptual-cognitive skills have been identified.23 Therefore, it is not difficult to deduce that superior performance on a battery of neurocognitive tests may translate to enhanced combat effectiveness or combat survivability, although this would be difficult to quantify.
In addition, patients who were administered the PVT test 1-hour following their SGB demonstrated improved reaction times, suggesting that SGB is unlikely to have any negative impact upon reaction times, either immediately after SGB or at the 1- to 3-week mark. This fact supports post-SGB patients being able to return to their usual level of function within 24 hours post-procedure.
CONCLUSION
Although further research may be beneficial, our case series found SGB did not impair reaction time, memory, or concentration among our 11 patients. Providers can offer SGB as a viable treatment option to personnel with PTSD symptoms without reservation that the procedure might inadvertently increase the risk of a negative outcome in a deploying population. SGB did not appear to impair reaction times/vigilance 1-hour post-SGB. Consistent with previously published studies, SGB continues to demonstrate its potential usefulness to effectively treat PTSD symptoms.