-
PDF
- Split View
-
Views
-
Cite
Cite
Shari P Feirman, Allison M Glasser, Shyanika Rose, Ray Niaura, David B Abrams, Lyubov Teplitskaya, Andrea C Villanti, Computational Models Used to Assess US Tobacco Control Policies, Nicotine & Tobacco Research, Volume 19, Issue 11, November 2017, Pages 1257–1267, https://doi.org/10.1093/ntr/ntx017
Close - Share Icon Share
Abstract
Simulation models can be used to evaluate existing and potential tobacco control interventions, including policies. The purpose of this systematic review was to synthesize evidence from computational models used to project population-level effects of tobacco control interventions. We provide recommendations to strengthen simulation models that evaluate tobacco control interventions.
Studies were eligible for review if they employed a computational model to predict the expected effects of a non-clinical US-based tobacco control intervention. We searched five electronic databases on July 1, 2013 with no date restrictions and synthesized studies qualitatively.
Six primary non-clinical intervention types were examined across the 40 studies: taxation, youth prevention, smoke-free policies, mass media campaigns, marketing/advertising restrictions, and product regulation. Simulation models demonstrated the independent and combined effects of these interventions on decreasing projected future smoking prevalence. Taxation effects were the most robust, as studies examining other interventions exhibited substantial heterogeneity with regard to the outcomes and specific policies examined across models.
Models should project the impact of interventions on overall tobacco use, including nicotine delivery product use, to estimate preventable health and cost-saving outcomes. Model validation, transparency, more sophisticated models, and modeling policy interactions are also needed to inform policymakers to make decisions that will minimize harm and maximize health.
In this systematic review, evidence from multiple studies demonstrated the independent effect of taxation on decreasing future smoking prevalence, and models for other tobacco control interventions showed that these strategies are expected to decrease smoking, benefit population health, and are reasonable to implement from a cost perspective. Our recommendations aim to help policymakers and researchers minimize harm and maximize overall population-level health benefits by considering the real-world context in which tobacco control interventions are implemented.
Introduction
In 2014, approximately 17% of adults in the United States were current cigarette smokers,1 down from 21% in 20052 and 25% in 1997.3 This success can be attributed, at least in part, to population-based tobacco control interventions.4–6 Widespread tobacco control strategies include raising tobacco product price, implementing youth prevention interventions, banning smoking in public spaces, restricting marketing and advertising, educating the public through mass media and school-based interventions,7,8 and supporting access to evidence-based cessation interventions.9,10 The tobacco marketplace has become increasingly diverse and, in recent years, other strategies have been implemented, such as banning the sale of certain flavored tobacco products11 and requiring smokeless tobacco warning labels.12
To extend or generalize empirical data on the effects of these policies,13–18 simulation models can project the potential future impacts of novel policy options and serve as a decision tool for policymakers.19 Computational simulation models can account for the impact of complex, potentially non-linear factors that contribute to an outcome of interest.20 These tools have been used to understand complex public health problems, including obesity21 and infectious diseases.22 The Center for Tobacco Products at the Food and Drug Administration (FDA), which has the authority to regulate cigarettes and other tobacco products, has expressed interest in using simulation models to inform regulatory decision-making,23,24 as has the National Institutes of Health in its strategic plan for behavioral sciences.25 Such tools may also be valuable to state and local decision-makers.
The current analysis builds upon a systematic review that identified studies using computational models to project tobacco-related outcomes.26 For the present study, we identified a subset of US-based studies that used computational models to evaluate the effects of population-based tobacco control interventions, including policy and non-policy efforts. Due to the quantity of papers, the current analysis focuses on non-clinical tobacco control interventions (eg, policy, mass media). Evidence on clinical interventions, such as smoking cessation treatment, has been addressed elsewhere.9,10,27 For the current paper, we identified the main non-clinical intervention types assessed, common methods (including assumptions) used across models, and gaps in the literature. Based on the models in this review, we aimed to provide insight regarding the strengths and limitations of evidence for various interventions to inform tobacco control research and policymaking.
Methods
Detailed methods for the overarching tobacco modeling systematic review are published elsewhere.26,28 Briefly, we searched five databases (CINAHL, Embase, PsychINFO, PubMed, and EconLit) on July 1, 2013 with no date restrictions; our unique search strategies for each database have been published elsewhere.28 Eligible studies employed a computational model to project a tobacco-related outcome (eg, tobacco use prevalence, disease prevalence, and tobacco-related costs). Although computational models can be used for a variety of purposes, for this review, we included models that were used to estimate outcomes prospectively; that is, “predictive” models. Only English language studies were included.
Eligibility Criteria
For this analysis, studies had to assess the effects of a non- clinical tobacco control intervention (eg, policy, and mass media). We deemed clinical interventions (eg, cessation treatment, and cancer screening) to be qualitatively different than non-clinical interventions. Eligible studies examined a United States—only target population and described a real or hypothetical intervention.
Data Extraction
We consulted the “Guide to Community Preventive Services” to determine intervention types for inclusion in our data extraction form.7 For each of these intervention types (ie, taxation, youth prevention interventions, smoke-free spaces, warning labels and package changes, media campaigns, marketing or advertising restrictions/bans, and other interventions), we collected details using a standardized form. For taxation studies, we recorded the amount of the tax increase and its effect on smoking prevalence. Two coders (SF and AG) jointly extracted data.
Analysis
Our analysis focused on the convergent validity of findings from computational models per guidelines from the International Society for Pharmacoeconomics and Outcomes Research and the Society for Medical Decision Making (ISPOR-SMDM) Modeling Good Research Practices Task Force.29 This involved determining the extent to which multiple models that analyzed the same question produced similar results. For papers that employed the same model across multiple studies to assess the same intervention type, we included information about how many times that model was used to assess each intervention type, but only extracted data from the most recently published study. Agreement between studies that employ identical models would be expected; synthesizing such data would not provide insight into convergent validity across models.
We synthesized the results qualitatively because the studies examined heterogeneous interventions and outcomes, employed heterogeneous model assumptions (eg, varying time horizons) and examined heterogeneous population (including variations by age, state, and race/ethnicity). However, because taxation models included standard inputs and outputs, we synthesized quantitative results from studies examining tax interventions to illustrate the relationship between cigarette price increases and smoking prevalence. We standardized all costs to 2014 dollars with the use of the Consumer Price Index inflation calculator for goods and services purchased by urban households.30 For papers that did not specify a year for costs, we assumed costs were in the paper’s publication year.
Given the goals of this review, we did not assess the risk of bias in individual studies.31 In our previous systematic review, we identified models that were used in multiple studies26; in this analysis, we highlight those methodological commonalities, where applicable. We report items in accordance with PRISMA guidelines.32
Results
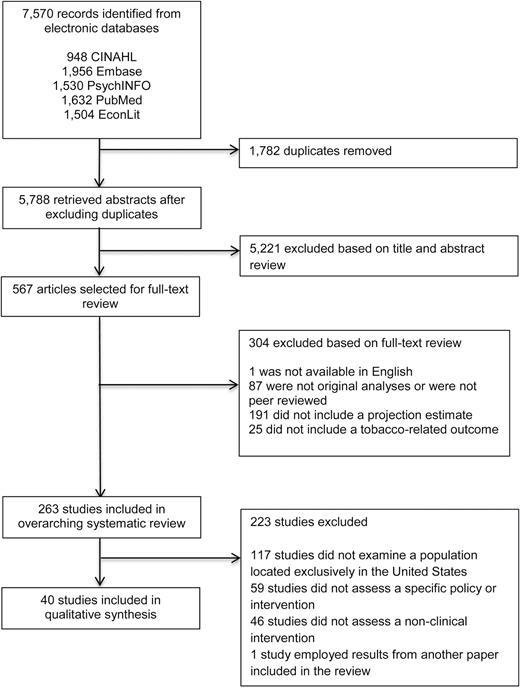
We included 40 studies in this review.33–72Figure 1 presents the study selection process.
The most frequently modeled interventions were taxation and youth prevention interventions, followed by mass media, smoke-free air policies, product regulation, and marketing/advertising restrictions (Table 1). Seven studies assessed other heterogeneous interventions. No studies examining warning labels or package changes were found.
Policies and Interventions Assessed in Each Study
| First author, year published . | Taxation . | Youthprevention . | Smoke-free policy . | Mass media . | Marketing/ Advertising . | Product regulation . | Other . | Model name, if applicable . | Longest time horizona . | Sensitivity analysisa . |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahmad, 200533 | X | Tobacco policy model | ||||||||
| Ahmad, 200534 | X | Tobacco policy model | ||||||||
| Ahmad, 200536 | X | Tobacco policy model | ||||||||
| Ahmad, 200535 | X | Tobacco policy model | ||||||||
| Ahmad, 200737 | X | X | Tobacco policy model | |||||||
| Ahmad, 200838 | X | Tobacco policy model | 20 y | Yes | ||||||
| Cutler, 200239 | X | 26 y | Yes | |||||||
| DiFranza, 200140 | X | Lifetime | Yes | |||||||
| Emery, 199942 | X | 25 y | Yes | |||||||
| Emery, 200141 | X | Kaplan model | 75 y | Yes | ||||||
| Holtgrave, 200943 | X | Lifetime | Yes | |||||||
| Kaplan, 200144 | X | Kaplan model | ||||||||
| Levy, 200046 | X | SimSmokeb | ||||||||
| Levy, 200147 | X | SimSmoke | ||||||||
| Levy, 200148 | X | SimSmoke | ||||||||
| Levy, 200149 | X | SimSmoke | ||||||||
| Levy, 200352 | X | X | X | Xc | X | SimSmoke | ||||
| Levy, 200554 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200553 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200756 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200750 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200857 | X | X | X | Xc | SimSmoke | |||||
| Levy, 201051 | X | X | Xc | SimSmoke | ||||||
| Levy, 201155 | X | SimSmoke | ||||||||
| Levy, 201273 | X | X | X | X | SimSmoke | 48 y | No | |||
| Mejia, 201058 | X | Lifetime | Yes | |||||||
| Miller, 201059 | X | 90 y | Yes | |||||||
| Ong, 200460 | X | 7 y | Yes | |||||||
| Ong, 200561 | X | 1 y | Yes | |||||||
| Rivara, 200462d | X | X | 67 y | Yes | ||||||
| Secker-Walker, 199764 | X | Lifetime | Yes | |||||||
| Secker-Walker, 200563 | X | Lifetime | Yes | |||||||
| Simpson, 201365 | X | 20 y | Yes | |||||||
| Swank, 198866 | X | 8 y | Yes | |||||||
| Tengs, 200169 | X | Tobacco policy model | ||||||||
| Tengs, 200467 | X | Tobacco policy model | ||||||||
| Tengs, 200568 | X | Tobacco policy model | ||||||||
| Villanti, 201270 | X | Lifetime | Yes | |||||||
| Wang, 200171 | X | Lifetime | Yes | |||||||
| Warner, 199472 | X | 14 y | Yes | |||||||
| Total | 15 | 17 | 11 | 13 | 2 | 4 | 7 |
| First author, year published . | Taxation . | Youthprevention . | Smoke-free policy . | Mass media . | Marketing/ Advertising . | Product regulation . | Other . | Model name, if applicable . | Longest time horizona . | Sensitivity analysisa . |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahmad, 200533 | X | Tobacco policy model | ||||||||
| Ahmad, 200534 | X | Tobacco policy model | ||||||||
| Ahmad, 200536 | X | Tobacco policy model | ||||||||
| Ahmad, 200535 | X | Tobacco policy model | ||||||||
| Ahmad, 200737 | X | X | Tobacco policy model | |||||||
| Ahmad, 200838 | X | Tobacco policy model | 20 y | Yes | ||||||
| Cutler, 200239 | X | 26 y | Yes | |||||||
| DiFranza, 200140 | X | Lifetime | Yes | |||||||
| Emery, 199942 | X | 25 y | Yes | |||||||
| Emery, 200141 | X | Kaplan model | 75 y | Yes | ||||||
| Holtgrave, 200943 | X | Lifetime | Yes | |||||||
| Kaplan, 200144 | X | Kaplan model | ||||||||
| Levy, 200046 | X | SimSmokeb | ||||||||
| Levy, 200147 | X | SimSmoke | ||||||||
| Levy, 200148 | X | SimSmoke | ||||||||
| Levy, 200149 | X | SimSmoke | ||||||||
| Levy, 200352 | X | X | X | Xc | X | SimSmoke | ||||
| Levy, 200554 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200553 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200756 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200750 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200857 | X | X | X | Xc | SimSmoke | |||||
| Levy, 201051 | X | X | Xc | SimSmoke | ||||||
| Levy, 201155 | X | SimSmoke | ||||||||
| Levy, 201273 | X | X | X | X | SimSmoke | 48 y | No | |||
| Mejia, 201058 | X | Lifetime | Yes | |||||||
| Miller, 201059 | X | 90 y | Yes | |||||||
| Ong, 200460 | X | 7 y | Yes | |||||||
| Ong, 200561 | X | 1 y | Yes | |||||||
| Rivara, 200462d | X | X | 67 y | Yes | ||||||
| Secker-Walker, 199764 | X | Lifetime | Yes | |||||||
| Secker-Walker, 200563 | X | Lifetime | Yes | |||||||
| Simpson, 201365 | X | 20 y | Yes | |||||||
| Swank, 198866 | X | 8 y | Yes | |||||||
| Tengs, 200169 | X | Tobacco policy model | ||||||||
| Tengs, 200467 | X | Tobacco policy model | ||||||||
| Tengs, 200568 | X | Tobacco policy model | ||||||||
| Villanti, 201270 | X | Lifetime | Yes | |||||||
| Wang, 200171 | X | Lifetime | Yes | |||||||
| Warner, 199472 | X | 14 y | Yes | |||||||
| Total | 15 | 17 | 11 | 13 | 2 | 4 | 7 |
aFor models used in multiple studies, we extracted data only from the most recently published paper. We answered “Yes” under the Sensitivity Analysis column if the authors varied at least one parameter or if multiple discount rates were considered.
bMethods preceded the publication of the SimSmoke model but were similar to those of SimSmoke.
cMass media campaign implemented along with other tobacco control policies.
dTo avoid duplication, we did not include data from a paper by Fishman et al.88 in this review because the relevant data in that paper were based on findings from the study by Rivara et al.62.
Policies and Interventions Assessed in Each Study
| First author, year published . | Taxation . | Youthprevention . | Smoke-free policy . | Mass media . | Marketing/ Advertising . | Product regulation . | Other . | Model name, if applicable . | Longest time horizona . | Sensitivity analysisa . |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahmad, 200533 | X | Tobacco policy model | ||||||||
| Ahmad, 200534 | X | Tobacco policy model | ||||||||
| Ahmad, 200536 | X | Tobacco policy model | ||||||||
| Ahmad, 200535 | X | Tobacco policy model | ||||||||
| Ahmad, 200737 | X | X | Tobacco policy model | |||||||
| Ahmad, 200838 | X | Tobacco policy model | 20 y | Yes | ||||||
| Cutler, 200239 | X | 26 y | Yes | |||||||
| DiFranza, 200140 | X | Lifetime | Yes | |||||||
| Emery, 199942 | X | 25 y | Yes | |||||||
| Emery, 200141 | X | Kaplan model | 75 y | Yes | ||||||
| Holtgrave, 200943 | X | Lifetime | Yes | |||||||
| Kaplan, 200144 | X | Kaplan model | ||||||||
| Levy, 200046 | X | SimSmokeb | ||||||||
| Levy, 200147 | X | SimSmoke | ||||||||
| Levy, 200148 | X | SimSmoke | ||||||||
| Levy, 200149 | X | SimSmoke | ||||||||
| Levy, 200352 | X | X | X | Xc | X | SimSmoke | ||||
| Levy, 200554 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200553 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200756 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200750 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200857 | X | X | X | Xc | SimSmoke | |||||
| Levy, 201051 | X | X | Xc | SimSmoke | ||||||
| Levy, 201155 | X | SimSmoke | ||||||||
| Levy, 201273 | X | X | X | X | SimSmoke | 48 y | No | |||
| Mejia, 201058 | X | Lifetime | Yes | |||||||
| Miller, 201059 | X | 90 y | Yes | |||||||
| Ong, 200460 | X | 7 y | Yes | |||||||
| Ong, 200561 | X | 1 y | Yes | |||||||
| Rivara, 200462d | X | X | 67 y | Yes | ||||||
| Secker-Walker, 199764 | X | Lifetime | Yes | |||||||
| Secker-Walker, 200563 | X | Lifetime | Yes | |||||||
| Simpson, 201365 | X | 20 y | Yes | |||||||
| Swank, 198866 | X | 8 y | Yes | |||||||
| Tengs, 200169 | X | Tobacco policy model | ||||||||
| Tengs, 200467 | X | Tobacco policy model | ||||||||
| Tengs, 200568 | X | Tobacco policy model | ||||||||
| Villanti, 201270 | X | Lifetime | Yes | |||||||
| Wang, 200171 | X | Lifetime | Yes | |||||||
| Warner, 199472 | X | 14 y | Yes | |||||||
| Total | 15 | 17 | 11 | 13 | 2 | 4 | 7 |
| First author, year published . | Taxation . | Youthprevention . | Smoke-free policy . | Mass media . | Marketing/ Advertising . | Product regulation . | Other . | Model name, if applicable . | Longest time horizona . | Sensitivity analysisa . |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahmad, 200533 | X | Tobacco policy model | ||||||||
| Ahmad, 200534 | X | Tobacco policy model | ||||||||
| Ahmad, 200536 | X | Tobacco policy model | ||||||||
| Ahmad, 200535 | X | Tobacco policy model | ||||||||
| Ahmad, 200737 | X | X | Tobacco policy model | |||||||
| Ahmad, 200838 | X | Tobacco policy model | 20 y | Yes | ||||||
| Cutler, 200239 | X | 26 y | Yes | |||||||
| DiFranza, 200140 | X | Lifetime | Yes | |||||||
| Emery, 199942 | X | 25 y | Yes | |||||||
| Emery, 200141 | X | Kaplan model | 75 y | Yes | ||||||
| Holtgrave, 200943 | X | Lifetime | Yes | |||||||
| Kaplan, 200144 | X | Kaplan model | ||||||||
| Levy, 200046 | X | SimSmokeb | ||||||||
| Levy, 200147 | X | SimSmoke | ||||||||
| Levy, 200148 | X | SimSmoke | ||||||||
| Levy, 200149 | X | SimSmoke | ||||||||
| Levy, 200352 | X | X | X | Xc | X | SimSmoke | ||||
| Levy, 200554 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200553 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200756 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200750 | X | X | X | Xc | SimSmoke | |||||
| Levy, 200857 | X | X | X | Xc | SimSmoke | |||||
| Levy, 201051 | X | X | Xc | SimSmoke | ||||||
| Levy, 201155 | X | SimSmoke | ||||||||
| Levy, 201273 | X | X | X | X | SimSmoke | 48 y | No | |||
| Mejia, 201058 | X | Lifetime | Yes | |||||||
| Miller, 201059 | X | 90 y | Yes | |||||||
| Ong, 200460 | X | 7 y | Yes | |||||||
| Ong, 200561 | X | 1 y | Yes | |||||||
| Rivara, 200462d | X | X | 67 y | Yes | ||||||
| Secker-Walker, 199764 | X | Lifetime | Yes | |||||||
| Secker-Walker, 200563 | X | Lifetime | Yes | |||||||
| Simpson, 201365 | X | 20 y | Yes | |||||||
| Swank, 198866 | X | 8 y | Yes | |||||||
| Tengs, 200169 | X | Tobacco policy model | ||||||||
| Tengs, 200467 | X | Tobacco policy model | ||||||||
| Tengs, 200568 | X | Tobacco policy model | ||||||||
| Villanti, 201270 | X | Lifetime | Yes | |||||||
| Wang, 200171 | X | Lifetime | Yes | |||||||
| Warner, 199472 | X | 14 y | Yes | |||||||
| Total | 15 | 17 | 11 | 13 | 2 | 4 | 7 |
aFor models used in multiple studies, we extracted data only from the most recently published paper. We answered “Yes” under the Sensitivity Analysis column if the authors varied at least one parameter or if multiple discount rates were considered.
bMethods preceded the publication of the SimSmoke model but were similar to those of SimSmoke.
cMass media campaign implemented along with other tobacco control policies.
dTo avoid duplication, we did not include data from a paper by Fishman et al.88 in this review because the relevant data in that paper were based on findings from the study by Rivara et al.62.
Three models were used across multiple studies: twelve studies employed the SimSmoke model,47–57,73 nine used the Tobacco Policy Model (TPM),33–38,67–69 and two employed the Kaplan model.41,44 One study served as a precursor to the SimSmoke model,74 so was coded as a SimSmoke study. Methods for these models are described elsewhere.26
Taxation
Fifteen studies investigated the impact of a cigarette tax on smoking prevalence.35,37,38,41,44,50–54,56,57,62,73,74 No studies examined the impact of taxes on non-cigarette products or the impact of a cigarette tax on the prevalence of non-cigarette tobacco use. Three of the 15 taxation studies employed the TPM,35,37,38 two employed the Kaplan model,41,44 and nine used SimSmoke.50–54,56,57,73,74 As noted in the Methods, for papers employing the same model across multiple studies to assess the same intervention type, we extracted data only from the most recent study. Thus, we discuss the most recent TPM paper,38 SimSmoke paper,73 Kaplan paper,41 and one remaining study.62
The four taxation papers38,41,62,73 were diverse in their assumptions (Table 2) and study designs, but all found a positive relationship between taxation and decreases in smoking prevalence. These studies considered tax increases ranging from $0.7141 to $4.6338 and employed different assumptions regarding the economic elasticity of cigarettes. Two studies38,73 assumed price elasticity varied by age; a price elasticity range of −0.673 to −0.83138 was assumed for youth (ages 15–17), and a price elasticity range of −0.373 to −0.356538 was assumed for young adults (ages 18–24 and ages 18–23, respectively). Categorization of older age groups varied between the two studies; Ahmad et al. assumed a price elasticity of −0.328638 for an oldest age group of ≥65, whereas Levy, Boyle and Abrams assumed a price elasticity of −0.173 for its oldest age group (≥35). One study focused on Latino smokers in California and assumed a Latino-specific price elasticity that ranged from −0.8 to −1.2.41 Another study assumed a price elasticity for youth smokers that ranged from 0.0 to −1.2.62 Three studies examined the effect of a cigarette tax on adults aged ≥1838,41,73 and one examined the effect for a cohort of 18 year-olds.62
Assumptions for Models Examining Tax Increases
| Study ID . | Pre-tax cost of cigarette package in 2014 dollarsa . | Tax amount(s) in 2014 dollarsa . | Population . | Price elasticity . | Notes . | |
|---|---|---|---|---|---|---|
| Ahmad, 200838 | $4.63 | $0.92, $1.85, $2.78, $3.70, $4.63 | US population | Age | Price elasticity for smokers | Federal excise tax; the authors conducted sensitivity analyses whereby they varied the price elasticity assumptions by −50%, −25%, 0%, +25% and +50%. |
| 15–17 | −0.831 | |||||
| 18–23 | −0.3565 | |||||
| 24–29 | −0.2957 | |||||
| 30–39 | −0.1809 | |||||
| 40–65 | −0.1979 | |||||
| ≥65 | −0.3286 | |||||
| Emery, 200141 | $3.55 | $0.71 and $1.42 | Adult Latino smokers in California | Price elasticity assumptions were Latino-specific and analyses were conducted with price elasticity valued at −0.8, −1.0, and −1.2 | State excise tax | |
| Levy, 201273 | Not specified | $1.66 | Current, never, and former smokers aged ≥ 18 years in Minnesota | Age | Price elasticity | Tax amount includes an excise tax, a health impact fee and an additional tax in lieu of a sales tax |
| 15–17 | −0.6 | |||||
| 18–24 | −0.3 | |||||
| 25–34 | −0.2 | |||||
| ≥35 | −0.1 | |||||
| Rivara, 200462 | $4.58 | $1.42 | 18 year olds in the United States | Analyses were conducted with price elasticity valued at −0.6, −1.2, and 0.0 | State and federal excise taxes | |
| Study ID . | Pre-tax cost of cigarette package in 2014 dollarsa . | Tax amount(s) in 2014 dollarsa . | Population . | Price elasticity . | Notes . | |
|---|---|---|---|---|---|---|
| Ahmad, 200838 | $4.63 | $0.92, $1.85, $2.78, $3.70, $4.63 | US population | Age | Price elasticity for smokers | Federal excise tax; the authors conducted sensitivity analyses whereby they varied the price elasticity assumptions by −50%, −25%, 0%, +25% and +50%. |
| 15–17 | −0.831 | |||||
| 18–23 | −0.3565 | |||||
| 24–29 | −0.2957 | |||||
| 30–39 | −0.1809 | |||||
| 40–65 | −0.1979 | |||||
| ≥65 | −0.3286 | |||||
| Emery, 200141 | $3.55 | $0.71 and $1.42 | Adult Latino smokers in California | Price elasticity assumptions were Latino-specific and analyses were conducted with price elasticity valued at −0.8, −1.0, and −1.2 | State excise tax | |
| Levy, 201273 | Not specified | $1.66 | Current, never, and former smokers aged ≥ 18 years in Minnesota | Age | Price elasticity | Tax amount includes an excise tax, a health impact fee and an additional tax in lieu of a sales tax |
| 15–17 | −0.6 | |||||
| 18–24 | −0.3 | |||||
| 25–34 | −0.2 | |||||
| ≥35 | −0.1 | |||||
| Rivara, 200462 | $4.58 | $1.42 | 18 year olds in the United States | Analyses were conducted with price elasticity valued at −0.6, −1.2, and 0.0 | State and federal excise taxes | |
aCosts were converted to 2014 dollars using the CPI inflation calculator available at http://data.bls.gov/cgi-bin/cpicalc.pl (Accessed December 20, 2015).
Assumptions for Models Examining Tax Increases
| Study ID . | Pre-tax cost of cigarette package in 2014 dollarsa . | Tax amount(s) in 2014 dollarsa . | Population . | Price elasticity . | Notes . | |
|---|---|---|---|---|---|---|
| Ahmad, 200838 | $4.63 | $0.92, $1.85, $2.78, $3.70, $4.63 | US population | Age | Price elasticity for smokers | Federal excise tax; the authors conducted sensitivity analyses whereby they varied the price elasticity assumptions by −50%, −25%, 0%, +25% and +50%. |
| 15–17 | −0.831 | |||||
| 18–23 | −0.3565 | |||||
| 24–29 | −0.2957 | |||||
| 30–39 | −0.1809 | |||||
| 40–65 | −0.1979 | |||||
| ≥65 | −0.3286 | |||||
| Emery, 200141 | $3.55 | $0.71 and $1.42 | Adult Latino smokers in California | Price elasticity assumptions were Latino-specific and analyses were conducted with price elasticity valued at −0.8, −1.0, and −1.2 | State excise tax | |
| Levy, 201273 | Not specified | $1.66 | Current, never, and former smokers aged ≥ 18 years in Minnesota | Age | Price elasticity | Tax amount includes an excise tax, a health impact fee and an additional tax in lieu of a sales tax |
| 15–17 | −0.6 | |||||
| 18–24 | −0.3 | |||||
| 25–34 | −0.2 | |||||
| ≥35 | −0.1 | |||||
| Rivara, 200462 | $4.58 | $1.42 | 18 year olds in the United States | Analyses were conducted with price elasticity valued at −0.6, −1.2, and 0.0 | State and federal excise taxes | |
| Study ID . | Pre-tax cost of cigarette package in 2014 dollarsa . | Tax amount(s) in 2014 dollarsa . | Population . | Price elasticity . | Notes . | |
|---|---|---|---|---|---|---|
| Ahmad, 200838 | $4.63 | $0.92, $1.85, $2.78, $3.70, $4.63 | US population | Age | Price elasticity for smokers | Federal excise tax; the authors conducted sensitivity analyses whereby they varied the price elasticity assumptions by −50%, −25%, 0%, +25% and +50%. |
| 15–17 | −0.831 | |||||
| 18–23 | −0.3565 | |||||
| 24–29 | −0.2957 | |||||
| 30–39 | −0.1809 | |||||
| 40–65 | −0.1979 | |||||
| ≥65 | −0.3286 | |||||
| Emery, 200141 | $3.55 | $0.71 and $1.42 | Adult Latino smokers in California | Price elasticity assumptions were Latino-specific and analyses were conducted with price elasticity valued at −0.8, −1.0, and −1.2 | State excise tax | |
| Levy, 201273 | Not specified | $1.66 | Current, never, and former smokers aged ≥ 18 years in Minnesota | Age | Price elasticity | Tax amount includes an excise tax, a health impact fee and an additional tax in lieu of a sales tax |
| 15–17 | −0.6 | |||||
| 18–24 | −0.3 | |||||
| 25–34 | −0.2 | |||||
| ≥35 | −0.1 | |||||
| Rivara, 200462 | $4.58 | $1.42 | 18 year olds in the United States | Analyses were conducted with price elasticity valued at −0.6, −1.2, and 0.0 | State and federal excise taxes | |
aCosts were converted to 2014 dollars using the CPI inflation calculator available at http://data.bls.gov/cgi-bin/cpicalc.pl (Accessed December 20, 2015).
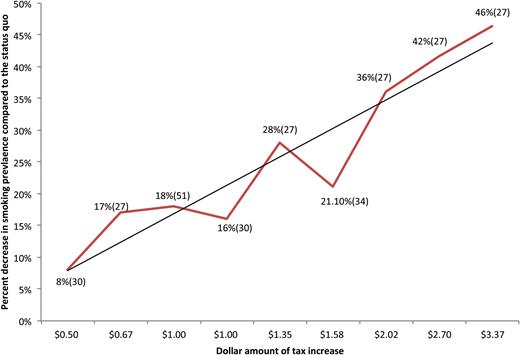
Figure 2 illustrates the findings of these studies and shows a linear relationship between taxation and projected smoking prevalence. For this figure, we synthesized results from these four studies using two guiding principles: (1) if sensitivity analyses were conducted, we included the most conservative estimate of impact on smoking prevalence; and (2) if multiple analytic horizons were used, we included the longest one. The decrease in smoking prevalence attributable to a tax on cigarettes ranged from 8% (from a $0.71 tax) to 46% (from a $4.63 tax).
Relationship between cigarette tax increase and smoking prevalence. Data points indicate percent decrease in smoking prevalence compared to the status quo (reference number).
Youth Prevention
Fifteen studies assessed youth prevention interventions; 12 assessed youth access interventions33,34,37,40,48,50,52–54,56,57,73 and three assessed school-based education interventions.57,69,71
Youth Access
Eight of the 12 youth access papers employed the SimSmoke model48,50,52–54,56,57,73 and three employed the TPM.33,34,37 Thus, one SimSmoke study,73 one TPM study,37 and one other study40 are discussed below.
The specific youth access interventions examined across papers were heterogeneous. The SimSmoke study assessed the impacts of strongly-enforced/well-publicized and weakly-enforced youth access restrictions.73 Enforcement was defined in terms of compliance checks, penalties for noncompliance, publicity/merchant awareness, and community participation. The TPM was used to examine the impact of raising the national minimum legal tobacco purchasing age to 21.37 DiFranza et al. assessed an enforcement approach whereby law enforcement agencies identify merchants who do not comply with youth access laws by employing minors to attempt tobacco purchases.40 Analyses included a range of enforcement-related costs from $50 to $350 per outlet for four inspections per year. These costs included, among other costs, payroll for personnel who license vendors, supervise inspectors, administer civil fines, and handle legal challenges in court.
While the youth access studies employed diverse model assumptions and projected heterogeneous outcomes, they all found that youth access interventions produced favorable results. The SimSmoke model assumed that, depending on enforcement level and publicity, youth access restrictions would produce between a 2.5%–30% relative reduction in smoking prevalence among youth in the year of implementation and the same rate of reduction in initiation and cessation in subsequent years.73 The TPM projected that, compared to the expected rates of smoking under the status quo, raising the minimum legal tobacco purchasing age to 21 would produce a 14.6% decrease in smoking prevalence among 15–17 year-olds and an 8.7% decrease in smoking prevalence among adults after 75 years.37 DiFranza et al. examined the costs saved by 5%, 10%, 25% and 50% reductions in youth tobacco use resulting from enforcement and found that the cost per life-year saved ranged from $65–$12 095, depending on the model assumptions employed.40
Youth Education
The programs assessed across the three school-based education intervention studies57,69,71 differed from one another. Levy et al. used SimSmoke to assess a hypothetical “well-tested school education program accompanied by a media campaign” implemented in Kentucky.57 Wang et al. examined an actual campaign, Project Toward No Tobacco Use, designed to prevent tobacco use among junior and senior high school students (the efficacy of this campaign was evaluated from 1989 to 1991).71 Tengs et al. used the TPM to examine a hypothetical intensive national school-based tobacco prevention program delivered to seventh and eighth grade students.69
Youth education interventions were found to reduce tobacco use, and two studies examining economic outcomes found that these interventions were reasonable to implement from a cost perspective. Levy et al. projected that, over 20 years, a school education program (accompanied by a media campaign) would reduce adult smoking prevalence by 5.3% compared to the status quo. This is equal to six smoking-attributable deaths averted compared to the status quo scenario.57 The small number of smoking-attributable deaths averted is likely due to the short analytic horizon, as most of the health benefits resulting from youth interventions are not seen for many years. Wang et al. estimated that, of 770 students exposed to Project Toward No Tobacco Use, 34.9 (low estimate: 19.7; high estimate 51.0) established smokers would be prevented, translating into $24 119 per life-year saved ($15 363 per Quality Adjusted Life-Year (QALY)).71 Tengs et al. estimated that the tobacco prevention intervention would reduce smoking initiation rates by 5.8%–64% for seventh grade students and 5%–56% for eighth grade students, translating to $6963–$483 135 per QALY saved.69
Smoke-Free Policies
Eleven studies examined smoke-free policies, nine of which employed SimSmoke.49–54,56,57,73 The most recent SimSmoke paper73 and two other studies are discussed below.60,61 These studies examined the effect of indoor smoke-free air policies on combustible tobacco use. Outdoor smoke-free policies and the effects of smoke-free policies on smokeless tobacco use were not examined.
The smoke-free policy studies employed heterogeneous assumptions regarding the effectiveness of the intervention. In the SimSmoke paper, Levy et al. assumed that a smoke-free policy implemented in Minnesota would produce between a 2%–6% relative reduction in smoking prevalence in the year of implementation and a 2%–6% reduction in initiation and cessation rates in subsequent years (over 30 years), depending on the enforcement level.73 Ong and Glantz estimated that 14.2% (n = 10 400) of indoor workers who smoked prior to the implementation of a smoke-free policy for all indoor workplaces in Minnesota would quit after 1 year.61 In a separate study, Ong and Glantz estimated that making all US indoor workplaces smoke-free would produce 725 000 new quitters (14.7% of current smokers affected by the policy) and 14.1 million former passive smokers aged 35–64 after 1 year.60
While different outcomes were estimated across the smoke-free policy studies, they all found that smoke-free policies were beneficial. Considering varying enforcement levels, SimSmoke predicted that, with the policy implemented by 2011, smoking prevalence would be reduced by 7.9% for men and 8.2% for women over 30 years.73 This translated to more than 9000 cumulative smoking-attributable deaths averted.73 The Minnesota-based study by Ong and Glantz estimated the cost-effectiveness of the smoke-free policy and found that it would cost $1068 per quitter ($676 per QALY).61 For the analysis of a nation-wide smoke-free policy, Ong and Glantz considered the effect of the intervention on strokes and myocardial infarctions and predicted that 610 deaths would be averted 1 year after implementation, translating to $82 million in medical costs averted.60 The model predicted that, after 7 years, 2420 deaths would be averted, nearly $385 million in medical costs.
Mass Media Campaigns
Thirteen studies investigated the effects of a mass media campaign.43,47,50–54,56,57,62,64,70,73 Nine of these studies employed SimSmoke.47,50–54,56,57,73 The most recent SimSmoke study73 and four other studies43,62,64,70 are discussed below. Mass media interventions have operated through one or more media channels including television, radio, print media and billboards and, more recently, via internet-based social media platforms. Content typically includes providing information regarding adverse effects of smoking, motivational messages to quit or not start, and where to find smoking cessation resources. Mass media interventions are designed to change knowledge, attitudes and smoking behaviors while also changing social norms about smoking.75
The mass media campaigns examined across papers were diverse. The SimSmoke model considered the effects of a media campaign implemented in Minnesota.73 Rivara et al. estimated the effects of a hypothetical “large-scale” mass media intervention.62 Two studies evaluated national campaigns sponsored by the American Legacy Foundation.43,70 Become an EX, evaluated by Villanti et al., was a cessation campaign for adult smokers,70 and truth, evaluated by Holtgrave et al., was a youth smoking prevention campaign.43 Secker-Walker et al. evaluated a smoking prevention television and radio campaign implemented in Montana and the northeastern United States.64
Although diverse, these studies all found that mass media campaigns produced favorable results, and the studies with economic outcomes found that it made sense from a cost perspective to implement these interventions. The SimSmoke model assumed that, depending on the level of publicity, a mass media campaign could produce between a 1.2%–6% relative reduction in smoking prevalence over the next year and in initiation and cessation in future years.73 This translated to more than 12 000 smoking-attributable deaths averted over 30 years due to the campaign. Rivara et al. estimated that the hypothetical multimedia campaign, implemented for a cohort of 18-year-olds in the year 2000, would produce a 9% decrease in smoking prevalence in this cohort by 2067, saving 544 841 years of potential life lost.62 Villanti et al. estimated that, among a hypothetical nationwide cohort of smokers aged 18–49 (n = 2 012 000), Become an EX produced 4238 additional quits and saved 4450 QALYs ($41 220–$89 714 per QALY) during the campaign period in 2008.70 Holtgrave et al. estimated that truth averted between 169 800 and 300 000 tobacco use cases in the United States. This translated to 178 290–1 050 000 QALYs saved, which, at most, would cost $5914 per QALY saved.43 Secker-Walker et al. estimated that the multimedia campaign implemented in Montana and the northeastern United States would produce a 5.5% relative decrease in smoking prevalence in weekly smoking compared to schools that did not receive the campaign, costing between $48–$2613 per life year saved, depending on the model assumptions.64
Marketing and Advertising Bans
Two studies evaluated the effects of a marketing or advertising ban and found that these interventions produced favorable results.42,52 Levy et al., using SimSmoke, estimated that a national ban on all tobacco advertising could produce a 5.3% and 6.1% relative reduction in adult smoking after 5 and 40 years (beginning in 2000), respectively, compared with the status quo scenario.52 This translated to an additional 13 493 smoking-attributable deaths averted over 40 years compared to the status quo. Emery et al. projected that banning all tobacco industry advertising and promotional activities for 25 years (beginning in 1998) could avert nearly 60 000 smoking-attributable deaths annually.42 This would save nearly 900 000 life-years and $4.15 billion in medical expenses.
Product Regulations
Four studies examined potential product regulations implemented nationally. One study examined a menthol cigarette ban55 and three studies examined regulations to mandate changes to the content of cigarettes.36,67,68
Levy et al. examined the potential effects of a menthol cigarette ban on population-level health using SimSmoke.55 They predicted that the ban could avert between 323 107 and 633 252 smoking attributable deaths over 40 years.
The three studies that examined regulations to mandate cigarette content changes considered the potential unintended negative consequences of regulation—that some individuals might smoke more, instead of less—and identified threshold values at which the positive outcomes of regulation would likely outweigh the negative outcomes. Ahmad et al. examined the effect of making cigarettes less harmful and/or less addictive.36 They found that making cigarettes less addictive or less harmful would produce a net gain in population health in all scenarios modeled if smoking behavior improved by 60% and 40%, respectively. Tengs et al. also examined the effects of making cigarettes less addictive.68 They concluded that, if nicotine reduction in cigarettes caused at least a 20% reduction in cigarette initiation and relapse and at least a 20% increase in cessation, the result of regulation would be positive under all scenarios examined. In another study, Tengs et al. examined the effect of making cigarettes safer.67 They found that, if cigarettes could be altered in such a way that excess mortality among smokers decreased by at least 70%, there would be a net population health benefit regardless of changes in smoking behavior.
Other Policies and Interventions
Seven studies assessed other interventions that could not be easily categorized. These studies drastically varied by intervention type, setting, study design and outcomes modeled. Findings from two local-level studies demonstrated the cost-effectiveness of a community-based cessation intervention for women63 and the cost savings that a hospital could experience from hiring nonsmokers.66 Evaluations of state-level comprehensive tobacco control programs in California59 and New York65 predicted that these programs would produce net positive benefits, even after considering increased healthcare costs from an extended lifetime59 and uncertainty in model parameter estimates.65 Other state-level studies similarly showed that tobacco control interventions produced favorable results; Warner et al. found that a ban on the sale of tobacco products in Michigan would increase employment and health,72 and Cutler et al. found that the Master Settlement Agreement produced net benefits in Massachusetts, granted that the “loss of pleasure” foregone by quitting smoking was not assumed to offset the benefits of smoking cessation.39 Mejia et al. examined the promotion of smokeless tobacco as a harm reduction strategy and found that this strategy was unlikely to produce substantial health benefits.58 This study was the only one in this review to explicitly include a non-cigarette tobacco product in its model.
Studies That Assessed Multiple Interventions
Ten studies examined the effects of multiple interventions,37,50–54,56,57,62,73 eight of which employed SimSmoke.50–54,56,57,73
Taxation was found to be a more effective strategy than other interventions. The most recent SimSmoke paper,73 Rivara et al.,62 and Ahmad et al.37 all compared multiple interventions, including taxation. The SimSmoke study found that taxation was more effective than smoke-free air policies, a hypothetical tobacco media campaign, and youth access in reducing smoking prevalence. Rivara et al. found that taxation was more effective than a multimedia campaign. Ahmad et al. examined different levels of taxation compared with raising the legal tobacco purchasing age to 21 in the United States and found that taxation was only more effective than the age increase when the price was sufficiently high; specifically, after 75 years, enforcing a higher smoking age in the present would reduce smoking prevalence comparable to a 40% price increase.
The SimSmoke study73 and Rivara et al.62 examined the effects of implementing multiple interventions together and found that combined interventions produced more favorable outcomes than interventions implemented in isolation, even taxation. The SimSmoke model found youth access policies to be the least effective of the policies examined; smoke-free air laws and mass media campaigns followed taxation in favorability, with smoke-free air laws producing slightly more favorable results than mass media.
Discussion
In this systematic review of studies using computational models to project the impact of selected tobacco control interventions, evidence from multiple studies demonstrated the independent effect of taxation on decreasing future smoking prevalence. This finding is consistent with evaluations of enacted taxation policies, which strongly support price increases as a tobacco control strategy.4–6 Two models compared multi-component interventions with independent interventions and found that multi-component interventions produced more favorable results. This is consistent with CDC’s recommendation that tobacco control interventions are most effective when implemented in a comprehensive manner.8
Models for other tobacco control interventions generally showed that these strategies are expected to decrease smoking, benefit population health, and are reasonable to implement from a cost perspective.36,37,40–43,52,60–62,67–71,73 However, it is difficult to draw generalized conclusions regarding the magnitude of the effects of these interventions. This is not to say that these policies are necessarily weak. Rather, in the papers included this review, non-taxation policies were not quantified in a consistent way. The SimSmoke model, for example, explores the impact of mass media campaigns implemented with different levels of intensity, defined by differential levels of funding.73 Defining intensity in this way precludes us from directly comparing the SimSmoke findings with analyses of mass media campaigns that do not consider costs.62 Moreover, categorizing the intensity of an intervention according to costs does not account for how those costs are used and, thus, may not be an accurate measure of intensity; the reach of campaigns with similar budgets may differ dramatically depending on how funds are used. Thus, because we cannot quantify the intensity of these policies across studies—as opposed to taxes, where the dollar amount represents a somewhat standard measure—and because these studies were heterogeneous in many ways, we cannot assess the relative effectiveness of these interventions. It should also be noted, this review is limited in that it does not include cessation treatment interventions, which simulation models have also shown to be effective.27,51,76 Additionally, in some cases, the evidence was not conducive to assessing convergent validity, as 29% (12/41) of the studies employed the SimSmoke model and 22% (9/42) employed the TPM.
Limitations
The results of this study should be considered in light of some limitations. We restricted the papers in this review to those that examined US-based populations in order to focus our analysis on a somewhat homogenous population. This decision may have been too restrictive, as the exclusion of international studies may have introduced bias if those studies approach modeling differently than US-based studies. Conversely, our exclusion criteria may have been too broad, as several US-based models examined geographic50,57,73 and racial/ethnic41,42 subpopulations and, thus, may not be comparable to studies examining the entire US population. Given the vastness and diversity of the tobacco modeling literature,26 we believe that this review strikes a balance between including studies that can reasonably be discussed together, despite their heterogeneity, and excluding other studies.
The models in this review have some limitations with regard to their utility for informing tobacco-related policy-making. First, most of the studies modeled the effect of an intervention on cigarette use and found that the intervention reduced smoking prevalence. While we have no reason to believe that any of these interventions would increase smoking prevalence, the benefits of these interventions may have been overstated with respect to long-term health outcomes. The taxation studies, for example, do not consider how a cigarette tax might impact the use of other, less expensive, but similarly toxic combustible tobacco products. The models also have not sufficiently incorporated effects of the introduction of other, possibly safer products, and issues such as differential taxation according to product harm potential, whether such products are effective substitutes for existing products, cohort effects, etc. Interactions and synergistic effects of multiple types of interventions and policies were not modeled in most of the studies in this review. This potentially underestimates the impacts of these interventions, as policies implemented together may enhance the effects of one another, even if their impacts in isolation are weak.6,77,78 Interactions (eg, policy impact on tobacco education or cessation treatment) and feedback mechanisms (eg, tobacco industry response to regulation) that could produce unexpected results are rarely considered, and positive intervention effects are typically assumed. Thus, a systems approach to constructing models may be the most appropriate way to represent the complex tobacco control environment.79 Third, the models did not assess the potential impact of many policies that have been introduced in recent years, such as non-cigarette tobacco product taxes, outdoor smoke-free air laws, and bans on the sale of non-menthol flavored cigarettes.
The need for standardizing computational modeling methods has been emphasized.80 This includes providing greater detail on all aspects of model and parameter development to facilitate transparency and validation.29 Here, we provide additional recommendations specifically for models evaluating tobacco control interventions. These guidelines are informed by the belief that overall tobacco use, as opposed to cigarette use, is the best indicator of whether an intervention ultimately induces or minimizes harm. First, we recommend that models consider the effects of interventions on uptake, cessation and relapse rates of multiple tobacco products, including transition patterns between products to examine possible substitution behaviors. While only one study included in this review included multiple tobacco products,58 other models that have been published since our search date have addressed this issue81,82 and can provide frameworks for future studies. Second, to capture how changes in tobacco behavior may affect long-term harm, we recommend that modelers consider the risk profiles of different products. Empirical evidence is needed to support the implementation of this recommendation; however, researchers can use data informed by expert panels83,84 to populate models that are developed in the short-term. Third, we recommend that researchers consider the potential unintended consequences of any intervention assessed that would not be captured by our first two recommendations. Three of the product regulation studies in this review36,67,68 provide an example of this; they include analyses to determine when the intervention might produce a negative outcome. Fourth, more sophisticated models, such as system dynamic models, agent-based models, and hybrid models, may be needed as the tobacco landscape evolves to account for multilevel influences on behavior and feedback loops, such as the behavior of the tobacco industry and other factors currently not included in most models.79,85 With new tobacco products available to consumers, the tobacco environment is becoming increasingly complex,86 and this complexity should be reflected in the models used to inform tobacco-related decision-making. Fifth, more attention must be paid to model validation and calibration.87 Validation includes evaluation of model structure, data sources, assumptions, and results; comparison of results with other models; and external and predictive validity, the latter of which is rarely seen.29 Our recommendations aim to help policymakers and researchers minimize harm and maximize overall population-level health benefits by considering the real-world context in which tobacco control interventions are implemented.
Funding
This work was supported by Truth Initiative. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report. All authors are employed by the sponsor. No financial disclosures were reported by the authors of this paper.
Declaration of Interests
None declared.
Acknowledgments
We would like to acknowledge Donna Hesson at the Welch Medical Library for her assistance with the search strategy. We thank Jodie Briggs for her help in preparing this manuscript for publication.
References



Comments